Sandbox:Cherry: Difference between revisions
No edit summary |
(→Table) |
||
| Line 54: | Line 54: | ||
* Ingestion of [[corrosive|corrosives]] | * Ingestion of [[corrosive|corrosives]] | ||
| | | | ||
* [[Epigastric pain]] | |||
* [[ | |||
|Food | |Food | ||
|- | |- | ||
| Line 78: | Line 60: | ||
|✔ | |✔ | ||
|✔ | |✔ | ||
| | |<nowiki>✔</nowiki> | ||
|✔ | |✔ | ||
|[[Melena|Black stools]] in case of | |[[Melena|Black stools]] in case of Peptic Ulcer Disease | ||
| | | | ||
*Helps in the determination of site of [[obstruction]] | *Helps in the determination of site of [[obstruction]] | ||
Revision as of 17:28, 25 January 2018
Pathophysiology prev
| https://https://www.youtube.com/watch?v=5szNmKtyBW4%7C350}} |
|
Cirrhosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case studies |
|
Sandbox:Cherry On the Web |
|
American Roentgen Ray Society Images of Sandbox:Cherry |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief:
Table
| Disease | Cause | Symptoms | Diagnosis | Other findings | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pain | Nausea
& Vomiting |
Heartburn | Belching or
Bloating |
Weight loss | Loss of
Appetite |
Stools | Endoscopy findings | |||||
| Location | Aggravating Factors | Alleviating Factors | ||||||||||
| Gastric outlet obstruction |
|
Food | ||||||||||
| ✔ | ✔ | ✔ | ✔ | ✔ | Black stools in case of Peptic Ulcer Disease |
|
- | |||||
| Acute gastritis |
|
Food | Antacids | ✔ | ✔ | ✔ | - | ✔ | Black stools | - | ||
| Chronic gastritis |
|
Food | Antacids | ✔ | ✔ | ✔ | ✔ | ✔ | - | H. pylori gastritis
Lymphocytic gastritis
|
- | |
| Atrophic gastritis | Epigastric pain | - | - | ✔ | - | ✔ | ✔ | - | H. pylori
|
Autoimmune gastritis diagnosis include:
| ||
| Crohn's disease | - | - | - | - | - | ✔ | ✔ |
|
|
|||
| GERD |
|
|
|
✔
(Suspect delayed gastric emptying) |
✔ | - | - | - | - |
|
Other symptoms:
Complications
| |
| Peptic ulcer disease |
|
|
|
|
✔ | ✔ | - | - | - | Gastric ulcers
Duodenal ulcers
|
Other diagnostic tests | |
| Gastrinoma |
|
- | - | ✔
(suspect gastric outlet obstruction) |
✔ | - | - | - | Useful in collecting the tissue for biopsy |
Diagnostic tests
| ||
| Gastric Adenocarcinoma |
|
- | - | ✔ | ✔ | ✔ | ✔ | ✔ |
|
Esophagogastroduodenoscopy
|
Other symptoms | |
| Primary gastric lymphoma |
|
- | - | - | - | - | ✔ | - | - | Useful in collecting the tissue for biopsy | Other symptoms
| |
Video codes
Normal video
{{#ev:youtube|x6e9Pk6inYI}} {{#ev:youtube|4uSSvD1BAHg}} {{#ev:youtube|PQXb5D-5UZw}}
Video in table
Floating video
| Title |
| https://https://www.youtube.com/watch?v=ypYI_lmLD7g%7C350}} |
Redirect
- REDIRECTEsophageal web
synonym website
https://mq.b2i.sg/snow-owl/#!terminology/snomed/10743008
Image
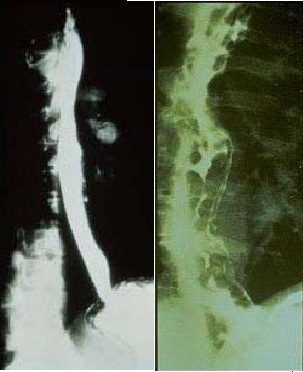
Image to the right
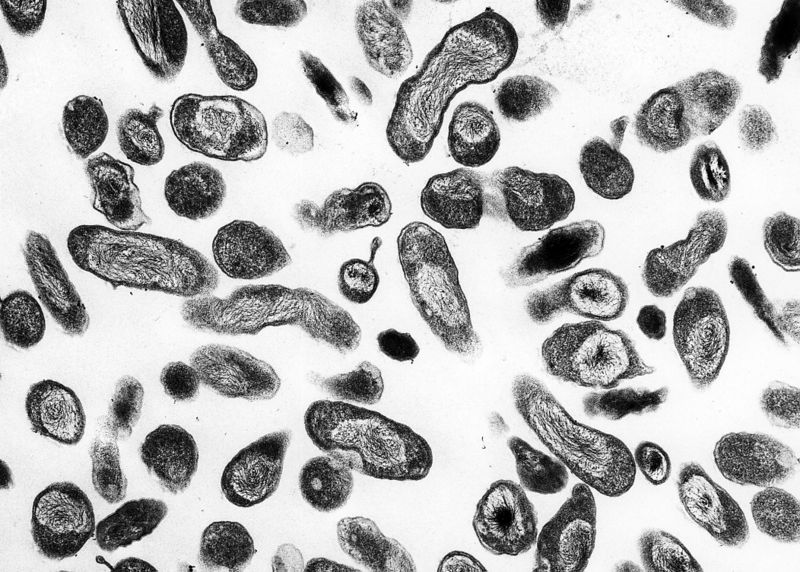 |
Image and text to the right
<figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline>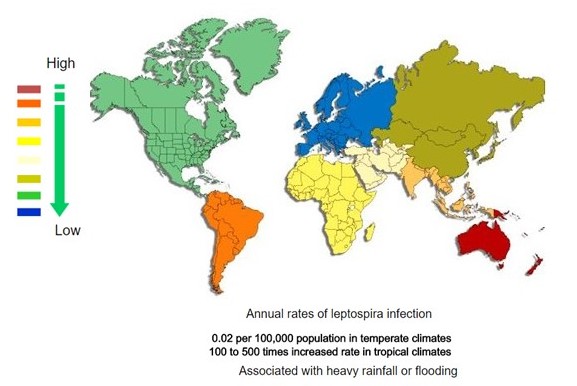 </figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline> Recent out break of leptospirosis is reported in Bronx, New York and found 3 cases in the months January and February, 2017.
</figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline> Recent out break of leptospirosis is reported in Bronx, New York and found 3 cases in the months January and February, 2017.
Gallery
-
Histopathology of a pancreatic endocrine tumor (insulinoma). Source:https://librepathology.org/wiki/Neuroendocrine_tumour_of_the_pancreas[34]
-
Histopathology of a pancreatic endocrine tumor (insulinoma). Chromogranin A immunostain. Source:https://librepathology.org/wiki/Neuroendocrine_tumour_of_the_pancreas[34]
-
Histopathology of a pancreatic endocrine tumor (insulinoma). Insulin immunostain. Source:https://librepathology.org/wiki/Neuroendocrine_tumour_of_the_pancreas[34]
References
- ↑ Miner PB, Harri JE, McPhee MS (1982). "Intermittent gastric outlet obstruction from a pedunculated gastric polyp". Gastrointest. Endosc. 28 (3): 219–20. PMID 7129059.
- ↑ Gencosmanoglu R, Sen-Oran E, Kurtkaya-Yapicier O, Tozun N (2003). "Antral hyperplastic polyp causing intermittent gastric outlet obstruction: case report". BMC Gastroenterol. 3: 16. doi:10.1186/1471-230X-3-16. PMC 166166. PMID 12831404.
- ↑ Zargar SA, Kochhar R, Nagi B, Mehta S, Mehta SK (1989). "Ingestion of corrosive acids. Spectrum of injury to upper gastrointestinal tract and natural history". Gastroenterology. 97 (3): 702–7. PMID 2753330.
- ↑ Taylor SM, Adams DB, Anderson MC (1991). "Duodenal stricture: a complication of chronic fibrocalcific pancreatitis". South. Med. J. 84 (3): 338–41. PMID 2000520.
- ↑ Menke DM, Kyle RA, Fleming CR, Wolfe JT, Kurtin PJ, Oldenburg WA (1993). "Symptomatic gastric amyloidosis in patients with primary systemic amyloidosis". Mayo Clin. Proc. 68 (8): 763–7. PMID 8331978.
- ↑ Friedman S, Janowitz HD (1998). "Systemic amyloidosis and the gastrointestinal tract". Gastroenterol. Clin. North Am. 27 (3): 595–614, vi. PMID 9891699.
- ↑ Khan S, Orenstein SR (2000). "Eosinophilic gastroenteritis masquerading as pyloric stenosis". Clin Pediatr (Phila). 39 (1): 55–7. doi:10.1177/000992280003900109. PMID 10660821.
- ↑ Chaudhary R, Shrivastava RK, Mukhopadhyay HG, Diwan RN, Das AK (2001). "Eosinophilic gastritis--an unusual cause of gastric outlet obstruction". Indian J Gastroenterol. 20 (3): 110. PMID 11400803.
- ↑ Tursi A, Rella G, Inchingolo CD, Maiorano M (2007). "Gastric outlet obstruction due to gastroduodenal eosinophilic gastroenteritis". Endoscopy. 39 Suppl 1: E184. doi:10.1055/s-2006-945125. PMID 17614041.
- ↑ Chen MJ, Chu CH, Lin SC, Shih SC, Wang TE (2003). "Eosinophilic gastroenteritis: clinical experience with 15 patients". World J. Gastroenterol. 9 (12): 2813–6. PMC 4612059. PMID 14669340.
- ↑ Lee CM, Changchien CS, Chen PC, Lin DY, Sheen IS, Wang CS, Tai DI, Sheen-Chen SM, Chen WJ, Wu CS (1993). "Eosinophilic gastroenteritis: 10 years experience". Am. J. Gastroenterol. 88 (1): 70–4. PMID 8420276.
- ↑ Aranha GV, Prinz RA, Greenlee HB, Freeark RJ (1984). "Gastric outlet and duodenal obstruction from inflammatory pancreatic disease". Arch Surg. 119 (7): 833–5. PMID 6732492.
- ↑ Agrawal NM, Gyr N, McDowell W, Font RG (1974). "Intestinal obstruction due to acute pancreatitis. Case report and review of literature". Am J Dig Dis. 19 (2): 179–85. PMID 4811173.
- ↑ Bradley EL (1989). "Complications of chronic pancreatitis". Surg. Clin. North Am. 69 (3): 481–97. PMID 2658160.
- ↑ Levenick JM, Gordon SR, Sutton JE, Suriawinata A, Gardner TB (2009). "A comprehensive, case-based review of groove pancreatitis". Pancreas. 38 (6): e169–75. doi:10.1097/MPA.0b013e3181ac73f1. PMID 19629001.
- ↑ Stampfl DA, Grimm IS, Barbot DJ, Rosato FE, Gordon SJ (1990). "Sarcoidosis causing duodenal obstruction. Case report and review of gastrointestinal manifestations". Dig. Dis. Sci. 35 (4): 526–32. PMID 2180656.
- ↑ Johnson FE, Humbert JR, Kuzela DC, Todd JK, Lilly JR (1975). "Gastric outlet obstruction due to X-linked chronic granulomatous disease". Surgery. 78 (2): 217–23. PMID 807981.
- ↑ Mulholland MW, Delaney JP, Simmons RL (1983). "Gastrointestinal complications of chronic granulomatous disease: surgical implications". Surgery. 94 (4): 569–75. PMID 6623357.
- ↑ Huang A, Abbasakoor F, Vaizey CJ (2006). "Gastrointestinal manifestations of chronic granulomatous disease". Colorectal Dis. 8 (8): 637–44. doi:10.1111/j.1463-1318.2006.01030.x. PMID 16970572.
- ↑ Bakken DA, Abramo TJ (1997). "Gastric lactobezoar: a rare cause of gastric outlet obstruction". Pediatr Emerg Care. 13 (4): 264–7. PMID 9291515.
- ↑ De Backer A, Van Nooten V, Vandenplas Y (1999). "Huge gastric trichobezoar in a 10-year-old girl: case report with emphasis on endoscopy in diagnosis and therapy". J. Pediatr. Gastroenterol. Nutr. 28 (5): 513–5. PMID 10328129.
- ↑ Phillips MR, Zaheer S, Drugas GT (1998). "Gastric trichobezoar: case report and literature review". Mayo Clin. Proc. 73 (7): 653–6. doi:10.1016/S0025-6196(11)64889-1. PMID 9663194.
- ↑ White NB, Gibbs KE, Goodwin A, Teixeira J (2003). "Gastric bezoar complicating laparoscopic adjustable gastric banding, and review of literature". Obes Surg. 13 (6): 948–50. doi:10.1381/096089203322618849. PMID 14738689.
- ↑ Zapata R, Castillo F, Córdova A (2006). "[Gastric food bezoar as a complication of bariatric surgery. Case report and review of the literature]". Gastroenterol Hepatol (in Spanish; Castilian). 29 (2): 77–80. PMID 16448609.
- ↑ Nugent FW, Roy MA (1989). "Duodenal Crohn's disease: an analysis of 89 cases". Am. J. Gastroenterol. 84 (3): 249–54. PMID 2919581.
- ↑ Kefalas CH (2003). "Gastroduodenal Crohn's disease". Proc (Bayl Univ Med Cent). 16 (2): 147–51. PMC 1201000. PMID 16278730.
- ↑ Matsui T, Hatakeyama S, Ikeda K, Yao T, Takenaka K, Sakurai T (1997). "Long-term outcome of endoscopic balloon dilation in obstructive gastroduodenal Crohn's disease". Endoscopy. 29 (7): 640–5. doi:10.1055/s-2007-1004271. PMID 9360875.
- ↑ Fitzgibbons TJ, Green G, Silberman H, Eliasoph J, Halls JM, Yellin AE (1980). "Management of Crohn's disease involving the duodenum, including duodenal cutaneous fistula". Arch Surg. 115 (9): 1022–8. PMID 6106466.
- ↑ Amarapurkar DN, Patel ND, Amarapurkar AD (2003). "Primary gastric tuberculosis--report of 5 cases". BMC Gastroenterol. 3: 6. PMC 155648. PMID 12703983.
- ↑ Rao YG, Pande GK, Sahni P, Chattopadhyay TK (2004). "Gastroduodenal tuberculosis management guidelines, based on a large experience and a review of the literature". Can J Surg. 47 (5): 364–8. PMC 3211943. PMID 15540690.
- ↑ Padussis J, Loffredo B, McAneny D (2005). "Minimally invasive management of obstructive gastroduodenal tuberculosis". Am Surg. 71 (8): 698–700. PMID 16217956.
- ↑ Di Placido R, Pietroletti R, Leardi S, Simi M (1996). "Primary gastroduodenal tuberculous infection presenting as pyloric outlet obstruction". Am. J. Gastroenterol. 91 (4): 807–8. PMID 8677960.
- ↑ Subei I, Attar B, Schmitt G, Levendoglu H (1987). "Primary gastric tuberculosis: a case report and literature review". Am. J. Gastroenterol. 82 (8): 769–72. PMID 3605037.
- ↑ 34.0 34.1 34.2 Neuroendocrine tumor of the pancreas. Libre Pathology. http://librepathology.org/wiki/index.php/Neuroendocrine_tumour_of_the_pancreas
REFERENCES
![Histopathology of a pancreatic endocrine tumor (insulinoma). Source:https://librepathology.org/wiki/Neuroendocrine_tumour_of_the_pancreas[34]](/images/2/2f/Pancreatic_insulinoma_histology_2.JPG)
![Histopathology of a pancreatic endocrine tumor (insulinoma). Chromogranin A immunostain. Source:https://librepathology.org/wiki/Neuroendocrine_tumour_of_the_pancreas[34]](/images/a/a3/Pancreatic_insulinoma_histopathology_3.JPG)
![Histopathology of a pancreatic endocrine tumor (insulinoma). Insulin immunostain. Source:https://librepathology.org/wiki/Neuroendocrine_tumour_of_the_pancreas[34]](/images/d/d5/Pancreatic_insulinoma_histology_4.JPG)