Atrioventricular block: Difference between revisions
No edit summary |
|||
| Line 1: | Line 1: | ||
__NOTOC__ | |||
{{Infobox_Disease | | {{Infobox_Disease | | ||
Name = {{PAGENAME}} | | Name = {{PAGENAME}} | | ||
| Line 13: | Line 14: | ||
MeshID = D006327 | | MeshID = D006327 | | ||
}} | }} | ||
{{ | {{Atrioventricular block}} | ||
{{CMG}} | {{CMG}} | ||
Revision as of 12:38, 27 August 2012
| Atrioventricular block | |
| ICD-10 | I44.0-I44.3 |
|---|---|
| ICD-9 | 426.0-426.1 |
| MeSH | D006327 |
|
Atrioventricular block Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Atrioventricular block On the Web |
|
American Roentgen Ray Society Images of Atrioventricular block |
|
Risk calculators and risk factors for Atrioventricular block |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Synonyms and keywords: AV block
Overview
An atrioventricular block (or AV block) is a type of heart block involving an impairment of the conduction between the atria and ventricles of the heart.[1] It usually involves the atrioventricular node, but it can involve other structures too. Atrioventricular (AV) block is caused by one of the following mechanisms i.e. fibrosis or degeneration of the conduction system, ischemic heart disease, or medications. AV block is categorized by degree and site of conduction block. In first-degree AV block, all atrial impulses are conducted to the ventricle. However, there is a delay within the AV node, resulting in a prolonged PR interval on ECG (>200 msec or >5 small blocks). Second-degree AV block can be of one of the two types: Mobitz I and Mobitz II. Mobitz I, or Wenckebach block , consists of progressive prolongation of PR interval, until loss of conduction to the ventricle occurs (missed beat). Mobitz I block is rarely symptomatic and does not require treatment. On the other hand, Mobitz II AV block is characterized by a constant PR interval with intermittent missed beats. The missed beats can occur with varying frequency such as occasional to 3:1 or 2:1. Complete heart block (third-degree heart block) is characterized by a complete lack of conduction from the atria to the ventricles. The ventricular rates in complete heart blocks are slower than the atrial rate. A junctional escape rate is generally between 40 and 60 beats/min and shows narrow QRS complex on EKG, whereas a ventricular escape rate is slower with a wide QRS complex. Treatment involves addressing the reversible causes such as withholding medications, treatment of ischemia, antibiotics treatment for lyme disease. A permanent pacemaker is indicated for symptomatic bradycardia due to advanced second- or third-degree heart blocks.
Classification
- First Degree AV Block
- Prolongation of PR interval
- Second Degree AV Block also known as Mobitz I and Mobitz II
- Type I AV Block (Wenchebach)
- Progressive prolongation of the PR interval before dropped beat.
- Usually block is in the AV node
- Type II AV Block
- No change in PR interval before dropped beat
- Usually infranodal
- Type I AV Block (Wenchebach)
- Third Degree AV Block also known as complete heart block
- No relationship between Atrial and ventricular activity.
Pathophysiology
Intrinsic Etiology
- Congenital
- Degenerative (Lev’s and Lenegre’s)
- Ischemia
- Infiltrative (Sarcoidosis, Amyloidosis, Hemochromatosis)
- Inflammatory (systemic lupus erythematosus (SLE), Scleroderma, rheumatoid arthritis (RA))
- Myopathic (Myotonic Dystrophy, Erbs Palsy)
- Infectious (Lyme, Endocarditis, Chagas)
- Trauma (Valve Replacement, Line insertions)
Extrinsic Etiology
- Autonomic (Carotid hypersensitivity, situational, vasovagal)
- Medications (Beta blockers, calcium-channel blocker (CCB), Digoxin, Clonidine, antiarrhythmics)
- Hypothyroidism
- Hypothermia
- Neurologic
- Electrolytes (Hyperkalemia, Hypokalemia)
Differential Diagnosis of AV Block in General
Normal Variants
- PR prolongation can be found in 0.5% of healthy patients
- Second degree block type I may be seen in healthy patients during sleep
- Transient AV block can occur with vagal maneuvers
ST Elevation MI
In acute ST elevation MI:
- First degree block occurs in 8% to 13%
- Second degree block in 3.5% to 10%
- Complete heart block in 2.5% to 8%
Inferior ST Elevation MI
- In 90% of patients the inferior wall is supplied by the RCA which gives off a branch to the AV node
- As a rule the AV block is transient and normal function returns within a week of the acute episode
Anterior ST Elevation MI
- Incidence of second degree AV block and third degree AV block is 5 to 7%
- Block is the result of damage to the interventricular septum supplied by the LAD
- There is damage to the bundle branches either in the form of bilateral bundle branch block or trifascicular block
- RBBB, RBBB + LAHB, RBBB + LPHB or LBBB often appear before the development of AV block
- The PR is normal or minimally prolonged before the onset of second degree AV block or third degree AV block
- Although the AV block is usually transient, there is a relatively high incidence of recurrence or high-degree AV block after the acute event
- In addition to ischemia, fibrosis and calcification of the summit of the ventricular septum that involve the branching part of the bundle branches, may play a role in the genesis of the conduction defect.
- It used to be thought that CAD was the most frequent cause of chronic complete AV block, but it actually causes only 15% of cases
Degenerative Diseases
- Sclerodegenerative disease of the bundle branches first described by Lenegre
- The pathologic process is called idiopathic bilateral bundle branch fibrosis and the heart block is called primary heart block
- This is the most common cause of chronic AV block (46%)
- Lev described similar degenerative lesions, which he referred to as sclerosis of the left side of the cardiac skeleton. There is progressive fibrosis and calcification of the mitral annulus, the central fibrous body, the pars membranacea, the base of the aorta, and the summit of the muscular ventricular septum. Various portions of the His bundle or the bundle branches may be involved, resulting in AV block.
Hypertension
- Chronic AV block in patients with HTN is thought to be due to CAD or sclerosis of the left side of the cardiac skeleton exacerbated by hypertension
Diseases of the Myocardium
- Acute rheumatic fever: PR prolongation is a common (25 to 95% of cases) sign in patients with acute rheumatic fever
- Type I second degree AV block may occur, but complete AV block is uncommon
- usually transient, disappears when the patient recovers
- Amyloidosis
- Ankylosing spondylitis
- Chagas disease
- Dermatomyositis
- Dilated cardiomyopathy results in various degrees of heart block are seen in 15% of patients
- Diphtheria
- HCM: 3% of patients with HCM will develop heart block
- Hemochromatosis
- Lyme disease
- Muscular dystrophy
- Myocarditis
- Sarcoid
- Scleroderma
- SLE
- Tumors, primary and secondary
Valvular Heart Disease
- Calcific aortic stenosis may be accompanied by chronic partial or complete AV block
- There is an extension of the calcification to involve the main bundle or its bifurcation, resulting in degeneration and necrosis of the conduction tissue
- May also occur in rheumatic mitral valve disease, but is less common
- Occasionally, massive calcification of the mitral annulus as an aging process may cause AV block
- May also be seen in bacterial endocarditis, especially of the aortic valve
Drugs
- When second degree AV block is induced, it is always of the Type I variety
- When complete block occurs, the QRS complexes are narrow because the block is of the AV node
- The ventricular response rate is more rapid than that due to organic lesions, and increased automaticity of the AV junctional pacemaker may be responsible.
- Quinidine and Procainamide may produce slight prolongation of the PR
- β blockers may cause AV block
- Diltiazem and verapamil may cause AV conduction delay and PR interval prolongation
Congenital
- Occurs in the absence of other evidence of organic heart disease
- Site is usually proximal to the bifurcation of the His bundle, most often in the AV node
- Narrow QRS with a rate > 40 beats per minute
- Frequently seen in those with corrected transposition of the great vessels, and occasionally in ASDs and Ebstein's anomaly
Trauma
- May be induced during open heart surgery in the area of AV conduction tissue
- Seen in patients operated on for the correction of VSD, tetralogy of Fallot, and endocardial cushion defect.
- May be due to edema, transient ischemia, or actual disruption of the conduction tissue. The block may therefore be permanent or transient.
- Also reported with both penetrating and non-penetrating trauma of the chest
Treatment
- Remove extrinsic causes
- Treat reversible intrinsic causes
Pharmacotherapy
Acute Pharmacotherapies
- Pharmacologic interventions (Atropine, Isoproterenol, Theophylline)
Surgery and Device Based Therapy
- Temporary Pacing
- Permant Pacing
Indications for Surgery and Device Based Therapy
Indications for Permanent Pacemaker in Acquired Atrioventricular Block in Adults (AHA, 1998)
- Class I
- Third-degree AV block plus:
- Symptoms related to bradycardia
- Arrhythmia or other condition requiring nodal blockers
- Asystole > 3 seconds (while awake), ventricular rate <40
- Neuromeuscular disease
- Second Degree AV block plus:
- Symptomatic Bradycardia
- Third-degree AV block plus:
- Class II
- Asymptomatic Third-degree AV Block with HR >40
- Asymptomatic Type II, second-degreee AV Block
- Asymptomatic Type I, second-degree AV Block (with wide complex)
- Class III
- Asymptomatic Type I, second-degree AV block (with narrow complex)
ACC / AHA Guidelines- Recommendations for Acquired Atrioventricular Block in Adults (DO NOT EDIT) [2]
| “ |
Class I1. Permanent pacemaker implantation is indicated for third-degree and advanced second-degree AV block at any anatomic level associated with bradycardia with symptoms (including heart failure) or ventricular arrhythmias presumed to be due to AV block. (Level of Evidence: C) 2. Permanent pacemaker implantation is indicated for third-degree and advanced second-degree AV block at any anatomic level associated with arrhythmias and other medical conditions that require drug therapy that results in symptomatic bradycardia. (Level of Evidence: C) 3. Permanent pacemaker implantation is indicated for third-degree and advanced second-degree AV block at any anatomic level in awake, symptom-free patients in sinus rhythm, with documented periods of asystole greater than or equal to 3.0 seconds86 or any escape rate less than 40 bpm, or with an escape rhythm that is below the AV node. (Level of Evidence: C) 4. Permanent pacemaker implantation is indicated for third-degree and advanced second-degree AV block at any anatomic level in awake, symptom-free patients with AF and bradycardia with 1 or more pauses of at least 5 seconds or longer. (Level of Evidence: C) 5. Permanent pacemaker implantation is indicated for third-degree and advanced second-degree AV block at any anatomic level after catheter ablation of the AV junction. (Level of Evidence: C) 6. Permanent pacemaker implantation is indicated for third-degree and advanced second-degree AV block at any anatomic level associated with postoperative AV block that is not expected to resolve after cardiac surgery. (Level of Evidence: C) 7. Permanent pacemaker implantation is indicated for third-degree and advanced second-degree AV block at any anatomic level associated with neuromuscular diseases with AV block, such as myotonic muscular dystrophy, Kearns-Sayre syndrome, Erb dystrophy (limb-girdle muscular dystrophy), and peroneal muscular atrophy, with or without symptoms. (Level of Evidence: B) 8. Permanent pacemaker implantation is indicated for second-degree AV block with associated symptomatic bradycardia regardless of type or site of block. (Level of Evidence: B) 9. Permanent pacemaker implantation is indicated for asymptomatic persistent third-degree AV block at any anatomic site with average awake ventricular rates of 40 bpm or faster if cardiomegaly or LV dysfunction is present or if the site of block is below the AV node. (Level of Evidence: B) 10. Permanent pacemaker implantation is indicated for second- or third-degree AV block during exercise in the absence of myocardial ischemia. (Level of Evidence: C) Class IIa1. Permanent pacemaker implantation is reasonable for persistent third-degree AV block with an escape rate greater than 40 bpm in asymptomatic adult patients without cardiomegaly. (Level of Evidence: C) 2. Permanent pacemaker implantation is reasonable for asymptomatic second-degree AV block at intra- or infra-His levels found at electrophysiological study. (Level of Evidence: B) 3. Permanent pacemaker implantation is reasonable for first- or second-degree AV block with symptoms similar to those of pacemaker syndrome or hemodynamic compromise. (Level of Evidence: B) 4. Permanent pacemaker implantation is reasonable for asymptomatic type II second-degree AV block with a narrow QRS. When type II second-degree AV block occurs with a wide QRS, including isolated right bundle-branch block, pacing becomes a Class I recommendation. (See Section 2.1.3, “Chronic Bifascicular Block.”) (Level of Evidence: B) Class IIb1. Permanent pacemaker implantation may be considered for neuromuscular diseases such as myotonic muscular dystrophy, Erb dystrophy (limb-girdle muscular dystrophy), and peroneal muscular atrophy with any degree of AV block (including first-degree AV block), with or without symptoms, because there may be unpredictable progression of AV conduction disease. (Level of Evidence: B) 2. Permanent pacemaker implantation may be considered for AV block in the setting of drug use and/or drug toxicity when the block is expected to recur even after the drug is withdrawn. (Level of Evidence: B) Class III1. Permanent pacemaker implantation is not indicated for asymptomatic first-degree AV block. (Level of Evidence: B) (See Section 2.1.3, “Chronic Bifascicular Block.”) 2. Permanent pacemaker implantation is not indicated for asymptomatic type I second-degree AV block at the supra-His (AV node) level or that which is not known to be intra- or infra-Hisian. (Level of Evidence: C) 3. Permanent pacemaker implantation is not indicated for AV block that is expected to resolve and is unlikely to recur (e.g., drug toxicity, Lyme disease, or transient increases in vagal tone or during hypoxia in sleep apnea syndrome in the absence of symptoms). (Level of Evidence: B) |
” |
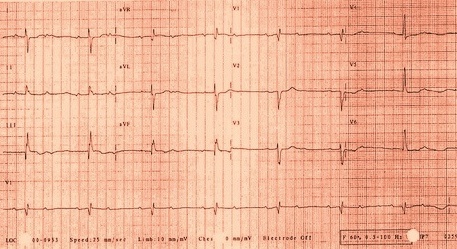
Examples
-
First degree AV block is a misnomer in that every P wave is conducted to the ventricles, however, with a PR interval exceeding 200 msec. Prolonged PR conduction, a more appropriate classification for this conduction disturbance, may be the result of conduction delay within the atrium, AV node, bundle of His or bundle branches. Prolongation of the PR interval most often indicates AV nodal conduction delay.
-
Two-to-one AV block can represent benign block within the AV node or disease of the His-Purkinje system. Certain electrocardiographic features and maneuvers can help in distinguishing where the location of block exists. A long PR interval with a narrow QRS suggests an intranodal block. A short PR interval with intraventricular conduction delay or bundle branch block suggests disease below the node. Responses to atropine, exercise and carotid sinus massage can be helpful in diagnosis. Atropine will improve AV nodal conduction but will worsen block within diseased His-Purkinje fibers. Exercise has a similar effect, improving conduction in cases where block exists only in the node, but worsening when block is subnodal. Alternatively, Carotid Sinus Massage will slow conduction when block occurs in the AV node, but will improve conduction in diseased His-Purkinje tissue by allowing for refractoriness to recover
Sources
- The ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities [2]
References
- ↑ Template:Dorlands
- ↑ Jump up to: 2.0 2.1 Epstein AE, DiMarco JP, Ellenbogen KA, Estes NAM III, Freedman RA, Gettes LS, Gillinov AM, Gregoratos G, Hammill SC, Hayes DL, Hlatky MA, Newby LK, Page RL, Schoenfeld MH, Silka MJ, Stevenson LW, Sweeney MO. ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices). Circulation. 2008; 117: 2820–2840. PMID 18483207