Acute flaccid myelitis: Difference between revisions
| Line 6: | Line 6: | ||
==Overview== | ==Overview== | ||
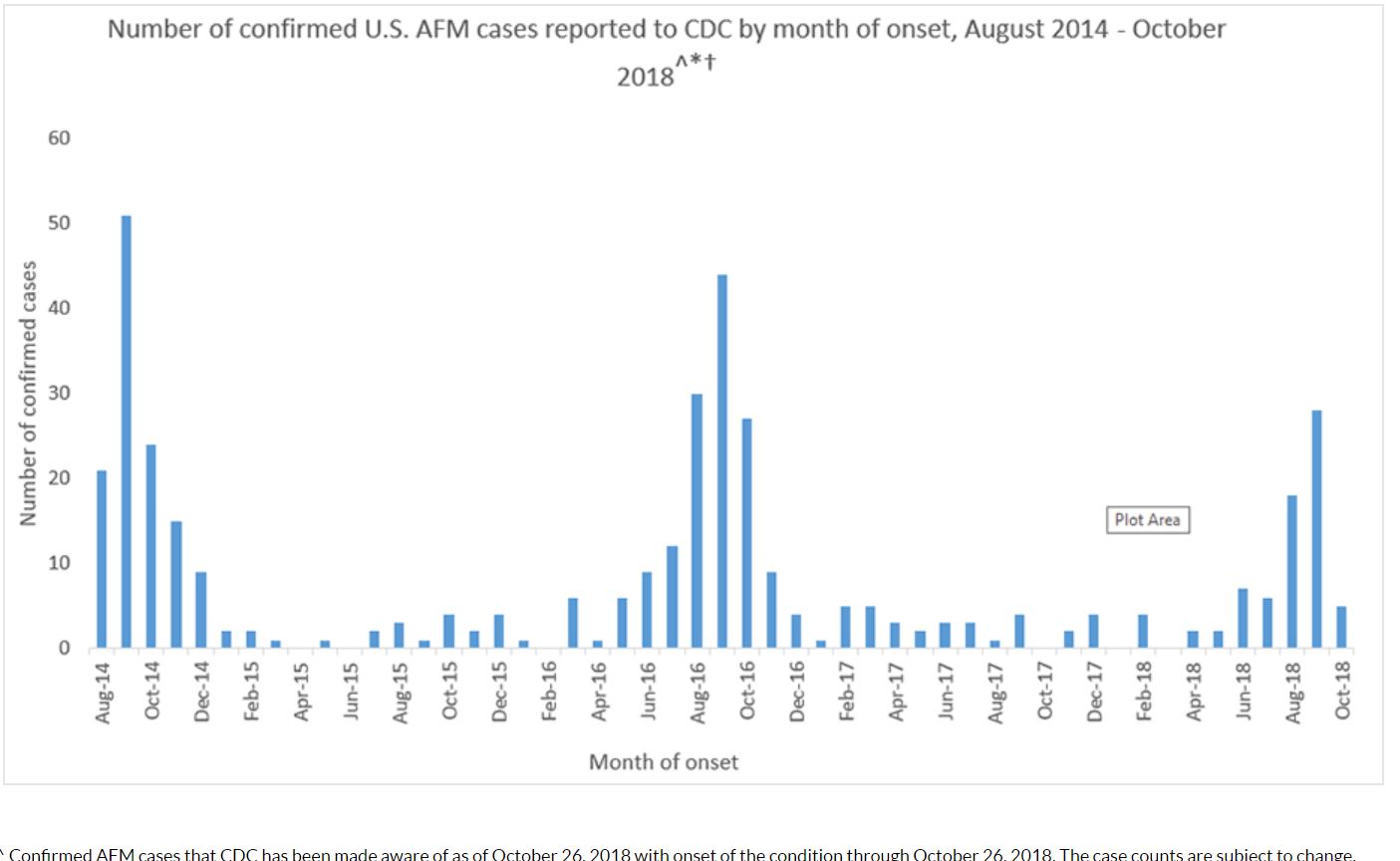
Acute flaccid myelitis (AFM) is a rare but serious neurological condition characterized by sudden onset of paralysis and weakness in extremities (lower > upper). AFM affects the area of the spinal cord called gray matter, which causes the muscles and reflexes in the body to become weak. It is typically a lower motor neuron lesion but cases have been identified where there was reported involvement of the midbrain and medulla oblangata. The risk of getting AFM varies by age and year. We have seen increases in AFM cases every two years since 2014 and mostly in young children. Still, CDC estimates that less than one to two in a million children in the United States will get AFM every year. AFM should be differentiated from other diseases which present with muscle weakness, hypotonia and flaccid paralysis. AFM has been known to be associated with viral infections such as West Nile virus, coxsackie virus, Adenovirus, Poliovirus, Enterovirus D71 and Enterovirus D68 as well as environmental toxins. The clinical course of the disease is characterized by prodormal phase, progressive neurological injury phase and convalescent phase. There is no specific treatment for AFM and prevention is aimed at measures which curtail the rate of infection by viruses known to be associated with AFM. | |||
== Historical Perspective == | == Historical Perspective == | ||
Revision as of 18:03, 20 November 2018
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Syed Hassan A. Kazmi BSc, MD [2]
Synonyms and keywords:; Acute flaccid paralysis, acute flaccid paralysis with anterior myelitis, paralysis with anterior myelitis, AFM, Enterovirus D68-Associated Anterior Myelitis
Overview
Acute flaccid myelitis (AFM) is a rare but serious neurological condition characterized by sudden onset of paralysis and weakness in extremities (lower > upper). AFM affects the area of the spinal cord called gray matter, which causes the muscles and reflexes in the body to become weak. It is typically a lower motor neuron lesion but cases have been identified where there was reported involvement of the midbrain and medulla oblangata. The risk of getting AFM varies by age and year. We have seen increases in AFM cases every two years since 2014 and mostly in young children. Still, CDC estimates that less than one to two in a million children in the United States will get AFM every year. AFM should be differentiated from other diseases which present with muscle weakness, hypotonia and flaccid paralysis. AFM has been known to be associated with viral infections such as West Nile virus, coxsackie virus, Adenovirus, Poliovirus, Enterovirus D71 and Enterovirus D68 as well as environmental toxins. The clinical course of the disease is characterized by prodormal phase, progressive neurological injury phase and convalescent phase. There is no specific treatment for AFM and prevention is aimed at measures which curtail the rate of infection by viruses known to be associated with AFM.
Historical Perspective
- In 2014, physicians in California and Colorado (USA) noted an increase in the number of patients presenting with the acute onset of flaccid paralysis and MRI findings consistent with lesions in the gray matter of the spinal cord.
- In 2014, a total of 120 cases were identified in the US and 22 were identified in 2015
- In 2016, 145 cases of AFM were diagnosed across the USA.
Causes
Acute flaccid myelitis (AFM) may be caused by viral infections or environmental toxins. The following viruses are known to be associated with AFM:
- West Nile Virus
- Coxsackievirus
- Adenovirus
- Poliovirus
- Enterovirus 71 (EV 71) and Entervirus D68 (EV 68)
Differentiating Acute Flaccid Myelitis From Other Diseases
The following table differentiates acute flaccid myelitis from other diseases that cause muscle weakness, hypotonia, and flaccid paralysis:
| Diseases | History and Physical | Diagnostic tests | Other Findings | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Motor Deficit | Sensory deficit | Cranial nerve Involvement | Autonomic dysfunction | Proximal/Distal/Generalized | Ascending/Descending/Systemic | Unilateral (UL)
or Bilateral (BL) or No Lateralization (NL) |
Onset | Lab or Imaging Findings | Specific test | ||
| Acute Flaccid Myelitis | + | + | + | - | Proximal > Distal | Ascending | UL/BL | Sudden | MRI (Longitudinal hyperintense lesions) | MRI and CSF PCR for viral etiology | Drooping eyelids
Difficulty swallowing Respiratory failure |
| Adult Botulism | + | - | + | + | Generalized | Descending | BL | Sudden | Toxin test | Blood, Wound, or Stool culture | Diplopia, Hyporeflexia, Hypotonia, possible respiratory paralysis |
| Infant Botulism | + | - | + | + | Generalized | Descending | BL | Sudden | Toxin test | Blood, Wound, or Stool culture | Flaccid paralysis (Floppy baby syndrome), possible respiratory paralysis |
| Guillian-Barre syndrome | + | - | - | - | Generalized | Ascending | BL | Insidious | CSF: ↑Protein
↓Cells |
Clinical & Lumbar Puncture | Progressive ascending paralysis following infection, possible respiratory paralysis |
| Eaton Lambert syndrome | + | - | + | + | Generalized | Systemic | BL | Intermittent | EMG, repetitive nerve stimulation test (RNS) | Voltage gated calcium channel (VGCC) antibody | Diplopia, ptosis, improves with movement (as the day progresses) |
| Myasthenia gravis | + | - | + | + | Generalized | Systemic | BL | Intermittent | EMG, Edrophonium test | Ach receptor antibody | Diplopia, ptosis, worsening with movement (as the day progresses) |
| Electrolyte disturbance | + | + | - | - | Generalized | Systemic | BL | Insidious | Electrolyte panel | ↓Ca++, ↓Mg++, ↓K+ | Possible arrhythmia |
| Organophosphate toxicity | + | + | - | + | Generalized | Ascending | BL | Sudden | Clinical diagnosis: physical exam & history | Clinical suspicion confirmed with RBC AchE activity | History of exposure to insecticide or living in farming environment. with : Diarrhea, Urination, Miosis, Bradycardia, Lacrimation, Emesis, Salivation, Sweating |
| Tick paralysis (Dermacentor tick) | + | - | - | - | Generalized | Ascending | BL | Insidious | Clinical diagnosis: physical exam & history | - | History of outdoor activity in Northeastern United States. The tick is often still latched to the patient at presentation (often in head and neck area) |
| Tetrodotoxin poisoning | + | - | + | + | Generalized | Systemic | BL | Sudden | Clinical diagnosis: physical exam & dietary history | - | History of consumption of puffer fish species. |
| Stroke | +/- | +/- | +/- | +/- | Generalized | Systemic | UL | Sudden | MRI +ve for ischemia or hemorrhage | MRI | Sudden unilateral motor and sensory deficit in a patient with a history of atherosclerotic risk factors (diabetes, hypertension, smoking) or atrial fibrillation. |
| Poliomyelitis | + | + | + | +/- | Proximal > Distal | Systemic | BL or UL | Sudden | PCR of CSF | Asymmetric paralysis following a flu-like syndrome. | |
| Transverse myelitis | + | + | + | + | Proximal > Distal | Systemic | BL or UL | Sudden | MRI & Lumbar puncture | MRI | History of chronic viral or autoimmune disease (e.g. HIV) |
| Neurosyphilis | + | + | - | +/- | Generalized | Systemic | BL | Insidious | MRI & Lumbar puncture | CSF VDRL-specifc
CSF FTA-Ab -sensitive |
History of unprotected sex or multiple sexual partners.
History of genital ulcer (chancre), diffuse maculopapular rash. |
| Muscular dystrophy | + | - | - | - | Proximal > Distal | Systemic | BL | Insidious | Genetic testing | Muscle biopsy | Progressive proximal lower limb weakness with calf pseudohypertrophy in early childhood. Gower sign positive. |
| Multiple sclerosis exacerbation | + | + | + | + | Generalized | Systemic | NL | Sudden | ↑CSF IgG levels
(monoclonal) |
Clinical assessment and MRI | Blurry vision, urinary incontinence, fatigue |
| Amyotrophic lateral sclerosis | + | - | - | - | Generalized | Systemic | BL | Insidious | Normal LP (to rule out DDx) | MRI & LP | Patient initially presents with upper motor neuron deficit (spasticity) followed by lower motor neuron deficit (flaccidity). |
| Inflammatory myopathy | + | - | - | - | Proximal > Distal | Systemic | UL or BL | Insidious | Elevated CK & Aldolase | Muscle biopsy | Progressive proximal muscle weakness in 3rd to 5th decade of life. With or without skin manifestations. |
Epidemiology and Demographics
Incidence and Prevalence
USA
- From June 1, 2012 to July 31, 2015, 59 reported cases met the California Department of Public Health (CDPH) case definition of acute flaccid myelitis (AFM), which defines AFM as acute onset of flaccid limb paralysis along with a lesion in the gray matter of the spinal cord.
- Between August and December of 2014, 120 children from 34 US states met the criteria of AFM as outlined by the CDC.
- From August 2014 through October 2018, CDC has received information on a total of 404 confirmed cases of acute flaccid myelitis (AFM) across the US; most of the cases have occurred in children
- In 2015, 22 people were confirmed to have AFM. (Note: The cases occurred in 17 states across the U.S.)
- In 2016, 149 people were confirmed to have AFM. (Note: The cases occurred in 39 states across the U.S. and DC)
- In 2017, CDC received information for 33 confirmed cases of AFM. (Note: The cases occurred in 16 states across the U.S.)
- In October 2018, the New York State Department of Health (NYSDOH) confirmed 39 cases of the enterovirus EV-D68 in children across the state which was associated with an increase in number of cases of AFM.
Age
- AFM affects older children. Median age at presentation is 7 years.
Gender
- Male children are affected more frequently than females.
Risk Factors
The following risk factors increase the risk of development of AFM:
- Pulmonary comorbities (Asthma, COPD)
- Immunocompromised states (Immunosuppressants, organ transplantation, diabetes, systemic autoimmune diseases, hematologic malignancies)
Natural History, Complications and Prognosis
Natural History
- The clinical course of AFM typically consists of three phases:
- Prodormal phase
- Progressive neurological injury phase
- Convalescent phase
Prodormal phase
- A prodromal, often febrile, illness often precedes the onset of neurological deficits in most patients by a median of 5 days.
- The prodormal period consists of respiratory symptoms such as rhinorrhea, cough, or pharyngitis and/or gastrotestinal symptoms such as nausea, vomiting or diarrhea.
- Some patients report clinical improvement in their preceding illness before return of fever accompanied by headaches, stiff neck, or pain in the neck, back, or affected limb around the time of neurological deficit onset
Progressive neurological injury
- The pattern of limb weakness in AFM corresponds to a lower motor neuron lesion and upper extremities are more commonly affected.
- Involvement of cranial nerves points towards lesions in the cranial nerve motor nuclei of the brainstem
- On CSF examination, mild pleocytosis with mildly elevated protein may be seen
- On MRI, confluent, longitudinally extensive gray matter lesions may be seen in spinal cord. This may progress to nerve root enhancement on MRI in 2-3 weeks.
- On electromyography (EMG), reduced recruitment of motor unit potentials (MUPs) and low amplitude of compound muscle action potentials may be seen.
Convalescent phase
- Months after the initial acute neurological illness, patients suffering from AFM may smild improvements with rehabilitation therapies.
- On CSF examination, pleocytosis may resolve and protein remains elevated
- On EMG, fibrillations may be seen
Complications
AFM may lead to the development of following complications:
- Respiratory failure
- Urinary tract infections
- Skin ulcers and traumatic injury (specially in the affected extremity)
- Progressive muscular atrophy
Prognosis
- Physical and occupational therapy are especially important during recovery from AFM
- The extent of recovery varies. Although some people may make a full recovery, most have continued muscle weakness even after a year.
- Long term outcomes for patients suffering from AFM are not known.
Diagnosis
Diagnostic Criteria
| Diagnosis | Criteria |
|---|---|
| Confirmed |
AND
|
| Probable |
AND
|
Symptoms
The following are the symptoms of acute flaccid myelitis:
- Acute onset of flaccid limb paralysis (asymmetric)
- Fever
- Pain in the paralytic limb
- Eyelid drooping
- Difficulty with swallowing or slurred speech
- Cranial nerve abnormalities
- Headache
- Neck pain
- Bowel/bladder changes
Physical Examination
Temperature
- A fever is often present
Extremities
- Weakness of the extremities, predominantly of the proximal muscles, is characteristic of this form of the disease. Lower extremities are more often involved.
- Asymmetrical flaccid paralysis, predominantly of the proximal muscles, is characteristic of this form of the disease. Lower extremities are more often involved.
Neurologic
- Meningeal signs may be present on physical exam, such as:
- Initially hyperactive deep tendon reflexes, that later become absent.
- Common combinations of limb involvement include:
- One lower limb, followed by one upper limb
- Both lower limbs, followed by both upper limbs
- Quadriplegia is a rare finding in infants.
Laboratory Findings
Non specific tests
Blood tests
It is performed routinely to any suspected meningitis patients. It includes the following:
Virus detection
Virus may be detected through two ways:
- Samples can be taken by different ways from the suspected meningitis patients to detect the virus causing the disease.They may be collected for testing by:
- Polymerase Chain Reaction (PCR) can be used to detect the viruses in the blood. It can detect the DNA of the viruses like the enteroviruses and herpes simplex viruses.
Specific tests
Specific diagnostic tests include lumbar puncture with CSF examination. CSF examination findings in viral meningitis are as follows:
| Cerebrospinal fluid level | Normal level | Viral meningitis |
|---|---|---|
| Cells/ul | < 5 | >100 |
| Cells | Lymphos:Monos 7:3 | Lymphocytes>granulocytes |
| Total protein (mg/dl) | 45-60 | Normal or slightly elevated |
| Glucose ratio (CSF/plasma) | > 0.5 | >0.6 |
| Lactate (mmols/l) | < 2.1 | < 2.1 |
| Others | ICP:6-12 (cm H2O) | Throat swap |
Video explaining the lumbar puncture procedure: {{#ev:youtube|weoY_9tOcJQ}}
Imaging Findings
Magnetic resonance imaging (MRI) may reveal the following findings in patients suffering from AFM:
- Longitudinal hyperintense gray matter lesions in the spinal cord (may span more than 1 spinal segments).
- Hyperintense brainstem lesions ranging from midbrain to medulla oblongata.
Treatment
Medical Therapy
- There is no specific treatment for AFM.
- Treatments that have been tried include:
- Immunoglobulin (IVIG)
- Plasma exchange
- Physiotherapy
- Occupational therapy
- There is no clear evidence that any of these treatments affect recovery. The extent of recovery varies. Although some people may make a full recovery, most have continued muscle weakness even after a year.
Prevention
- There is no specific action to take to prevent AFM.
- Certain viruses are known to cause AFM including enteroviruses, such as poliovirus and enterovirus A71 (EV-A71), and West Nile virus.
- Poliovirus infection can be prevented by getting vaccinated. Polio vaccine contains inactivated (not live) virus, and protects against poliovirus. This vaccine does not protect against other viruses that may cause AFM.
- Protection from mosquito bites, which can carry West Nile virus, can be achieved by using mosquito repellent, staying indoors at dusk and dawn (when bites are more common), and removing standing or stagnant water (where mosquitoes can breed).
- Protection from enteroviruses by washing hands often with soap and water, avoiding close contact with people who are sick, and cleaning and disinfecting frequently touched surfaces, including toys.