Alcoholic liver disease
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
| Alcoholic liver disease | |
 | |
|---|---|
| Microscopy of liver showing fatty change, cell necrosis, Mallory bodies | |
| ICD-10 | K70 |
| ICD-9 | 571.1 |
| MedlinePlus | 000281 |
| MeSH | D008108 |
Alcoholic liver disease is the major cause of liver disease in Western countries, (in Asian countries, viral hepatitis is the major cause). It arises from the excessive ingestion of alcohol and can present as fatty liver, alcoholic hepatitis, and cirrhosis. Fatty liver and alcoholic hepatitis are reversible with abstinence from alcohol. Alcoholic hepatitis involves acute or chronic inflammation of liver parenchyma and is the most common precursor of cirrhosis in the United States
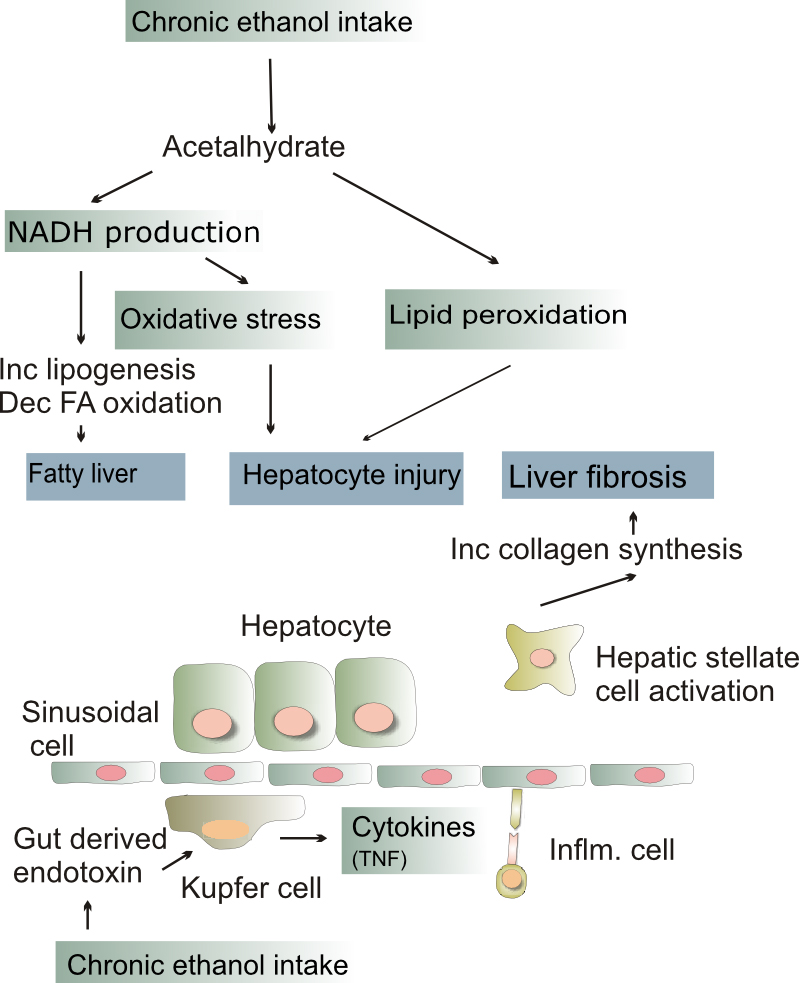
Pathophysiology
Fatty change and alcoholic hepatitis are probably reversible. The later stages of fibrosis and cirrhosis tend to be irreversible but can usually be quite well managed for long periods of time. The cause of fatty change are:
- The excess generation of NAD by the enzymes alcohol dehydrogenase and aldehyde dehydrogenase which cause shunting of normal substrates from catabolism towards lipid biosynthesis.
- Impaired assembly and secretion of lipoproteins and increased peripheral lipid catabolism may also contribute
The cause of alcoholic hepatitis are:
- Acetaldehyde formed from alcohol induces lipid peroxidation and acetaldehyde protein adduct formation which disrupt cytoskeleton
- Directly affect microtubule organization, mitochondrial function and membrane fluidity
- Generation of ROS
- Neutrophil attack at the site of hepatocyte necrosis
Fatty change
- Fatty change, or steatosis is the accumulation of fat in liver cells which can be seen as fatty globules under the microscope.
- Alcoholism causes large fatty globules (macrovesicular steatosis).
- Other causes of macrovesicular steatosis include diabetes, obesity and starvation.
- Alcoholic fatty change is probably dose related.
- Small fatty globules have different causes.
Alcoholic hepatitis
- Some people get an acute hepatitis or inflammatory reaction to the cells affected by fatty change. This is not directly related to the dose of alcohol.
- Some people seem more prone to this reaction than others. This is called alcoholic steatonecrosis and the inflammation probably predisposes to liver fibrosis.
Liver fibrosis
- Liver fibrosis, in itself, is largely asymptomatic but as it progresses it can turn into cirrhosis, where the fibrosis alters the architecture and impairs the function of the liver.
Cirrhosis
- Cirrhosis is a late stage of liver disease marked by fibrosis and altered liver architecture.
- It is often progressive and may eventually lead to liver failure.
- Late complications of cirrhosis or liver failure include portal hypertension, coagulation disorders, ascites and other complications including hepatic encephalopathy and the hepatorenal syndrome.
- Cirrhosis also has number of other causes, such as hepatitis and toxins. The late stages of cirrhosis (say from viral hepatitis or alcohol) may look similar. This phenomenon is termed a "final common pathway" for a disease.
Differential diagnosis
- Cholecystitis
- Cholelithiasis
- Drug toxicity
- Hepatitis (viral, autoimmune)
- Nonalcoholic fatty liver disease
History and symptoms
History
- Recent history of heavy drinking
- Chronic alcohol intake i.e. > 80 g/d in men and 40 g/d in women with alcoholic hepatitis or cirrhosis.
Symptoms
- Heaviness and pain below right side of chest (hepatomegaly)
- Abdominal pain
- Jaundice
- Anorexia
- Nausea/vomiting
Physical examination
- Fever
- Jaundice
- Abdominal tenderness
- Hepatosplenomegaly
- Ascites
- Confusion, coma (encephalopathy)
Lab diagnosis
Hemogram
- Macrocytic Anemia
- Thrombocytopenia (causes are toxic effect of alcohol on platelet and splenomegaly)
- Leukocytosis
Liver function test
- Raised serum bilirubin
- Elevated liver enzyme
- AST usually elevated more than ALT (commonly by factor of 2 or more)
- AST usually elevated but not more than 300 u/L
- Elevated alkaline phosphatase (infrequently more than 3 times of normal)
- Prolonged prothrombin time (> 6 seconds above control)
- Serum protein
- Decreased serum albumin
- Increased gamma globulin
- Iron studies
- Increased transferrin saturation, hepatic iron stores, and sideroblastic anemia
- Folic acid deficiency
Ultrasonography
- Used for excluding biliary obstruction
- Ascites
CT scan
- To exclude pancreatic disease
- To exclude Space occupying lesions
- Collateral vessels
MRI
- To exclude pancreatic disease
- To exclude space occupying lesions
- Collateral vessels
Other studies
Liver biopsy
- Fatty liver
- Macrovesicular fat
- Alcoholic hepatitis
- Polymorphonuclear infiltration
- Hepatic necrosis
- Mallory bodies in hepatocytes
- Perivenular and perisinusoidal fibrosis
- Ballooning hepatocytes
- Steatosis,
- Alcoholic cirrhosis
Treatment
Medical therapy
General
- Abstinence from alcohol
- Counseling and family support during alcohol abstinence
- Naltrexone or acamprosate to reduce relapse
- Nutritional support - Adequate amounts of carbohydrates and calories as alcoholics are commonly malnourished. This prevents endogenous protein catabolism, and hypoglycemia. Administration of thiamine is important with glucose supplements. This is so because glucose administration increases B1 consumption and B1 deficiency may lead to Wernicke–Korsakoff syndrome.
- Folic acid, thiamine, and zinc supplements are recommended.
Prognosis
In absence of steroid therapy 1 in every three patient dies.
Poor Prognostic factor
- Prolonged prothrombin time
- Serum Bilirubin >10 mg/dL
- Hepatic encephalopathy
- Azotemia
- Leukocytosis
- Unresponsive to steroid treatment
- Reversal portal flow on doppler USG
Prognostic scores
- MELD score for cirrhosis
- Glasgow alcoholic hepatitis score (age, white blood cell, blood urea nitrogen, prothrombin time ratio, and bilirubin level)
- ABIC score - age, serum bilirubin, serum creatinine
Drug therapy
Alcoholic hepatitis
- Methylprednisolone
- Decreases short term mortality
- Usually given for 1 month
- Serum bilirubin is used as a predictor for treatment success. Failure of the serum bilirubin level to decline after 7 days of treatment predicts poor prognosis
- Another predictor of treatment is Lille model comprising, age, serum creatinine, serum albumin, prothrombin time (or INR), serum bilirubin on admission, and serum bilirubin on day 7
- Pentoxifylline
- It is a tumor necrosis factor inhibitor
- Used in patients with contraindications to steroids
- Usually given for 1 months
- Decreases mortality
- Decreases risk of hepatorenal syndrome
Other less commonly used drugs