Asthma classification: Difference between revisions
No edit summary |
|||
| Line 6: | Line 6: | ||
Asthma is classified into atopic and non-atopic types based on the onset of symptoms. Atopic refers to early-onset whereas non-atopic refers to late-onset. Despite the differentiation, a significant degree of overlap exists between the two types. The severity of symptoms is further classified based on the GINA severity grades into mild intermittent, mild persistent, moderate persistent and severe persistent asthma. | Asthma is classified into atopic and non-atopic types based on the onset of symptoms. Atopic refers to early-onset whereas non-atopic refers to late-onset. Despite the differentiation, a significant degree of overlap exists between the two types. The severity of symptoms is further classified based on the GINA severity grades into mild intermittent, mild persistent, moderate persistent and severe persistent asthma. | ||
==Classification Based on Symptom Onset== | ==Classification== | ||
===Based on Symptom Onset=== | |||
====Early-onset Asthma (Atopic, Allergic, Extrinsic)==== | ====Early-onset Asthma (Atopic, Allergic, Extrinsic)==== | ||
*Early-age of onset | *Early-age of onset | ||
*[[Atopy|Atopic individuals]] have an increased predisposition | *[[Atopy|Atopic individuals]] have an increased predisposition | ||
*[[Asthma triggers|Environmental allergens]] play a strong role in the pathogenesis | *[[Asthma triggers|Environmental allergens]] play a strong role in the pathogenesis | ||
*Positive personal and/or family history of [[atopic | *Positive personal and/or family history of [[atopic diseases]] such as [[allergic rhinitis]], [[urticaria]] and [[eczema]] | ||
*[[Asthma laboratory tests|Laboratory tests]] may reveal increased [[Asthma laboratory tests#Serum and Sputum Examination|serum IgE levels]], positive [[Asthma laboratory tests#Allergy Testing|skin test]] to specific aero-allergens and a positive [[Asthma bronchial challenge test#Bronchoprovocation Test|bronchoprovocation test]] | *[[Asthma laboratory tests|Laboratory tests]] may reveal increased [[Asthma laboratory tests#Serum and Sputum Examination|serum IgE levels]], positive [[Asthma laboratory tests#Allergy Testing|skin test]] to specific aero-allergens and a positive [[Asthma bronchial challenge test#Bronchoprovocation Test|bronchoprovocation test]] | ||
====Late-onset Asthma (Non-Atopic, Idiosyncratic, Intrinsic)==== | ====Late-onset Asthma (Non-Atopic, Idiosyncratic, Intrinsic)==== | ||
*Late-age of onset | *Late-age of onset | ||
*Non-atopic individuals have an increased predisposition | *Non- atopic individuals have an increased predisposition | ||
*[[Asthma triggers|Indoor allergens]] play a strong role in the pathogenesis | *[[Asthma triggers|Indoor allergens]] play a strong role in the pathogenesis | ||
*Negative personal and/or family history of [[atopic diseases|allergic diseases]] | *Negative personal and/or family history of [[atopic diseases|allergic diseases]] | ||
*[[Asthma laboratory tests|Laboratory tests]] may reveal normal [[Asthma laboratory tests#Serum and Sputum Examination|serum IgE levels]] and a negative [[Asthma bronchial challenge test#Bronchoprovocation Test|bronchoprovocation test]] | *[[Asthma laboratory tests|Laboratory tests]] may reveal normal [[Asthma laboratory tests#Serum and Sputum Examination|serum IgE levels]] and a negative [[Asthma bronchial challenge test#Bronchoprovocation Test|bronchoprovocation test]] | ||
== | ===Based on GINA Severity Grade=== | ||
Asthma is classified into four subgroup, namely, mild intermittent, mild persistent, moderate persistent and severe persistent based on the ''Global Initiative for Asthma - GINA severity grades''.<ref name="pmid18166595">Bateman ED, Hurd SS, Barnes PJ, Bousquet J, Drazen JM, FitzGerald M et al. (2008) [http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=18166595 Global strategy for asthma management and prevention: GINA executive summary.] ''Eur Respir J'' 31 (1):143-78. [http://dx.doi.org/10.1183/09031936.00138707 DOI:10.1183/09031936.00138707] PMID: [http://pubmed.gov/18166595 18166595]</ref> | Asthma is classified into four subgroup, namely, mild intermittent, mild persistent, moderate persistent and severe persistent based on the ''Global Initiative for Asthma - GINA severity grades''.<ref name="pmid18166595">Bateman ED, Hurd SS, Barnes PJ, Bousquet J, Drazen JM, FitzGerald M et al. (2008) [http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=18166595 Global strategy for asthma management and prevention: GINA executive summary.] ''Eur Respir J'' 31 (1):143-78. [http://dx.doi.org/10.1183/09031936.00138707 DOI:10.1183/09031936.00138707] PMID: [http://pubmed.gov/18166595 18166595]</ref> | ||
==Mild Intermittent Asthma== | ===Mild Intermittent Asthma=== | ||
{| border="1" align="center" style="background:lightskyblue" | {| border="1" align="center" style="background:lightskyblue" | ||
|- | |- | ||
| Line 39: | Line 39: | ||
|} | |} | ||
====Step 1 | ====Step 1 Therapy:==== | ||
Short-acting inhaled [[Bronchodilator#Short-acting β2-agonists|β2-agonists]] on need basis.<ref name="pmid7436160">Shim C, Williams MH (1980) [http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=7436160 Bronchial response to oral versus aerosol metaproterenol in asthma.] ''Ann Intern Med'' 93 (3):428-31. PMID: [http://pubmed.gov/7436160 7436160]</ref><ref name="pmid7282733">Shim C, Williams MH (1981) [http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=7282733 Comparison of oral aminophylline and aerosol metaproterenol in asthma.] ''Am J Med'' 71 (3):452-5. PMID: [http://pubmed.gov/7282733 7282733]</ref> | Short-acting inhaled [[Bronchodilator#Short-acting β2-agonists|β2-agonists]] on need basis.<ref name="pmid7436160">Shim C, Williams MH (1980) [http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=7436160 Bronchial response to oral versus aerosol metaproterenol in asthma.] ''Ann Intern Med'' 93 (3):428-31. PMID: [http://pubmed.gov/7436160 7436160]</ref><ref name="pmid7282733">Shim C, Williams MH (1981) [http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=7282733 Comparison of oral aminophylline and aerosol metaproterenol in asthma.] ''Am J Med'' 71 (3):452-5. PMID: [http://pubmed.gov/7282733 7282733]</ref> | ||
==Mild Persistent Asthma== | ===Mild Persistent Asthma=== | ||
{| border="1" align="center" style="background:lightskyblue" | {| border="1" align="center" style="background:lightskyblue" | ||
|- | |- | ||
| Line 57: | Line 56: | ||
|} | |} | ||
====Step 2 | ====Step 2 Therapy:==== | ||
*Preferred drug of choice is once a day [[steroid|low-dose steroid]] inhalation. | *Preferred drug of choice is once a day [[steroid|low-dose steroid]] inhalation. | ||
*Alternative therapies include: | *Alternative therapies include: | ||
| Line 63: | Line 62: | ||
:*[[Theophylline]], [[montelukast]], [[zafirlukast]] along with a short-acting inhaled [[Bronchodilator#Short-acting β2-agonists|β2-agonists]].<ref name="pmid11037987">Berridge MS, Lee Z, Heald DL (2000) [http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=11037987 Pulmonary distribution and kinetics of inhaled [11C]triamcinolone acetonide.] ''J Nucl Med'' 41 (10):1603-11. PMID: [http://pubmed.gov/11037987 11037987]</ref> | :*[[Theophylline]], [[montelukast]], [[zafirlukast]] along with a short-acting inhaled [[Bronchodilator#Short-acting β2-agonists|β2-agonists]].<ref name="pmid11037987">Berridge MS, Lee Z, Heald DL (2000) [http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=11037987 Pulmonary distribution and kinetics of inhaled [11C]triamcinolone acetonide.] ''J Nucl Med'' 41 (10):1603-11. PMID: [http://pubmed.gov/11037987 11037987]</ref> | ||
==Moderate Persistent Asthma== | ===Moderate Persistent Asthma=== | ||
{| border="1" align="center" style="background:lightskyblue" | {| border="1" align="center" style="background:lightskyblue" | ||
|- | |- | ||
| Line 78: | Line 76: | ||
|} | |} | ||
====Step 3 | ====Step 3 Therapy:==== | ||
*Preferred drug of choice: | *Preferred drug of choice: | ||
:*Moderate dose of inhaled [[steroid]], ''OR'' | :*Moderate dose of inhaled [[steroid]], ''OR'' | ||
:*Low dose inhaled [[steroid]] along with inhaled [[Bronchodilators#Long-acting β2-agonists|long-acting β2-agonists]] <ref name="pmid11174215">Nelson HS (2001) [http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=11174215 Advair: combination treatment with fluticasone propionate/salmeterol in the treatment of asthma.] ''J Allergy Clin Immunol'' 107 (2):398-416. [http://dx.doi.org/10.1067/mai.2001.112939 DOI:10.1067/mai.2001.112939] PMID: [http://pubmed.gov/11174215 11174215]</ref> or [[Bronchodilators#Theophylline|sustained-release theophylline]] for nocturnal symptoms, | :*Low dose inhaled [[steroid]] along with inhaled [[Bronchodilators#Long-acting β2-agonists|long-acting β2-agonists]] <ref name="pmid11174215">Nelson HS (2001) [http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=11174215 Advair: combination treatment with fluticasone propionate/salmeterol in the treatment of asthma.] ''J Allergy Clin Immunol'' 107 (2):398-416. [http://dx.doi.org/10.1067/mai.2001.112939 DOI:10.1067/mai.2001.112939] PMID: [http://pubmed.gov/11174215 11174215]</ref> or [[Bronchodilators#Theophylline|sustained-release theophylline]] for nocturnal symptoms, | ||
*Alternative strategy includes the use of low-dose of inhaled [[steroid]] along with long-acting bronchodilators (either [[Bronchodilators#Long-acting β2-agonists|inhaled long-acting β2-agonists]] or [[Bronchodilators#Theophylline|sustained-release theophylline]]) and/or a short-acting inhaled [[Bronchodilator#Short-acting β2-agonists|β2-agonists]] on need basis. | *Alternative strategy includes the use of low-dose of inhaled [[steroid]] along with long-acting bronchodilators (either [[Bronchodilators#Long-acting β2-agonists|inhaled long-acting β2-agonists]] or [[Bronchodilators#Theophylline|sustained-release theophylline]]) and/or a short-acting inhaled [[Bronchodilator#Short-acting β2-agonists|β2-agonists]] on need basis. | ||
==Severe Persistent Asthma== | ===Severe Persistent Asthma=== | ||
{| border="1" align="center" style="background:lightskyblue" | {| border="1" align="center" style="background:lightskyblue" | ||
|- | |- | ||
| Line 100: | Line 96: | ||
|} | |} | ||
====Step 4 | ====Step 4 Therapy:==== | ||
*Preferred drug of choice: Medium-dose of inhaled [[steroid]] along with [[Bronchodilators#Long-acting β2-agonists|inhaled long-acting β2-agonists]] | *Preferred drug of choice: Medium-dose of inhaled [[steroid]] along with [[Bronchodilators#Long-acting β2-agonists|inhaled long-acting β2-agonists]] | ||
*Alternative strategy includes the use of medium-dose inhaled [[steroids]] along with long-acting [[bronchodilators]] (such as [[Bronchodilators#Long-acting β2-agonists|inhaled β2-agonists]] or [[Bronchodilators#Theophylline|sustained-release theophylline]] used alone or in combination) and/or short-acting inhaled [[Bronchodilator#Short-acting β2-agonists|β2-agonists]] may be used on need basis. | *Alternative strategy includes the use of medium-dose inhaled [[steroids]] along with long-acting [[bronchodilators]] (such as [[Bronchodilators#Long-acting β2-agonists|inhaled β2-agonists]] or [[Bronchodilators#Theophylline|sustained-release theophylline]] used alone or in combination) and/or short-acting inhaled [[Bronchodilator#Short-acting β2-agonists|β2-agonists]] may be used on need basis. | ||
====Step 5 Therapy:==== | |||
*Preferred drug of choice: High-dose of inhaled [[steroid]] along with [[Bronchodilators#Long-acting β2-agonists|inhaled long-acting β2-agonists]] and [[omalizumab]] in patients who have allergies. | *Preferred drug of choice: High-dose of inhaled [[steroid]] along with [[Bronchodilators#Long-acting β2-agonists|inhaled long-acting β2-agonists]] and [[omalizumab]] in patients who have allergies. | ||
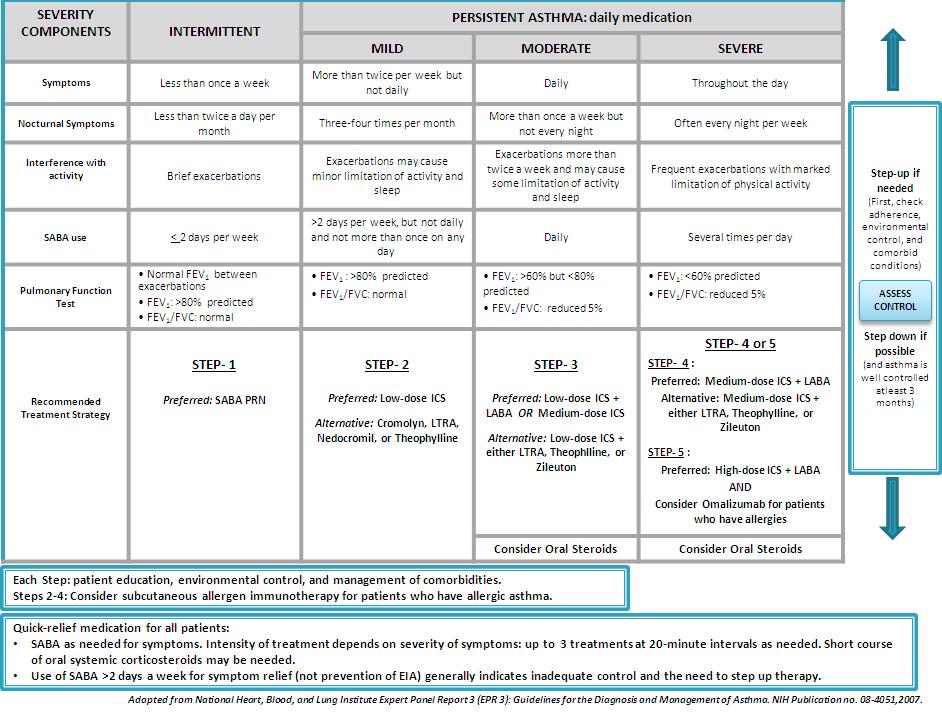
==Guidelines for Diagnosis and Management of Asthma Based On The National Heart, Blood, and Lung Institute Expert Panel Report 3 (EPR3) <ref name="pmid18240881">Urbano FL (2008) [http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=18240881 Review of the NAEPP 2007 Expert Panel Report (EPR-3) on Asthma Diagnosis and Treatment Guidelines.] ''J Manag Care Pharm'' 14 (1):41-9. PMID: [http://pubmed.gov/18240881 18240881]</ref>== | ==Guidelines for Diagnosis and Management of Asthma Based On The National Heart, Blood, and Lung Institute Expert Panel Report 3 (EPR3) <ref name="pmid18240881">Urbano FL (2008) [http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=18240881 Review of the NAEPP 2007 Expert Panel Report (EPR-3) on Asthma Diagnosis and Treatment Guidelines.] ''J Manag Care Pharm'' 14 (1):41-9. PMID: [http://pubmed.gov/18240881 18240881]</ref>== | ||
[[File:Asthma Severity Classification.JPG|center| | [[File:Asthma Severity Classification.JPG|center|1000px]] | ||
<br clear="left"/> | <br clear="left"/> | ||
Revision as of 19:57, 26 February 2013
|
Asthma Microchapters |
|
Diagnosis |
|---|
|
Other Diagnostic Studies |
|
Treatment |
|
Case Studies |
|
Asthma classification On the Web |
|
American Roentgen Ray Society Images of Asthma classification |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: Lakshmi Gopalakrishnan, M.B.B.S. [2]
Overview
Asthma is classified into atopic and non-atopic types based on the onset of symptoms. Atopic refers to early-onset whereas non-atopic refers to late-onset. Despite the differentiation, a significant degree of overlap exists between the two types. The severity of symptoms is further classified based on the GINA severity grades into mild intermittent, mild persistent, moderate persistent and severe persistent asthma.
Classification
Based on Symptom Onset
Early-onset Asthma (Atopic, Allergic, Extrinsic)
- Early-age of onset
- Atopic individuals have an increased predisposition
- Environmental allergens play a strong role in the pathogenesis
- Positive personal and/or family history of atopic diseases such as allergic rhinitis, urticaria and eczema
- Laboratory tests may reveal increased serum IgE levels, positive skin test to specific aero-allergens and a positive bronchoprovocation test
Late-onset Asthma (Non-Atopic, Idiosyncratic, Intrinsic)
- Late-age of onset
- Non- atopic individuals have an increased predisposition
- Indoor allergens play a strong role in the pathogenesis
- Negative personal and/or family history of allergic diseases
- Laboratory tests may reveal normal serum IgE levels and a negative bronchoprovocation test
Based on GINA Severity Grade
Asthma is classified into four subgroup, namely, mild intermittent, mild persistent, moderate persistent and severe persistent based on the Global Initiative for Asthma - GINA severity grades.[1]
Mild Intermittent Asthma
| Symptoms per day | Symptoms per night | PEF or FEV1 | PEF variability |
| Less than once a week. Brief exacerbations. Asymptomatic and normal PEFR between exacerbations. | Less than or equal to twice a month | ≥ 80% of predicted normal | < 20% |
Step 1 Therapy:
Short-acting inhaled β2-agonists on need basis.[2][3]
Mild Persistent Asthma
| Symptoms per day | Symptoms per night | PEF or FEV1 | PEF variability |
| Symptoms more than twice a week but less than once a day. Exacerbations may affect activity and sleep. | Greater than or equal to twice a month | ≥ 80% | 20-30% |
Step 2 Therapy:
- Preferred drug of choice is once a day low-dose steroid inhalation.
- Alternative therapies include:
- Use of anti-inflammatory drugs such as cromolyn or nedocromil, OR
- Theophylline, montelukast, zafirlukast along with a short-acting inhaled β2-agonists.[4]
Moderate Persistent Asthma
| Symptoms per day | Symptoms per night | PEF or FEV1 | PEF variability |
| Daily symptoms. Exacerbations more than twice a week. Exacerbations may affect activity and sleep. Daily use of bronchodilators. | More than once a month | 60-80% | ≥ 30% |
Step 3 Therapy:
- Preferred drug of choice:
- Moderate dose of inhaled steroid, OR
- Low dose inhaled steroid along with inhaled long-acting β2-agonists [5] or sustained-release theophylline for nocturnal symptoms,
- Alternative strategy includes the use of low-dose of inhaled steroid along with long-acting bronchodilators (either inhaled long-acting β2-agonists or sustained-release theophylline) and/or a short-acting inhaled β2-agonists on need basis.
Severe Persistent Asthma
| Symptoms per day | Symptoms per night | PEF or FEV1 | PEF variability |
| Continued symptoms. Frequent exacerbations. Limited physical activity. | Frequent | ≤ 60% | ≥ 30% |
Step 4 Therapy:
- Preferred drug of choice: Medium-dose of inhaled steroid along with inhaled long-acting β2-agonists
- Alternative strategy includes the use of medium-dose inhaled steroids along with long-acting bronchodilators (such as inhaled β2-agonists or sustained-release theophylline used alone or in combination) and/or short-acting inhaled β2-agonists may be used on need basis.
Step 5 Therapy:
- Preferred drug of choice: High-dose of inhaled steroid along with inhaled long-acting β2-agonists and omalizumab in patients who have allergies.
Guidelines for Diagnosis and Management of Asthma Based On The National Heart, Blood, and Lung Institute Expert Panel Report 3 (EPR3) [6]
References
- ↑ Bateman ED, Hurd SS, Barnes PJ, Bousquet J, Drazen JM, FitzGerald M et al. (2008) Global strategy for asthma management and prevention: GINA executive summary. Eur Respir J 31 (1):143-78. DOI:10.1183/09031936.00138707 PMID: 18166595
- ↑ Shim C, Williams MH (1980) Bronchial response to oral versus aerosol metaproterenol in asthma. Ann Intern Med 93 (3):428-31. PMID: 7436160
- ↑ Shim C, Williams MH (1981) Comparison of oral aminophylline and aerosol metaproterenol in asthma. Am J Med 71 (3):452-5. PMID: 7282733
- ↑ Berridge MS, Lee Z, Heald DL (2000) Pulmonary distribution and kinetics of inhaled [11Ctriamcinolone acetonide.] J Nucl Med 41 (10):1603-11. PMID: 11037987
- ↑ Nelson HS (2001) Advair: combination treatment with fluticasone propionate/salmeterol in the treatment of asthma. J Allergy Clin Immunol 107 (2):398-416. DOI:10.1067/mai.2001.112939 PMID: 11174215
- ↑ Urbano FL (2008) Review of the NAEPP 2007 Expert Panel Report (EPR-3) on Asthma Diagnosis and Treatment Guidelines. J Manag Care Pharm 14 (1):41-9. PMID: 18240881