Coenzyme Q10: Difference between revisions
| (2 intermediate revisions by the same user not shown) | |||
| Line 37: | Line 37: | ||
==Chemical properties== | ==Chemical properties== | ||
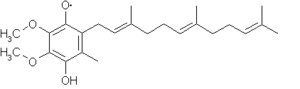
The oxidized structure of CoQ | The oxidized structure of CoQ is given here. The various kinds of CoQ can be distinguished by the number of [[isoprene|isoprenoid]] [[side-chain]]s they have. The most common CoQ in human [[mitochondria]] is CoQ<sub>10</sub>. The image to the right has three [[isoprene|isoprenoid]] units and would be called Q<sub>3</sub>. [[image:Ubiquinone3.png|center|300px]] | ||
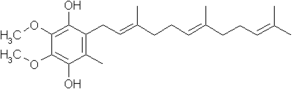
If CoQ is reduced by one equivalent, the following structure results, a ubisemiquinone, and is denoted QH. Note the [[free-radical]] on one of the ring oxygens (either oxygen may become a free-radical, in this case the top oxygen is shown as such). [[image:Ubisemiquinone3.png|center|300px]] | If CoQ is reduced by one equivalent, the following structure results, a ubisemiquinone, and is denoted QH. Note the [[free-radical]] on one of the ring oxygens (either oxygen may become a free-radical, in this case the top oxygen is shown as such). [[image:Ubisemiquinone3.png|center|300px]] | ||
| Line 66: | Line 66: | ||
A 2007 [[meta-analysis]] of all published trials of the use of CoQ<sub>10</sub> in the treating [[hypertension]] acts as the most comprehensive and current assessment of the efficacy and consistency of its therapeutic effect as well the incidence of side effects.<ref name="Rosenfeldt-2007">{{Cite journal |last1 = Rosenfeldt | first1 = FL. | last2 = Haas | first2 = SJ. | last3 = Krum | first3 = H. | last4 = Hadj | first4 = A. | last5 = Ng | first5 = K.|last6 = Leong | first6 = JY. | last7 = Watts | first7 = GF. | title = Coenzyme Q10 in the treatment of hypertension: a meta-analysis of the clinical trials. | journal = J Hum Hypertens | volume = 21 | issue = 4 | pages = 297-306 | month = Apr | year = 2007 | doi = 10.1038/sj.jhh.1002138 | PMID = 17287847 }}</ref> The analysis included 12 clinical trials, including three randomized controlled trials, one crossover study, and eight open label studies. Combined, the trials enrolled 326 patients, 120 as part of randomized trials and 214 as part of open label studies. Within the randomized controlled trials, the treatment groups experienced a significant average drop in [[blood pressure|systolic]] and [[blood pressure|diastolic blood pressure]] compared to control groups (16.6 mm Hg and 8.2 mm Hg decrease, respectively; P<0.001). During the treatment phase of the lone 18 patient cross-over study systolic and diastolic pressures were on average also significantly decreased (11 mm Hg and 8 mm Hg decrease, respectively; P<0.001). Likewise, the weighted mean systolic and diastolic blood pressures of patients enrolled in open label observational studies were significantly lower after patients began taking CoQ<sub>10</sub> (13.5 mm Hg and 10.3 mm Hg decrease, respectively, P<0.001). Overall, CoQ<sub>10</sub> treatment resulted in systolic blood pressure decreases between 11 and 17 mm Hg and diastolic blood pressure decreases between 8 and 10 mm Hg. Among all the studies CoQ<sub>10</sub> treatment produced minimal side effects, the most common being gastrointestinal effects. | A 2007 [[meta-analysis]] of all published trials of the use of CoQ<sub>10</sub> in the treating [[hypertension]] acts as the most comprehensive and current assessment of the efficacy and consistency of its therapeutic effect as well the incidence of side effects.<ref name="Rosenfeldt-2007">{{Cite journal |last1 = Rosenfeldt | first1 = FL. | last2 = Haas | first2 = SJ. | last3 = Krum | first3 = H. | last4 = Hadj | first4 = A. | last5 = Ng | first5 = K.|last6 = Leong | first6 = JY. | last7 = Watts | first7 = GF. | title = Coenzyme Q10 in the treatment of hypertension: a meta-analysis of the clinical trials. | journal = J Hum Hypertens | volume = 21 | issue = 4 | pages = 297-306 | month = Apr | year = 2007 | doi = 10.1038/sj.jhh.1002138 | PMID = 17287847 }}</ref> The analysis included 12 clinical trials, including three randomized controlled trials, one crossover study, and eight open label studies. Combined, the trials enrolled 326 patients, 120 as part of randomized trials and 214 as part of open label studies. Within the randomized controlled trials, the treatment groups experienced a significant average drop in [[blood pressure|systolic]] and [[blood pressure|diastolic blood pressure]] compared to control groups (16.6 mm Hg and 8.2 mm Hg decrease, respectively; P<0.001). During the treatment phase of the lone 18 patient cross-over study systolic and diastolic pressures were on average also significantly decreased (11 mm Hg and 8 mm Hg decrease, respectively; P<0.001). Likewise, the weighted mean systolic and diastolic blood pressures of patients enrolled in open label observational studies were significantly lower after patients began taking CoQ<sub>10</sub> (13.5 mm Hg and 10.3 mm Hg decrease, respectively, P<0.001). Overall, CoQ<sub>10</sub> treatment resulted in systolic blood pressure decreases between 11 and 17 mm Hg and diastolic blood pressure decreases between 8 and 10 mm Hg. Among all the studies CoQ<sub>10</sub> treatment produced minimal side effects, the most common being gastrointestinal effects. | ||
The most likely physiological explanation for the the [[hypotension|hypotensive]] effect of CoQ<sub>10</sub> observed in this meta-analysis is [[oxidative stress]] relief. CoQ10 indirectly increases the amount of free NO by neutralizing destructive [[radical|free radicals]]. Indeed, this explanation supports the finding that CoQ<sub>10</sub> does not have a hypotensive or [[vasodilator|vasodilating]] effect in patients who are healthy and do not have NO activity suppressed by oxidative stress. | The most likely physiological explanation for the the [[hypotension|hypotensive]] effect of CoQ<sub>10</sub> observed in this meta-analysis is [[oxidative stress]] relief. CoQ10 indirectly increases the amount of free [[nitric oxide|NO]] by neutralizing destructive [[radical|free radicals]]. Indeed, this explanation supports the finding that CoQ<sub>10</sub> does not have a hypotensive or [[vasodilator|vasodilating]] effect in patients who are healthy and do not have NO activity suppressed by oxidative stress. | ||
===Coronary Artery Disease=== | ===Coronary Artery Disease=== | ||
| Line 76: | Line 76: | ||
Slides about the role of mitochondria in heart failure: [[File:Mitochondrial_Dysfunction_and_CHF_for_wikidoc.pdf]] | Slides about the role of mitochondria in heart failure: [[File:Mitochondrial_Dysfunction_and_CHF_for_wikidoc.pdf]] | ||
CoQ<sub>10</sub> levels are decreased in the setting of [[heart failure]], and progressive heart failure leads to lower and lower levels of CoQ<sub>10</sub>. There have been modest sized [[double blind]] [[randomized controlled trials]] that have demonstrated CoQ<sub>10</sub> is associated with improved symptoms, functional capacity and quality of life in patients with heart failure. The drug is generally well tolerated, with few side effects. | CoQ<sub>10</sub> levels are decreased in the setting of [[heart failure]] (HF), and progressive heart failure leads to lower and lower levels of CoQ<sub>10</sub>. There have been modest sized [[double blind]] [[randomized controlled trials]] that have demonstrated CoQ<sub>10</sub> is associated with improved symptoms, functional capacity and quality of life in patients with heart failure. The drug is generally well tolerated, with few side effects. | ||
Congestive heart failure (CHF) is the third most common cause of cardiovascular disease, the leading cause of morbidity and mortality in the U.S. and around the world.<ref>{{Cite web | last = | first = | title = related:mdvAhRE800UJ:scholar.google.com/ - Google Scholar | url =http://scholar.google.com/scholar?q=related:mdvAhRE800UJ:scholar.google.com/&hl=en&num=20&as_sdt=0,5 | publisher = | date = | accessdate = 28 May 2013}}</ref> A 2006 double-blind, placebo-controlled cross-over design study of 23 patients divided into three groups treated with a differing orders and combinations of exercise, 100 mg tid CoQ<sub>10</sub>, and placebo demonstrated that both peak VO2 and endothelium-dependent dilation of the brachial artery (EDDBA) improved significantly after CoQ<sub>10</sub> and after exercise treatment.<ref name="Belardinelli-2006">{{Cite journal | last1 = Belardinelli | first1 = R. | last2 = Muçaj | first2 = A. | last3 = Lacalaprice | first3 = F. | last4 = Solenghi | first4 = M. | last5 = Seddaiu | first5 = G. | last6 = Principi | first6 = F. | last7 = Tiano | first7 = L. | last8 = Littarru | first8 = GP. | title = Coenzyme Q10 and exercise training in chronic heart failure. | journal = Eur Heart J | volume = 27 | issue = 22 | pages = 2675-81 | month = Nov | year = 2006 | doi = 10.1093/eurheartj/ehl158 |PMID = 16882678 }}</ref> As in other studies, CoQ<sub>10</sub> supplementation resulted in a four-fold increase in plasma CoQ<sub>10</sub> levels. This study showed additionally that exercise further increased plasma CoQ10 levels. While CoQ10 demonstrated a main effect on peak V02 (+ 9%), EDDBA (+38%), and the systolic wall thickening score index (SWTI) (-12%), exercise was also demonstrated to have comparable effects. While the combination of CoQ<sub>10</sub> supplementation and exercise resulted in the greatest benefit in these categories, the only significant synergistic effect observed between the two treatments was for peak SWTI. | Congestive heart failure (CHF) is the third most common cause of cardiovascular disease, the leading cause of [[morbidity]] and [[mortality rate|mortality]] in the U.S. and around the world.<ref>{{Cite web | last = | first = | title = related:mdvAhRE800UJ:scholar.google.com/ - Google Scholar | url =http://scholar.google.com/scholar?q=related:mdvAhRE800UJ:scholar.google.com/&hl=en&num=20&as_sdt=0,5 | publisher = | date = | accessdate = 28 May 2013}}</ref> A 2006 double-blind, placebo-controlled cross-over design study of 23 patients divided into three groups treated with a differing orders and combinations of exercise, 100 mg tid CoQ<sub>10</sub>, and placebo demonstrated that both peak VO2 and endothelium-dependent dilation of the brachial artery (EDDBA) improved significantly after CoQ<sub>10</sub> and after exercise treatment.<ref name="Belardinelli-2006">{{Cite journal | last1 = Belardinelli | first1 = R. | last2 = Muçaj | first2 = A. | last3 = Lacalaprice | first3 = F. | last4 = Solenghi | first4 = M. | last5 = Seddaiu | first5 = G. | last6 = Principi | first6 = F. | last7 = Tiano | first7 = L. | last8 = Littarru | first8 = GP. | title = Coenzyme Q10 and exercise training in chronic heart failure. | journal = Eur Heart J | volume = 27 | issue = 22 | pages = 2675-81 | month = Nov | year = 2006 | doi = 10.1093/eurheartj/ehl158 |PMID = 16882678 }}</ref> As in other studies, CoQ<sub>10</sub> supplementation resulted in a four-fold increase in plasma CoQ<sub>10</sub> levels. This study showed additionally that exercise further increased plasma CoQ10 levels. While CoQ10 demonstrated a main effect on peak V02 (+ 9%), EDDBA (+38%), and the systolic wall thickening score index (SWTI) (-12%), exercise was also demonstrated to have comparable effects. While the combination of CoQ<sub>10</sub> supplementation and exercise resulted in the greatest benefit in these categories, the only significant synergistic effect observed between the two treatments was for peak SWTI. | ||
A 2013 meta-analysis serves as the most recent and comprehensive review of the effects of CoQ<sub>10</sub> supplementation on HF, specifically its impact on the ejection fraction (EF) and New York Heart Association (NYHA) functional classification in patients with CHF.<ref name="Fotino-2013">{{Cite journal | last1 = Fotino | first1 = AD. | last2 = Thompson-Paul | first2 = AM. | last3 = Bazzano | first3 = LA. | title = Effect of coenzyme Q₁₀ supplementation on heart failure: a meta-analysis. | journal = Am J Clin Nutr | volume = 97 | issue = 2 | pages = 268-75 | month = Feb | year = 2013 | doi = 10.3945/ajcn.112.040741 | PMID = 23221577 }}</ref> The study found 120 potentially relevant studies during a literature review and selected 13 for the analysis, of which 7 were crossover and 6 were parallel-arm studies, with 12 double-blinded studies and 1 single-blind study. The enrollment of the analyzed studies was 395. A confounder in the analysis was the wide range in study duration (4 to 28 weeks) and variable CoQ<sub>10</sub> daily dosing (60 to 300mg). Supplementation with CoQ<sub>10</sub> resulted in a pooled mean net change of 3.67% (95% CI: 1.60%, 5.74%) in the EF and a 0.30 decrease (95% CI: -0.66, 0.06) in the NYHA functional class. Significant improvement in EF was seen in crossover trials, trials twelve weeks long or longer, studies published before 1994, studies with a daily CoQ<sub>10</sub> dose >=100 mg, and in patients with less severe CHF. The study cautiously suggests that CoQ<sub>10</sub> supplementation may improve EF in patients with CHF. | A 2013 meta-analysis serves as the most recent and comprehensive review of the effects of CoQ<sub>10</sub> supplementation on HF, specifically its impact on the [[ejection fraction]] (EF) and New York Heart Association (NYHA) functional classification in patients with CHF.<ref name="Fotino-2013">{{Cite journal | last1 = Fotino | first1 = AD. | last2 = Thompson-Paul | first2 = AM. | last3 = Bazzano | first3 = LA. | title = Effect of coenzyme Q₁₀ supplementation on heart failure: a meta-analysis. | journal = Am J Clin Nutr | volume = 97 | issue = 2 | pages = 268-75 | month = Feb | year = 2013 | doi = 10.3945/ajcn.112.040741 | PMID = 23221577 }}</ref> The study found 120 potentially relevant studies during a literature review and selected 13 for the analysis, of which 7 were crossover and 6 were parallel-arm studies, with 12 double-blinded studies and 1 single-blind study. The enrollment of the analyzed studies was 395. A confounder in the analysis was the wide range in study duration (4 to 28 weeks) and variable CoQ<sub>10</sub> daily dosing (60 to 300mg). Supplementation with CoQ<sub>10</sub> resulted in a pooled mean net change of 3.67% (95% CI: 1.60%, 5.74%) in the EF and a 0.30 decrease (95% CI: -0.66, 0.06) in the NYHA functional class. Significant improvement in EF was seen in crossover trials, trials twelve weeks long or longer, studies published before 1994, studies with a daily CoQ<sub>10</sub> dose >=100 mg, and in patients with less severe CHF. The study cautiously suggests that CoQ<sub>10</sub> supplementation may improve EF in patients with CHF. | ||
===== Q-SYMBIO Trial===== | ===== Q-SYMBIO Trial===== | ||
Latest revision as of 15:08, 29 May 2013
|
WikiDoc Resources for Coenzyme Q10 |
|
Articles |
|---|
|
Most recent articles on Coenzyme Q10 Most cited articles on Coenzyme Q10 |
|
Media |
|
Powerpoint slides on Coenzyme Q10 |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Coenzyme Q10 at Clinical Trials.gov Clinical Trials on Coenzyme Q10 at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Coenzyme Q10
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Coenzyme Q10 Discussion groups on Coenzyme Q10 Patient Handouts on Coenzyme Q10 Directions to Hospitals Treating Coenzyme Q10 Risk calculators and risk factors for Coenzyme Q10
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Coenzyme Q10 |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Coenzyme Q10 (also known as ubiquinone, ubidecarenone, coenzyme Q, and abbreviated at times to CoQ10, CoQ, Q10, or Q) is a benzoquinone, where Q refers to the quinone chemical group, and 10 refers to the isoprenyl chemical subunits.
This vitamin-like substance is, by nature, present in most human cells except red blood cells and eye lens cells (no mitochondria) and are responsible for the production of the body’s own energy. In each human cell, food energy is converted into energy in the mitochondria with the aid of CoQ10. Ninety-five percent of all the human body’s energy requirements (ATP) is converted with the aid of CoQ10.[1][2] Therefore, those organs with the highest energy requirements – such as the heart and the liver – have the highest CoQ10 concentrations.[3][4][5]
History
CoQ10 was first discovered by Crane et al. in 1957 within beef heart mitochondria.[6] This vitamin-like nutrient has since been implicated in three major biological processes, imparting its alternate name of “ubiquinone”. Floating within the inner membrane of mitochrodria, CoQ10 plays an important role in oxidative phosphorylation where it is responsible for the two electron oxidation of NADH.[7][8] Second, CoQ10 serves as a free radical scavenger that is the only lipid-soluble antioxidant that can be enzymatically regenerated to a reduced, active form.[9][10][11] In this capacity it plays an important role in decreasing the amount of superoxide radical (O2-). This radical is produced by physiological stress, such as that caused by disease, and reacts rapidly with endothelial nitric oxide (NO) which is important for endothelial health and NO-mediated vasodilation. Lastly, CoQ10 has more recently been identified as a potent gene regulator, significantly impacting the expression of genes encoding proteins involved in cell signaling, intermediate metabolism, transport, transcriptional control, disease mutation, phosphorylation, embryonal development, and binding.[12]
Occurrence in nature
CoQ10 occurs in mackerel and herring fresh heart tissue in concentrations of 105-148 μg/g. In fresh mackerel "red and white tissue," CoQ10 concentrations of 67 and 15 μg/g, respectively, have been reported. In fresh herring tissue, an amount of 15–24 μg/g of CoQ10 has been reported.[13]
CoQ10 Content of various foods:[14]
| Food | CoQ10 [μg/g] |
Portion of Food [g] |
CoQ10 Amount in Portion [mg] |
|---|---|---|---|
| Pork heart | 203 | 120 | 24 |
| Chicken leg | 17 | 120 | 2.0 |
| Beef heart | 41 | 120 | 4.8 |
Chemical properties
The oxidized structure of CoQ is given here. The various kinds of CoQ can be distinguished by the number of isoprenoid side-chains they have. The most common CoQ in human mitochondria is CoQ10. The image to the right has three isoprenoid units and would be called Q3.

If CoQ is reduced by one equivalent, the following structure results, a ubisemiquinone, and is denoted QH. Note the free-radical on one of the ring oxygens (either oxygen may become a free-radical, in this case the top oxygen is shown as such).
If CoQ is reduced by two equivalents, the compound becomes a ubiquinol, denoted QH2:
Biochemical role
CoQ is found in the membranes of endoplasmic reticulum, peroxisomes, lysosomes, vesicles, and the inner membrane of the mitochondrion, where it is an important part of the electron transport chain; there it passes reducing equivalents to acceptors such as Coenzyme Q: cytochrome c - oxidoreductase:
- CoQH2+ 2 FeIII-cytochrome c → CoQ + 2 FeII-cytochrome c
CoQ is also essential in the formation of the apoptosome, along with other adapter proteins. The loss of trophic factors activates pro-apoptotic enzymes, causing the breakdown of mitochondria.
Biosynthesis
The benzoquinone portion of CoQ10 is synthesized from tyrosine, whereas the isoprene sidechain is synthesized from acetyl-CoA through the mevalonate pathway. The mevalonate pathway is used for the first steps of cholesterol biosynthesis.
Supplementation
Because of its ability to transfer electrons and therefore act as an antioxidant, CoQ10 is also used as a dietary supplement. When you are younger the body can synthesize Q10 from the lower-numbered ubiquinones such as Q6 or Q8. The sick and elderly may not be able to make enough, thus Q10 becomes a vitamin later in life and in illness.
Mitochondrial disorders
Supplementation of CoQ10 is a treatment for some of the very rare and serious mitochondrial disorders and other metabolic disorders, where patients are not capable of producing enough CoQ10 because of their disorder. CoQ10 is then prescribed by a physician.[15]
Cardiac and Vascular Disease
In 1970 Folkers et al. demonstrated that between 70-75% of patients with heart disease have low levels of CoQ10.[16] The increasing severity of heart disease was correlated with progressively declining blood and myocardial tissue levels of CoQ10 in 1972.[17] Though it is thought that normal CoQ10 serum levels can be maintained by doses of 30-60mg/day (per 1kg), clinical benefit may not actually be obtained until serum CoQ10 levels reach 2-4 times their normal level. In patients with cardiomyopathy and low levels of myocardial CoQ10, the addition of 100mg/day of oral CoQ10 over a 2-8 month period has been shown to increase myocardial CoQ10 levels between 20 and 85%.[18] Though these studies have correlated a CoQ10 deficit with cardiovascular disease and demonstrate that CoQ10 serum and myocardial levels can be elevated with CoQ10 supplementation, the true efficacy of CoQ10 supplementation in cardiovascular disease remains unclear.
Hypertension
A 2007 meta-analysis of all published trials of the use of CoQ10 in the treating hypertension acts as the most comprehensive and current assessment of the efficacy and consistency of its therapeutic effect as well the incidence of side effects.[19] The analysis included 12 clinical trials, including three randomized controlled trials, one crossover study, and eight open label studies. Combined, the trials enrolled 326 patients, 120 as part of randomized trials and 214 as part of open label studies. Within the randomized controlled trials, the treatment groups experienced a significant average drop in systolic and diastolic blood pressure compared to control groups (16.6 mm Hg and 8.2 mm Hg decrease, respectively; P<0.001). During the treatment phase of the lone 18 patient cross-over study systolic and diastolic pressures were on average also significantly decreased (11 mm Hg and 8 mm Hg decrease, respectively; P<0.001). Likewise, the weighted mean systolic and diastolic blood pressures of patients enrolled in open label observational studies were significantly lower after patients began taking CoQ10 (13.5 mm Hg and 10.3 mm Hg decrease, respectively, P<0.001). Overall, CoQ10 treatment resulted in systolic blood pressure decreases between 11 and 17 mm Hg and diastolic blood pressure decreases between 8 and 10 mm Hg. Among all the studies CoQ10 treatment produced minimal side effects, the most common being gastrointestinal effects.
The most likely physiological explanation for the the hypotensive effect of CoQ10 observed in this meta-analysis is oxidative stress relief. CoQ10 indirectly increases the amount of free NO by neutralizing destructive free radicals. Indeed, this explanation supports the finding that CoQ10 does not have a hypotensive or vasodilating effect in patients who are healthy and do not have NO activity suppressed by oxidative stress.
Coronary Artery Disease
CoQ10 treatment has also proven beneficial in the treatment of coronary artery disease (CAD). A placebo-controlled study of 19 patients with CAD was conducted to evaluate the effect of 100 mg CoQ10 tid for one month on vascular function as evaluated by extracellular superoxide dismutase (ecSOD) activity and brachial artery vasomotility measured by flow-dependent endothelial-mediated dilation (FMD). A secondary endpoint was to determine the effect of CoQ10 on the cardiopulmonary test.[20] A four-fold increase in serum CoQ10 levels was reported within the treatment group and was significantly correlated with endothelium-dependent (ED) relaxation. ecSOD activation, peak VO2, and O2 pulse increases were also significantly greater in the treatment group compared to the placebo group. The effect of CoQ10 treatment was greatest on patients with the lowest levels of ecSOD and hence most vulnerable to oxidative stress.
ecSOD is an enzyme highly expressed in the heart that has been examined for its role in several diseases, including vascular-related diseases such as CAD. These results build upon and confirm a 2000 study demonstrating that ecSOD activity is substantially reduced in patients with CAD and that endothelium-bound ecSOD activity level strongly correlates with endothelial-mediated dilation (FMD), a biomarker of vascular function.[21] It it also known that NO can induce ecSOD expression. Therefore, likely physiological explanation for the benefit of CoQ10 for vascular health in CAD stems in part from the ability of CoQ10 to relieve oxidative stress on NO, resulting increased ecSOD activity. The effect of CoQ10 on peak VO2 and O2 pulse is most likely attributable to its bioenergetic properties.
Congestive Heart Failure
Slides about the role of mitochondria in heart failure: File:Mitochondrial Dysfunction and CHF for wikidoc.pdf
CoQ10 levels are decreased in the setting of heart failure (HF), and progressive heart failure leads to lower and lower levels of CoQ10. There have been modest sized double blind randomized controlled trials that have demonstrated CoQ10 is associated with improved symptoms, functional capacity and quality of life in patients with heart failure. The drug is generally well tolerated, with few side effects.
Congestive heart failure (CHF) is the third most common cause of cardiovascular disease, the leading cause of morbidity and mortality in the U.S. and around the world.[22] A 2006 double-blind, placebo-controlled cross-over design study of 23 patients divided into three groups treated with a differing orders and combinations of exercise, 100 mg tid CoQ10, and placebo demonstrated that both peak VO2 and endothelium-dependent dilation of the brachial artery (EDDBA) improved significantly after CoQ10 and after exercise treatment.[23] As in other studies, CoQ10 supplementation resulted in a four-fold increase in plasma CoQ10 levels. This study showed additionally that exercise further increased plasma CoQ10 levels. While CoQ10 demonstrated a main effect on peak V02 (+ 9%), EDDBA (+38%), and the systolic wall thickening score index (SWTI) (-12%), exercise was also demonstrated to have comparable effects. While the combination of CoQ10 supplementation and exercise resulted in the greatest benefit in these categories, the only significant synergistic effect observed between the two treatments was for peak SWTI.
A 2013 meta-analysis serves as the most recent and comprehensive review of the effects of CoQ10 supplementation on HF, specifically its impact on the ejection fraction (EF) and New York Heart Association (NYHA) functional classification in patients with CHF.[24] The study found 120 potentially relevant studies during a literature review and selected 13 for the analysis, of which 7 were crossover and 6 were parallel-arm studies, with 12 double-blinded studies and 1 single-blind study. The enrollment of the analyzed studies was 395. A confounder in the analysis was the wide range in study duration (4 to 28 weeks) and variable CoQ10 daily dosing (60 to 300mg). Supplementation with CoQ10 resulted in a pooled mean net change of 3.67% (95% CI: 1.60%, 5.74%) in the EF and a 0.30 decrease (95% CI: -0.66, 0.06) in the NYHA functional class. Significant improvement in EF was seen in crossover trials, trials twelve weeks long or longer, studies published before 1994, studies with a daily CoQ10 dose >=100 mg, and in patients with less severe CHF. The study cautiously suggests that CoQ10 supplementation may improve EF in patients with CHF.
Q-SYMBIO Trial
In a modest sized, multicenter, double blind,randomized controlled trial, 420 patients with New York Heart Association (NYHA) Class III or IV heart failure who were receiving standard therapy, were randomized to either CoQ10 or placebo. The patients were followed for two years. [25]. The primary endpoint (MACE=unplanned hospitalization due to worsening of heart failure, cardiovascular death, urgent cardiac transplantation and mechanical circulatory support) was reduced from 29 events (14%) in patients randomized to CoQ10 compared to 55 (25%) in patients randomized to placebo (hazard ratio=2; p=0.003 by time to event analysis). Randomization to CoQ10 was associated with a halving of all cause mortality: there were 18 (9%) deaths among patients in the CoQ10 group versus 36 (17%) deaths among patients in the placebo group (hazard ratio=2.1; p=0.01). Cardiovascular mortality was also reduced (p-0.02) as was the risk of rehospitalisations for heart failure (p=0.05). There tended to be fewer adverse events among patients randomized to CoQ10 compared to the placebo (p=0.073). It is unclear if there were greater benefits among patients treated with statins, drugs that lower CoQ10.
Treatment of Statin Intolerance
CoQ10 shares a common biosynthetic pathway with cholesterol. The synthesis of an intermediary precursor of CoQ10, mevalonate, is inhibited by some beta blockers, blood pressure-lowering medication,[26] and statins, a class of cholesterol-lowering drugs.[27] Statins can reduce serum levels of CoQ10 by up to 40%.[28] Some research suggests the logical option of supplementation with CoQ10 as a routine adjunct to any treatment that may reduce endogenous production of CoQ10, based on a balance of likely benefit against very small risk.[29][30]
Cardiac arrest
Another recent study shows a survival benefit after cardiac arrest if CoQ10 is administered in addition to commencing active cooling (to 32–34 degrees Celsius).[31]
Migraine headaches
Supplementation of CoQ10 has been found to have a beneficial effect on the condition of some sufferers of migraine headaches. So far, three studies have been done, of which two were small, did not have a placebo group, were not randomized, and were open-label,[32] and one was a double-blind, randomized, placebo-controlled trial, which found statistically significant results despite its small sample size of 42 patients.[33] Dosages were 150 to 300 mg/day.
Cancer
It is also being investigated as a treatment for cancer, and as relief from cancer treatment side-effects.[34]
Brain health and neurodegenerative diseases
Recent studies have shown that the antioxidant properties of CoQ10 benefit the body and the brain in animal models.[35] Some of these studies indicate that CoQ10 protects the brain from neurodegenerative disease such as Parkinson's,[36] although it does not relieve the symptoms.[37] Dosage was 300 mg per day.
Lifespan
Studies have shown that low dosages of CoQ10 reduce oxidation and DNA double-strand breaks, and a combination of a diet rich in polyunsaturated fatty acids and CoQ10supplementation leads to a longer lifespan in rats[38]
See Also
- Idebenone - synthetic analog with reduced oxidant generating properties
External links
- A User-Friendly Summary of CoQ10
- An Introduction to Coenzyme Q10 at University of Washington
- Possible Health Benefits of Coenzyme Q10 at Oregon State University
- Study Suggests Coenzyme Q10 Slows Functional Decline in Parkinson's Disease at National Institute of Neurological Disorders and Stroke
References
- ↑ Ernster L, Dallner G: Biochemical, physiological and medical aspects of ubiquinone function. Biochim Biophys Acta 1271: 195-204, 1995
- ↑ Dutton PL, Ohnishi T, Darrouzet E, Leonard, MA, Sharp RE, Cibney BR, Daldal F and Moser CC. 4 Coenzyme Q oxidation reduction reactions in mitochondrial electron transport (pp 65-82) in Coenzyme Q: Molecular mechanisms in health and disease edited by Kagan VE and Quinn PJ, CRC Press (2000), Boca Raton
- ↑ Okamoto, T.et al (1989) Interna.J.Vit.Nutr.Res.,59,288-292
- ↑ Aberg,F.et al (1992)Archives of Biochemistry and Biophysics, 295, 230-234
- ↑ Shindo, Y., Witt, E., Han, D., Epstein, W., and Packer, L., Enzymic and non-enzymic antioxidants in epidermis and dermis of human skin, Invest. Dermatol., 102 (1994) 122-124.
- ↑ CRANE, FL.; HATEFI, Y.; LESTER, RL.; WIDMER, C. (1957). "Isolation of a quinone from beef heart mitochondria". Biochim Biophys Acta. 25 (1): 220–1. PMID 13445756. Unknown parameter
|month=ignored (help) - ↑ Lenaz, G. (1988). "Role of mobility of redox components in the inner mitochondrial membrane". J Membr Biol. 104 (3): 193–209. PMID 2850362. Unknown parameter
|month=ignored (help) - ↑ Mitchell, P. (1976). "Possible molecular mechanisms of the protonmotive function of cytochrome systems". J Theor Biol. 62 (2): 327–67. PMID 186667. Unknown parameter
|month=ignored (help) - ↑ "Highlights in ubiquinone research: proceedings of the International ... - Giorgio Lenaz, Universit di Bologna - Google Books". Retrieved 28 May 2013.
- ↑ Ernster, L.; Forsmark-Andrée, P. (1993). "Ubiquinol: an endogenous antioxidant in aerobic organisms". Clin Investig. 71 (8 Suppl): S60–5. PMID 8241707.
- ↑ Villalba, JM.; Navarro, F.; Gómez-Díaz, C.; Arroyo, A.; Bello, RI.; Navas, P. (1997). "Role of cytochrome b5 reductase on the antioxidant function of coenzyme Q in the plasma membrane". Mol Aspects Med. 18 Suppl: S7–13. PMID 9266501.
- ↑ Groneberg, DA.; Kindermann, B.; Althammer, M.; Klapper, M.; Vormann, J.; Littarru, GP.; Döring, F. (2005). "Coenzyme Q10 affects expression of genes involved in cell signalling, metabolism and transport in human CaCo-2 cells". Int J Biochem Cell Biol. 37 (6): 1208–18. doi:10.1016/j.biocel.2004.11.017. PMID 15778085. Unknown parameter
|month=ignored (help) - ↑ Nathalie Soucheta and Serge Laplante, Seasonal variation of Co-enzyme Q10 content in pelagic fish tissues from Eastern Quebec
- ↑ www.thefactsaboutfitness.com
- ↑ Berbel-Garcia, A. (2004). "Coenzyme Q 10 improves lactic acidosis, strokelike episodes, and epilepsy in a patient with MELAS". Clinical Neuropharmacology. 27: 187–191. PMID 15319706. Unknown parameter
|coauthors=ignored (help); Unknown parameter|month=ignored (help);|access-date=requires|url=(help) - ↑ Folkers, K.; Littarru, GP.; Ho, L.; Runge, TM.; Havanonda, S.; Cooley, D. (1970). "Evidence for a deficiency of coenzyme Q10 in human heart disease". Int Z Vitaminforsch. 40 (3): 380–90. PMID 5450999.
- ↑ Littaru, GP.; Ho, L.; Folkers, K. (1972). "Deficiency of coenzyme Q 10 in human heart disease. I.". Int J Vitam Nutr Res. 42 (2): 291–305. PMID 5053855.
- ↑ Folkers, K.; Vadhanavikit, S.; Mortensen, SA. (1985). "Biochemical rationale and myocardial tissue data on the effective therapy of cardiomyopathy with coenzyme Q10". Proc Natl Acad Sci U S A. 82 (3): 901–4. PMID 3856239. Unknown parameter
|month=ignored (help) - ↑ Rosenfeldt, FL.; Haas, SJ.; Krum, H.; Hadj, A.; Ng, K.; Leong, JY.; Watts, GF. (2007). "Coenzyme Q10 in the treatment of hypertension: a meta-analysis of the clinical trials". J Hum Hypertens. 21 (4): 297–306. doi:10.1038/sj.jhh.1002138. PMID 17287847. Unknown parameter
|month=ignored (help) - ↑ Tiano, L.; Belardinelli, R.; Carnevali, P.; Principi, F.; Seddaiu, G.; Littarru, GP. (2007). "Effect of coenzyme Q10 administration on endothelial function and extracellular superoxide dismutase in patients with ischaemic heart disease: a double-blind, randomized controlled study". Eur Heart J. 28 (18): 2249–55. doi:10.1093/eurheartj/ehm267. PMID 17644511. Unknown parameter
|month=ignored (help) - ↑ Landmesser, U.; Merten, R.; Spiekermann, S.; Büttner, K.; Drexler, H.; Hornig, B. (2000). "Vascular extracellular superoxide dismutase activity in patients with coronary artery disease: relation to endothelium-dependent vasodilation". Circulation. 101 (19): 2264–70. PMID 10811593. Unknown parameter
|month=ignored (help) - ↑ "related:mdvAhRE800UJ:scholar.google.com/ - Google Scholar". Retrieved 28 May 2013. External link in
|title=(help) - ↑ Belardinelli, R.; Muçaj, A.; Lacalaprice, F.; Solenghi, M.; Seddaiu, G.; Principi, F.; Tiano, L.; Littarru, GP. (2006). "Coenzyme Q10 and exercise training in chronic heart failure". Eur Heart J. 27 (22): 2675–81. doi:10.1093/eurheartj/ehl158. PMID 16882678. Unknown parameter
|month=ignored (help) - ↑ Fotino, AD.; Thompson-Paul, AM.; Bazzano, LA. (2013). "Effect of coenzyme Q₁₀ supplementation on heart failure: a meta-analysis". Am J Clin Nutr. 97 (2): 268–75. doi:10.3945/ajcn.112.040741. PMID 23221577. Unknown parameter
|month=ignored (help) - ↑ http://www.escardio.org/about/press/press-releases/pr-13/Pages/first-drug-in-decade-improves-heart-failure-mortality.aspx
- ↑ Kishi T, Watanabe T, Folkers K (1977). "Bioenergetics in clinical medicine XV. Inhibition of coenzyme Q10-enzymes by clinically used adrenergic blockers of beta-receptors". Res Commun Chem Pathol Pharmacol. 17 (1): 157–64. PMID 17892.
- ↑ The Synthesis of Cholesterol
- ↑ Ghirlanda G, Oradei A, Manto A, Lippa S, Uccioli L, Caputo S, Greco A, Littarru G (1993). "Evidence of plasma CoQ10-lowering effect by HMG-CoA reductase inhibitors: a double-blind, placebo-controlled study". J Clin Pharmacol. 33 (3): 226–9. PMID 8463436.
- ↑ Sarter B (2002). "Coenzyme Q10 and cardiovascular disease: a review". J Cardiovasc Nurs. 16 (4): 9–20. PMID 12597259.
- ↑ Thibault A, Samid D, Tompkins A, Figg W, Cooper M, Hohl R, Trepel J, Liang B, Patronas N, Venzon D, Reed E, Myers C (1996). "Phase I study of lovastatin, an inhibitor of the mevalonate pathway, in patients with cancer". Clin Cancer Res. 2 (3): 483–91. PMID 9816194.
- ↑
Damian, M. S. (2004). "Coenzyme Q10 Combined With Mild Hypothermia After Cardiac Arrest". Circulation, American Heart Foundation. 110: 3011–3016. Retrieved 2006-12-01. Unknown parameter
|month=ignored (help); Unknown parameter|coauthors=ignored (help) - ↑ Rozen T, Oshinsky M, Gebeline C, Bradley K, Young W, Shechter A, Silberstein S (2002). "Open label trial of coenzyme Q10 as a migraine preventive". Cephalalgia. 22 (2): 137–41. PMID 11972582.
- ↑ Sándor PS; et al. (2005). "Efficacy of coenzyme Q10 in migraine prophylaxis: A randomized controlled trial". Neurology. 64: 713–715.
- ↑ Katsuhisa Sakano, Mami Takahashi, Mitsuaki Kitano, Takashi Sugimura, Keiji Wakabayashi: Suppression of Azoxymethane-induced Colonic Premalignant Lesion Formation by Coenzyme Q10 in Rats. Asian Pacific J Cancer Prev, 7, 599-603, 2006
- ↑ Matthews, R. T. (1998). "Coenzyme Q10 administration increases brain mitochondrial concentrations and exerts neuroprotective effects". PNAS. 95: 8892–8897. Retrieved 2006-12-01. Unknown parameter
|month=ignored (help); Unknown parameter|coauthors=ignored (help) - ↑ Biol Signals Recept. 2001 May-Aug;10(3-4):224-53
- ↑ Alexander Storch, MD; Wolfgang H. Jost, MD; Peter Vieregge, MD; Jörg Spiegel, MD; Wolfgang Greulich, MD; Joachim Durner, MD; Thomas Müller, MD; Andreas Kupsch, MD; Henning Henningsen, MD; Wolfgang H. Oertel, MD; Gerd Fuchs, MD; Wilfried Kuhn, MD; Petra Niklowitz, MD; Rainer Koch, PhD; Birgit Herting, MD; Heinz Reichmann, MD; for the German Coenzyme Q10 Study Group (May 14, 2007). "Randomized, Double-blind, Placebo-Controlled Trial on Symptomatic Effects of Coenzyme Q10 in Parkinson Disease". Archives of Neurologu.
- ↑ Quiles JL, Ochoa JJ, Huertas JR, Mataix J (2004). "Coenzyme Q supplementation protects from age-related DNA double-strand breaks and increases lifespan in rats fed on a PUFA-rich diet". Exp Gerontol. 39 (2): 189–94. PMID 15036411.
bg:Коензим Q cs:Koenzym Q10 de:Ubichinon it:Coenzima Q nl:Co-enzym Q10 oc:Coenzim Q10 sl:Ubikinon fi:Ubikinoni uk:Убіхінон