Lopressor/warnings: Difference between revisions
| Line 61: | Line 61: | ||
Start at a low dose and uptitrate slowly in patients with impaired [[Liver function tests|hepatic function]]. | Start at a low dose and uptitrate slowly in patients with impaired [[Liver function tests|hepatic function]]. | ||
====Information for Patients==== | |||
Advise patients to take Lopressor regularly and continuously, as directed, with or immediately following meals. If a dose should be missed, the patient should take only the next scheduled dose (without doubling it). | Advise patients to take Lopressor regularly and continuously, as directed, with or immediately following meals. If a dose should be missed, the patient should take only the next scheduled dose (without doubling it). Patients should not discontinue Lopressor without consulting the physician. | ||
Patients should not discontinue Lopressor without consulting the physician. | |||
Advise patients to: | Advise patients to: | ||
Revision as of 04:53, 13 March 2014
 | |
| Clinical data | |
|---|---|
| Trade names | Lopressor, Toprol-xl |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682864 |
| [[Regulation of therapeutic goods |Template:Engvar data]] |
|
| Pregnancy category | |
| Routes of administration | Oral, IV |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 12% |
| Metabolism | Hepatic via CYP2D6, CYP3A4 |
| Elimination half-life | 3-7 hours |
| Excretion | Renal |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| E number | {{#property:P628}} |
| ECHA InfoCard | {{#property:P2566}}Lua error in Module:EditAtWikidata at line 36: attempt to index field 'wikibase' (a nil value). |
| Chemical and physical data | |
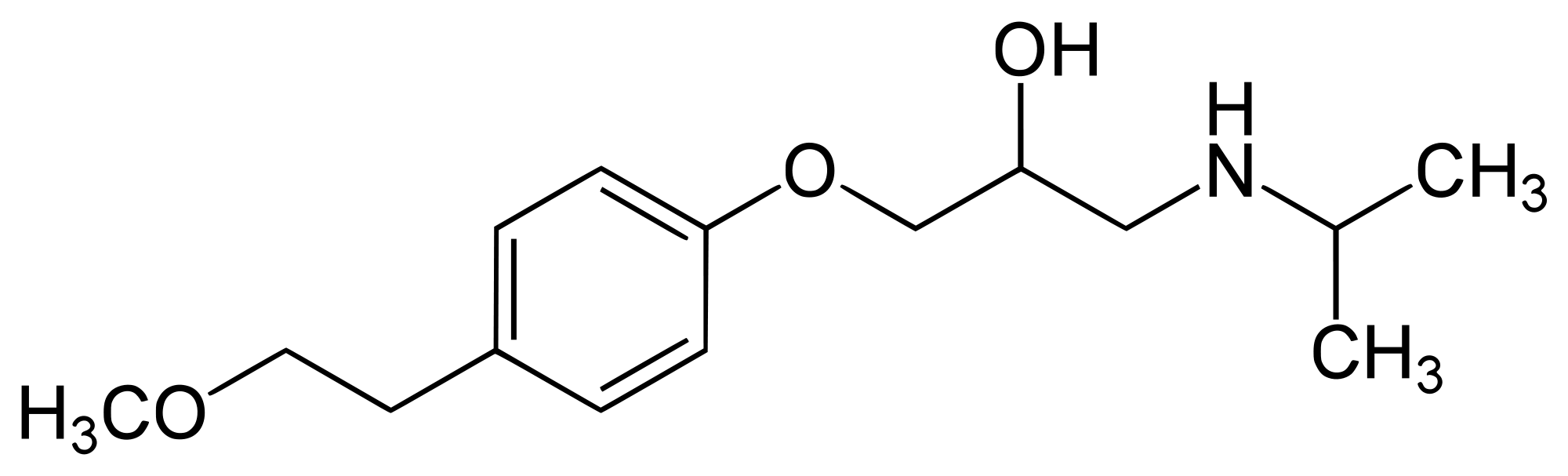
| Formula | C15H25NO3 |
| Molar mass | 267.364 g/mol |
| 3D model (JSmol) | |
| Melting point | 120 °C (248 °F) |
| |
| |
| (verify) | |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
|
WARNING See full prescribing information for complete boxed warning.
|
Warnings
Hypertension and Angina
Cardiac Failure: Sympathetic stimulation is a vital component supporting circulatory function in congestive heart failure, and beta blockade carries the potential hazard of further depressing myocardial contractility and precipitating more severe failure.
In Patients Without a History of Cardiac Failure: Continued depression of the myocardium with beta-blocking agents over a period of time can, in some cases, lead to cardiac failure. At the first sign or symptom of impending cardiac failure, fully digitalize patients and/or give a diuretic. The response should be observed closely. If cardiac failure continues, despite adequate digitalization and diuretic therapy, withdraw Lopressor.
Bronchospastic Diseases: PATIENTS WITH BRONCHOSPASTIC DISEASES SHOULD, IN GENERAL, NOT RECEIVE BETA BLOCKERS, including Lopressor. Because of its relative beta-1 selectivity, however, Lopressor may be used with caution in patients with bronchospastic disease who do not respond to, or cannot tolerate, other antihypertensive treatment. Since beta-1 selectivity is not absolute, a beta2-stimulating agent should be administered concomitantly, and the lowest possible dose of Lopressor should be used. In these circumstances it would be prudent initially to administer Lopressor in smaller doses three times daily, instead of larger doses two times daily, to avoid the higher plasma levels associated with the longer dosing interval (see Dosage and Administration).
Major Surgery: Chronically administered beta-blocking therapy should not be routinely withdrawn prior to major surgery; however, the impaired ability of the heart to respond to reflex adrenergic stimuli may augment the risks of general anesthesia and surgical procedures.
Diabetes and Hypoglycemia: Beta blockers may mask tachycardia occurring with hypoglycemia, but other manifestations such as dizziness and sweating may not be significantly affected.
Pheochromocytoma: If Lopressor is used in the setting of pheochromocytoma, it should be given in combination with an alpha blocker, and only after the alpha blocker has been initiated. Administration of beta blockers alone in the setting of pheochromocytoma has been associated with a paradoxical increase in blood pressure due to the attenuation of beta-mediated vasodilatation in skeletal muscle.
Thyrotoxicosis: Beta-adrenergic blockade may mask certain clinical signs (e.g., tachycardia) of hyperthyroidism. Avoid abrupt withdrawal of beta blockade, which might precipitate a thyroid storm.
Myocardial Infarction
Cardiac Failure: Sympathetic stimulation is a vital component supporting circulatory function, and beta blockade carries the potential hazard of depressing myocardial contractility and precipitating or exacerbating minimal cardiac failure.
During treatment with Lopressor, monitor the hemodynamic status of the patient. If heart failure occurs or persists despite appropriate treatment, discontinue Lopressor.
Bradycardia: Lopressor produces a decrease in sinus heart rate in most patients; this decrease is greatest among patients with high initial heart rates and least among patients with low initial heart rates. Acute myocardial infarction (particularly inferior infarction) may in itself produce significant lowering of the sinus rate. If the sinus rate decreases to <40 beats/min, particularly if associated with evidence of lowered cardiac output, atropine (0.25-0.5 mg) should be administered intravenously. If treatment with atropine is not successful, discontinue Lopressor and consider cautious administration of isoproterenol or installation of a cardiac pacemaker.
AV Block: Lopressor slows AV conduction and may produce significant first- (PR interval ≥0.24 sec), second-, or third-degree heart block. Acute myocardial infarction also produces heart block.
If heart block occurs, discontinue Lopressor and administer atropine (0.25-0.5 mg) intravenously. If treatment with atropine is not successful, consider administration of isoproterenol or installation of a cardiac pacemaker.
Hypotension: If hypotension (systolic blood pressure ≤90 mmHg) occurs, discontinue Lopressor, and assess the hemodynamic status of the patient and the extent of myocardial damage. Invasive monitoring of central venous, pulmonary capillary wedge, and arterial pressures may be required. Institute appropriate therapy with fluids, positive inotropic agents, balloon counterpulsation, or other treatment modalities. If hypotension is associated with sinus bradycardia or AV block, direct treatment at reversing these (see above).
Precautions
General
Start at a low dose and uptitrate slowly in patients with impaired hepatic function.
Information for Patients
Advise patients to take Lopressor regularly and continuously, as directed, with or immediately following meals. If a dose should be missed, the patient should take only the next scheduled dose (without doubling it). Patients should not discontinue Lopressor without consulting the physician.
Advise patients to:
- Avoid operating automobiles and machinery or engaging in other tasks requiring alertness until the patient’s response to therapy with Lopressor has been determined.
- Contact the physician if any difficulty in breathing occurs.
- Inform the physician or dentist before any type of surgery that he or she is taking Lopressor.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term studies in animals have been conducted to evaluate carcinogenic potential. In a 2-year study in rats at three oral dosage levels of up to 800 mg/kg per day, there was no increase in the development of spontaneously occurring benign or malignant neoplasms of any type. The only histologic changes that appeared to be drug related were an increased incidence of generally mild focal accumulation of foamy macrophages in pulmonary alveoli and a slight increase in biliary hyperplasia. In a 21-month study in Swiss albino mice at three oral dosage levels of up to 750 mg/kg per day, benign lung tumors (small adenomas) occurred more frequently in female mice receiving the highest dose than in untreated control animals. There was no increase in malignant or total (benign plus malignant) lung tumors, or in the overall incidence of tumors or malignant tumors. This 21-month study was repeated in CD-1 mice, and no statistically or biologically significant differences were observed between treated and control mice of either sex for any type of tumor.
All mutagenicity tests performed (a dominant lethal study in mice, chromosome studies in somatic cells, a Salmonella/mammalian-microsome mutagenicity test, and a nucleus anomaly test in somatic interphase nuclei) were negative.
Reproduction toxicity studies in mice, rats and rabbits did not indicate teratogenic potential for metoprolol tartrate. Embryotoxicity and/or fetotoxicity in rats and rabbits were noted starting at doses of 50 mg/kg in rats and 25 mg/kg in rabbits, as demonstrated by increases in preimplantation loss, decreases in the number of viable fetuses per dose, and/or decreases in neonatal survival. High doses were associated with some maternal toxicity, and growth delay of the offspring in utero, which was reflected in minimally lower weights at birth. The oral NOAELs for embryo-fetal development in mice, rats, and rabbits were considered to be 25, 200, and 12.5 mg/kg. This corresponds to dose levels that are approximately 0.3, 4, and 0.5 times, respectively, when based on surface area, the maximum human oral dose (8 mg/kg/day) of metoprolol tartrate. Metoprolol tartrate has been associated with reversible adverse effects on spermatogenesis starting at oral dose levels of 3.5 mg/kg in rats (a dose that is only 0.1-times the human dose, when based on surface area), although other studies have shown no effect of metoprolol tartrate on reproductive performance in male rats.[1]
References
Adapted from the FDA Package Insert.
- Pages with script errors
- Template:drugs.com link with non-standard subpage
- Drugs with non-standard legal status
- E number from Wikidata
- ECHA InfoCard ID from Wikidata
- Chemical articles with unknown parameter in Infobox drug
- Infobox drug articles with non-default infobox title
- Beta blockers
- Cardiovascular Drugs
- Drugs