Ebola case studies
|
Ebola Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Postmortem Care |
|
Case Studies |
|
Ebola case studies On the Web |
|
American Roentgen Ray Society Images of Ebola case studies |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Recent outbreaks
As of August 30, 2007, 103 people (100 adults and three children) were infected by a suspected hemorrhagic fever outbreak in the village of Mweka, Democratic Republic of the Congo (DRC). The outbreak started after the funerals of two village chiefs, and 217 people in four villages fell ill. The World Health Organization sent a team to take blood samples for analysis and confirmed that many of the cases are the result of the Ebola virus [1]. The Congo's last major Ebola epidemic killed 245 people in 1995 in Kikwit, about 200 miles from the source of the Aug. 2007 outbreak.[2]
On November 30, 2007, the Uganda Ministry of Health confirmed an outbreak of Ebola in the Bundibugyo District. After confirmation of samples tested by the United States National Reference Laboratories and the Centers for Disease Control, the World Health Organization confirmed the presence of a new species of the Ebola virus.[3] The epidemic came to an official end on February 20, 2008. 149 cases of this new strain were reported and 37 of those led to deaths.
Uganda outbreak
On October 8, 2000, an outbreak of an unusual febrile illness with occasional hemorrhage and significant mortality was reported to the Ministry of Health (MoH) in Kampala by the superintendent of St. Mary's Hospital in Lacor, and the District Director of Health Services in the Gulu District. A preliminary assessment conducted by MoH found additional cases in Gulu District and in Gulu Hospital, the regional referral hospital. On October 15, suspicion of Ebola hemorrhagic fever (EHF) was confirmed when the National Institute of Virology (NIV), Johannesburg, South Africa, identified Ebola virus infection among specimens from patients, including health-care workers at St. Mary's Hospital. This report describes surveillance and control activities related to the EHF outbreak and presents preliminary clinical and epidemiologic findings.
Control activities were organized around surveillance and epidemiology, clinical case management, social education and mobilization, and coordination and logistic support. An active EHF surveillance system was initiated to determine the extent and magnitude of the outbreak, identify foci of disease activity, and detect cases early. Ill persons were encouraged to be assessed at a hospital and, if indicated, to be hospitalized to reduce further community transmission. Targeted prevention activities included follow-up of contacts of identified cases for 21 days; establishment of trained burial teams for all potential and confirmed EHF deaths; community education; cessation of traditional healing and burial practices; cessation of large public gatherings; and updates of hospital infection-control measures, including isolation wards. Laboratory testing was performed at a field laboratory established at St. Mary's Hospital by CDC and supplemented by additional testing at CDC and NIV. Sequence analysis revealed that the virus associated with this outbreak was Ebola-Sudan and differed at the nucleotide sequence level from earlier Ebola-Sudan isolates by 3.3% and 4.2% in the polymerase (362 nucleotides sequenced) and nucleocapsid (146 nucleotides sequenced) protein encoding genes, respectively.
During the third week of October, active surveillance was established and included three case notification categories: alert, suspect, and probable. The alert category comprised persons with sudden onset of high fever, sudden death, or hemorrhage, and was used by community members to alert health-care personnel. The suspect category comprised persons with fever and contact with a potential case-patient; persons with unexplained bleeding; persons with fever and three or more specified symptoms (i.e., headache, vomiting, anorexia, diarrhea, weakness or severe fatigue, abdominal pain, body aches or joint pains, difficulty swallowing, difficulty breathing, and hiccups), and all unexplained deaths. The suspect category was used by mobile surveillance teams to determine whether a patient required transport to an isolation ward. The probable category included persons who met these criteria and were assessed and reported by a physician. Laboratory tests included virus antigen detection and antibody ELISA tests and reverse transcriptase polymerase chain reaction. Laboratory-confirmed case-patients were defined as patients who met the surveillance case definitions and were either positive for Ebola virus antigen or Ebola IgG antibody.
During October 5--November 27, among 62 persons with laboratory-confirmed EHF admitted to Gulu Hospital, symptoms included diarrhea (66%), asthenia (64%), anorexia (61%), headache (63%), nausea and vomiting (60%), abdominal pain (55%), and chest pain (48%). Patients presented for care a mean of 8 days (range: 2--20 days) after symptom onset. Bleeding occurred in 12 (20%) patients and primarily involved the gastrointestinal tract. Among the 62 confirmed case-patients, 36 (58%) died; among patients aged <15 years, four of five died (case fatality: 80%). Spontaneous abortions were reported among pregnant women infected with EHF. Patients who died usually exhibited a rapid progression of shock, increasing coagulopathy, and loss of consciousness.
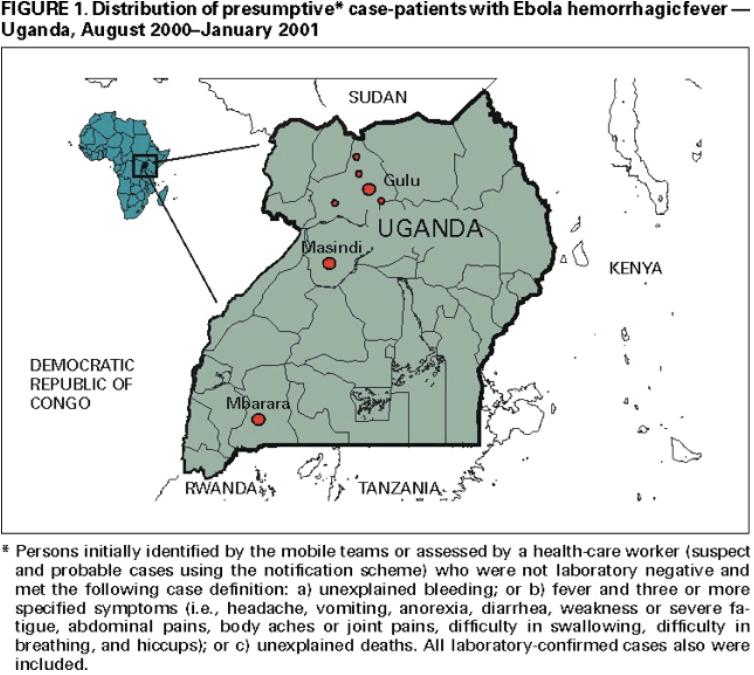
As of January 23, 2001, 425 presumptive* case-patients with 224 (53%) deaths attributed to EHF were recorded from three districts in Uganda: 393 (93%) from Gulu, 27 (6%) from Masindi, and five (1%) from Mbarara. The combined area comprises approximately 11,700 square miles (31,000 square kilometers; 2000 combined population: 1.8 million) (See the map of Uganda below) (1). Although the cluster of cases in early October triggered identification of the outbreak and response measures, investigations (i.e., case-record review and interviews with surviving patients or their surrogates) identified cases occurring in the community and patients hospitalized several weeks earlier. The onset of illness of the earliest presumptive case was August 30, 2000, and onset of last presumptive case was January 9, 2001 (See the graph below the map of Uganda). The ages of presumptive case-patients ranged from 3 days--72 years (median: 28 years); 269 (63%) were women. Mean time from symptom onset to death was 8 days (95% confidence interval=±5 days); 218 (51%) presumptive cases were laboratory confirmed.
Epidemiologic investigations identified the three most important means of transmission as attending funerals of presumptive EHF case-patients where ritual contact with the deceased occurred, and intrafamilial or nosocomial transmission. Fourteen (64%) of 22 health-care workers in Gulu were infected after establishing the isolation wards; these incidences led to the reinforcement of infection-control measures. Two distant focal outbreaks were initiated by movement of infected contacts of EHF cases from Gulu to Mbarara and Masindi districts. National notification and surveillance efforts led to the rapid identification of these foci and effective containment.
References
- ↑ "Ebola Outbreak Confirmed in Congo". NewScientist.com. 2007-09-11. Retrieved 2008-02-25.
- ↑ "Mystery DR Congo fever kills 100". BBC News. 2007-08-31. Retrieved 2008-02-25.
- ↑ "Uganda: Deadly Ebola Outbreak Confirmed - UN". UN News Service. 2007-11-30. Retrieved 2008-02-25.