Meropenem microbiology: Difference between revisions
No edit summary |
|||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Meropenem}} | {{Meropenem}} | ||
{{CMG}} | {{CMG}} | ||
==Microbiology== | ==Microbiology== | ||
| Line 9: | Line 8: | ||
Meropenem is a broad-spectrum [[Carbapenem]] antibiotic. It is active against Gram-positive and Gram-negative bacteria. The bactericidal activity of meropenem results from the inhibition of cell wall synthesis. Meropenem readily penetrates the cell wall of most Gram-positive and Gram-negative bacteria to reach penicillin-binding-protein (PBP) targets. Its strongest affinities are toward PBPs 2, 3 and 4 of [[Escherichia coli]] and [[Pseudomonas | Meropenem is a broad-spectrum [[Carbapenem]] antibiotic. It is active against Gram-positive and Gram-negative bacteria. The bactericidal activity of meropenem results from the inhibition of cell wall synthesis. Meropenem readily penetrates the cell wall of most Gram-positive and Gram-negative bacteria to reach penicillin-binding-protein (PBP) targets. Its strongest affinities are toward PBPs 2, 3 and 4 of [[Escherichia coli]] and [[Pseudomonas | ||
aeruginosa]]; and PBPs 1, 2 and 4 of [[Staphylococcus aureus]]. Bactericidal concentrations (defined as a 3 log10 reduction in cell counts within 12 to 24 hours) are typically 1-2 times the bacteriostatic concentrations of meropenem, with the exception of [[Listeria monocytogenes]] | aeruginosa]]; and PBPs 1, 2 and 4 of [[Staphylococcus aureus]]. Bactericidal concentrations (defined as a 3 log10 reduction in cell counts within 12 to 24 hours) are typically 1-2 times the bacteriostatic concentrations of meropenem, with the exception of [[Listeria monocytogenes]] | ||
against which lethal activity is not observed. | against which lethal activity is not observed. | ||
Meropenem has significant stability to hydrolysis by β-lactamases of most categories, both penicillinases and cephalosporinases produced by Gram-positive and Gram-negative bacteria. | Meropenem has significant stability to hydrolysis by β-lactamases of most categories, both penicillinases and cephalosporinases produced by Gram-positive and Gram-negative bacteria. | ||
Meropenem should not be used to treat methicillin-resistant [[staphylococci]] (MRSA). | Meropenem should not be used to treat methicillin-resistant [[staphylococci]] (MRSA). | ||
In vitro tests show meropenem to act synergistically with aminoglycoside antibiotics against some | In vitro tests show meropenem to act synergistically with aminoglycoside antibiotics against some | ||
isolates of [[Pseudomonas aeruginosa]]. | isolates of [[Pseudomonas aeruginosa]]. | ||
'''Lists of Microorganisms ''' | '''Lists of Microorganisms ''' | ||
Meropenem has been shown to be active against most isolates of the following microorganisms, both in vitro and in clinical infections as described in the INDICATIONS AND USAGE section. | Meropenem has been shown to be active against most isolates of the following microorganisms, both in vitro and in clinical infections as described in the INDICATIONS AND USAGE section. | ||
''''[[Aerobic]] and facultative Gram-positive microorganisms '''' | ''''[[Aerobic]] and facultative Gram-positive microorganisms '''' | ||
[[Enterococcus faecalis]] (excluding [[vancomycin]]-resistant isolates) | *[[Enterococcus faecalis]] (excluding [[vancomycin]]-resistant isolates) | ||
[[Staphylococcus aureus]] (β-lactamase and non-β-lactamase producing, [[methicillin]]-susceptible isolates | *[[Staphylococcus aureus]] (β-lactamase and non-β-lactamase producing, [[methicillin]]-susceptible isolates | ||
only) | only) | ||
[[Streptococcus agalactiae]] | *[[Streptococcus agalactiae]] | ||
[[Streptococcus pneumoniae]] ([[penicillin]]-susceptible isolates only) | *[[Streptococcus pneumoniae]] ([[penicillin]]-susceptible isolates only) | ||
'''NOTE''': [[Penicillin]]-resistant isolates had [[meropenem]] MIC90 values of 1 or 2 µg/mL, which is above the 0.12 µg/mL susceptible breakpoint for this species. | '''NOTE''': [[Penicillin]]-resistant isolates had [[meropenem]] MIC90 values of 1 or 2 µg/mL, which is above the 0.12 µg/mL susceptible breakpoint for this species. | ||
[[Streptococcus pyogenes]] | *[[Streptococcus pyogenes]] | ||
Viridans group streptococci | Viridans group [[streptococci]] | ||
'''[[Aerobic]] and facultative Gram-negative microorganisms ''' | '''[[Aerobic]] and facultative Gram-negative microorganisms ''' | ||
[[Escherichia coli]] | [[Escherichia coli]] | ||
[[Haemophilus influenzae]] (β-lactamase and non-β-lactamase producing) | [[Haemophilus influenzae]] (β-lactamase and non-β-lactamase producing) | ||
[[Klebsiella pneumoniae]] | [[Klebsiella pneumoniae]] | ||
[[Neisseria meningitidis ]] | [[Neisseria meningitidis ]] | ||
[[Pseudomonas aeruginosa ]] | [[Pseudomonas aeruginosa ]] | ||
[[Proteus mirabilis]] | [[Proteus mirabilis]] | ||
The following in vitro data are available, but their clinical significance is unknown. | '''[[[[anaerobic]]]] microorganisms ''' | ||
*[[[[Bacteroides]]]] fragilis | |||
At least 90% of the following microorganisms exhibit an in vitro minimum inhibitory concentration (MIC) less than or equal to the susceptible breakpoints for meropenem. However, the safety and effectiveness of meropenem in treating clinical infections due to these microorganisms have not been | *[[[[Bacteroides]]]] [[thetaiotaomicron ]] | ||
*[[Peptostreptococcus]] species | |||
The following in vitro data are available, but their clinical significance is unknown. | |||
At least 90% of the following microorganisms exhibit an in vitro minimum inhibitory concentration (MIC) less than or equal to the susceptible breakpoints for meropenem. However, the safety and effectiveness of meropenem in treating clinical infections due to these microorganisms have not been | |||
established in adequate and well-controlled trials. | established in adequate and well-controlled trials. | ||
Aerobic and facultative Gram-positive microorganisms | Aerobic and facultative Gram-positive microorganisms | ||
Staphylococcus epidermidis (β-lactamase and non-β-lactamase-producing, methicillin-susceptible | Staphylococcus epidermidis (β-lactamase and non-β-lactamase-producing, methicillin-susceptible | ||
isolates only). | isolates only). | ||
'''Aerobic and facultative Gram-negative microorganisms ''' | '''Aerobic and facultative Gram-negative microorganisms ''' | ||
Acinetobacter species | *Acinetobacter species | ||
Aeromonas hydrophila | *Aeromonas hydrophila | ||
Campylobacter jejuni | *Campylobacter jejuni | ||
Citrobacter diversus | *Citrobacter diversus | ||
Moraxella catarrhalis | *Moraxella catarrhalis | ||
(β-lactamase and non-β-lactamase-producing isolates) | (β-lactamase and non-β-lactamase-producing isolates) | ||
Citrobacter freundii | *Citrobacter freundii * | ||
Enterobacter cloacae | *Enterobacter cloacae | ||
Haemophilus influenzae | *Haemophilus influenzae | ||
(ampicillin-resistant, non-β-lactamase-producing isolates[BLNAR isolates]) | (ampicillin-resistant, non-β-lactamase-producing isolates[BLNAR isolates]) | ||
Proteus vulgaris | *Proteus vulgaris | ||
Salmonella species | *Salmonella species | ||
Serratia marcescens | *Serratia marcescens | ||
Hafnia alvei | *Hafnia alvei | ||
Klebsiella oxytoca | *Klebsiella oxytoca | ||
*Shigella species | |||
*Moraxella catarrhalis | |||
* | |||
* | |||
*Yersinia enterocolitica* | |||
*Pasteurella multocida | |||
'''[[anaerobic]] microorganisms ''' | |||
*[[Bacteroides]] distasonis | |||
*[[Bacteroides]] ovatus | |||
*[[Bacteroides]] uniformis | |||
*[[Bacteroides]] ureolyticus | |||
*[[Bacteroides]] vulgatus | |||
*[[Clostridium difficile]] | |||
*[[Clostridium perfringens]] | |||
*[[Eubacterium lentum]] | |||
*[[Fusobacterium species]] | |||
*[[Prevotella bivia]] | |||
*[[Prevotella intermedia]] | |||
*[[Prevotella melaninogenica]] | |||
*[[Porphyromonas asaccharolytica]] | |||
*[[Propionibacterium acnes]] | |||
'''''SUSCEPTIBILITY TEST METHODS ''''' | '''''SUSCEPTIBILITY TEST METHODS ''''' | ||
When available, the clinical microbiology laboratory should provide cumulative results of in vitro susceptibility test results for antimicrobial drugs used in local hospitals and practice areas to the physician as periodic reports that describe the susceptibility profile of nosocomial and community- | When available, the clinical microbiology laboratory should provide cumulative results of in vitro susceptibility test results for antimicrobial drugs used in local hospitals and practice areas to the physician as periodic reports that describe the susceptibility profile of nosocomial and community- | ||
acquired pathogens. These reports should aid the physician in selecting the most effective antimicrobial. | acquired pathogens. These reports should aid the physician in selecting the most effective antimicrobial. | ||
'''Dilution techniques: ''' | '''Dilution techniques: ''' | ||
Quantitative methods are used to determine antimicrobial minimum inhibitory concentrations (MICs). These MICs provide estimates of the susceptibility of bacteria to antimicrobial compounds. The MICs should be determined using a standardized procedure. Standardized procedures are based on a dilution | Quantitative methods are used to determine antimicrobial minimum inhibitory concentrations (MICs). These MICs provide estimates of the susceptibility of bacteria to antimicrobial compounds. The MICs should be determined using a standardized procedure. Standardized procedures are based on a dilution | ||
method1,3 (broth or agar) or equivalent with standardized inoculum concentrations and standardized concentrations of meropenem powder. The MIC values should be interpreted according to the criteria provided in Table below. | method1,3 (broth or agar) or equivalent with standardized inoculum concentrations and standardized concentrations of meropenem powder. The MIC values should be interpreted according to the criteria provided in Table below. | ||
'''Diffusion techniques: ''' | '''Diffusion techniques: ''' | ||
Quantitative methods that require measurement of zone diameters also provide reproducible estimates of the susceptibility of bacteria to antimicrobial compounds. One such standardized procedure requires the use of standardized inoculum concentrations. This procedure uses paper disks impregnated with 10-µg of meropenem to test the susceptibility of microorganisms to meropenem. The disk diffusion interpretive criteria are provided in Table below. | Quantitative methods that require measurement of zone diameters also provide reproducible estimates of the susceptibility of bacteria to antimicrobial compounds. One such standardized procedure requires the use of standardized inoculum concentrations. This procedure uses paper disks impregnated with 10-µg of meropenem to test the susceptibility of microorganisms to meropenem. The disk diffusion interpretive criteria are provided in Table below. | ||
Streptococcus pneumoniae isolates should be tested using 1-µg/mL oxacillin disk. Isolates with oxacillin zone sizes of ≥ 20 mm are susceptible (MIC ≤ 0.06 µg/mL) to penicillin and can be considered susceptible to meropenem for approved indications, and meropenem need not be tested. A meropenem MIC should be determined on isolates of S. pneumoniae with oxacillin zone sizes of ≤19 mm. The disk test does not distinguish penicillin intermediate isolates (i.e., MICs = 0.12-1.0 µg/mL) from isolates that are penicillin resistant (i.e., MICs ≥ 2 µg/mL). Viridans group streptococci should be tested for meropenem susceptibility using an MIC method. Reliable disk diffusion tests for meropenem do not yet exist for testing streptococci. | Streptococcus pneumoniae isolates should be tested using 1-µg/mL oxacillin disk. Isolates with oxacillin zone sizes of ≥ 20 mm are susceptible (MIC ≤ 0.06 µg/mL) to penicillin and can be considered susceptible to meropenem for approved indications, and meropenem need not be tested. A meropenem MIC should be determined on isolates of S. pneumoniae with oxacillin zone sizes of ≤19 mm. The disk test does not distinguish penicillin intermediate isolates (i.e., MICs = 0.12-1.0 µg/mL) from isolates that are penicillin resistant (i.e., MICs ≥ 2 µg/mL). Viridans group streptococci should be tested for meropenem susceptibility using an MIC method. Reliable disk diffusion tests for meropenem do not yet exist for testing streptococci. | ||
''' | '''[[anaerobic]] techniques: ''' | ||
For anaerobic bacteria, the susceptibility to meropenem as MICs can be determined by standardized test methods.The MIC values obtained should be interpreted according to the criteria provided in Table below. | For [[[[anaerobic]]]] bacteria, the susceptibility to meropenem as MICs can be determined by standardized test methods.The MIC values obtained should be interpreted according to the criteria provided in Table below. | ||
{| | {| | ||
| Line 113: | Line 117: | ||
|[[File:Meropenem 11.jpg|thumb|800px|left]] | |[[File:Meropenem 11.jpg|thumb|800px|left]] | ||
|- | |- | ||
|} | |||
No interpretative criteria have been established for testing enterococci and Neisseria meningitidis. | |||
A report of Susceptible indicates that the antimicrobial is likely to inhibit growth of the pathogen if the antimicrobial compound in the blood reaches the concentrations usually achievable. A report of Intermediate indicates that the result should be considered equivocal, and, if the microorganism is not fully susceptible to alternative, clinically feasible drugs, the test should be repeated. This category implies possible clinical applicability in body sites where the drug is physiologically concentrated or in situations where a high dosage of drug can be used. This category also provides a buffer zone that prevents small uncontrolled technical factors from causing major discrepancies in interpretation. A report of Resistant indicates that the antimicrobial is not likely to inhibit growth of the pathogen if the ntimicrobial compound in the blood reaches the concentrations usually achievable; other therapy should be selected. | |||
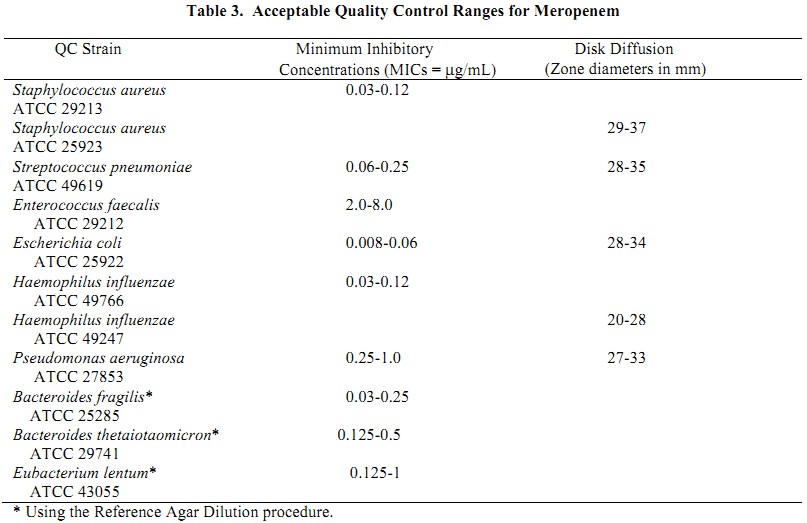
Quality control: | |||
Quality control: | |||
Standardized susceptibility test procedures require the use of quality control microorganisms to control the technical aspects of the test procedures. Standard meropenem powder should provide the following range of values noted in Table below. | Standardized susceptibility test procedures require the use of quality control microorganisms to control the technical aspects of the test procedures. Standard meropenem powder should provide the following range of values noted in Table below. | ||
| Line 129: | Line 130: | ||
|[[File:Meropenem 12.jpg|thumb|800px|left]] | |[[File:Meropenem 12.jpg|thumb|800px|left]] | ||
|- | |- | ||
|} | |}<ref>{{Cite web | last = | first = |title = http://www.accessdata.fda.gov/drugsatfda_docs/label/2008/050706s022lbl.pdf | url =http://www.accessdata.fda.gov/drugsatfda_docs/label/2008/050706s022lbl.pdf | publisher = |date = | accessdate = }}</ref> | ||
==References== | ==References== | ||
Revision as of 22:58, 20 December 2013
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Microbiology
Meropenem is a broad-spectrum Carbapenem antibiotic. It is active against Gram-positive and Gram-negative bacteria. The bactericidal activity of meropenem results from the inhibition of cell wall synthesis. Meropenem readily penetrates the cell wall of most Gram-positive and Gram-negative bacteria to reach penicillin-binding-protein (PBP) targets. Its strongest affinities are toward PBPs 2, 3 and 4 of Escherichia coli and [[Pseudomonas aeruginosa]]; and PBPs 1, 2 and 4 of Staphylococcus aureus. Bactericidal concentrations (defined as a 3 log10 reduction in cell counts within 12 to 24 hours) are typically 1-2 times the bacteriostatic concentrations of meropenem, with the exception of Listeria monocytogenes against which lethal activity is not observed. Meropenem has significant stability to hydrolysis by β-lactamases of most categories, both penicillinases and cephalosporinases produced by Gram-positive and Gram-negative bacteria. Meropenem should not be used to treat methicillin-resistant staphylococci (MRSA). In vitro tests show meropenem to act synergistically with aminoglycoside antibiotics against some isolates of Pseudomonas aeruginosa.
Lists of Microorganisms
Meropenem has been shown to be active against most isolates of the following microorganisms, both in vitro and in clinical infections as described in the INDICATIONS AND USAGE section.
'Aerobic and facultative Gram-positive microorganisms '
- Enterococcus faecalis (excluding vancomycin-resistant isolates)
- Staphylococcus aureus (β-lactamase and non-β-lactamase producing, methicillin-susceptible isolates
only)
- Streptococcus pneumoniae (penicillin-susceptible isolates only)
NOTE: Penicillin-resistant isolates had meropenem MIC90 values of 1 or 2 µg/mL, which is above the 0.12 µg/mL susceptible breakpoint for this species.
Viridans group streptococci
Aerobic and facultative Gram-negative microorganisms Escherichia coli Haemophilus influenzae (β-lactamase and non-β-lactamase producing) Klebsiella pneumoniae Neisseria meningitidis Pseudomonas aeruginosa Proteus mirabilis
[[anaerobic]] microorganisms
- [[Bacteroides]] fragilis
- [[Bacteroides]] thetaiotaomicron
- Peptostreptococcus species
The following in vitro data are available, but their clinical significance is unknown.
At least 90% of the following microorganisms exhibit an in vitro minimum inhibitory concentration (MIC) less than or equal to the susceptible breakpoints for meropenem. However, the safety and effectiveness of meropenem in treating clinical infections due to these microorganisms have not been established in adequate and well-controlled trials.
Aerobic and facultative Gram-positive microorganisms Staphylococcus epidermidis (β-lactamase and non-β-lactamase-producing, methicillin-susceptible isolates only).
Aerobic and facultative Gram-negative microorganisms
- Acinetobacter species
- Aeromonas hydrophila
- Campylobacter jejuni
- Citrobacter diversus
- Moraxella catarrhalis
(β-lactamase and non-β-lactamase-producing isolates)
- Citrobacter freundii *
- Enterobacter cloacae
- Haemophilus influenzae
(ampicillin-resistant, non-β-lactamase-producing isolates[BLNAR isolates])
- Proteus vulgaris
- Salmonella species
- Serratia marcescens
- Hafnia alvei
- Klebsiella oxytoca
- Shigella species
- Moraxella catarrhalis
- Yersinia enterocolitica*
- Pasteurella multocida
anaerobic microorganisms
- Bacteroides distasonis
- Bacteroides ovatus
- Bacteroides uniformis
- Bacteroides ureolyticus
- Bacteroides vulgatus
- Clostridium difficile
- Clostridium perfringens
- Eubacterium lentum
- Fusobacterium species
- Prevotella bivia
- Prevotella intermedia
- Prevotella melaninogenica
- Porphyromonas asaccharolytica
- Propionibacterium acnes
SUSCEPTIBILITY TEST METHODS
When available, the clinical microbiology laboratory should provide cumulative results of in vitro susceptibility test results for antimicrobial drugs used in local hospitals and practice areas to the physician as periodic reports that describe the susceptibility profile of nosocomial and community- acquired pathogens. These reports should aid the physician in selecting the most effective antimicrobial.
Dilution techniques: Quantitative methods are used to determine antimicrobial minimum inhibitory concentrations (MICs). These MICs provide estimates of the susceptibility of bacteria to antimicrobial compounds. The MICs should be determined using a standardized procedure. Standardized procedures are based on a dilution method1,3 (broth or agar) or equivalent with standardized inoculum concentrations and standardized concentrations of meropenem powder. The MIC values should be interpreted according to the criteria provided in Table below.
Diffusion techniques: Quantitative methods that require measurement of zone diameters also provide reproducible estimates of the susceptibility of bacteria to antimicrobial compounds. One such standardized procedure requires the use of standardized inoculum concentrations. This procedure uses paper disks impregnated with 10-µg of meropenem to test the susceptibility of microorganisms to meropenem. The disk diffusion interpretive criteria are provided in Table below. Streptococcus pneumoniae isolates should be tested using 1-µg/mL oxacillin disk. Isolates with oxacillin zone sizes of ≥ 20 mm are susceptible (MIC ≤ 0.06 µg/mL) to penicillin and can be considered susceptible to meropenem for approved indications, and meropenem need not be tested. A meropenem MIC should be determined on isolates of S. pneumoniae with oxacillin zone sizes of ≤19 mm. The disk test does not distinguish penicillin intermediate isolates (i.e., MICs = 0.12-1.0 µg/mL) from isolates that are penicillin resistant (i.e., MICs ≥ 2 µg/mL). Viridans group streptococci should be tested for meropenem susceptibility using an MIC method. Reliable disk diffusion tests for meropenem do not yet exist for testing streptococci.
anaerobic techniques: For [[anaerobic]] bacteria, the susceptibility to meropenem as MICs can be determined by standardized test methods.The MIC values obtained should be interpreted according to the criteria provided in Table below.
 |
No interpretative criteria have been established for testing enterococci and Neisseria meningitidis.
A report of Susceptible indicates that the antimicrobial is likely to inhibit growth of the pathogen if the antimicrobial compound in the blood reaches the concentrations usually achievable. A report of Intermediate indicates that the result should be considered equivocal, and, if the microorganism is not fully susceptible to alternative, clinically feasible drugs, the test should be repeated. This category implies possible clinical applicability in body sites where the drug is physiologically concentrated or in situations where a high dosage of drug can be used. This category also provides a buffer zone that prevents small uncontrolled technical factors from causing major discrepancies in interpretation. A report of Resistant indicates that the antimicrobial is not likely to inhibit growth of the pathogen if the ntimicrobial compound in the blood reaches the concentrations usually achievable; other therapy should be selected.
Quality control: Standardized susceptibility test procedures require the use of quality control microorganisms to control the technical aspects of the test procedures. Standard meropenem powder should provide the following range of values noted in Table below.
 |
References
- ↑ "http://www.accessdata.fda.gov/drugsatfda_docs/label/2008/050706s022lbl.pdf" (PDF). External link in
|title=(help)
Adapted from the FDA Package Insert.