Hepatitis B pathophysiology
|
Hepatitis B |
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Hepatitis B pathophysiology On the Web |
|
American Roentgen Ray Society Images of Hepatitis B pathophysiology |
|
Risk calculators and risk factors for Hepatitis B pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor In Chief: Cafer Zorkun, M.D., Ph.D. [2]
Pathophysiology
Hepatitis B is a serious disease caused by a virus that attacks the liver. The virus, which is called hepatitis B virus (HBV), can cause lifelong infection, cirrhosis (scarring) of the liver, liver cancer, liver failure, and death.
HBV is a 42-nm DNA virus classified in the Hepadnaviridae family. The liver is the primary site of HBV replication. After a susceptible person is exposed, the virus enters the liver via the bloodstream; no evidence exists indicating that the virus replicates at mucosal surfaces. HBV infection can produce either asymptomatic or symptomatic infection. The average incubation period is 90 days (range: 60--150 days) from exposure to onset of jaundice and 60 days (range: 40--90 days) from exposure to onset of abnormal serum alanine aminotransferase (ALT) levels.
Structure
Virions consist of an outer lipid envelope and an icosahedral nucleocapsid core composed of protein. The nucleocapsid encloses the viral DNA and a DNA polymerase that has reverse transcriptase activity. The outer envelope contains embedded proteins which are involved in viral binding of, and release into, susceptible cells. Virion shape is generally spherical with a diameter of 40 - 48 nanometers (nm), but pleomorphic forms exist, including filamentous and spherical bodies lacking a core. These "subviral" particles are not infectious.
The DNA genome is not segmented but rather partially double-stranded, containing a long and short segment which overlap approximately 240 nucleotides to form an open circle. The longer strand is 3020-3320 nucleotides long, and the shorter is 1700-2800 nucleotides long.[1] The virus can be divided into four major serotypes (adr, adw, ayr, ayw) based on antigenic epitopes present on its envelope proteins, and into eight genotypes (A-H) according to overall nucleotide sequence variation of the genome. Different genotypes have distinct geographic distributions. For example, genotypes B and C are prevalent in China and neighboring countries.
Replication
Hepatitis B is one of a few known non-retroviral viruses which employ reverse transcription as a part of its replication process. (HIV, a completely unrelated virus, also uses reverse transcription, but it is a retrovirus.) HBV invades hepatocytes by binding to surface receptors and becoming internalized. The viral core particles then migrate to the nucleus and the partially double-stranded, relaxed circular genomes (RC-DNA) are repaired to form a covalently closed circular DNA (cccDNA), which is the template for transcription of viral genomic and sub-genomic RNAs by cellular RNA polymerase II. Of these, the pregenomic RNA (pgRNA) is selectively packaged into progeny capsids and is then reverse-transcribed into new RC-DNA. The core can either bud into the endoplasmic reticulum to be enveloped and exported from the cell or recycled back into the nucleus for conversion to cccDNA.
Transmission
Transmission results from exposure to infectious blood or body fluids containing blood. Possible forms of transmission include (but are not limited to) unprotected sexual contact, blood transfusions, re-use of contaminated needles and syringes, and vertical transmission from mother to child during childbirth. Without intervention, a mother who is positive for the hepatitis B surface antigen confers a 20% risk of passing the infection to her offspring at the time of birth. This risk is as high as 90% if the mother is also positive for the hepatitis B e antigen. HBV can also be transmitted between family members within households, possibly by contact of nonintact skin or mucous membrane with secretions or saliva containing HBV.[2]
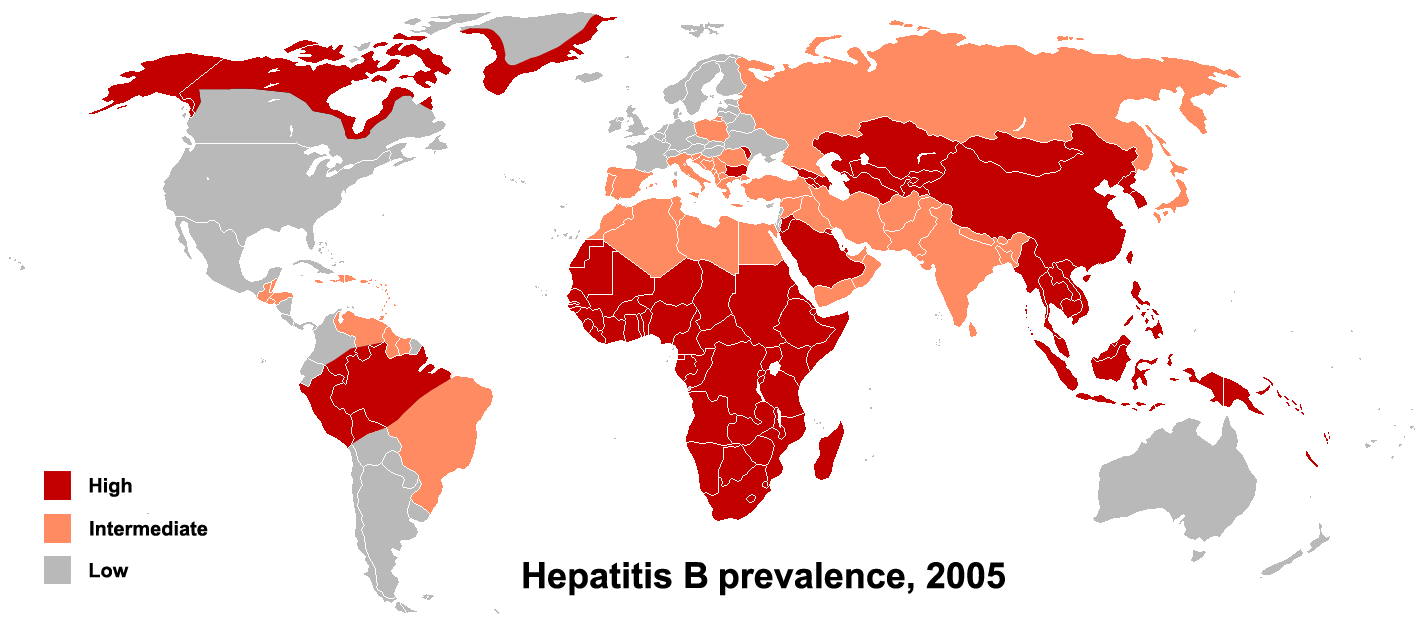
The primary method of transmission reflects the prevalence of chronic HBV infection in a given area. In low prevalence areas such as the continental United States and Western Europe, where less than 2% of the population is chronically infected, injection drug abuse and unprotected sex are the primary methods, although other factors may be important.[3] In moderate prevalence areas, which include Eastern Europe, Russia, and Japan, where 2-7% of the population is chronically infected, the disease is predominantly spread among children. In high prevalence areas such as China and South East Asia, transmission during childbirth is most common, although in other areas of high endemicity such as Africa, transmission during childhood is also a significant factor.[4] The prevalence of chronic HBV infection in areas of high endemicity is at least 8%.
Roughly 16-40% of unimmunized sexual partners of individuals with hepatitis B will be infected through sexual contact. The risk of transmission is closely related to the rate of viral replication in the infected individual at the time of exposure.
Immunopathogenesis
During HBV infection, the host immune response causes both hepatocellular damage and viral clearance. While the innate immune response does not play a significant role in these processes, the adaptive immune response, particularly virus-specific cytotoxic T lymphocytes (CTLs), contributes to nearly all of the liver injury associated with HBV infection. By killing infected cells and by producing antiviral cytokines capable of purging HBV from viable hepatocytes, CTLs also eliminate the virus.[5] Although liver damage is initiated and mediated by the CTLs, antigen-nonspecific inflammatory cells can worsen CTL-induced immunopathology and platelets may facilitate the accumulation of CTLs into the liver.[6]
References
- ↑ Hepadnaviridae characteristics - ICTVdB
- ↑ Petersen NJ, Barrett DH, Bond WW, Berquist KR, Favero MS, Bender TR, Maynard JE (1976). "Hepatitis B surface antigen in saliva, impetiginous lesions, and the environment in two remote Alaskan villages". Appl. Environ. Microbiol. 32 (4): 572–574. PMID 791124.
- ↑ Redd JT, Baumbach J, Kohn W; et al. (2007). "Patient-to-patient transmission of hepatitis B virus associated with oral surgery" (PDF). J Infect Dis. 195 (9): 1311&ndash, 4.
- ↑ Alter MJ (2003). "Epidemiology and prevention of hepatitis B". Semin. Liver Dis. 23 (1): 39–46. doi:10.1055/s-2003-37583. PMID 12616449.
- ↑ Iannacone M.; et al. (2006). "Pathogenetic and antiviral immune responses against hepatitis B virus". Future Virology. 1 (2): 189–196. External link in
|journal=(help) - ↑ Iannacone M, Sitia G, Isogawa M, Marchese P, Castro M, Lowenstein P, Chisari F, Ruggeri Z, Guidotti L (2005). "Platelets mediate cytotoxic T lymphocyte-induced liver damage". Nature Medicine. 11 (11): 1167–1169. PMID 16258538.