Osteoarthritis overview: Difference between revisions
No edit summary |
|||
| Line 20: | Line 20: | ||
Osteoarthritis is radiographically classified depending on the degree of joint involvement. The Kellgren-Lawrence is a common method to classify the severity of OA in the knee using five different grades. This classification was proposed by Kellgren et al. in 1957 and was then accepted by WHO in 1961. | Osteoarthritis is radiographically classified depending on the degree of joint involvement. The Kellgren-Lawrence is a common method to classify the severity of OA in the knee using five different grades. This classification was proposed by Kellgren et al. in 1957 and was then accepted by WHO in 1961. | ||
==Pathophysiology== | ==Pathophysiology== | ||
Revision as of 20:26, 16 June 2018
| https://https://www.youtube.com/watch?v=sUOlmI-naFs%7C350}} |
|
Osteoarthritis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Osteoarthritis overview On the Web |
|
American Roentgen Ray Society Images of Osteoarthritis overview |
|
Risk calculators and risk factors for Osteoarthritis overview |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mohammadmain Rezazadehsaatlou, Irfan Dotani
Overview
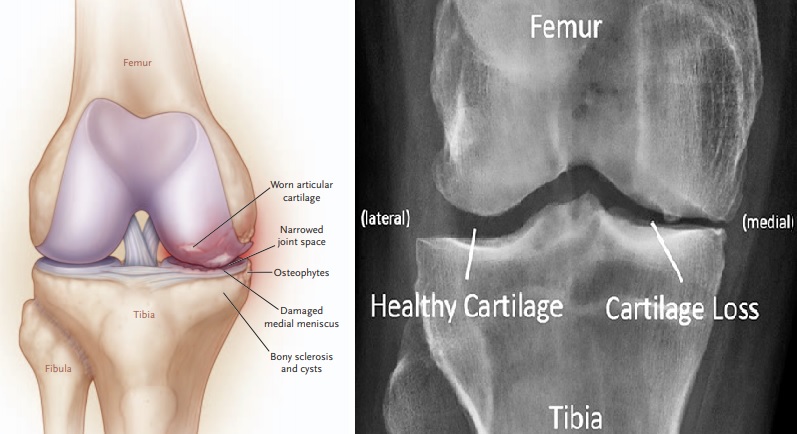
Osteoarthritis / Osteoarthrosis (OA, also known as degenerative joint disease, degenerative arthritis, arthrosis or in more colloquial terms "wear and tear") is the most common form of arthritis, caused by wearing of the cartilage that covers and cushions joint spaces. As the cartilage wears away, the patient may experience pain described as "weight-bearing" whenever walking and standing. Due to the movement limitations caused by pain, regional muscles may experience atrophy. Ligaments may become laxer as well due to this. OA is derived from the Greek word "osteo", meaning "of the bone", "arthro", meaning "joint", and "itis", meaning inflammation, although inflammation is not a common finding in this regard. OA possesses a great degree of variability in disease onset, progression, and severity. OA is characterized by a variety of structural and functional impairments occurring in an involved joint. Destruction, degeneration, articular cartilage loss, and even the soft tissue involvement are the main pathological process of this disease. It can be diagnosed through radiographic evaluations. Moreover, clinical sign and symptoms are helpful in the final diagnosis of this disease. OA can be defined radiologically, clinically, or pathologically, with radiographic OA being considered as the reference standard.[5] The symptoms that are consistently associated with OA are joint pain, stiffness, swelling, and limitation of joint function. Few individuals who present these symptoms may not demonstrate radiographic OA. However, others confirmed to have OA using radiographic techniques may not present with clinical manifestations of the disease.[5] These unique characteristics have made it difficult to identify the underlying mechanisms contributing to the disease as well as the treatments for reducing the incidence and severity of the disease. In addition, the stimuli that may initiate the processes associated with OA are multifactorial and include occupational and non-occupational (e.g., genetics, obesity, age, etc.) factors. OA affects nearly 43 million patients in United States and almost 15% of the world population, accounting for 25% of visits to primary care physicians, and half of all NSAID (Non-Steroidal Anti-Inflammatory Drugs) prescriptions. It is estimated that 80% of the population will have radiographic evidence of OA by age 65, although only 60% of those will be symptomatic.[1] There is no recent discovery of a cure for OA, as cartilage has not been induced to regenerate. However, if OA is caused by cartilage damage (for example as a result of an injury) Autologous Chondrocyte Implantation may be a possible treatment. Other treatments are with NSAIDs, local injections of glucocorticoid or hyaluronan, and in severe cases, with joint replacement surgery. Many physicians have also reported good pain relief by treating ligaments (which is responsible for a bone to bone connection) with Prolotherapy. Clinical trials employing tissue-engineering methods have demonstrated regeneration of cartilage in damaged knees, including those that have progressed to osteoarthritis.[2] Furthermore, in January 2007, Johns Hopkins University was offering to license a technology of this kind, listing several clinical competitors in its market analysis. Osteoarthritis is capable of influencing any joint in the human body; meanwhile, the most commonly affected joints are the knee and hip joints given that the degree of weight bearing required of these joints is immense. Other joints, such as the distal interphalangeal joints of the fingers and shoulder joints are also commonly affected as well. The economic burden of OA for United States economy is more than $60 billion per year; which has more economic pressure than rheumatoid arthritis. This cost can be considered into two subgroups: the medical related costs and the lost expediency of patients at work.
Historical Perspective
The earliest descriptions of OA were provided by Heberden and Haygarth in the 19th century. [3] [4] In the 1930s and 1940s, Dr. Stecher showed that there were two forms of OA: idiopathic and post-traumatic. [5] In the 1950s, the connection between Heberden’s nodes and large joint OA were revealed by Kellgren and Moore. In this regard, the first x-ray grading system for OA was developed by Jonas Kellgren and John Lawrence in the 1950s. Surgical management of OA was developed in the 1960s by Drs. Charnley and McKee.
Classification
Osteoarthritis is radiographically classified depending on the degree of joint involvement. The Kellgren-Lawrence is a common method to classify the severity of OA in the knee using five different grades. This classification was proposed by Kellgren et al. in 1957 and was then accepted by WHO in 1961.
Pathophysiology
Causes
Differentiating Osteoarthritis overview from Other Diseases
Epidemiology and Demographics
Risk Factors
Screening
Routine screening for osteoarthritis is not indicated unless the patient is symptomatic.