Acne vulgaris
Template:DiseaseDisorder infobox Editor-In-Chief: C. Michael Gibson, M.S., M.D. [2]
|
WikiDoc Resources for Acne vulgaris |
|
Articles |
|---|
|
Most recent articles on Acne vulgaris Most cited articles on Acne vulgaris |
|
Media |
|
Powerpoint slides on Acne vulgaris |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Acne vulgaris at Clinical Trials.gov Trial results on Acne vulgaris Clinical Trials on Acne vulgaris at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Acne vulgaris NICE Guidance on Acne vulgaris
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Acne vulgaris Discussion groups on Acne vulgaris Patient Handouts on Acne vulgaris Directions to Hospitals Treating Acne vulgaris Risk calculators and risk factors for Acne vulgaris
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Acne vulgaris |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
For patient information click [[
|
Acne vulgaris Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Acne vulgaris On the Web |
|
American Roentgen Ray Society Images of Acne vulgaris |
(patient information)|here]]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [3] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Acne Vulgaris (commonly called Acne) is a skin disease, caused by changes in the pilosebaceous units (skin structures consisting of a hair follicle and its associated sebaceous gland). Severe acne is inflammatory, but acne can also manifest in noninflammatory forms.[1] Acne lesions are commonly referred to as pimples, spots, or zits.
In the United States, acne affects 17 million people. It is most common during adolescence, affecting more than 85% of teenagers, and frequently continues into adulthood. [2] For most people, acne diminishes over time and tends to disappear, or at least decrease, after one reaches his or her early twenties. There is, however, no way to predict how long it will take for it to disappear entirely, and some individuals will continue to suffer from acne decades later, into their thirties and forties and even beyond.[3]
The term acne comes from a corruption of the Greek άκμή (acme in the sense of a skin eruption) in the writings of Aëtius Amidenus. The vernacular term bacne or backne is often used to indicate acne found specifically on one's back.[4] or backne is often used to indicate acne found specifically on one's back.[5]
Diagnosis
Common Causes
Acne develops as a result of blockages in follicles. Hyperkeratinization and formation of a plug of keratin and sebum (a microcomedo) is the earliest change. Enlargement of sebaceous glands and an increase in sebum production occur with increased androgen (DHEA-S) production at adrenarche. The microcomedo may enlarge to form an open comedo (blackhead) or closed comedo (whitehead). Increased sebum production provides an environment for the overgrowth of Propionibacterium acnes. Bacterial overgrowth of Propionibacterium acnes can cause inflammation, leading to inflammatory lesions (papules, pustules, or nodules) in the dermis around the microcomedo or comedo, which may result in scarring or hyperpigmentation.[6]
There are many misconceptions and myths about acne.
Primary causes
Exactly why some people get acne and some do not is not fully known. It is known to be partly hereditary. Several factors are known to be linked to acne:
- Family/Genetic history. The tendency to develop acne runs in families. For example, school-age boys with acne have other members of their family with acne. A family history of acne is associated with an earlier occurrence of acne and an increased number of retentional acne lesions. [7]
- Hormonal activity, such as menstrual cycles and puberty. During puberty, an increase in male sex hormones called androgens cause the glands to get larger and make more sebum. [8]
- Stress, through increased output of hormones from the adrenal (stress) glands.
- Hyperactive sebaceous glands, secondary to the three hormone sources above.
- Accumulation of dead skin cells.
- Bacteria in the pores, to which the body becomes 'allergic'. Propionibacterium acnes (P. acnes) is the anaerobic bacterium that causes acne. In-vitro resistance of P. acnes to commonly used antibiotics has been increasing. [9]
- Skin irritation or scratching of any sort will activate inflammation.
- Use of anabolic steroids.
- Any medication containing halogens (iodides, chlorides, bromides), lithium, barbiturates, or androgens.
- Exposure to high levels of chlorine compounds, particularly chlorinated dioxins, can cause severe, long-lasting acne, known as Chloracne.
- Exposure to certain drugs and chemical compounds, including narcotics (opiates and opioids), especially when taken intravenously
Several hormones have been linked to acne: the androgens testosterone, dihydrotestosterone (DHT) and dehydroepiandrosterone sulfate (DHEAS), 17-hydroxyprogesterone, as well as insulin-like growth factor 1 (IGF-I). In addition, acne-prone skin has been shown to be insulin resistant.
Development of acne vulgaris in later years is uncommon, although this is the age group for Rosacea which may have similar appearances. True acne vulgaris in adults may be a feature of an underlying condition such as pregnancy and disorders such as polycystic ovary syndrome or the rare Cushing's syndrome. Menopause-associated acne occurs as production of the natural anti-acne ovarian hormone estradiol fails at menopause. The lack of estradiol also causes thinning hair, hot flashes, thin skin, wrinkles, vaginal dryness, and predisposes to osteopenia and osteoporosis as well as triggering acne (known as acne climacterica in this situation).
Diet
Milk
A recent study, based on a survey of 47,335 women, did find a positive epidemiological association between acne and consumption of partially skimmed milk, instant breakfast drink, sherbet, cottage cheese and cream cheese.[10] The researchers hypothesize that the association may be caused by hormones (such as several sex hormones and bovine IGF-I) present in cow milk. Though there is evidence of an association between milk and acne, the exact cause is unclear. Most dermatologists are awaiting confirmatory research linking diet and acne but some support the idea that acne sufferers should experiment with their diets, and refrain from consuming such fare if they find such food affects the severity of their acne.[11]
Seafood
Seafood often contains relatively high levels of iodine. Iodine is known to make existing acne worse but there is probably not enough to cause an acne outbreak.[12] Still, people who are prone to acne may want to avoid excessive consumption of foods high in iodine.
High carbohydrates/High GI
It has also been suggested that there is a link between a diet high in refined sugars and other processed foods and acne. The theory is that rapidly digested carbohydrate food such as white bread and refined sugars produces an overload in metabolic glucose that is rapidly converted into the types of fat that can build up in sebaceous glands. According to this hypothesis, the startling absence of acne in non-westernized societies could be explained by the low glycemic index of these cultures' diets. Others have cited possible genetic reasons for there being no acne in these populations, but similar populations shifting to these diets do develop acne. Note also that the populations studied consumed no milk or other dairy products.[13] Further research is necessary to establish whether a reduced consumption of high-glycemic foods (such as soft drinks, sweets, white bread) can significantly alleviate acne, though consumption of high-glycemic foods should in any case be kept to a minimum, for general health reasons.[14] Avoidance of 'junk food' with its high fat and sugar content is also recommended.[15] On the other hand there is no evidence that fat alone makes skin oilier or acne worse.
The University of Pennsylvania and the US Naval Academy conducted experiments that fed subjects chocolate or a bar with similar amounts of macronutrients (fat, sugar etc.) and found that consumption of chocolate, frequent or not, had no effect on the developing of acne. [16]
A 2005 systematic review found "surprisingly little evidence exists for the efficacy or lack of efficacy of dietary factors, face-washing and sunlight exposure in the management of acne."[17] A study in November 2006 in Australia gave a 50% reduction in 12 weeks in mild-moderate facial acne by introducing its subjects to a high protein, low GI diet. [18]
The American Medical Association says chocolate does not contribute to acne. [19]
A recent study[20] shows that a diet high enough in sugars triggers the liver to convert these sugars into lipid; as a side-effect this stops production of Sex hormone binding globulin- a chemical which reduces the level of testosterone in the blood. Since high testosterone levels generally trigger acne, the researchers believe that this can be a cause.
Vitamins A and E
Studies have shown that newly diagnosed acne patients tend to have lower levels of vitamin A circulating in their bloodstream than those that are acne free.[21] In addition people with severe acne also tend to have lower blood levels of vitamin E.[22]
Hygiene
Acne is not caused by dirt. This misconception probably comes from the fact that blackheads look like dirt stuck in the openings of pores. The black color is simply not dirt but compact keratin. In fact, the blockages of keratin that cause acne occur deep within the narrow follicle channel, where it is impossible to wash them away. These plugs are formed by the failure of the cells lining the duct to separate and flow to the surface in the sebum created there by the body.
Sex
Common myths state that masturbation causes acne and, conversely, that celibacy or sexual intercourse can cure it. Acne has not been linked to any type of sexual activity.
Complete Differential Diagnosis
- Acne conglobata
- Acne fulminans
- Acne vulgaris
- Gram-negative folliculitis
- Hidradenitis suppurativa
- Malassezia folliculitis
- Miliaria ("heat rash")
- Pyoderma faciale
- Rosacea
History and Symptoms

The most common form of acne is known as "acne vulgaris", meaning "common acne." Many teenagers get this type of acne.
The face and upper neck are the most commonly affected, but the chest, back and shoulders may have acne as well. The upper arms can also have acne, but lesions found there are often keratosis pilaris, not acne. The typical acne lesions are comedones and inflammatory papules, pustules, and nodules. Some of the large nodules were previously called "cysts" and the term nodulocystic has been used to describe severe cases of inflammatory acne. True cysts are rarely found in acne, and the term should be abandoned and the term severe nodular acne used instead.[23]
Aside from scarring, its main effects are psychological, such as reduced self-esteem[24] and, according to at least one study, depression or suicide.[25] Acne usually appears during adolescence, when people already tend to be most socially insecure. Early and aggressive treatment is therefore advocated to lessen the overall impact to individuals.[24]
Physical Examination
Skin

Treatments
Treatment ranges from knowledge of proper skin-care procedure to use of treatment products and diet control.
Acne skincare
Proper clinical skincare of acne involves gentle hygiene and minimal and restrained interaction with pimples so that the skin (epidermis and dermis) is never bruised due to coarse crushing, which worsens infection and may lead to scarring. Clinical lancing with a sterilised needle evacuates matured pustules so that when they are pressed the fluids end up outside the dermis rather than further underneath. Without restrained use of clinical lancing, it is harder for someone with serious acne to avoid causing damage to the dermis, increased infection due to ruptured skin cells, and scarring.
Available treatment products
There are many products sold for the treatment of acne, many of them without any scientifically-proven effects. Generally speaking successful treatments give little improvement within the first week or two; and then the acne decreases over approximately 3 months, after which the improvement starts to flatten out. Many treatments that promise big improvements within 2 weeks are likely to be largely disappointing. However short bursts of cortisone can give very quick results, and other treatments can rapidly improve some active spots, but not usually all active spots.
Modes of improvement are not necessarily fully understood but in general treatments are believed to work in at least 4 different ways (with many of the best treatments providing multiple simultaneous effects):
- normalising shedding into the pore to prevent blockage
- killing P. acnes
- antinflammatory effects
- hormonal manipulation
A combination of treatments can greatly reduce the amount and severity of acne in many cases. Those treatments that are most effective tend to have greater potential for side effects and need a greater degree of monitoring, so a step-wise approach is often taken. Many people consult with doctors when deciding which treatments to use, especially when considering using any treatments in combination. There are a number of treatments that have been proven effective:
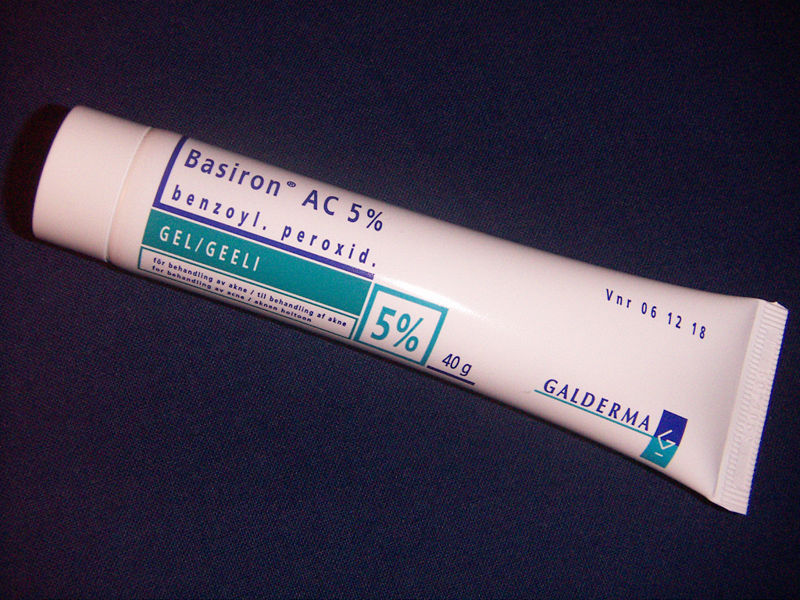
Topical bactericidals
Widely available OTC bactericidal products containing benzoyl peroxide may be used in mild to moderate acne. The gel or cream containing benzoyl peroxide is rubbed, twice daily, into the pores over the affected region. Bar soaps or washes may also be used and vary from 2 to 10% in strength. In addition to its therapeutic effect as a keratolytic (a chemical that dissolves the keratin plugging the pores) benzoyl peroxide also prevents new lesions by killing P.acnes. In one study, roughly 70% of participants using a 10% benzoyl peroxide solution experienced a reduction in acne lesions after 6 weeks.[27]Unlike antibiotics, benzoyl peroxide has the advantage of being a strong oxidizer (essentially a mild bleach) and thus does not appear to generate bacterial resistance. However, it routinely causes dryness, local irritation and redness. A sensible regimen may include the daily use of low-concentration (2.5%) benzoyl peroxide preparations, combined with suitable non-comedogenic moisturisers to help avoid overdrying the skin.[28]
Care must be taken when using benzoyl peroxide, as it can very easily bleach any fabric or hair it comes in contact with.
Other antibacterials that have been used include triclosan, or chlorhexidine gluconate but these are often less effective.
Prescription-strength benzoyl peroxide preparations do not necessarily differ with regard to the maximum concentration of the active ingredient (10%), but the drug is made available dissolved in a vehicle that more deeply penetrates the pores of the skin.
Topical antibiotics
Externally applied antibiotics such as erythromycin, clindamycin, Stiemycin or tetracycline aim to kill the bacteria that are harbored in the blocked follicles. Whilst topical use of antibiotics is equally as effective as oral, this method avoids possible side effects of stomach upset or drug interactions (e.g. it will not affect the oral contraceptive pill), but may prove awkward to apply over larger areas than just the face alone.
Oral antibiotics
Oral antibiotics used to treat acne include erythromycin or one of the tetracycline antibiotics (tetracycline, the better absorbed oxytetracycline, or one of the once daily doxycycline, minocycline or lymecycline). Trimethoprim is also sometimes used (off-label use in UK). However, reducing the P. acnes bacteria will not, in itself, do anything to reduce the oil secretion and abnormal cell behaviour that is the initial cause of the blocked follicles. Additionally the antibiotics are becoming less and less useful as resistant P. acnes are becoming more common. Acne will generally reappear quite soon after the end of treatment—days later in the case of topical applications, and weeks later in the case of oral antibiotics.
It has been found that sub-antimicrobial doses of antibiotics such as minocycline also improve acne. It is believed that minocycline's anti-inflammatory effect also prevents acne. These low doses do not kill bacteria and hence cannot induce resistance. Oral antibiotics such as Doxycycline have better results on the treatment of acne.[29] and generally will work better if started with at a higher dose.
Hormonal treatments
In females, acne can be improved with hormonal treatments. The common combined oestrogen/progestogen methods of hormonal contraception have some effect, but the anti-testosterone, Cyproterone, in combination with an oestrogen (Diane 35) is particularly effective at reducing androgenic hormone levels. Diane-35 is not available in the USA, but a newer oral contraceptive containing the progestin drospirenone is now available with fewer side effects than Diane 35 / Dianette. Both can be used where blood tests show abnormally high levels of androgens, but are effective even when this is not the case. Along with this, treatment with low dose spironolactone can have anti-androgenetic properties, especially in patients with polycystic ovarian syndrome.
If a pimple is large and/or does not seem to be affected by other treatments, a dermatologist may administer an injection of cortisone directly into it, which will usually reduce redness and inflammation almost immediately. This has the effect of flattening the pimple, thereby making it easier to cover up with makeup, and can also aid in the healing process. Side effects are minimal, but may include a temporary whitening of the skin around the injection point. This method also carries a much smaller risk of scarring than surgical removal.
Topical retinoids
A group of medications for normalizing the follicle cell lifecycle are topical retinoids such as tretinoin (brand name Retin-A), adapalene (brand name Differin) and tazarotene (brand name Tazorac). Like isotretinoin, they are related to vitamin A, but they are administered as topicals and generally have much milder side effects. They can, however, cause significant irritation of the skin. The retinoids appear to influence the cell creation and death lifecycle of cells in the follicle lining. This helps prevent the hyperkeratinization of these cells that can create a blockage. Retinol, a form of vitamin A, has similar but milder effects and is used in many over-the-counter moisturizers and other topical products. Effective topical retinoids have been in use over 30 years but are available only on prescription so are not as widely used as the other topical treatments. Topical retinoids often cause an initial flare up of acne and facial flushing (physiology).
Oral retinoids
A daily oral intake of vitamin A derivatives like isotretinoin (marketed as Accutane, Sotret, Claravis) over a period of 4-6 months can cause long-term resolution or reduction of acne by reducing the secretion of oils from the glands. It is believed that isotretinoin works primarily by reducing the secretion of oils from the glands, however some studies suggest that it affects other acne-related factors as well. Isotretinoin has been shown to be very effective in treating severe acne and can either improve or clear well over 80% of patients. The drug has a much longer effect than anti-bacterial treatments and will often cure acne for good. The treatment requires close medical supervision by a dermatologist because the drug has many known side effects (many of which can be severe). About 25% of patients may relapse after one treatment. In those cases, a second treatment for another 4-6 months may be indicated to obtain desired results. It is often recommended that one lets a few months pass between the two treatments, because the condition can actually improve somewhat in the time after stopping the treatment and waiting a few months also gives the body a chance to recover. Occasionally a third or even a fourth course is used, but the benefits are often less substantial. The most common side effects are dry skin and occasional nosebleeds (secondary to dry nasal mucosa). Oral retinoids also often cause an initial flare up of acne within a month or so, which can be severe. There are reports that the drug has damaged the liver of patients. For this reason, it is recommended that patients have blood samples taken and examined before and during treatment. In some cases, treatment is terminated due to elevated liver enzymes in the blood, which might be related to liver damage. Others claim that the reports of permanent damage to the liver are unsubstantiated, and routine testing is considered unnecessary by some dermatologists. Blood triglycerides also need to be monitored. However, routine testing are part of the official guidelines for the use of the drug in many countries. Some press reports suggest that isotretinoin may cause depression but as of September 2005 there is no agreement in the medical literature as to the risk. The drug also causes birth defects if women become pregnant while taking it or take it while pregnant. For this reason, female patients are required to use two separate forms of birth control or vow abstinence while on the drug. Because of this, the drug is supposed to be given to females as a last resort after milder treatments have proven insufficient. Restrictive rules (see iPledge Program) for use were put into force in the USA beginning in March 2006 to prevent misuse.[30] This has occasioned widespread editorial comment.[31]
Phototherapy
'Blue' and red light
It has long been known that short term improvement can be achieved with sunlight. However, studies have shown that sunlight worsens acne long-term. More recently, visible light has been successfully employed to treat acne (Phototherapy) - in particular intense violet light (405-420nm) generated by purpose-built fluorescent lighting, dichroic bulbs, LEDs or lasers. Used twice weekly, this has been shown to reduce the number of acne lesions by about 64%;[32] and is even more effective when applied daily. The mechanism appears to be that a porphyrin (Coproporphyrin III) produced within P. acnes generates free radicals when irradiated by 420nm and shorter wavelengths of light.[33] Particularly when applied over several days, these free radicals ultimately kill the bacteria.[34] Since porphyrins are not otherwise present in skin, and no UV light is employed, it appears to be safe, and has been licensed by the U.S. FDA.[35] The treatment apparently works even better if used with red visible light (660 nanometer) resulting in a 76% reduction of lesions after 3 months of daily treatment for 80% of the patients;[36] and overall clearance was similar or better than benzoyl peroxide. Unlike most of the other treatments few if any negative side effects are typically experienced, and the development of bacterial resistance to the treatment seems very unlikely. After treatment, clearance can be longer lived than is typical with topical or oral antibiotic treatments; several months is not uncommon. The equipment or treatment, however, is relatively new and reasonably expensive to buy initially, although the total cost of ownership can be similar to many other treatment methods (such as the total cost of benzoyl peroxide, moisturiser, washes) over a couple of years of use.
Photodynamic therapy
In addition, basic science and clinical work by dermatologists Yoram Harth and Alan Shalita and others has produced evidence that intense blue/violet light (405-425 nanometer) can decrease the number of inflammatory acne lesion by 60-70% in 4 weeks of therapy, particularly when the P.acnes is pretreated with delta-aminolevulinic acid (ALA), which increases the production of porphyrins. However this photodynamic therapy is controversial and apparently not published in a peer reviewed journal.
Laser treatment
Laser surgery has been in use for some time to reduce the scars left behind by acne, but research has been done on lasers for prevention of acne formation itself. The laser is used to produce one of the following effects:
- to burn away the follicle sac from which the hair grows
- to burn away the sebaceous gland which produces the oil
- to induce formation of oxygen in the bacteria, killing them
Since lasers and intense pulsed light sources cause thermal damage to the skin there are concerns that laser or intense pulsed light treatments for acne will induce hyperpigmented macules (spots) or cause long term dryness of the skin.
The FDA has approved several companies, such as Candela Corp. to use a cosmetic laser for the treatment of acne.[37] However, efficacy studies have used very small sample sizes (fewer than 100 subjects) for periods of six months or less, and have shown contradictory results.[38][39] Also, laser treatment being relatively new, protocols remain subject to experimentation and revision,[40] and treatment can be quite expensive. Also, some Smoothbeam laser devices had to be recalled due to coolant failure, which resulted in painful burn injuries to patients.[41]
Less widely used treatments
- Azelaic acid (brand names Azelex, Finevin, Skinoren) is suitable for mild, comedonal acne.[42]
- Zinc: Orally administered zinc gluconate has been shown to be effective in the treatment of inflammatory acne, although less so than tetracyclines.[43][44]
- Tea Tree Oil (Melaleuca Oil) has been used with some success, comparable to benzoyl peroxide but without excessive drying, and has been shown to be an effective anti-inflammatory in skin infections. [45][46][47]
- Nicotinamide, (Vitamin B3) used topically in the form of a gel, has been shown in a 1995 study to be more effective than a topical antibiotic used for comparison, as well as having fewer side effects.[48] Topical nicotinamide is available both on prescription and over-the-counter. The property of topical nicotinamide's benefit in treating acne seems to be its anti-inflammatory nature. It is also purported to result in increased synthesis of collagen, keratin, involucrin and flaggrin.
- There are also certain treatments for acne mentioned in Ayurveda using herbs such as Aloe vera,[49] Aruna, Haldi (Turmeric),and Papaya.[50] There is limited evidence from conventional medical studies on these products.[45] Products from Rubia cordifolia, Curcuma longa (commonly known as Turmeric), Hemidesmus indicus (known as ananthamoola or anantmula), and Azadirachta indica (Neem) have been shown to have anti-inflammatory effects, but not aloe vera.[51]
- Rofecoxib was shown to improve premenstrual acne vulgaris in a placebo controlled study.[52]
- Naproxen or ibuprofen are used for some moderate acne for their anti-inflammatory effect.[53]
History of some acne treatments
The history of acne reaches back to the dawn of recorded history. In Ancient Egypt, it is recorded that several pharaohs were acne sufferers. From Ancient Greece comes the English word 'acne' (meaning 'point' or 'peak'). Acne treatments are also of considerable antiquity:
- Ancient Rome: bathing in hot, and often sulfurous, mineral water was one of the few available acne treatments. One of the earliest texts to mention skin problems is De Medicina by the Roman writer Celsus.
- 1800s: Nineteenth century dermatologists used sulphur in the treatment of acne. It was believed to dry the skin.
- 1920s: Benzoyl Peroxide is used
- 1930s: Laxatives were used as a cure for what were known as 'chastity pimples'. Radiation also was used.
- 1950s: When antibiotics became available, it was discovered that they had beneficial effects on acne. They were taken orally to begin with. Much of the benefit was not from killing bacteria but from the anti-inflammatory effects of tetracycline and its relatives. Topical antibiotics became available later.
- 1970s: Tretinoin (original Trade Name Retin A) was found effective for acne.[54] This preceded the development of oral isotretinoin (sold as Accutane and Roaccutane) in 1980.[55]
- 1980s: Accutane is introduced in America
- 1990s: Laser treatment introduced
- 2000s: Blue/red light therapy
Future treatments
A 2007 microbiology article reporting the first genome sequencing of a Propionibacterium acnes bacteriophage (PA6) said this "should greatly enhance the development of a potential bacteriophage therapy to treat acne and therefore overcome the significant problems associated with long-term antibiotic therapy and bacterial resistance."[56]
Preferred treatments by types of acne vulgaris
- Comedonal (non-inflammatory) acne: local treatment with azelaic acid, salicylic acid, topical retinoids, benzoyl peroxide.
- Mild papulo-pustular (inflammatory) acne: benzoyl peroxide or topical retinoids, topical antibiotics (such as erythromycin).
- Moderate inflammatory acne: benzoyl peroxide or topical retinoids combined with oral antibiotics (tetracyclines). Isotretinoin is an option.
- Severe inflammatory acne, nodular acne, acne resistant to the above treatments: isotretinoin, or contraceptive pills with cyproterone for females with virilization or drospirenone.
Acne scars
See Acne scarring.
Severe acne often leaves small scars where the skin gets a "volcanic" shape. Acne scars are difficult and expensive to treat, and it is unusual for the scars to be successfully removed completely.
Physical acne scars are often referred to as "Icepick" scars. This is because the scars tend to cause an indentation in the skin's surface. There are a range of treatments available.
Although quite rare, the medical condition Atrophia Maculosa Varioliformis Cutis results in "acne like" depressed scars on the face.
Ice pick scars - Deep pits, that are the most common and a classic sign of acne scarring.
Box car scars - Angular scars that usually occur on the temple and cheeks, and can be either superficial or deep, these are similar to chickenpox scars.
Rolling scars - Scars that give the skin a wave-like appearance.
Hypertrophic scars - Thickened, or keloid scars.
[57]
Pigmentation
Pigmented scars is a slightly misleading term, suggesting a change in the skin's pigmentation, and that they are true scars. Neither is true. Pigmented scars are usually the result of nodular or cystic acne (the painful 'bumps' lying under the skin). They often leave behind an inflamed red mark. Often, the pigmentation scars can be avoided simply by avoiding aggravation of the nodule or cyst. When sufferers try to 'pop' cysts or nodules, pigmentation scarring becomes significantly worse, and may even bruise the affected area. Pigmentation scars nearly always fade with time taking between 3 months to two years to do so, although rarely can persist.
On the other hand, some people, particularly people with naturally tanned skin do develop brown hyperpigmentation scars which is caused by a local increased production of the pigment melanin. These too typically fade over time.
Grading scale
There are multiple grading scales for grading the severity of acne vulgaris,[58] three of these being: Leeds acne grading technique: Counts and categorises lesions into inflammatory and non-inflammatory (ranges from 0-10.0). 'Cook's acne grading scale: Uses photographs to grade severity from 0 to 8 (0 being the least severe and 8 being the most severe). Pillsbury scale: Simply classifies the severity of the acne from 1 (least severe) to 4 (most severe).
See also
References
- ↑ http://www.emedicine.com/DERM/topic2.htm
- ↑ James WD (2005). "Clinical practice. Acne". N Engl J Med. 352 (14): 1463–72. PMID 15814882.
- ↑ Anderson, Laurence. 2006. Looking Good, the Australian guide to skin care, cosmetic medicine and cosmetic surgery. AMPCo. Sydney. ISBN 0 85557 044 X.
- ↑ Cure forAcne
- ↑ Cure forAcne
- ↑ Simpson, Nicholas B.; Cunliffe, William J. (2004). "Disorders of the sebaceous glands". In Burns, Tony; Breathnach, Stephen; Cox, Neil; Griffiths, Christopher. Rook's textbook of dermatology (7th ed. ed.). Malden, Mass.: Blackwell Science. pp. pp. 43.1-75. ISBN 0-632-06429-3.
- ↑ F. Ballangera, P. Baudrya, J.M. N'Guyenb, A. Khammaria, B. Dréno Heredity: A Prognostic Factor for Acne 5/2/2005
- ↑ US Dept Health and Human Services January 2005
- ↑ National Guideline Clearinghouse 11/12/2007
- ↑ Adebamowo CA, Spiegelman D, Danby FW, Frazier AL, Willett WC, Holmes MD (2005). "High school dietary dairy intake and teenage acne". J Am Acad Dermatol. 52 (2): 207–14. PMID 15692464.
- ↑ Fries JH (1978). "Chocolate: a review of published reports of allergic and other deleterious effects, real or presumed". Ann Allergy. 41 (4): 195–207. PMID 152075.
- ↑ Danby FW (2007). "Acne and iodine: Reply". J Am Acad Dermatol. 56 (1): 164–5. PMID 17190637.
- ↑ Loren Cordain, et al. "Acne Vulgaris - A Disease of Western Civilization" Arch Dermatol. 2002;138:1584-1590. Observation
- ↑ Smith R, Mann N, Makelainen H, Braue A, Varigos G (2004). "The effect of short-term altered macronutrient status on acne vulgaris and biochemical markers of insulin sensitivity". Asia Pac J Clin Nutr. 13 (Suppl): S67. PMID 15294556.
- ↑ Anderson, Laurence. 2006. Looking Good, the Australian guide to skin care, cosmetic medicine and cosmetic surgery. AMPCo. Sydney. ISBN 0-85557-044-X.
- ↑ "Sweet news about chocolate". usaweekend.com. 1998-06-05. Retrieved 2007-05-27.
- ↑ Magin P, Pond D, Smith W, Watson A (2005). "A systematic review of the evidence for 'myths and misconceptions' in acne management: diet, face-washing and sunlight". Fam Pract. 22 (1): 62–70. PMID 15644386.
- ↑ RMIT acne study
- ↑ JAMA Patient Page - Acne
- ↑ [1]
- ↑ Naweko San-Joyz (April 11, 2007). "How Does Vitamin A Prevent Acne Outbreaks?". American Chronical. Retrieved 2007-09-17.
- ↑ El-Akawi Z, Abdel-Latif N, Abdul-Razzak K (2006). "Does the plasma level of vitamins A and E affect acne condition?". Clin. Exp. Dermatol. 31 (3): 430–4. doi:10.1111/j.1365-2230.2006.02106.x. PMID 16681594.
- ↑ Thiboutot, Diane M.; Strauss, John S. (2003). "Diseases of the sebaceous glands". In Burns, Tony; Breathnach, Stephen; Cox, Neil; Griffiths, Christopher. Fitzpatrick's dermatology in general medicine (6th ed. ed.). New York: McGraw-Hill. pp. pp. 672-87. ISBN 0-07-138076-0.
- ↑ 24.0 24.1 Goodman G (2006). "Acne and acne scarring - the case for active and early intervention" (PDF). Aust Fam Physician. 35 (7): 503–4. PMID 16820822.
- ↑ Purvis D, Robinson E, Merry S, Watson P (2006). "Acne, anxiety, depression and suicide in teenagers: a cross-sectional survey of New Zealand secondary school students". J Paediatr Child Health. 42 (12): 793–6. PMID 17096715.
One study has estimated the incidence of suicidal ideation in patients with acne as 7.1% :
* Picardi A, Mazzotti E, Pasquini P (2006). "Prevalence and correlates of suicidal ideation among patients with skin disease". J Am Acad Dermatol. 54 (3): 420–6. PMID 16488292. - ↑ http://picasaweb.google.com/mcmumbi/USMLEIIImages/photo#5089143049752456450
- ↑ Comparative evaluation of retinoic acid, benzoyl peroxide and erythromycin lotion in acne vulgarils
- ↑ Kern, Daniel W. "Clear skin regimen: A free, step by step program." Acne.org. Instructions
- ↑ Thiboutot, D, (2000). "Prescription Medications for Treating Acne". Acne Net. 9 (7–8): 179–187. PMID 15636181.
- ↑ "The iPLEDGE Program - Guide to Best Practices for Isotretinoin - "The resource to help the prescriber prepare, plan treatments, and prevent pregnancies during the course of isotretinoin therapy"" (PDF). 2005.
- ↑ Bernadine Healy (2005-05-09). "Pledging for Accutane". US News Best Health. Check date values in:
|date=(help) - ↑ Kawada A, Aragane Y, Kameyama H, Sangen Y, Tezuka T (2002). "Acne phototherapy with a high-intensity, enhanced, narrow-band, blue light source: an open study and in vitro investigation". J Dermatol Sci. 30 (2): 129–35. PMID 12413768.
- ↑ Kjeldstad B (1984). "Photoinactivation of Propionibacterium acnes by near-ultraviolet light". Z Naturforsch [C]. 39 (3–4): 300–2. PMID 6730638.
- ↑ Ashkenazi H, Malik Z, Harth Y, Nitzan Y (2003). "Eradication of Propionibacterium acnes by its endogenic porphyrins after illumination with high intensity blue light". FEMS Immunol Med Microbiol. 35 (1): 17–24. PMID 12589953.
- ↑ "New Light Therapy for Acne" U.S. Food and Drug Administration, FDA Consumer magazine, November-December 2002 Notice
- ↑ Papageorgiou P, Katsambas A, Chu A (2000). "Phototherapy with blue (415 nm) and red (660 nm) light in the treatment of acne vulgaris" (PDF). Br J Dermatol. 142 (5): 973–8. PMID 10809858.
- ↑ http://www.reflectionscenter.com/sb_acne_press_trade.pdf
- ↑ http://news.bbc.co.uk/2/hi/health/3808055.stm
- ↑ http://www.cosmeticsurgery-news.com/article1053.html
- ↑ http://www.dermatologytimes.com/dermatologytimes/article/articleDetail.jsp?id=93752
- ↑ http://www.fda.gov/bbs/topics/enforce/2004/ENF00830.html
- ↑ MedlinePlus (2001-07-24). "Azelaic Acid (Topical)".
- ↑ Dreno B, Amblard P, Agache P, Sirot S, Litoux P (1989). "Low doses of zinc gluconate for inflammatory acne". Acta Derm Venereol. 69 (6): 541–3. PMID 2575335.
- ↑ Dreno B, Moyse D, Alirezai M, Amblard P, Auffret N, Beylot C, Bodokh I, Chivot M, Daniel F, Humbert P, Meynadier J, Poli F (2001). "Multicenter randomized comparative double-blind controlled clinical trial of the safety and efficacy of zinc gluconate versus minocycline hydrochloride in the treatment of inflammatory acne vulgaris". Dermatology. 203 (2): 135–40. PMID 11586012.
- ↑ 45.0 45.1 Mantle D, Gok MA, Lennard TW (2001). "Adverse and beneficial effects of plant extracts on skin and skin disorders". Adverse drug reactions and toxicological reviews. 20 (2): 89–103. PMID 11482001.
- ↑ Koh KJ, Pearce AL, Marshman G, Finlay-Jones JJ, Hart PH (2002). "Tea tree oil reduces histamine-induced skin inflammation". Br. J. Dermatol. 147 (6): 1212–7. PMID 12452873.
- ↑ Khalil Z, Pearce AL, Satkunanathan N, Storer E, Finlay-Jones JJ, Hart PH (2004). "Regulation of wheal and flare by tea tree oil: complementary human and rodent studies". J. Invest. Dermatol. 123 (4): 683–90. doi:10.1111/j.0022-202X.2004.23407.x. PMID 15373773.
- ↑ Shalita A, Smith J, Parish L, Sofman M, Chalker D (1995). "Topical nicotinamide compared with clindamycin gel in the treatment of inflammatory acne vulgaris". Int J Dermatol. 34 (6): 434–7. PMID 7657446.
- ↑ "Greenleaf Aloe Vera Gel". Brihans.
- ↑ Ayurveda Encyclopedia, "Acne Treatment"
- ↑ Jain A, Basal E (2003). "Inhibition of Propionibacterium acnes-induced mediators of inflammation by Indian herbs". Phytomedicine. 10 (1): 34–8. PMID 12622461.
- ↑ Tehrani R, Dharmalingam M (2004). "Management of premenstrual acne with Cox-2 inhibitors: A placebo controlled study". Indian J Dermatol Venereol Leprol [serial online]. 70: 345–348. Retrieved 2007-06-23.
- ↑ Dermnet NZ-Acne management
- ↑ "Tretinoin (retinoic acid) in acne". The Medical letter on drugs and therapeutics. 15 (1): 3. 1973. PMID 4265099.
- ↑ Jones H, Blanc D, Cunliffe WJ (1980). "13-cis retinoic acid and acne". Lancet. 2 (8203): 1048–9. PMID 6107678.
- ↑ Farrar MD, Howson KM, Bojar RA, West D, Towler JC, Parry J, Pelton K, Holland KT (2007). "Genome sequence and analysis of a Propionibacterium acnes bacteriophage" (PDF). J Bacteriol. 189 (11): 4161–7. PMID 17400737.
- ↑ Types of Acne Scars
- ↑ Leeds, Cook's and Pillsbury scales obtained from here
Further reading
- Review articles and guidelines:
- Webster GF (2002). "Acne vulgaris" (PDF). BMJ. 325 (7362): 475–9. PMID 12202330.
- Gollnick H, Cunliffe W, Berson D, Dreno B, Finlay A, Leyden JJ, Shalita AR, Thiboutot D; Global Alliance to Improve Outcomes in Acne (2003). "Management of acne: a report from a Global Alliance to Improve Outcomes in Acne". J Am Acad Dermatol. 49 (1 Suppl): S1–37. PMID 12833004.
- Feldman S, Careccia RE, Barham KL, Hancox J (2004). "Diagnosis and treatment of acne" (PDF). Am Fam Physician. 69 (9): 2123–30. PMID 15152959.
- Haider A, Shaw JC (2004). "Treatment of acne vulgaris" (PDF). JAMA. 292 (6): 726–35. PMID 15304471.
- Katsambas AD, Cunliffe WJ (eds.) (2004). "Acne and its treatment". Clin Dermatol. 22 (5): 359–447.
- James WD (2005). "Clinical practice. Acne". N Engl J Med. 352 (14): 1463–72. PMID 15814882.
- "Drugs for acne, rosacea and psoriasis". Treat Guidel Med Lett. 3 (35): 49–56. 2005. PMID 15961971.
- Sinclair W, Jordaan HF; Global Alliance to Improve Outcomes in Acne (2005). "Acne guideline 2005 update" (PDF). S Afr Med J. 95 (11 Pt 2): 881–92. PMID 16344888.
- Zaenglein AL, Thiboutot DM (2006). "Expert committee recommendations for acne management" (PDF). Pediatrics. 118 (3): 1188–99. PMID 16951015.
- Purdy S, de Berker D (2006). "Acne". BMJ. 333 (7575): 949–53. PMID 17082546.
- Strauss JS, Krowchuk DP, Leyden JJ, Lucky AW, Shalita AR, Siegfried EC, Thiboutot DM, Van Voorhees AS, Beutner KA, Sieck CK, Bhushan R; American Academy of Dermatology/American Academy of Dermatology Association (2007). "Guidelines of care for acne vulgaris management". J Am Acad Dermatol. 56 (4): 651–63. PMID 17276540.
- Reference books and chapters:
- Plewig, Gerd; Kligman, Albert M. (2000). Acne and rosacea (3rd ed. ed.). New York: Springer-Verlag. ISBN 3-540-66751-2.
- Cunliffe, William J.; Gollnick, Harald P. M. (2001). Acne : diagnosis and management. London: Martin Dunitz. ISBN 1-85317-206-5.
- Thiboutot, Diane M.; Strauss, John S. (2003). "Diseases of the sebaceous glands". In Burns, Tony; Breathnach, Stephen; Cox, Neil; Griffiths, Christopher. Fitzpatrick's dermatology in general medicine (6th ed. ed.). New York: McGraw-Hill. pp. pp. 672-87. ISBN 0-07-138076-0.
- Zaenglein, Andrea L.; Thiboutot, Diane M. (2003). "Acne vulgaris". In Bolognia, Jean L.; Jorizzo, Joseph L.; Rapini, Ronald P. (eds.). Dermatology. London: Mosby. pp. pp. 531-44. ISBN 0-32302-4092.
- Habif, Thomas P. (2004). "Acne, rosacea, and related disorders". Clinical dermatology : a color guide to diagnosis and therapy (4th ed. ed.). Edinburgh: Mosby. pp. pp. 162-208. ISBN 0-323-01319-8.
- Simpson, Nicholas B.; Cunliffe, William J. (2004). "Disorders of the sebaceous glands". In Burns, Tony; Breathnach, Stephen; Cox, Neil; Griffiths, Christopher. Rook's textbook of dermatology (7th ed. ed.). Malden, Mass.: Blackwell Science. pp. pp. 43.1-75. ISBN 0-632-06429-3.
- James, William D.; Berger, Timothy G.; Elston, Dirk M. (2006). "Acne". Andrews' diseases of the skin : clinical dermatology (10th ed. ed.). Philadelphia: Saunders Elsevier. pp. pp. 231-50. ISBN 0-7216-2921-0.
External links
- Acne vulgaris: more than skin deep (on the psychological effects of acne)
- Acne photo library at Dermnet
- Story on Acne from the Better Health Channel (Quality assured by the Victorian government, Australia)
- "AcneNet". American Academy of Dermatology. - Dermatologist-reviewed information about acne.
- "Acne Questions and Answers". From the National Institute of Health.
ar:حب الشباب bg:Акне cs:Akné da:Akne de:Akne el:Ακμή eo:Akno gl:Acne ko:여드름 id:Jerawat ia:Acne it:Acne he:אקנה ka:აკნე lt:Spuogas ms:Jerawat nl:Acne no:Akne qu:Muchhi simple:Acne sk:Akné sr:Акне fi:Akne sv:Akne th:สิว
