Nasopharyngeal angiofibroma
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mahda Alihashemi M.D. [2] Maria Fernanda Villarreal, M.D. [3]
Synonyms and keywords: Juvenile nasopharyngeal angiofibroma (JNA); angiofibroma of the nasopharynx, nasopharyngeal fibroma, bleeding fibroma of adolescence, fibroangioma
Overview
Nasopharyngeal angiofibroma was first described by Hippocrates, a Greek physician, in the 5th century BC. Nasopharyngeal angiofibroma may be classified according to Fisch classification into 4 groups. Nasopharyngeal angiofibroma is a histologically benign tumor. This tumor is located in the posterolateral wall of the nasal cavity. On gross pathology, characteristic findings of nasopharyngeal angiofibroma include tan to purple-red, rubbery-firm unencapsulated polypoid fibrous mass. Fibroblastic cells with plump (near cuboidal) nuclei and abundant capillaries are seen on microscopic histopathological analysis. The cause of Nasopharyngeal angiofibroma has not been identified, but it may be caused by hormonal effect. Incidence of juvenile nasopharyngeal angiofibroma is less than 0.5% of head and neck tumors. If left untreated, %9 of patients with nasopharyngeal angiofibroma may progress to develop hemorrhage and intracranial extension. The hallmark of Nasopharyngeal angiofibroma is the classic triad of epistaxis, unilateral nasal obstruction and a mass in the nasopharynx. Physical examination of patients with Nasopharyngeal angiofibroma is usually remarkable for nasal mass and rhinorrhea. Findings on an x-ray suggestive of nasopharyngeal angiofibroma include nasopharyngeal polyp and Antral sign or Holman-Miller sign (Forward bowing of the posterior wall of the maxillary sinus). CT scan and MRI demonstrate the extent of the tumor. The mainstay of treatment for nasopharyngeal angiofibroma is surgical resection.
Historical Perspective
- Nasopharyngeal angiofibroma was first described by Hippocrates, a Greek physician, in the 5th century BC.[1]
- In 1940, Friedberg was the first to use the term angiofibroma.
- The first endoscopic resection of nasopharyngeal angiofibroma was done in 1996.
Classification
Nasopharyngeal angiofibroma may be classified according to Fisch classification into 4 groups: [2]
- Type I: Sphenopalatine foramen, nasopharynx, and nasal cavity are involved without bone destruction.
- Type II: Nasal sinuses or the pterygomaxillary fossa are involved with bone destruction.
- Type IIIa: Infratemporal fossa or orbit are involved without intracranial involvement.
- Type IIIb: Infratemporal fossa or orbit are involved with intracranial extradural commitment.
- Type IVa: Intracranial extradural and/or intradural are involved, but optic nerve, sella, or cavernous sinus are not involved.
- Type IVb: Intracranial extradural and intradura, optic nerve, sella, and/or cavernous sinus are involved
.
Pathophysiology
Nasopharyngeal angiofibroma is a histologically benign tumor. This tumor is located in the posterolateral wall of the nasal cavity. Nasopharyngeal angiofibroma may involve sphenoid sinuses, maxillary, ethmoid, pterygoid plate , orbit, base of the skull and extradural. In rare cases, nasopharyngeal angiofibroma may involve pituitary, cavernous sinus and/or optic chiasm and anterior fossa. [3]
- Genetic alterations associated with the development of nasopharyngeal angiofibroma include:[4]
- Overexpression PDGF-B
- Overexpression BFGF
- Deletion of chromosome 17
- Tumor suppressor gene p53
- Overexpression of Her-2/neu oncogene
- On gross pathology, characteristic findings of nasopharyngeal angiofibroma include:
- On microscopic histopathological analysis, characteristic findings of nasopharyngeal angiofibroma include:
- Fibroblastic cells with plump (near cuboidal) nuclei
- Fibrous stroma
- Abundant capillaries
- Multinucleated stromal cells
Causes
The cause of Nasopharyngeal angiofibroma has not been identified, but it may be caused by hormonal effect. [6] Nasopharyngeal angiofibroma express higher levels of vascular endothelial growth factor (VEGF) and hormone receptors.
Differentiating Nasopharyngeal angiofibroma from Other Diseases
- Nasopharyngeal angiofibroma must be differentiated from other diseases that cause epistaxis, unilateral nasal obstruction, and rhinorrhea, such as:[7]
Epidemiology and Demographics
Incidence of juvenile nasopharyngeal angiofibroma is less than 0.5% of head and neck tumors. [8]
The incidence of juvenile nasopharyngeal angiofibroma is 0.6 per 100,000 individuals worldwide.[9]
Some reports suggest juvenile nasopharyngeal angiofibroma is more common in the indian subcontinent than in the west.[10]
Men are more commonly affected by juvenile nasopharyngeal angiofibroma than women.
Risk Factors
Common risk factors in the development of nasopharyngeal angiofibroma include:
Screening
There is insufficient evidence to recommend routine screening for nasopharyngeal angiofibroma.
Natural History, Complications, and Prognosis
- If left untreated, %9 of patients with nasopharyngeal angiofibroma may progress to develop hemorrhage and intracranial extension.
- Common complications of nasopharengeal angiofibroma include nasal obstruction and repeated bleeding.[12]
- Prognosis is generally good.
Diagnosis
Diagnostic Study of Choice
The diagnosis of nasopharyngeal angiofibroma is made when the following findings are met:
- Epistaxis
- Unilateral nasal obstruction
- Mass in the nasopharynx
History and Symptoms
The hallmark of Nasopharyngeal angiofibroma is the classic triad of epistaxis, unilateral nasal obstruction and a mass in the nasopharynx. The most common symptoms of Nasopharyngeal angiofibroma include nasal obstruction, epistaxis and headache. Less common symptoms of Nasopharyngeal angiofibroma include conductive hearing loss, diplopia, proptosis, anosmia, recurrent otitis media and eye pain. [13]
Physical Examination
Physical examination of patients with Nasopharyngeal angiofibroma is usually remarkable for nasal mass and rhinorrhea.[13]
Rare physical examination include:
Laboratory Findings
There are no diagnostic laboratory findings associated with nasopharyngeal angiofibroma.
Electrocardiogram
There are no ECG findings associated with nasopharyngeal angiofibroma.
X-ray
An x-ray may be helpful in the diagnosis of nasopharyngeal angiofibroma. Findings on an x-ray suggestive of nasopharyngeal angiofibroma include:[14]
- Nasopharyngeal polyp
- Antral sign or Holman-Miller sign: Forward bowing of the posterior wall of the maxillary sinus
- Maxillary sinus opacification
- Bony margin may be eroded
Echocardiography or Ultrasound
There are no echocardiography/ultrasound findings associated with nasopharyngeal angiofibroma.
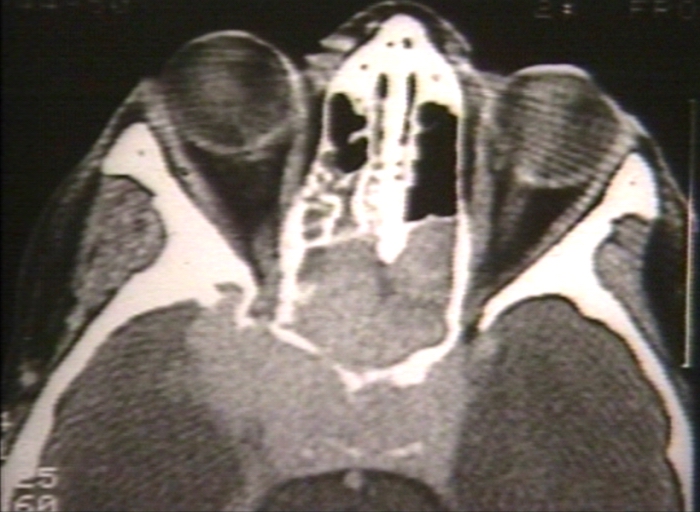
CT scan
CT scan demonstrate the extent of the tumor. Findings on CT scan suggestive of nasopharengeal angiofibroma include:[15]
- Extension to the sphenoid sinus
- Erosion of the greater sphenoidal wing
- invasion of the pterygomaxillary and infratemporal fossae
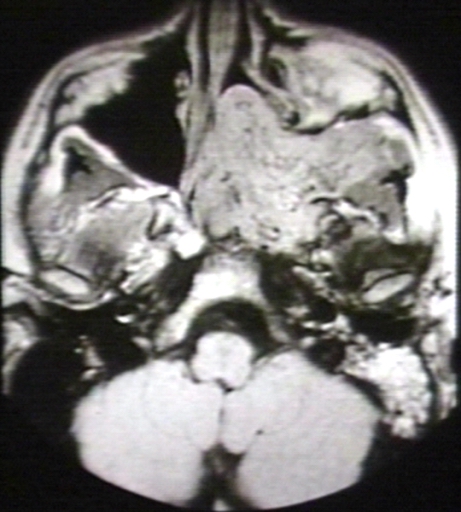
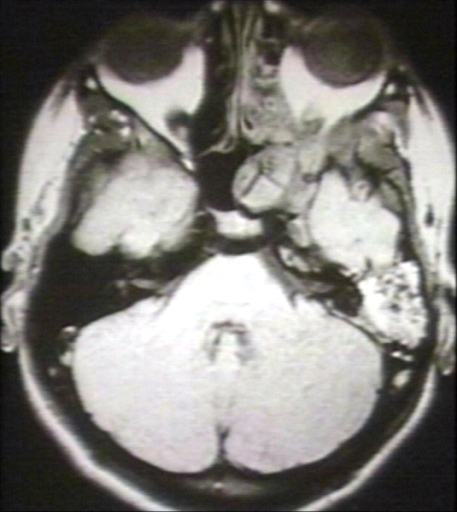
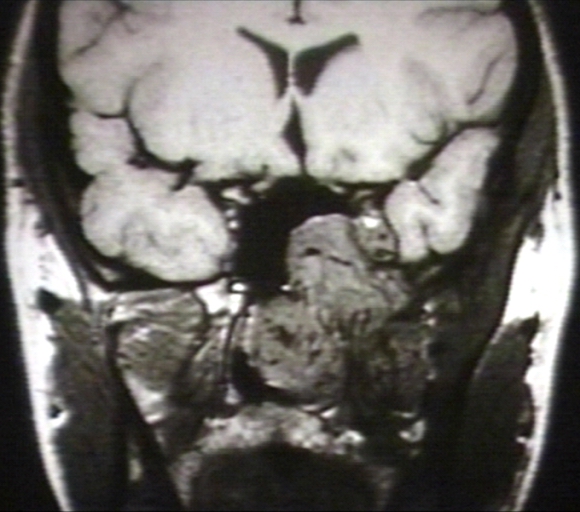
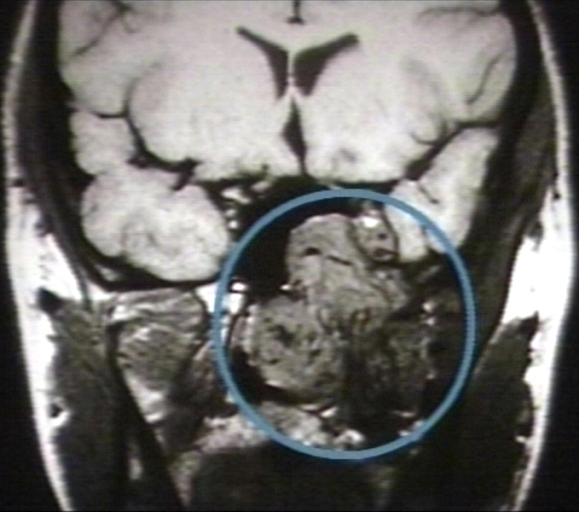
MRI
Cronal MRI demonstrate the extent of the tumor especially in intracranial involvement. [16] Findings on MRI suggestive of nasopharengeal angiofibroma include:[17]
- Largely isointense to muscle on T1-weighted images
- Hyperintense on T2-weighted images
- Internal signal-void regions
- Intense enhancement after intravenous (IV) contrast injection
- The images below demonstrate findings of nasopharyngeal angiofibroma.
-
Nasopharyngeal angiofibroma. Skull base invasionImage courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology
-
MRI (T1): Nasopharyngeal angiofibroma 1/3 Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology
-
MRI (T1): Nasopharyngeal angiofibroma Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology
-
MRI (T1): Nasopharyngeal angiofibroma 3/3 Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology
-
MRI (T1): Nasopharyngeal angiofibroma 3/3 (circled)Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology
Other Imaging Findings
DSA (digital subtraction angiography) of carotid artery is helpful in the diagnosis extension of nasopharengeal angiofibroma and feeding vessel.[18]
Other Diagnostic Studies
Other diagnostic studies for nasopharengeal angiofibroma include nasal endoscopy, which demonstrates hypervascularized large, lobulated mass behind the middle turbinate.[19][20]
Medical Therapy
The mainstay of treatment for nasopharyngeal angiofibroma is surgical resection. Medical therapies for nasopharyngeal angiofibroma include: [21]
Surgery
Arteriography followed by preoperative embolization and surgical resection is the mainstay of treatment for nasopharyngeal angiofibroma. [22]
Surgical approaches for nasopharyngeal angiofibroma include: [23]
- Transpalatal
- Transmaxillary
- Lateral rhinotomy
- Mid-facial degloving
- Extended sublabial Denker
- Le Fort type I osteotomy
- Endoscopic surgery
Primary Prevention
There are no established measures for the primary prevention of Nasopharyngeal angiofibroma.
Secondary Prevention
Once diagnosed and successfully treated, patients with nasopharyngeal angiofibroma are followed-up after surgery, and every 6 or 12 months, depending on the clinical progression.
References
- ↑ Moorthy PN, Ranganatha Reddy B, Qaiyum HA, Madhira S, Kolloju S (October 2010). "Management of juvenile nasopharyngeal angiofibroma: a five year retrospective study". Indian J Otolaryngol Head Neck Surg. 62 (4): 390–4. doi:10.1007/s12070-010-0097-2. PMC 3266082. PMID 22319699.
- ↑ Martins MB, de Lima FV, Mendonça CA, de Jesus EP, Santos AC, Barreto VM, Santos RC (January 2013). "Nasopharyngeal angiofibroma: Our experience and literature review". Int Arch Otorhinolaryngol. 17 (1): 14–9. doi:10.7162/S1809-97772013000100003. PMC 4423317. PMID 25991988.
- ↑ Pryor SG, Moore EJ, Kasperbauer JL (July 2005). "Endoscopic versus traditional approaches for excision of juvenile nasopharyngeal angiofibroma". Laryngoscope. 115 (7): 1201–7. doi:10.1097/01.MLG.0000162655.96247.66. PMID 15995507.
- ↑
- ↑ McKnight CD, Parmar HA, Watcharotone K, Mukherji SK (2017). "Reassessing the Anatomic Origin of the Juvenile Nasopharyngeal Angiofibroma". J Comput Assist Tomogr. 41 (4): 559–564. doi:10.1097/RCT.0000000000000566. PMID 28632604.
- ↑ Liu Z, Wang J, Wang H, Wang D, Hu L, Liu Q, Sun X (January 2015). "Hormonal receptors and vascular endothelial growth factor in juvenile nasopharyngeal angiofibroma: immunohistochemical and tissue microarray analysis". Acta Otolaryngol. 135 (1): 51–7. doi:10.3109/00016489.2014.952774. PMID 25384380.
- ↑ Alimli AG, Ucar M, Oztunali C, Akkan K, Boyunaga O, Damar C, Derinkuyu B, Tokgöz N (June 2016). "Juvenile Nasopharyngeal Angiofibroma: Magnetic Resonance Imaging Findings". J Belg Soc Radiol. 100 (1): 63. doi:10.5334/jbr-btr.1090. PMC 5854277. PMID 30038985.
- ↑ Gullane PJ, Davidson J, O'Dwyer T, Forte V (August 1992). "Juvenile angiofibroma: a review of the literature and a case series report". Laryngoscope. 102 (8): 928–33. doi:10.1288/00005537-199208000-00014. PMID 1323003.
- ↑ Coutinho-Camillo CM, Brentani MM, Nagai MA (March 2008). "Genetic alterations in juvenile nasopharyngeal angiofibromas". Head Neck. 30 (3): 390–400. doi:10.1002/hed.20775. PMID 18228521.
- ↑ Biswas D, Saha S, Bera SP (May 2007). "Relative distribution of the tumours of ear, nose and throat in the paediatric patients". Int. J. Pediatr. Otorhinolaryngol. 71 (5): 801–5. doi:10.1016/j.ijporl.2007.01.021. PMID 17368816.
- ↑ Ponti G, Losi L, Pellacani G, Rossi GB, Presutti L, Mattioli F, Villari D, Wannesson L, Alicandri Ciufelli M, Izzo P, De Rosa M, Marone P, Seidenari S (March 2008). "Wnt pathway, angiogenetic and hormonal markers in sporadic and familial adenomatous polyposis-associated juvenile nasopharyngeal angiofibromas (JNA)". Appl. Immunohistochem. Mol. Morphol. 16 (2): 173–8. doi:10.1097/PAI.0b013e31806bee12. PMID 18227724.
- ↑ Roy Chowdhury S, Rajkumar K, Deshmukh T (March 2017). "Complications of Midface Swing for Management of Juvenile Nasopharyngeal Angiofibroma". J Maxillofac Oral Surg. 16 (1): 96–100. doi:10.1007/s12663-016-0947-x. PMC 5328877. PMID 28286392.
- ↑ 13.0 13.1 Enepekides DJ (December 2004). "Recent advances in the treatment of juvenile angiofibroma". Curr Opin Otolaryngol Head Neck Surg. 12 (6): 495–9. PMID 15548906.
- ↑ Ikubor JE, Okolugbo NE, Okhakhu AL (2013). "Radiological features of juvenile nasopharyngeal angiofibroma". J West Afr Coll Surg. 3 (4): 84–91. PMC 4437236. PMID 26046027.
- ↑ Mishra S, Praveena NM, Panigrahi RG, Gupta YM (2013). "Imaging in the diagnosis of juvenile nasopharyngeal angiofibroma". J Clin Imaging Sci. 3 (Suppl 1): 1. doi:10.4103/2156-7514.109469. PMC 3716018. PMID 23878770.
- ↑ Mishra S, Praveena NM, Panigrahi RG, Gupta YM (2013). "Imaging in the diagnosis of juvenile nasopharyngeal angiofibroma". J Clin Imaging Sci. 3 (Suppl 1): 1. doi:10.4103/2156-7514.109469. PMC 3716018. PMID 23878770.
- ↑ Alimli AG, Ucar M, Oztunali C, Akkan K, Boyunaga O, Damar C, Derinkuyu B, Tokgöz N (June 2016). "Juvenile Nasopharyngeal Angiofibroma: Magnetic Resonance Imaging Findings". J Belg Soc Radiol. 100 (1): 63. doi:10.5334/jbr-btr.1090. PMC 5854277. PMID 30038985.
- ↑ Giavroglou C, Constantinidis J, Triaridis S, Daniilidis J, Dimitriadis A (January 2007). "[Angiographic evaluation and embolization of juvenile nasopharyngeal angiofibroma]". HNO (in German). 55 (1): 36–41. doi:10.1007/s00106-006-1410-y. PMID 16775738.
- ↑ Makhasana JA, Kulkarni MA, Vaze S, Shroff AS (2016). "Juvenile nasopharyngeal angiofibroma". J Oral Maxillofac Pathol. 20 (2): 330. doi:10.4103/0973-029X.185908. PMC 4989574. PMID 27601836.
- ↑ Nicolai P, Schreiber A, Bolzoni Villaret A (2012). "Juvenile angiofibroma: evolution of management". Int J Pediatr. 2012: 412545. doi:10.1155/2012/412545. PMID 22164185.
- ↑ Enepekides DJ (December 2004). "Recent advances in the treatment of juvenile angiofibroma". Curr Opin Otolaryngol Head Neck Surg. 12 (6): 495–9. PMID 15548906.
- ↑ Nicolai P, Schreiber A, Bolzoni Villaret A (2012). "Juvenile angiofibroma: evolution of management". Int J Pediatr. 2012: 412545. doi:10.1155/2012/412545. PMC 3228400. PMID 22164185.
- ↑ Nicolai P, Schreiber A, Bolzoni Villaret A (2012). "Juvenile angiofibroma: evolution of management". Int J Pediatr. 2012: 412545. doi:10.1155/2012/412545. PMID 22164185.