Ankle fracture: Difference between revisions
No edit summary |
No edit summary |
||
| (48 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
[[File: | [[File:Ankle-fracture-weber A.jpg|thumb]] | ||
__NOTOC__ | __NOTOC__ | ||
{{Infobox_Disease | | {{Infobox_Disease | | ||
| Line 20: | Line 21: | ||
{{CMG}}; {{AE}}[[User:DrMars|Mohammadmain Rezazadehsaatlou[2]]]. | {{CMG}}; {{AE}}[[User:DrMars|Mohammadmain Rezazadehsaatlou[2]]]. | ||
==Overview== | ==Overview<ref name="pmid28758439">{{cite journal |vauthors=Mason LW, Marlow WJ, Widnall J, Molloy AP |title=Pathoanatomy and Associated Injuries of Posterior Malleolus Fracture of the Ankle |journal=Foot Ankle Int |volume=38 |issue=11 |pages=1229–1235 |date=November 2017 |pmid=28758439 |doi=10.1177/1071100717719533 |url=}}</ref><ref name="pmid28348185">{{cite journal |vauthors=Mittal R, Harris IA, Adie S, Naylor JM |title=Surgery for Type B Ankle Fracture Treatment: a Combined Randomised and Observational Study (CROSSBAT) |journal=BMJ Open |volume=7 |issue=3 |pages=e013298 |date=March 2017 |pmid=28348185 |pmc=5372107 |doi=10.1136/bmjopen-2016-013298 |url=}}</ref><ref name="pmid28624992">{{cite journal |vauthors=Winge R, Bayer L, Gottlieb H, Ryge C |title=Compression therapy after ankle fracture surgery: a systematic review |journal=Eur J Trauma Emerg Surg |volume=43 |issue=4 |pages=451–459 |date=August 2017 |pmid=28624992 |doi=10.1007/s00068-017-0801-y |url=}}</ref>== | ||
The | The ankle joint is consisted of 2 different joints: | ||
'''1: The true ankle joint (Responsible for the dorsiflexion and plantar flexion movements of the ankle joint): It is consisted of three bone:''' | |||
''a: The tibia (medial ankle)'' | |||
''b: The fibula (lateral ankle)'' | |||
''c: The talus (the floor upon which the tibia and fibula rest).'' | |||
'''2: The subtalar joint (Responsible for the invertion and evertion of foot)''': | |||
''a: The talus'' | |||
''b: The calcaneus'' | |||
A combination of ankle bones, joint capsule, and ligaments system are responsible for the stability of the ankle joint. | |||
syndesmosis of this stabilizing system are | |||
Anterior tibiofibular ligament | |||
Posterior tibiofibular ligament | |||
Transverse tibiofibular ligament | |||
Interosseous membrane | |||
Generally, there are three sub-groups for the the ankle joint based on the location of the the tibia and fibula: | |||
* Medial malleolus - inside part of the tibia | |||
* Posterior malleolus - back part of the tibia | |||
* Lateral malleolus - end of the fibula | |||
Accordingly, there are thee type of ankle fracture invovlement: | |||
A '''unimalleolar fracture''' | |||
Involves either the distal fibula (more common) or the distal tibia | |||
A '''bimalleolar fracture''' | |||
Involves the lateral malleolus and the medial malleolus. | |||
A '''trimalleolar fracture''' | |||
Involves the lateral malleolus, the medial malleolus, and the distal posterior aspect of the tibia. | |||
== Historical Perspective <ref name="pmid28276651">{{cite journal |vauthors=Guo CJ, Li XC, Hu M, Xu Y, Xu XY |title=Realignment Surgery for Malunited Ankle Fracture |journal=Orthop Surg |volume=9 |issue=1 |pages=49–53 |date=February 2017 |pmid=28276651 |doi=10.1111/os.12312 |url=}}</ref><ref name="pmid26691309">{{cite journal |vauthors=Jonckheer P, Willems T, De Ridder R, Paulus D, Holdt Henningsen K, San Miguel L, De Sutter A, Roosen P |title=Evaluating fracture risk in acute ankle sprains: Any news since the Ottawa Ankle Rules? A systematic review |journal=Eur J Gen Pract |volume=22 |issue=1 |pages=31–41 |date=2016 |pmid=26691309 |doi=10.3109/13814788.2015.1102881 |url=}}</ref>== | |||
There are no reliable information regarding the historical perspective of the Ankle bone fracture but | |||
In 1758, Percival Pott described three types of ankle fractures based on the number of malleoli involved as: unimalleolar, bimalleolar, and trimalleolar. Despite its ease of use it failed to differentiate stable from unstable types. | |||
In 1949, a Danish physician, Niel Lauge-Hansen created a classification system based on a rotational mechanism of injury and he published his great work in a 1950 issue of ''Archives of Surgery,'' | |||
== Causes <ref name="pmid29079241">{{cite journal |vauthors=Elmajee M, Rafee A, Williams T |title=Ankle Fracture Associated With Rupture of the Achilles Tendon: Case Report and Review of the Literature |journal=J Foot Ankle Surg |volume=56 |issue=6 |pages=1320–1322 |date=2017 |pmid=29079241 |doi=10.1053/j.jfas.2017.05.043 |url=}}</ref><ref name="pmid29162365">{{cite journal |vauthors=González-Lucena G, Pérez-Prieto D, López-Alcover A, Ginés-Cespedosa A |title=Ankle fracture controversies: Do the foot and ankle specialists have a different vision? |journal=Rev Esp Cir Ortop Traumatol |volume=62 |issue=1 |pages=27–34 |date=2018 |pmid=29162365 |doi=10.1016/j.recot.2017.10.001 |url=}}</ref>== | |||
* Pressure during car accidents | |||
* Twisted ankle side to side | |||
* Rotated ankle side to side | |||
* Rolling ankle in or out | |||
* Hyper-flextion | |||
* Hyper-Extention | |||
* Tripping | |||
* Falling from a height | |||
* Jumping from a height | |||
As a person age, two factors cause higher risk of fractures: | |||
* Weaker bones | |||
* Greater risk of falling | |||
Stress fractures as a common causes of fractures can be found due to the repeated stresses and strains. Importantly children having more physically active lifestyles than adults, are also prone to fractures. People with any underlying diseases such as osteoporosis, infection, or a tumor affecting their bones having a higher risk of fractures. As mentioned in previous chapters, this type of fracture is known as a pathological fracture. Stress fractures, which result from repeated stresses and strains, commonly found among professional sports people, are also common causes of fractures. | |||
===Life-threatening Causes=== | |||
*There are no life-threatening causes of [[Ankle fracture]] ''',''' however complications resulting from [[Ankle fracture]] is common. | |||
===Common Causes=== | |||
Common causes of [[Ankle fracture]] may include: | |||
*[[Trauma]] | |||
== | ===Less Common Causes=== | ||
Less common causes of '''[[Ankle fracture]]''' include conditions that predisposes to fracture: | |||
*[[Osteoporosis]] | |||
*[[Osteopenia]] | |||
*[[Malignancy|Malignancies]] | |||
===Causes by Organ System=== | |||
== | {| style="width:80%; height:100px" border="1" | ||
| style="width:25%" bgcolor="LightSteelBlue" ; border="1" |'''Cardiovascular''' | |||
| style="width:75%" bgcolor="Beige" ; border="1" | No underlying causes | |||
|- | |||
| bgcolor="LightSteelBlue" | '''Chemical/Poisoning''' | |||
| bgcolor="Beige" | No underlying causes | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
| '''Dental''' | |||
| bgcolor="Beige" | No underlying causes | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
| '''Dermatologic''' | |||
| bgcolor="Beige" | No underlying causes | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
| '''Drug Side Effect''' | |||
| bgcolor="Beige" | No underlying causes | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
| '''Ear Nose Throat''' | |||
| bgcolor="Beige" | No underlying causes | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
| '''Endocrine''' | |||
| bgcolor="Beige" | No underlying causes | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
| '''Environmental''' | |||
| bgcolor="Beige" | No underlying causes | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
| '''Gastroenterologic''' | |||
| bgcolor="Beige" | No underlying causes | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
| '''Genetic''' | |||
| bgcolor="Beige" | No underlying causes | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
| '''Hematologic''' | |||
| bgcolor="Beige" | No underlying causes | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
| '''Iatrogenic''' | |||
| bgcolor="Beige" | No underlying causes | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
| '''Infectious Disease''' | |||
| bgcolor="Beige" | No underlying causes | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
| '''Musculoskeletal/Orthopedic''' | |||
| bgcolor="Beige" | [[Osteoporosis]] and [[osteopenia]]. | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
| '''Neurologic''' | |||
| bgcolor="Beige" | No underlying causes | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
| '''Nutritional/Metabolic''' | |||
| bgcolor="Beige" | [[Osteoporosis]] and [[osteopenia]]. | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
| '''Obstetric/Gynecologic''' | |||
| bgcolor="Beige" | No underlying causes | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
| '''Oncologic''' | |||
| bgcolor="Beige" | No underlying causes | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
| '''Ophthalmologic''' | |||
| bgcolor="Beige" | No underlying causes | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
| '''Overdose/Toxicity''' | |||
| bgcolor="Beige" | No underlying causes | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
| '''Psychiatric''' | |||
| bgcolor="Beige" | No underlying causes | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
| '''Pulmonary''' | |||
| bgcolor="Beige" | No underlying causes | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
| '''Renal/Electrolyte''' | |||
| bgcolor="Beige" | No underlying causes | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
| '''Rheumatology/Immunology/Allergy''' | |||
| bgcolor="Beige" | No underlying causes | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
| '''Sexual''' | |||
| bgcolor="Beige" | No underlying causes | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
| '''Trauma''' | |||
| bgcolor="Beige" | Falling of car accident to on side of Ankle . | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
| '''Urologic''' | |||
| bgcolor="Beige" | No underlying causes | |||
|- | |||
|- bgcolor="LightSteelBlue" | |||
| '''Miscellaneous''' | |||
| bgcolor="Beige" | No underlying causes | |||
|- | |||
|} | |||
== | ===Causes in Alphabetical Order=== | ||
List the causes of the disease in alphabetical order: | |||
<div style="-moz-column-count:3; column-count:3;"> | |||
* [[Trauma]] | |||
* [[Osteopenia]] | |||
* [[Osteoporosis]] | |||
</div> | |||
=== | == Pathophysiology <ref name="pmid27261811">{{cite journal |vauthors=Ortiz CA, Wagner P, Wagner E |title=State-of-the-Art in Ankle Fracture Management in Chile |journal=Foot Ankle Clin |volume=21 |issue=2 |pages=367–89 |date=June 2016 |pmid=27261811 |doi=10.1016/j.fcl.2016.01.008 |url=}}</ref>== | ||
The [[ | The main etiology of the [[Ankle fracture]] is thought to excessive inversion stress to the ankle joint. | ||
The ankle is more stable and resistant to eversion injuries than inversion injuries Because: | |||
The medial malleolus is shorter than the lateral malleolus causing higher range of the invertion than evertion of the talus bone. | |||
The deltoid ligament stabilized the medial wall of the ankle joint | |||
=== Pathophysiology === | On the other hand, the transverse malleolar, Vertical malleolar, and posterior malleolar fractures are associated with an avulsion injury, talar impaction, and other bone and/or ligamentous injury, respectively. | ||
Its known that the [[ | |||
=== Mechanism <ref name="pmid27984688">{{cite journal |vauthors=Cuzmar-Grimalt D, Escudero-Heldt M, Aldunate-González JT, Plaza-Guzmán N |title=[Ankle fracture in adolescents: triplanar injury associated to fracture of leg] |language=Spanish; Castilian |journal=Acta Ortop Mex |volume=30 |issue=3 |pages=144–146 |date=2016 |pmid=27984688 |doi= |url=}}</ref>=== | |||
In 80% of ankle fractures the foot is in supination position while, in 20% of fractures the foot is in pronation position. The [[Ankle fracture]] is caused by a falling or direct trauma to the ankle joint. The form and severity of this fracture depends on the position of the ankle joint at the moment of the trauma. The ankle joint is flexible but the medial side of the ankle joint is rigid because the medial malleolus is attached to the tibia and also the medial collateral ligaments are very strong. Also, lateral wall of the ankle include: the fibula, syndesmosis and lateral collateral ligaments play important rolls in this flexibility. This lateral wall of the ankle allows the talus to move in lateral and dorsal sides easily. The fibula has no weight-bearing roll but it provide a flexible lateral support. The syndesmosis is formed by the anterior and posterior tibiofibular ligaments which is the fibrous connection between the fibula and tibia. | |||
If we imagine the ankle as a ring in which bones and ligaments play an important role in the maintaining the stability of this joint. Meanwhile, if this ring is broken in one place it remains stable but when it is broken in two places, the ring is unstable and it is at the higher risk of fracture. Consequently the ankle is unstable when both the medial and the lateral malleoli are fractured. | |||
=== Pathophysiology <ref name="pmid28639869">{{cite journal |vauthors=Stull JD, Bhat SB, Kane JM, Raikin SM |title=Economic Burden of Inpatient Admission of Ankle Fractures |journal=Foot Ankle Int |volume=38 |issue=9 |pages=997–1004 |date=September 2017 |pmid=28639869 |doi=10.1177/1071100717709576 |url=}}</ref><ref name="pmid30468054">{{cite journal |vauthors=Hong X, Bao CS, Zheng WL |title=Inference on Injury Mechanism of Ankle Fracture by Lauge-Hansen Classification |journal=Fa Yi Xue Za Zhi |volume=34 |issue=5 |pages=512–515 |date=October 2018 |pmid=30468054 |doi=10.12116/j.issn.1004-5619.2018.05.015 |url=}}</ref>=== | |||
Its known that the [[Ankle fracture]] in normal healthy adults can be caused due to the high-energy trauma (e.g., motor vehicle accidents), sport related injuries, falling from height. But it should be noted that the most important Risk factors for insufficiency fractures is chronic metabolic disease such as steoporosis, osteopenia, eating-disordered behavior, higher age, prolonged corticosteroid usage, female gender, lower BMI, history of a recent falling, and prior fracture. | |||
* The pattern of bone fracture and severity of injury depends on variety of factors such as: | * The pattern of bone fracture and severity of injury depends on variety of factors such as: | ||
** Patients age | ** Patients age | ||
| Line 48: | Line 241: | ||
** As [[Osteocyte|osteocytes]] grow, viability of cells decrease thereby decreasing the bone mass density. | ** As [[Osteocyte|osteocytes]] grow, viability of cells decrease thereby decreasing the bone mass density. | ||
==Differentiating | ==Differentiating [[Ankle fracture]] from other Diseases <ref name="pmid28249677">{{cite journal |vauthors=Ashton F, Hamid K, Sulieman S, Eardley W, Baker P |title=Factors Influencing patient experience and satisfaction following surgical management of ankle fractures |journal=Injury |volume=48 |issue=4 |pages=960–965 |date=April 2017 |pmid=28249677 |doi=10.1016/j.injury.2017.02.017 |url=}}</ref><ref name="pmid29078057">{{cite journal |vauthors=Woo SH, Bae SY, Chung HJ |title=Short-Term Results of a Ruptured Deltoid Ligament Repair During an Acute Ankle Fracture Fixation |journal=Foot Ankle Int |volume=39 |issue=1 |pages=35–45 |date=January 2018 |pmid=29078057 |doi=10.1177/1071100717732383 |url=}}</ref>== | ||
In the orthopedic medicine its important to know that the | In the orthopedic medicine its important to know that the ankle fracture should be evaluated using radiography for both confirming diagnosis and also for evaluating the surrounding tissues. | ||
* Acute compartment syndrome of ankle joint | |||
* Ankle Dislocation | |||
* Soft tissue Injury around the ankle , | |||
* | * Deep Venous thrombosis | ||
* | * Thrombophlebitis | ||
* Foot Fracture | |||
* Gout | |||
* Pseudogout | |||
* Rheumatoid Arthritis | |||
* Tibia Fracture | |||
* Fibula Fracture | |||
* bimalleolar fracture | |||
* trimalleolar fracture | |||
* triplane fracture | |||
* Tillaux fracture | |||
* Bosworth fracture | |||
* '''pilon fracture''' | |||
* Wagstaffe-Le Forte fracture | |||
* Charcot-Marie-Tooth disease: in cases with repeated ankle fractures | |||
==Epidemiology and Demographics == | ==Epidemiology and Demographics<ref name="pmid24856790">{{cite journal |vauthors=Thakore RV, Hooe BS, Considine P, Sathiyakumar V, Onuoha G, Hinson JK, Obremskey WT, Sethi MK |title=Ankle fractures and employment: a life-changing event for patients |journal=Disabil Rehabil |volume=37 |issue=5 |pages=417–22 |date=2015 |pmid=24856790 |doi=10.3109/09638288.2014.923525 |url=}}</ref><ref name="pmid29252652">{{cite journal |vauthors=Krishna SV, Pilar A, Pai SN, Issac T |title=Traumatic Rupture of Posterior Tibial Tendon Following Closed Supination-Adduction Ankle Fracture: A Case Report |journal=JBJS Case Connect |volume=6 |issue=3 |pages=e75 |date=2016 |pmid=29252652 |doi=10.2106/JBJS.CC.15.00273 |url=}}</ref> == | ||
Of all cases with the ankle injuries only 15% of cases are true ankle fractures. The male-to-female ratio for ankle fracture is 2:1. The frequency of ankle fractures in adults and children is around 100 cases in 100,000 per year and 190 cases in 100,000 per year, respectively. | |||
==Risk Factors == | ==Risk Factors <ref name="pmid28865579">{{cite journal |vauthors=van Zuuren WJ, Schepers T, Beumer A, Sierevelt I, van Noort A, van den Bekerom MPJ |title=Acute syndesmotic instability in ankle fractures: A review |journal=Foot Ankle Surg |volume=23 |issue=3 |pages=135–141 |date=September 2017 |pmid=28865579 |doi=10.1016/j.fas.2016.04.001 |url=}}</ref>== | ||
There are different risk factors that presidpose patient for the [[ | There are different risk factors that presidpose patient for the [[Ankle fracture]] that include: | ||
* High-risk contact sports | * High-risk contact sports | ||
* Higher age (elderly adults are higher prone to such fractures) | * Higher age (elderly adults are higher prone to such fractures) | ||
| Line 66: | Line 273: | ||
* Direct blow | * Direct blow | ||
* Road / traffic accidents | * Road / traffic accidents | ||
* Falling | * Falling | ||
* Direct trauma to the | * Direct trauma to the ankle | ||
* Taking part in any rough or high-impact sport | * Taking part in any rough or high-impact sport | ||
* Street fights, gunshot wounds, and domestic violence, may also cause the | * Street fights, gunshot wounds, and domestic violence, may also cause the Ankle fracture | ||
* Road traffic accidents. | * Road traffic accidents. | ||
== Classification == | == Classification <ref name="pmid27645617">{{cite journal |vauthors=Juto H, Möller M, Wennergren D, Edin K, Apelqvist I, Morberg P |title=Substantial accuracy of fracture classification in the Swedish Fracture Register: Evaluation of AO/OTA-classification in 152 ankle fractures |journal=Injury |volume=47 |issue=11 |pages=2579–2583 |date=November 2016 |pmid=27645617 |doi=10.1016/j.injury.2016.05.028 |url=}}</ref><ref name="pmid29182957">{{cite journal |vauthors=Boszczyk A, Fudalej M, Kwapisz S, Klimek U, Maksymowicz M, Kordasiewicz B, Rammelt S |title=Ankle fracture - Correlation of Lauge-Hansen classification and patient reported fracture mechanism |journal=Forensic Sci. Int. |volume=282 |issue= |pages=94–100 |date=January 2018 |pmid=29182957 |doi=10.1016/j.forsciint.2017.11.023 |url=}}</ref><ref name="pmid28633779">{{cite journal |vauthors=Briet JP, Houwert RM, Smeeing DPJ, Dijkgraaf MGW, Verleisdonk EJ, Leenen LPH, Hietbrink F |title=Differences in Classification Between Mono- and Polytrauma and Low- and High-Energy Trauma Patients With an Ankle Fracture: A Retrospective Cohort Study |journal=J Foot Ankle Surg |volume=56 |issue=4 |pages=793–796 |date=2017 |pmid=28633779 |doi=10.1053/j.jfas.2017.04.012 |url=}}</ref> <ref name="pmid28416839">{{cite journal |vauthors=Gong XF, Lyu YW, Wang JH, Wang Y, Wu Y, Wang MY |title=[A correlation analysis of the ankle CT and ankle fracture classification] |language=Chinese |journal=Beijing Da Xue Xue Bao |volume=49 |issue=2 |pages=281–285 |date=April 2017 |pmid=28416839 |doi= |url=}}</ref>== | ||
The | The Ankle fracture may be classified based on the exact location of fracture: | ||
The '''Weber ankle fracture classification''' (or '''Danis-Weber classification''') can b used to classify the lateral malleolar fractures. | |||
{| class="wikitable" | |||
|+'''Weber ankle fracture classification''' (or '''Danis-Weber classification''') | |||
!Type | |||
! | |||
! | |||
! | |||
|- | |||
|A | |||
| | |||
* Usually transverse | |||
* Under the level of the talar dome | |||
* Tibiofibular syndesmosis is intact | |||
* Deltoid ligament is intact | |||
* Medial malleolus maybe affected | |||
* Usually stable if medial malleolus intact | |||
| | |||
* '''Stage 1''' - Tension on the lateral collateral ligaments cause | |||
the rupture of the ligaments | |||
==Screening== | ''or'' | ||
avulsion of the lateral malleolus below the syndesmosis. | |||
* '''Stage 2''' - Oblique fracture of the medial malleolus. | |||
|[[File:Ankle-fracture-weber A.jpg|alt=Ankle-fracture-weber A|thumb|390x390px|'''Ankle-fracture-weber A''']] | |||
|- | |||
|B | |||
| | |||
* Usually spiral | |||
* Distal extent at the level of the talar dome | |||
* Tibiofibular syndesmosis usually is intact | |||
* Deltoid ligament may be injured | |||
* Medial malleolus maybe fractured | |||
* Variable stability dependening on the medial structures | |||
* May require ORIF | |||
| | |||
* '''Stage 1''' - Rupture of the anterior syndesmosis | |||
* '''Stage 2''' - Oblique fracture of the fibula (the true Weber B fracture) | |||
* '''Stage 3''' - Rupture of the posterior syndesmosis ''or'' - fracture of the posterior malleolus | |||
* '''Stage 4''' - Avulsion of the medial malleolus ''or'' - rupture of the medial collateral bands | |||
|[[File:Ankle-fracture-weber-B.jpg|alt=Ankle-fracture-weber-B|thumb|'''Ankle-fracture-weber-B''']] | |||
|- | |||
|C | |||
| | |||
* Above the level of the ankle joint | |||
* Tibiofibular syndesmosis is injured | |||
* Deltoid ligament is injured | |||
* Medial malleolus maybe fractured | |||
* Fracture may arise as proximally as the level of fibular neck and not visualized on ankle films, requiring knee or full-length tibia-fibula radiographs (Maisonneuve fracture) | |||
* Unstable: | |||
* Usually requires ORIF | |||
| | |||
** '''Stage 1''' - Avulsion of the medial malleolus ''or'' - ligamentous rupture | |||
** '''Stage 2''' - Rupture of the anterior syndesmosis | |||
** '''Stage 3''' - Fibula fracture above the level of the syndesmosis (this is the true Weber C fracture) | |||
** '''Stage 4''' - Avulsion of the posterior malleolus ''or'' - rupture of the posterior syndesmosis | |||
|[[File:Ankle-fracture-weber-C.jpg|alt=Ankle-fracture-weber-C|thumb|'''Ankle-fracture-weber-C''']] | |||
|} | |||
The '''Lauge-Hansen classification''' system is also for the ankle injuries based on injury mechanisms. This classification system uses two words: | |||
* The first word describes the position of the foot during the injury such as: supination and pronation. | |||
* The second word describes the direction of the deforming force such as abduction, adduction, or external rotation. | |||
Accordingly, at least 13 different patterns have been described: | |||
{| class="wikitable" | |||
!Grade | |||
!Sequence | |||
|- | |||
|Supination-Adduction | |||
|Stage 1: With no medial malleolar fracture '''(Weber A)''' | |||
Stage 2: With oblique or vertical medial malleolar fracture | |||
|- | |||
|Supination-External rotation | |||
(40-70% of injuries) | |||
|Stage 1: Tear or avulsion of the anteroinferior tibiofibular ligament is torn or avulsed | |||
Stage 2: The talus displaces and fractures the fibula in an oblique or spiral fracture, starting at the joint '''(Weber B)''' | |||
Stage 3: Tear of the posteroinferior tibiofibular ligament or fracture posterior malleolus | |||
Stage 4: Tear of the deltoid ligament or transverse avulsion fracture medial malleolus | |||
|- | |||
|Pronation-Abduction | |||
|stage 1: Deltoid ligament disruption or transverse medial malleolus fracture | |||
stage 2: Posterior malleolus fracture | |||
stage 3: Oblique fibular fracture '''(Weber C)''' | |||
|- | |||
|Pronation-External rotation | |||
|stage 1: Deltoid ligament rupture, which may appear occult or as medial mortise widening, or transverse avulsion fracture of the medial malleolus | |||
stage 2: Involvement of the AITFL with extension into the interosseous membrane results in widening of the distal tibiofibular distance | |||
stage 3: A spiral or oblique fibular fracture (>6 cm) at the level or above the talotibial joint '''(Weber C)''' stage 4: Involvement of the posterior inferior tibiofibular ligament (PITFL), or posterior malleolus fracture | |||
|} | |||
AO/OTA classification of tibial malleolar fractures | |||
{| class="wikitable" | |||
|+'''AO/OTA classification of tibial malleolar fractures''' | |||
|Infrasyndesmotic | |||
| colspan="1" rowspan="1" |44-A1 | |||
44-A2 | |||
44-A3 | |||
|isolated fibula fracture | |||
fibula fracture with a medial malleolar involvement | |||
fibular fracturewith a posteromedial involvement | |||
|- | |||
|Transsyndesmotic | |||
| colspan="1" rowspan="1" |44-B1 | |||
44-B2 | |||
44-B3 | |||
| colspan="1" rowspan="1" |isolated fibula fracture | |||
fibula fracture with a medial involvement | |||
fibula fracture with a medial injury and the posterolateral rim involvement (Volkmann’s fragment) | |||
|- | |||
|Suprasyndesmotic | |||
| colspan="1" rowspan="1" |44-C1 | |||
44-C2 | |||
44-C3 | |||
| colspan="1" rowspan="1" |simple diaphyseal fibula fracture | |||
wedge or multifragmentary diaphyseal fibula involvement | |||
proximal fibula fracture | |||
|} | |||
==Screening<ref name="pmid29287221">{{cite journal |vauthors=Walsh AS, Sinclair V, Watmough P, Henderson AA |title=Ankle fractures: Getting it right first time |journal=Foot (Edinb) |volume=34 |issue= |pages=48–52 |date=March 2018 |pmid=29287221 |doi=10.1016/j.foot.2017.11.013 |url=}}</ref>== | |||
Osteoporosis is an important risk factor for human affecting human bone especially in men with the age of older than 50 years old and [[postmenopausal]] and women. | Osteoporosis is an important risk factor for human affecting human bone especially in men with the age of older than 50 years old and [[postmenopausal]] and women. | ||
| Line 84: | Line 419: | ||
* · Women with the age of 65≤ year old, with no previous history of pathological [[fracture]] due to the [[osteoporosis]] | * · Women with the age of 65≤ year old, with no previous history of pathological [[fracture]] due to the [[osteoporosis]] | ||
* · Women with the age of <65 years, with 10-year [[fracture]] risk of not less than a 65-year-old white woman (who has not any other risk factor) | * · Women with the age of <65 years, with 10-year [[fracture]] risk of not less than a 65-year-old white woman (who has not any other risk factor) | ||
Accordingly women older than age of 50 are the main target for the [[osteoporosis]] screening. There is no specific recommendation to screen men for the [[osteoporosis]]. | Accordingly women older than age of 50 are the main target for the [[osteoporosis]] screening. There is no specific recommendation to screen men for the [[osteoporosis]]. | ||
The [[USPSTF]] recommendations from 2002 included: | The [[USPSTF]] recommendations from 2002 included: | ||
| Line 101: | Line 436: | ||
· Women with advanced [[osteopenia]]: T-score of −2.00 to −2.49 - should have screening for 1 year. | · Women with advanced [[osteopenia]]: T-score of −2.00 to −2.49 - should have screening for 1 year. | ||
==Natural History, Complications and Prognosis == | ==Natural History, Complications and Prognosis <ref name="pmid26190633">{{cite journal |vauthors=Neilly D, Baliga S, Munro C, Johnston A |title=Acute compartment syndrome of the foot following open reduction and internal fixation of an ankle fracture |journal=Injury |volume=46 |issue=10 |pages=2064–8 |date=October 2015 |pmid=26190633 |doi=10.1016/j.injury.2015.06.006 |url=}}</ref><ref name="pmid27886683">{{cite journal |vauthors=Denning JR |title=Complications of Pediatric Foot and Ankle Fractures |journal=Orthop. Clin. North Am. |volume=48 |issue=1 |pages=59–70 |date=January 2017 |pmid=27886683 |doi=10.1016/j.ocl.2016.08.010 |url=}}</ref>== | ||
=== Natural History === | === Natural History<ref name="pmid25278340">{{cite journal |vauthors=Hinds RM, Garner MR, Lazaro LE, Warner SJ, Loftus ML, Birnbaum JF, Burket JC, Lorich DG |title=Ankle fracture spur sign is pathognomonic for a variant ankle fracture |journal=Foot Ankle Int |volume=36 |issue=2 |pages=159–64 |date=February 2015 |pmid=25278340 |doi=10.1177/1071100714553470 |url=}}</ref> === | ||
In cases with untreated [[ | In cases with untreated [[Ankle fracture]] the malunion and deformity of arm can be occurred. | ||
=== Complications === | === Complications <ref name="pmid28826651">{{cite journal |vauthors=Toth MJ, Yoon RS, Liporace FA, Koval KJ |title=What's new in ankle fractures |journal=Injury |volume=48 |issue=10 |pages=2035–2041 |date=October 2017 |pmid=28826651 |doi=10.1016/j.injury.2017.08.016 |url=}}</ref>=== | ||
The overall complication rate in the treatment of [[ | The overall complication rate in the treatment of [[Ankle fracture]] were found in around 40% of cases: | ||
# Neurovascular compromise: such as Ulna nerve damage | # Neurovascular compromise: such as Ulna nerve damage | ||
# Compartment syndrome | # Compartment syndrome | ||
| Line 116: | Line 451: | ||
# Infection | # Infection | ||
# Refracture following plate removal | # Refracture following plate removal | ||
# | # Neural injury | ||
# Instability of the DRUJ | # Instability of the DRUJ | ||
# Loss of Motion (Stiffness) | # Loss of Motion (Stiffness) | ||
| Line 122: | Line 457: | ||
# Heterotopic Ossification | # Heterotopic Ossification | ||
=== Prognosis <ref name=" | === Prognosis <ref name="pmid24939377">{{cite journal |vauthors=Goost H, Wimmer MD, Barg A, Kabir K, Valderrabano V, Burger C |title=Fractures of the ankle joint: investigation and treatment options |journal=Dtsch Arztebl Int |volume=111 |issue=21 |pages=377–88 |date=May 2014 |pmid=24939377 |pmc=4075279 |doi=10.3238/arztebl.2014.0377 |url=}}</ref>=== | ||
Successful treatment of | Successful treatment of Ankle fracture depends on the on-time interventions such as: accurate diagnosis and appropriate treatment and referral. Complex open fractures with soft-tissue injuries have a worse prognosis than isolated closed ankle fractures. | ||
==Diagnosis<ref name="pmid28826651">{{cite journal |vauthors=Toth MJ, Yoon RS, Liporace FA, Koval KJ |title=What's new in ankle fractures |journal=Injury |volume=48 |issue=10 |pages=2035–2041 |date=October 2017 |pmid=28826651 |doi=10.1016/j.injury.2017.08.016 |url=}}</ref>== | |||
The diagnosis of a [[Ankle fracture]] should be confirmed using a radiographic examination. | |||
== | ==History and Symptoms <ref name="pmid25729514">{{cite journal |vauthors=Young KW, Kim JS, Cho JH, Kim HS, Cho HK, Lee KT |title=Paratrooper's ankle fracture: posterior malleolar fracture |journal=Clin Orthop Surg |volume=7 |issue=1 |pages=15–21 |date=March 2015 |pmid=25729514 |pmc=4329528 |doi=10.4055/cios.2015.7.1.15 |url=}}</ref>== | ||
The related signs and symptoms include: | The related signs and symptoms include: | ||
* Deformity | |||
* Skin lacerations | * Skin lacerations | ||
* Open fractures | * Open fractures | ||
* | * Erythema | ||
* | * Edema | ||
* Stiffness | * Stiffness | ||
* | * Decreased range of motion | ||
* | * Tenderness | ||
* Loss of function of the | * Loss of function of the leg | ||
* Difficulties in detection of pulses | * Difficulties in detection of pulses | ||
* | * Nerve damage | ||
In the physical exam the orthopedic surgeon should check the vascular status and amount of swelling in the | In the physical exam the orthopedic surgeon should check the vascular status and amount of swelling in the ankle. In MULTI-trauma patients or in comatose or obtunded patients a tense compartment with neurological signs or stretch pain should be considered as the [[compartment syndrome]], and the compartment pressures should be measured and monitored. Normally the pain and soft-tissue swelling are found at the injury site. This injury should be confirmed using a radiographic evaluations. | ||
==Physical Examination== | ==Physical Examination<ref name="pmid26485938">{{cite journal |vauthors=Ovaska M, Madanat R, Mäkinen T, Lindahl J |title=[Complications in ankle fracture surgery] |language=Finnish |journal=Duodecim |volume=131 |issue=16 |pages=1451–9 |date=2015 |pmid=26485938 |doi= |url=}}</ref><ref name="pmid26537162">{{cite journal |vauthors=Hsu RY, Lee Y, Hayda R, DiGiovanni CW, Mor V, Bariteau JT |title=Morbidity and Mortality Associated with Geriatric Ankle Fractures: A Medicare Part A Claims Database Analysis |journal=J Bone Joint Surg Am |volume=97 |issue=21 |pages=1748–55 |date=November 2015 |pmid=26537162 |doi=10.2106/JBJS.O.00095 |url=}}</ref><ref name="pmid25269609">{{cite journal |vauthors=Beckenkamp PR, Lin CW, Chagpar S, Herbert RD, van der Ploeg HP, Moseley AM |title=Prognosis of physical function following ankle fracture: a systematic review with meta-analysis |journal=J Orthop Sports Phys Ther |volume=44 |issue=11 |pages=841–51, B2 |date=November 2014 |pmid=25269609 |doi=10.2519/jospt.2014.5199 |url=}}</ref>== | ||
The related signs and symptoms include: | The related signs and symptoms include: | ||
* Edema of the | * Edema of the ankle | ||
** Most of the time the edema will be a non-pitting edema | ** Most of the time the edema will be a non-pitting edema | ||
** Depends on the edema extent, it may even lead to compartment syndrome in the anterior and internal compartment of | ** Depends on the edema extent, it may even lead to compartment syndrome in the anterior and internal compartment of the ankle | ||
* Bruising | * Bruising | ||
** As a manifestation of internal injury to the local vessels by trauma or fractures bone | ** As a manifestation of internal injury to the local vessels by trauma or fractures bone | ||
* Decrease in range of motion | * Decrease in range of motion of the ankle | ||
** Movement of the | ** Movement of the ankle will be painful if possible at all | ||
* Tenderness | * [[Tenderness]] | ||
* Deformity | * Deformity | ||
** Fractured bone deformity may be touchable in the internal side of the | ** Fractured bone deformity may be touchable in the internal side of the ankle if the fracture is displaced | ||
In the physical exam the orthopedic surgeon should check the vascular status and amount of swelling in the | In the physical exam the orthopedic surgeon should check the vascular status and amount of swelling in the ankle. In polytrauma patients or in comatose or obtunded patients a tense compartment with neurological signs or stretch pain should be considered as the [[compartment syndrome]], and the compartment pressures should be measured and monitored. | ||
Physical examination of patients with [[ | Physical examination of patients with [[Ankle fracture]] is usually remarkable for [[swelling]], [[tenderness]], [[Bruise|bruises]], [[ecchymosis]], [[deformity]] and restricted [[range of motion]] of the ankle. | ||
=== Appearance of the Patient === | === Appearance of the Patient === | ||
* Patients with [[ | * Patients with [[Ankle fracture]] usually appears normal unless the patients had a high energy trauma causing the open wound fracture. | ||
=== Vital Signs === | === Vital Signs === | ||
| Line 167: | Line 501: | ||
=== Skin === | === Skin === | ||
* Skin examination of patients with [[ | * Skin examination of patients with [[Ankle fracture]] includes: | ||
** [[Bruise|Bruises]] | ** [[Bruise|Bruises]] | ||
** [[Ecchymosis]] | ** [[Ecchymosis]] | ||
=== HEENT === | === HEENT === | ||
* HEENT examination of patients with [[ | * HEENT examination of patients with [[Ankle fracture]] usually normal. | ||
=== Neck === | === Neck === | ||
* Neck examination of patients with [[ | * Neck examination of patients with [[Ankle fracture]] is usually normal | ||
=== Lungs === | === Lungs === | ||
* Pulmonary examination of patients with [[ | * Pulmonary examination of patients with [[Ankle fracture]] usually normal | ||
=== Heart === | === Heart === | ||
* Cardiovascular examination of patients with [[ | * Cardiovascular examination of patients with [[Ankle fracture]] usually normal | ||
=== Abdomen === | === Abdomen === | ||
* Abdominal examination of patients with [[ | * Abdominal examination of patients with [[Ankle fracture]] usually normal | ||
=== Back === | === Back === | ||
* Back examination of patients with [[ | * Back examination of patients with [[Ankle fracture]] usually normal | ||
=== Genitourinary === | === Genitourinary === | ||
* Genitourinary examination of patients with [[ | * Genitourinary examination of patients with [[Ankle fracture]] usually normal | ||
=== Neuromuscular === | === Neuromuscular === | ||
* Neuromuscular examination of patients with [[ | * Neuromuscular examination of patients with [[Ankle fracture]] is usually normal | ||
* However, some patients may develop [[neuropraxia]] of the branch of the Ulnar nerve resulting in decreased sensation of thumb, index and middle finger. | * However, some patients may develop [[neuropraxia]] of the branch of the Ulnar nerve resulting in decreased sensation of thumb, index and middle finger. | ||
==Laboratory Findings== | ==Laboratory Findings<ref name="pmid25554425">{{cite journal |vauthors=Yousri T, Jackson M |title=Ankle fractures: When can I drive, doctor? A simulation study |journal=Injury |volume=46 |issue=2 |pages=399–404 |date=February 2015 |pmid=25554425 |doi=10.1016/j.injury.2014.10.041 |url=}}</ref>== | ||
There is a limited laboratory tests useful in the diagnosis of bone fractures such as the [[ | There is a limited laboratory tests useful in the diagnosis of bone fractures such as the [[Ankle fracture]]. Meanwhile, aged men and women may have some abnormalities in their laboratory findings suggestive of osteoporosis. | ||
Laboratory tests for the diagnosis of osteoporosis are: | Laboratory tests for the diagnosis of osteoporosis are: | ||
| Line 207: | Line 541: | ||
* Serum 25-(OH)-vitamin D level | * Serum 25-(OH)-vitamin D level | ||
==X Ray <ref name=" | ==X Ray<ref name="pmid30216844">{{cite journal |vauthors=Boszczyk A, Fudalej M, Kwapisz S, Błoński M, Kiciński M, Kordasiewicz B, Rammelt S |title=X-ray features to predict ankle fracture mechanism |journal=Forensic Sci. Int. |volume=291 |issue= |pages=185–192 |date=October 2018 |pmid=30216844 |doi=10.1016/j.forsciint.2018.08.042 |url=}}</ref>== | ||
The orthopedic surgeon should consider to have at least two radiographic projections (ie, anteroposterior [AP] and lateral) of the | The orthopedic surgeon should consider to have at least two radiographic projections (ie, anteroposterior [AP] and lateral) of the ankle. These show the fracture, the extent of displacement, and the extent of comminution. The orthopedic surgeon should pay serious attention toward finding any foreign bodies in open fractures and gunshot injuries. Also imperative is to include the elbow and wrist joint in the radiographs of [[Ankle fracture]] to ensure that the distal radioulnar joint injuries are not missed. | ||
<gallery perrow="3"> | <gallery perrow="3"> | ||
File: | File:Ankle-fracture-weber-a-5 (3).jpg| Mortise Three views of the ankle demonstrate a horizontal fracture through the lateral malleolus, below the level of the ankle joint, consistent with a Weber A fracture. | ||
File:Ankle-fracture-weber-a-5 (1).jpg| Lateral Three views of the ankle demonstrate a horizontal fracture through the lateral malleolus, below the level of the ankle joint, consistent with a Weber A fracture. | |||
File:Ankle-fracture-weber-a-5 (2).jpg| Frontal Three views of the ankle demonstrate a horizontal fracture through the lateral malleolus, below the level of the ankle joint, consistent with a Weber A fracture. | |||
</gallery> | </gallery> | ||
==CT == | ==CT <ref name="pmid28112555">{{cite journal |vauthors=Golshani A, Zhu L, Cai C, Beckmann NM |title=Incidence and Association of CT Findings of Ankle Tendon Injuries in Patients Presenting With Ankle and Hindfoot Fractures |journal=AJR Am J Roentgenol |volume=208 |issue=2 |pages=373–379 |date=February 2017 |pmid=28112555 |doi=10.2214/AJR.16.16657 |url=}}</ref><ref name="pmid28416839">{{cite journal |vauthors=Gong XF, Lyu YW, Wang JH, Wang Y, Wu Y, Wang MY |title=[A correlation analysis of the ankle CT and ankle fracture classification] |language=Chinese |journal=Beijing Da Xue Xue Bao |volume=49 |issue=2 |pages=281–285 |date=April 2017 |pmid=28416839 |doi= |url=}}</ref>== | ||
* CT-scan in the case of the [[ | * CT-scan in the case of the [[Ankle fracture]]is the best modality if you can not have an exclusive diagnosis by X-ray itself can not be made. | ||
<gallery perrow="3"> | <gallery perrow="3"> | ||
File: | File:Ankle-fracture-dislocation.jpg|Sagittal bone window Displaced distal fibular fracture with mild posterior angulation/ displacement. Comminuted and moderately displaced posterior malleolus fracture with a large articular surface step. Medial malleolus avulsion fracture involving the deltoid ligament. Anterior subluxation of the tibia on the talus also with lateral talar shift. Associated soft tissue swelling. | ||
File:Ankle-fracture-dislocation1.jpg|Coronal bone window Displaced distal fibular fracture with mild posterior angulation/ displacement. Comminuted and moderately displaced posterior malleolus fracture with a large articular surface step. Medial malleolus avulsion fracture involving the deltoid ligament. Anterior subluxation of the tibia on the talus also with lateral talar shift. Associated soft tissue swelling. | |||
</gallery> | </gallery> | ||
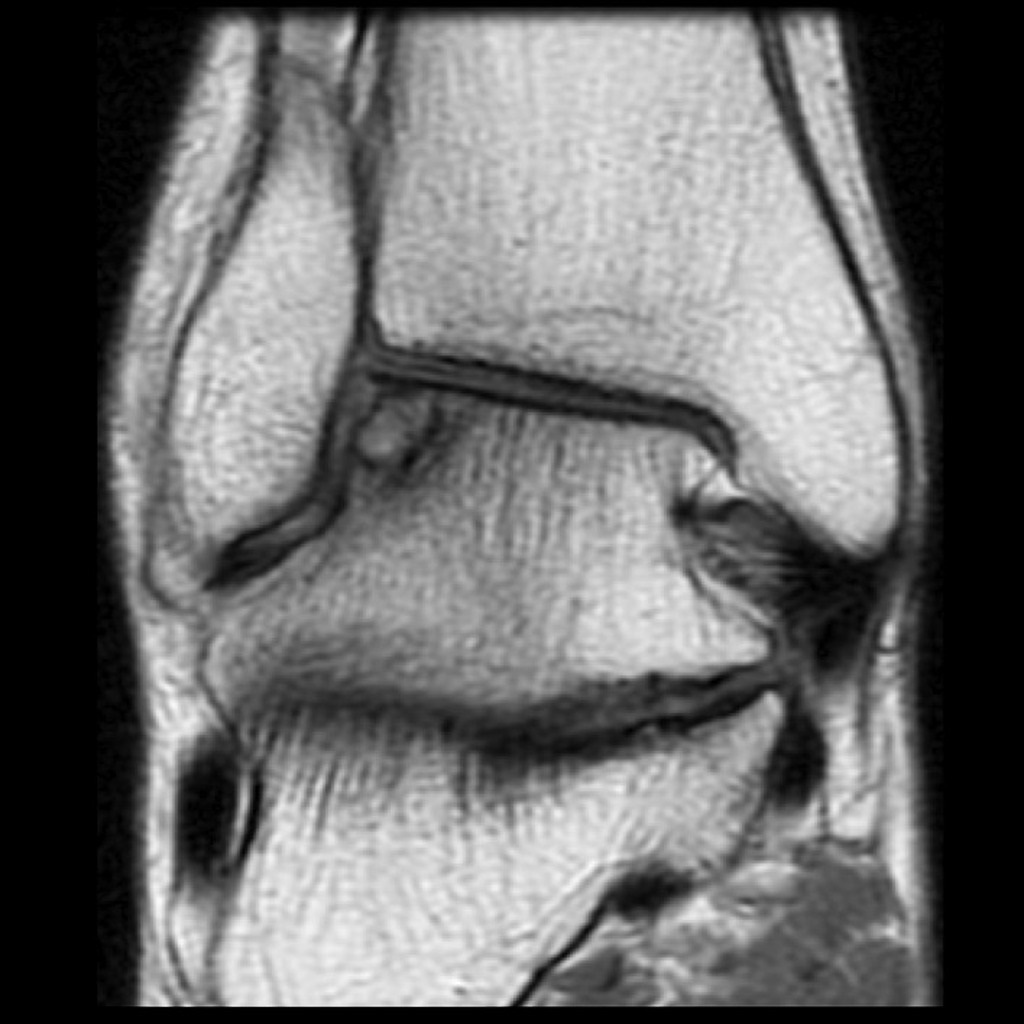
==MRI == | ==MRI <ref name="pmid29196821">{{cite journal |vauthors=Park YH, Yoon MA, Choi WS, Choi GW, Hong SJ, Kim HJ |title=The predictive value of MRI in the syndesmotic instability of ankle fracture |journal=Skeletal Radiol. |volume=47 |issue=4 |pages=533–540 |date=April 2018 |pmid=29196821 |doi=10.1007/s00256-017-2821-4 |url=}}</ref>== | ||
* Magnetic resonance imaging (MRI) is an expensive technique that should not be used routinely. | * Magnetic resonance imaging (MRI) is an expensive technique that should not be used routinely. | ||
* MRI is a powerful diagnostic tool to assess the abnormalities of the bone, ligaments and soft tissues associated with the [[ | * MRI is a powerful diagnostic tool to assess the abnormalities of the bone, ligaments and soft tissues associated with the [[Ankle fracture]], but it is known as a limited utility in radioulnar injuries and is not indicated in uncomplicated ankle fractures. | ||
* Meanwhile, the MRI can be useful in in following mentioned evaluations: | * Meanwhile, the MRI can be useful in in following mentioned evaluations: | ||
* Evaluation of occult [[Bone fracture|fractures]] | * Evaluation of occult [[Bone fracture|fractures]] | ||
| Line 232: | Line 568: | ||
* Evaluation of [[carpal tunnel syndrome]] | * Evaluation of [[carpal tunnel syndrome]] | ||
==Other Imaging Findings<ref name=" | <gallery perrow="3"> | ||
There are no other imaging findings associated with [[ | File:Subchondral-fracture-talar-dome (1).jpg| PD Subchondral fracture of the talar dome. Note the intact overlying cartilage. | ||
File:Subchondral-fracture-talar-dome.jpg| T2 fat sat Subchondral fracture of the talar dome. Note the intact overlying cartilage. | |||
</gallery> | |||
==Other Imaging Findings<ref name="pmid24375274">{{cite journal |vauthors=McDonald MR, Bulka CM, Thakore RV, Obremskey WT, Ehrenfeld JM, Jahangir AA, Sethi MK |title=Ankle radiographs in the early postoperative period: do they matter? |journal=J Orthop Trauma |volume=28 |issue=9 |pages=538–41 |date=September 2014 |pmid=24375274 |doi=10.1097/BOT.0000000000000052 |url=}}</ref>== | |||
There are no other imaging findings associated with [[Ankle fracture]] | |||
==Other Diagnostic Studies<ref name=" | ==Other Diagnostic Studies<ref name="pmid24375274">{{cite journal |vauthors=McDonald MR, Bulka CM, Thakore RV, Obremskey WT, Ehrenfeld JM, Jahangir AA, Sethi MK |title=Ankle radiographs in the early postoperative period: do they matter? |journal=J Orthop Trauma |volume=28 |issue=9 |pages=538–41 |date=September 2014 |pmid=24375274 |doi=10.1097/BOT.0000000000000052 |url=}}</ref>== | ||
There are no other Diagnostic studies associated with [[ | There are no other Diagnostic studies associated with [[Ankle fracture]] | ||
==Treatment == | ==Treatment <ref name="pmid29071495">{{cite journal |vauthors=Shen MS, Dodd AC, Lakomkin N, Mousavi I, Bulka C, Jahangir AA, Sethi MK |title=Open treatment of ankle fracture as inpatient increases risk of complication |journal=J Orthop Traumatol |volume=18 |issue=4 |pages=431–438 |date=December 2017 |pmid=29071495 |pmc=5685990 |doi=10.1007/s10195-017-0472-9 |url=}}</ref>== | ||
Immediate stabilization of patients is the first step. Then the radial fracture and the DRUJ stabilization is recommended in these cases. Open | Immediate stabilization of patients is the first step. Then the radial fracture and the DRUJ stabilization is recommended in these cases. Open ankle fractures considered as a surgical emergency. [[Ankle fracture]] occurs in younger patients who are skeletally immature; the normally they treated using a closed reduction and casting. Since closed reduction and cast application have led to unsatisfactory results. Then, Almost always the open reduction are necessary for the [[Ankle fracture]]. There are controversies regarding the indications for intramedullary nailing of ankle fractures. | ||
==Non-Operative | ==Non-Operative Treatment <ref name="pmid25419889">{{cite journal |vauthors=Drakos MC, Murphy CI |title=Bracing versus casting in ankle fractures |journal=Phys Sportsmed |volume=42 |issue=4 |pages=60–70 |date=November 2014 |pmid=25419889 |doi=10.3810/psm.2014.11.2092 |url=}}</ref><ref name="pmid29145978">{{cite journal |vauthors=Qin C, Dekker RG, Helfrich MM, Kadakia AR |title=Outpatient Management of Ankle Fractures |journal=Orthop. Clin. North Am. |volume=49 |issue=1 |pages=103–108 |date=January 2018 |pmid=29145978 |doi=10.1016/j.ocl.2017.08.012 |url=}}</ref>== | ||
* The first step in managing a patient with a fracture is to stabilize the patient if he/she is unstable due to blood loss, etc by giving them intravenous fluids and giving them some painkillers if the pain is severe. | * The first step in managing a patient with a fracture is to stabilize the patient if he/she is unstable due to blood loss, etc by giving them intravenous fluids and giving them some painkillers if the pain is severe. | ||
* In children, the usual plan is to attempt closed reduction followed by cast immobilization. In adults, treatment with immobilization in a molded long arm cast can be used in those rare occasions of a non-displaced fracture | * In children, the usual plan is to attempt closed reduction followed by cast immobilization. In adults, treatment with immobilization in a molded long arm cast can be used in those rare occasions of a non-displaced fracture of the ankle joint. If the fracture shifts in position, it may require surgery to put the bones back together. | ||
* Rigid immobilization is suggested in preference to removable splints in nonoperative treatment for the management of the [[ | * Rigid immobilization is suggested in preference to removable splints in nonoperative treatment for the management of the [[Ankle fracture]] | ||
* For all patients with [[ | * For all patients with [[Ankle fracture]], a post-reduction true lateral [[Radiography|radiograph]] is suggested. | ||
* Operative fixation is suggested in preference to [[Orthopedic cast|cast]] fixation for fractures with post-reduction radial [[shortening]] greater than 3 mm, dorsal tilt greater than 10º, or intra-articular displacement or step-off greater than 2 mm. | * Operative fixation is suggested in preference to [[Orthopedic cast|cast]] fixation for fractures with post-reduction radial [[shortening]] greater than 3 mm, dorsal tilt greater than 10º, or intra-articular displacement or step-off greater than 2 mm. | ||
* Patients probably do not need to begin early wrist motion routinely after stable [[Bone fracture|fracture]] fixation. | * Patients probably do not need to begin early wrist motion routinely after stable [[Bone fracture|fracture]] fixation. | ||
* Adjuvant treatment of [[ | * Adjuvant treatment of [[Ankle fracture]] with vitamin C is suggested for the prevention of disproportionate [[pain]] | ||
* Lateral epicondylar fractures should be immobilized for 7 days with patients elbow flexed at 90º, with the supinated ankle , and the extended wrist for relaxing the extensor muscles. | |||
* Lateral epicondylar fractures should be immobilized for 7 days with patients elbow flexed at 90º, with the supinated | === Complications of Non-surgical therapy<ref name="pmid25419889">{{cite journal |vauthors=Drakos MC, Murphy CI |title=Bracing versus casting in ankle fractures |journal=Phys Sportsmed |volume=42 |issue=4 |pages=60–70 |date=November 2014 |pmid=25419889 |doi=10.3810/psm.2014.11.2092 |url=}}</ref> === | ||
=== Complications of Non-surgical therapy === | |||
Failure of non-surgical therapy is common: | Failure of non-surgical therapy is common: | ||
* Re-displacement to its original position even in a cast | * Re-displacement to its original position even in a cast | ||
| Line 261: | Line 601: | ||
** Stiffness is universal following a prolonged period of immobilization and swelling | ** Stiffness is universal following a prolonged period of immobilization and swelling | ||
==Surgery == | ==Surgery <ref name="pmid26660864">{{cite journal |vauthors=Gonzalez TA, Macaulay AA, Ehrlichman LK, Drummond R, Mittal V, DiGiovanni CW |title=Arthroscopically Assisted Versus Standard Open Reduction and Internal Fixation Techniques for the Acute Ankle Fracture |journal=Foot Ankle Int |volume=37 |issue=5 |pages=554–62 |date=May 2016 |pmid=26660864 |doi=10.1177/1071100715620455 |url=}}</ref><ref name="pmid27441940">{{cite journal |vauthors=Ostrum RF, Avery MC |title=Open Reduction Internal Fixation of a Bimalleolar Ankle Fracture With Syndesmotic Injury |journal=J Orthop Trauma |volume=30 Suppl 2 |issue= |pages=S43–4 |date=August 2016 |pmid=27441940 |doi=10.1097/BOT.0000000000000588 |url=}}</ref><ref name="pmid30146336">{{cite journal |vauthors=Sung KH, Kwon SS, Yun YH, Park MS, Lee KM, Nam M, Jung JH, Lee SY |title=Short-Term Outcomes and Influencing Factors After Ankle Fracture Surgery |journal=J Foot Ankle Surg |volume=57 |issue=6 |pages=1096–1100 |date=2018 |pmid=30146336 |doi=10.1053/j.jfas.2018.03.045 |url=}}</ref>== | ||
Returning to the normal physical activity after [[ | Returning to the normal physical activity after [[Ankle fracture]]can take weeks to months of therapy under supervision an orthopedist. Meanwhile, a physiotherapy can be helpful for patient to achieve the normal wrist and elbow function caused by the immobilisation. All adult [[Ankle fracture]] should be considered to be treated with open reduction and internal fixation (ORIF). | ||
External fixation: For severe open fractures | External fixation: For severe open fractures | ||
Open reduction and internal fixation: For distal | Open reduction and internal fixation: For distal Ankle fracture which depending on each patients condition the following may be needed: | ||
Nerve placement | |||
Bone grafting | Bone grafting | ||
Osteotomy | Osteotomy | ||
| Line 273: | Line 613: | ||
<gallery perrow="3"> | <gallery perrow="3"> | ||
File: | File:Unstable-ankle-injury-2.jpg| Screw-plate stabilization of the fibular fracture and trans-syndesmotic screw stabilizing the ankle mortise. | ||
File:Ankle-fracture-weber-b-8 (1).jpg| Plate and screw internal fixation of distal fibular fracture. Lateral talar shift has been reduced with reduction of the fibula - distal syndesmosis must have been obviously stable at surgery and thus no diastasis screw was used. | |||
</gallery> | </gallery> | ||
=== Operation <ref name=" | === Operation <ref name="pmid27819005">{{cite journal |vauthors=Jung HG, Kim JI, Park JY, Park JT, Eom JS, Lee DO |title=Is Hardware Removal Recommended after Ankle Fracture Repair? |journal=Biomed Res Int |volume=2016 |issue= |pages=5250672 |date=2016 |pmid=27819005 |pmc=5081426 |doi=10.1155/2016/5250672 |url=}}</ref><ref name="pmid27816101">{{cite journal |vauthors=Chan KB, Lui TH |title=Role of Ankle Arthroscopy in Management of Acute Ankle Fracture |journal=Arthroscopy |volume=32 |issue=11 |pages=2373–2380 |date=November 2016 |pmid=27816101 |doi=10.1016/j.arthro.2016.08.016 |url=}}</ref>=== | ||
* There are a variety of methods and implants useful to stabilize the [[ | * There are a variety of methods and implants useful to stabilize the [[Ankle fracturee]], ranging from closed reduction and percutaneous pin fixation to the use of intra-medullary devices. | ||
* However, the most common fixation methods to treat complex [[ | * However, the most common fixation methods to treat complex [[Ankle fracture]] include [[external fixation]], and open reduction and internal fixation. | ||
=== External Fixation With or Without Percutaneous Pin Fixation === | === External Fixation With or Without Percutaneous Pin Fixation === | ||
* [[ | * [[Ankle]] spanning [[external fixation]] employs ligamentotaxis to restore and maintain length, alignment, and rotation of bone. | ||
* Reduction is typically obtained through closed or minimally open methods and preserves the [[Bone fracture|fracture]] biology. | * Reduction is typically obtained through closed or minimally open methods and preserves the [[Bone fracture|fracture]] biology. | ||
* The addition of percutaneous pins enhances the ability to reduce and stabilize fracture fragments. | * The addition of percutaneous pins enhances the ability to reduce and stabilize fracture fragments. | ||
| Line 289: | Line 629: | ||
==== Complications of External Fixation ==== | ==== Complications of External Fixation ==== | ||
* Pin tract [[infection]] | * Pin tract [[infection]] | ||
* Injury to the [[Superficial branch of the | * Injury to the [[Superficial branch of the nerve]] | ||
* [[Complex regional pain syndrome]] | * [[Complex regional pain syndrome]] | ||
=== Open reduction and internal fixation with plates and screws === | === Open reduction and internal fixation with plates and screws === | ||
* This is the most common type of surgical repair for [[ | * This is the most common type of surgical repair for [[Ankle fracture]] | ||
* During this type of procedure, the bone fragments are first repositioned (reduced) into their normal alignment. | * During this type of procedure, the bone fragments are first repositioned (reduced) into their normal alignment. | ||
* The bones held together with special screws and metal plates attached to the outer surface of the bone. | * The bones held together with special screws and metal plates attached to the outer surface of the bone. | ||
| Line 303: | Line 643: | ||
* Nonunion | * Nonunion | ||
=== Pain Management === | === Pain Management <ref name="pmid26021663">{{cite journal |vauthors=Saper D, Litrenta J, Otlans P, Daley J, Tornetta P |title=Factors affecting pain in acute ankle fractures: A prospective evaluation |journal=Injury |volume=46 |issue=8 |pages=1641–4 |date=August 2015 |pmid=26021663 |doi=10.1016/j.injury.2015.05.009 |url=}}</ref><ref name="pmid27923219">{{cite journal |vauthors=Lovy AJ, Dowdell J, Keswani A, Koehler S, Kim J, Weinfeld S, Joseph D |title=Nonoperative Versus Operative Treatment of Displaced Ankle Fractures in Diabetics |journal=Foot Ankle Int |volume=38 |issue=3 |pages=255–260 |date=March 2017 |pmid=27923219 |doi=10.1177/1071100716678796 |url=}}</ref>=== | ||
Pain after an injury or surgery is a natural part of the healing process. | Pain after an injury or surgery is a natural part of the healing process. | ||
Medications are often prescribed for short-term pain relief after surgery or an | Medications are often prescribed for short-term pain relief after surgery or an injury such as: | ||
* opioids | * opioids | ||
* non-steroidal anti-inflammatory drugs (NSAIDs) | * non-steroidal anti-inflammatory drugs (NSAIDs) | ||
| Line 313: | Line 653: | ||
=== Be aware that although opioids help relieve pain after surgery or an injury, they are a narcotic and can be addictive. It is important to use opioids only as directed by doctor. === | === Be aware that although opioids help relieve pain after surgery or an injury, they are a narcotic and can be addictive. It is important to use opioids only as directed by doctor. === | ||
=== Interventions === | === Interventions <ref name="pmid28148665">{{cite journal |vauthors=Olsen LL, Møller AM, Brorson S, Hasselager RB, Sort R |title=The impact of lifestyle risk factors on the rate of infection after surgery for a fracture of the ankle |journal=Bone Joint J |volume=99-B |issue=2 |pages=225–230 |date=February 2017 |pmid=28148665 |doi=10.1302/0301-620X.99B2.BJJ-2016-0344.R1 |url=}}</ref>=== | ||
The following options can be helpful for patients to rehabilitate after their fracture : | The following options can be helpful for patients to rehabilitate after their fracture : | ||
* Joints mobilization | * Joints mobilization | ||
| Line 319: | Line 659: | ||
* Soft tissue massage | * Soft tissue massage | ||
* Exercises and Activity modification | * Exercises and Activity modification | ||
== Postoperative Rehabilitation <ref name=" | == Postoperative Rehabilitation <ref name="pmid28291180">{{cite journal |vauthors=Nortunen S, Leskelä HV, Haapasalo H, Flinkkilä T, Ohtonen P, Pakarinen H |title=Dynamic Stress Testing Is Unnecessary for Unimalleolar Supination-External Rotation Ankle Fractures with Minimal Fracture Displacement on Lateral Radiographs |journal=J Bone Joint Surg Am |volume=99 |issue=6 |pages=482–487 |date=March 2017 |pmid=28291180 |doi=10.2106/JBJS.16.00450 |url=}}</ref>== | ||
* Complex [[ | * Complex [[Ankle fracture]] warrant individualized immobilization and rehabilitation strategies. | ||
* Because most multifragmentary [[Ankle fracture]] are the result of high-energy injuries, a prolonged period of [[wrist]] immobilization and [[Soft tissue|soft-tissue]] rest may be beneficial and has not been shown to affect clinical outcomes. | |||
* The | * The ankle is typically immobilized for 6 weeks post-operatively in a [[Splint (medicine)|splint]] with Full weight bearing commences at approximately 3 months post-operatively after consolidation of the [[Bone fracture|fracture]] is noted on radiographs. | ||
*<nowiki/>The presence of varying degrees of ankle [[stiffness]] is inevitable and may result from poor [[pain]] control, lack of effort in controlled mobilization, [[edema]], concomitant ipsilateral [[lower extremity]] [[Bone fracture|fracture]]<nowiki/>s, or [[Peripheral nervous system|peripheral]] <nowiki/>[[Peripheral nervous system|nerve]] injuries. Early stretching and mobilization of the intrinsic and extrinsic [[Tendon|tendons]] of the [[hand]] is important to prevent finger [[stiffness]]. [[Edema]] control can be initiated with compression gloves, digital massage, and active and passive ROM of the ankle. A home [[Physical exercise|exercise]] program or outpatient occupational therapy is started immediately post-operatively to maintain full [[range of motion]] of the ankle and limit the development of intrinsic muscle tightnes | |||
* The presence of varying degrees of | |||
==Primary Prevention<ref name=" | == Primary Prevention <ref name="pmid14291935">{{cite journal |vauthors=KARNAUKHOV AK |title=[POINTED PIN FOR OSTEOSYNTHESIS OF ANKLE FRACTURES] |language=Russian |journal=Voen Med Zh |volume=51 |issue= |pages=76 |date=1964 |pmid=14291935 |doi= |url=}}</ref><ref name="pmid26457936">{{cite journal |vauthors=Gee CW, Dahal L, Rogers BA, Harry LE |title=Ankle fractures in the elderly: an overlooked burden |journal=Br J Hosp Med (Lond) |volume=76 |issue=10 |pages=564–9 |date=October 2015 |pmid=26457936 |doi=10.12968/hmed.2015.76.10.564 |url=}}</ref>== | ||
There are various preventive options to reduce the incidence of the [[ | There are various preventive options to reduce the incidence of the [[Ankle fracture]] | ||
* Using ankle guards during practicing sports (skating, biking) | |||
* Using ankle guards during driving motorbikes | |||
* Avoid falls in elderly individuals | |||
* Prevention and/or treatment of osteoporosis | |||
*<nowiki/><nowiki/><nowiki/>Healthy diet | |||
==Secondary Prevention== | == Secondary Prevention <ref name="pmid24676720">{{cite journal |vauthors=Zwipp H, Amlang M |title=[Treatment of fractures of the ankle in the elderly] |language=German |journal=Orthopade |volume=43 |issue=4 |pages=332–8 |date=April 2014 |pmid=24676720 |doi=10.1007/s00132-013-2168-z |url=}}</ref>== | ||
It should be noted that the Post-menopausal women specially older than the age of 65 are at the higher risk of [[osteoporosis]] consequently these type of patients at greater risk for the pathological [[Bone fracture|fractures]] . | It should be noted that the Post-menopausal women specially older than the age of 65 are at the higher risk of [[osteoporosis]] consequently these type of patients at greater risk for the pathological [[Bone fracture|fractures]] . | ||
| Line 351: | Line 684: | ||
* [[Medical ultrasonography|Ultrasonography]] of the [[calcaneus]] | * [[Medical ultrasonography|Ultrasonography]] of the [[calcaneus]] | ||
=== Pharmacological therapy === | === Pharmacological therapy <ref name="pmid25586467">{{cite journal |vauthors=Ovaska M |title=Complications in ankle fracture surgery |journal=Acta Orthop Suppl |volume=86 |issue=358 |pages=1–32 |date=February 2015 |pmid=25586467 |doi=10.3109/17453674.2014.100227 |url=}}</ref>=== | ||
* The primary goal for the treatment of [[osteoporosis]] is to reduce longtime [[fracture]] risk in patients. Increasing [[Bone mineral density|bone mineral density (BMD)]] in response to the treatment is far less important than improvement of clinical aspects of [[osteoporosis]], i.e., [[Osteoporosis|osteoporotic]][[Bone fracture|fracture]]. Therefore, most of the [[drugs]] efficacy is measured by the extent they improve the [[fracture]] risk instead of increasing [[Bone mineral density|BMD]]. | * The primary goal for the treatment of [[osteoporosis]] is to reduce longtime [[fracture]] risk in patients. Increasing [[Bone mineral density|bone mineral density (BMD)]] in response to the treatment is far less important than improvement of clinical aspects of [[osteoporosis]], i.e., [[Osteoporosis|osteoporotic]][[Bone fracture|fracture]]. Therefore, most of the [[drugs]] efficacy is measured by the extent they improve the [[fracture]] risk instead of increasing [[Bone mineral density|BMD]]. | ||
* During the treatment, if a single [[fracture]] happens, it does not necessarily indicate treatment failure or the need to be started on an alternative treatment or patient referral to a [[specialist]]. | * During the treatment, if a single [[fracture]] happens, it does not necessarily indicate treatment failure or the need to be started on an alternative treatment or patient referral to a [[specialist]]. | ||
* [[Calcium]] and [[vitamin D]] supplementation have been found to be effective in reducing the long term [[Bone fracture|fracture]] risk, significantly. In order to suggest the people to use [[vitamin D]] and [[calcium]] [[supplements]], the [[physician]] needs to make sure that patient is not able to obtain the [[nutrients]] through the daily intake. The available supplemental ions of [[calcium]] include [[calcium carbonate]], [[Calcium citrate|calcium citrate,]] and [[vitamin D3]] in various [[Dosage form|dosage forms]]. | * [[Calcium]] and [[vitamin D]] supplementation have been found to be effective in reducing the long term [[Bone fracture|fracture]] risk, significantly. In order to suggest the people to use [[vitamin D]] and [[calcium]] [[supplements]], the [[physician]] needs to make sure that patient is not able to obtain the [[nutrients]] through the daily intake. The available supplemental ions of [[calcium]] include [[calcium carbonate]], [[Calcium citrate|calcium citrate,]] and [[vitamin D3]] in various [[Dosage form|dosage forms]]. | ||
=== Life style modifications<ref name=" | === Life style modifications<ref name="pmid29369927">{{cite journal |vauthors=Cordova CB, Dunn JC, Kusnezov N, Bader JM, Waterman BR, Orr JD |title=Comparing clinician use of three ankle fracture classifications |journal=JAAPA |volume=31 |issue=2 |pages=36–39 |date=February 2018 |pmid=29369927 |doi=10.1097/01.JAA.0000529773.90897.9f |url=}}</ref>=== | ||
* [[Exercise]]: Exercise promotes the [[mineralization]] of [[bone]] and [[bone]] accumulation particularly during growth. High impact exercise, in particular, has been shown to prevent the development of [[osteoporosis]]. However, it can have a negative effect on bone [[mineralization]] in cases of poor [[nutrition]], such as [[anorexia nervosa]] and [[celiac disease]]. | * [[Exercise]]: Exercise promotes the [[mineralization]] of [[bone]] and [[bone]] accumulation particularly during growth. High impact exercise, in particular, has been shown to prevent the development of [[osteoporosis]]. However, it can have a negative effect on bone [[mineralization]] in cases of poor [[nutrition]], such as [[anorexia nervosa]] and [[celiac disease]]. | ||
* [[Nutrition]]: A [[diet]] high in [[calcium]] and [[vitamin D]] prevents [[bone loss]]. Patients at risk for [[osteoporosis]], such as persons with chronic [[steroid]] use are generally treated with [[vitamin D]] and [[calcium]] supplementation. In [[Kidney|renal]] disease, more active forms of [[vitamin D]], such as 1,25-dihydroxycholecalciferol or [[calcitriol]] are used; as the kidney cannot adequately generate [[calcitriol]] from [[calcidiol]] (25-hydroxycholecalciferol), which is the storage form of [[vitamin D]]. | * [[Nutrition]]: A [[diet]] high in [[calcium]] and [[vitamin D]] prevents [[bone loss]]. Patients at risk for [[osteoporosis]], such as persons with chronic [[steroid]] use are generally treated with [[vitamin D]] and [[calcium]] supplementation. In [[Kidney|renal]] disease, more active forms of [[vitamin D]], such as 1,25-dihydroxycholecalciferol or [[calcitriol]] are used; as the kidney cannot adequately generate [[calcitriol]] from [[calcidiol]] (25-hydroxycholecalciferol), which is the storage form of [[vitamin D]]. | ||
| Line 363: | Line 696: | ||
{{Fractures}} | {{Fractures}} | ||
{{WH}} | {{WH}} | ||
| Line 374: | Line 701: | ||
==See also== | ==See also== | ||
* | * triplane fracture | ||
* | * Tillaux fracture | ||
* | * Bosworth fracture | ||
* | * '''pilon fracture''' | ||
* | * Wagstaffe-Le Forte fracture | ||
* [[Maisonneuve fracture|Maisonneuve Fracture]] | |||
*[[ | |||
==References== | ==References== | ||
<references /> | <references /> | ||
__NOTOC__ | __NOTOC__ | ||
[[Category:Bone fractures]] | |||
[[Category:Orthopedic_surgery]] | |||
[[Category:Orthopedics]] | |||
[[Category:Orthopedics]] | |||
[[Category:Radiology]] | |||
[[Category:Emergency medicine]] | [[Category:Emergency medicine]] | ||
Latest revision as of 14:31, 24 May 2021

| Ankle fracture | |
| ICD-10 | S42.2-S42.4 |
|---|---|
| ICD-9 | 812 |
| eMedicine | emerg/199 orthoped/271 orthoped/199 |
|
WikiDoc Resources for Ankle fracture |
|
Articles |
|---|
|
Most recent articles on Ankle fracture Most cited articles on Ankle fracture |
|
Media |
|
Powerpoint slides on Ankle fracture |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Ankle fracture at Clinical Trials.gov Trial results on Ankle fracture Clinical Trials on Ankle fracture at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Ankle fracture NICE Guidance on Ankle fracture
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Ankle fracture Discussion groups on Ankle fracture Patient Handouts on Ankle fracture Directions to Hospitals Treating Ankle fracture Risk calculators and risk factors for Ankle fracture
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Ankle fracture |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mohammadmain Rezazadehsaatlou[2].
Overview[1][2][3]
The ankle joint is consisted of 2 different joints:
1: The true ankle joint (Responsible for the dorsiflexion and plantar flexion movements of the ankle joint): It is consisted of three bone:
a: The tibia (medial ankle)
b: The fibula (lateral ankle)
c: The talus (the floor upon which the tibia and fibula rest).
2: The subtalar joint (Responsible for the invertion and evertion of foot):
a: The talus
b: The calcaneus A combination of ankle bones, joint capsule, and ligaments system are responsible for the stability of the ankle joint. syndesmosis of this stabilizing system are Anterior tibiofibular ligament Posterior tibiofibular ligament Transverse tibiofibular ligament Interosseous membrane Generally, there are three sub-groups for the the ankle joint based on the location of the the tibia and fibula:
- Medial malleolus - inside part of the tibia
- Posterior malleolus - back part of the tibia
- Lateral malleolus - end of the fibula
Accordingly, there are thee type of ankle fracture invovlement:
A unimalleolar fracture Involves either the distal fibula (more common) or the distal tibia
A bimalleolar fracture Involves the lateral malleolus and the medial malleolus.
A trimalleolar fracture Involves the lateral malleolus, the medial malleolus, and the distal posterior aspect of the tibia.
Historical Perspective [4][5]
There are no reliable information regarding the historical perspective of the Ankle bone fracture but
In 1758, Percival Pott described three types of ankle fractures based on the number of malleoli involved as: unimalleolar, bimalleolar, and trimalleolar. Despite its ease of use it failed to differentiate stable from unstable types.
In 1949, a Danish physician, Niel Lauge-Hansen created a classification system based on a rotational mechanism of injury and he published his great work in a 1950 issue of Archives of Surgery,
Causes [6][7]
- Pressure during car accidents
- Twisted ankle side to side
- Rotated ankle side to side
- Rolling ankle in or out
- Hyper-flextion
- Hyper-Extention
- Tripping
- Falling from a height
- Jumping from a height
As a person age, two factors cause higher risk of fractures:
- Weaker bones
- Greater risk of falling
Stress fractures as a common causes of fractures can be found due to the repeated stresses and strains. Importantly children having more physically active lifestyles than adults, are also prone to fractures. People with any underlying diseases such as osteoporosis, infection, or a tumor affecting their bones having a higher risk of fractures. As mentioned in previous chapters, this type of fracture is known as a pathological fracture. Stress fractures, which result from repeated stresses and strains, commonly found among professional sports people, are also common causes of fractures.
Life-threatening Causes
- There are no life-threatening causes of Ankle fracture , however complications resulting from Ankle fracture is common.
Common Causes
Common causes of Ankle fracture may include:
Less Common Causes
Less common causes of Ankle fracture include conditions that predisposes to fracture:
Causes by Organ System
| Cardiovascular | No underlying causes |
| Chemical/Poisoning | No underlying causes |
| Dental | No underlying causes |
| Dermatologic | No underlying causes |
| Drug Side Effect | No underlying causes |
| Ear Nose Throat | No underlying causes |
| Endocrine | No underlying causes |
| Environmental | No underlying causes |
| Gastroenterologic | No underlying causes |
| Genetic | No underlying causes |
| Hematologic | No underlying causes |
| Iatrogenic | No underlying causes |
| Infectious Disease | No underlying causes |
| Musculoskeletal/Orthopedic | Osteoporosis and osteopenia. |
| Neurologic | No underlying causes |
| Nutritional/Metabolic | Osteoporosis and osteopenia. |
| Obstetric/Gynecologic | No underlying causes |
| Oncologic | No underlying causes |
| Ophthalmologic | No underlying causes |
| Overdose/Toxicity | No underlying causes |
| Psychiatric | No underlying causes |
| Pulmonary | No underlying causes |
| Renal/Electrolyte | No underlying causes |
| Rheumatology/Immunology/Allergy | No underlying causes |
| Sexual | No underlying causes |
| Trauma | Falling of car accident to on side of Ankle . |
| Urologic | No underlying causes |
| Miscellaneous | No underlying causes |
Causes in Alphabetical Order
List the causes of the disease in alphabetical order:
Pathophysiology [8]
The main etiology of the Ankle fracture is thought to excessive inversion stress to the ankle joint. The ankle is more stable and resistant to eversion injuries than inversion injuries Because: The medial malleolus is shorter than the lateral malleolus causing higher range of the invertion than evertion of the talus bone. The deltoid ligament stabilized the medial wall of the ankle joint
On the other hand, the transverse malleolar, Vertical malleolar, and posterior malleolar fractures are associated with an avulsion injury, talar impaction, and other bone and/or ligamentous injury, respectively.
Mechanism [9]
In 80% of ankle fractures the foot is in supination position while, in 20% of fractures the foot is in pronation position. The Ankle fracture is caused by a falling or direct trauma to the ankle joint. The form and severity of this fracture depends on the position of the ankle joint at the moment of the trauma. The ankle joint is flexible but the medial side of the ankle joint is rigid because the medial malleolus is attached to the tibia and also the medial collateral ligaments are very strong. Also, lateral wall of the ankle include: the fibula, syndesmosis and lateral collateral ligaments play important rolls in this flexibility. This lateral wall of the ankle allows the talus to move in lateral and dorsal sides easily. The fibula has no weight-bearing roll but it provide a flexible lateral support. The syndesmosis is formed by the anterior and posterior tibiofibular ligaments which is the fibrous connection between the fibula and tibia.
If we imagine the ankle as a ring in which bones and ligaments play an important role in the maintaining the stability of this joint. Meanwhile, if this ring is broken in one place it remains stable but when it is broken in two places, the ring is unstable and it is at the higher risk of fracture. Consequently the ankle is unstable when both the medial and the lateral malleoli are fractured.
Pathophysiology [10][11]
Its known that the Ankle fracture in normal healthy adults can be caused due to the high-energy trauma (e.g., motor vehicle accidents), sport related injuries, falling from height. But it should be noted that the most important Risk factors for insufficiency fractures is chronic metabolic disease such as steoporosis, osteopenia, eating-disordered behavior, higher age, prolonged corticosteroid usage, female gender, lower BMI, history of a recent falling, and prior fracture.
- The pattern of bone fracture and severity of injury depends on variety of factors such as:
- Patients age
- Patients Weight
- Patients past medical history specifically any bone diseases affecting the quality of bone (such as osteoporosis, malignancies)
- Energy of trauma
- Bone quality
- Position of the specific organ during the trauma
- The below-mentioned processes cause decreased bone mass density:
- Autophagy is the mechanism through which osteocytes evade oxidative stress.
- The capability of autophagy in cells decreases as they age, a major factor of aging.
- As osteocytes grow, viability of cells decrease thereby decreasing the bone mass density.
Differentiating Ankle fracture from other Diseases [12][13]
In the orthopedic medicine its important to know that the ankle fracture should be evaluated using radiography for both confirming diagnosis and also for evaluating the surrounding tissues.
- Acute compartment syndrome of ankle joint
- Ankle Dislocation
- Soft tissue Injury around the ankle ,
- Deep Venous thrombosis
- Thrombophlebitis
- Foot Fracture
- Gout
- Pseudogout
- Rheumatoid Arthritis
- Tibia Fracture
- Fibula Fracture
- bimalleolar fracture
- trimalleolar fracture
- triplane fracture
- Tillaux fracture
- Bosworth fracture
- pilon fracture
- Wagstaffe-Le Forte fracture
- Charcot-Marie-Tooth disease: in cases with repeated ankle fractures
Epidemiology and Demographics[14][15]
Of all cases with the ankle injuries only 15% of cases are true ankle fractures. The male-to-female ratio for ankle fracture is 2:1. The frequency of ankle fractures in adults and children is around 100 cases in 100,000 per year and 190 cases in 100,000 per year, respectively.
Risk Factors [16]
There are different risk factors that presidpose patient for the Ankle fracture that include:
- High-risk contact sports
- Higher age (elderly adults are higher prone to such fractures)
- Reduced bone density (osteoporosis)
- Direct blow
- Road / traffic accidents
- Falling
- Direct trauma to the ankle
- Taking part in any rough or high-impact sport
- Street fights, gunshot wounds, and domestic violence, may also cause the Ankle fracture
- Road traffic accidents.
Classification [17][18][19] [20]
The Ankle fracture may be classified based on the exact location of fracture:
The Weber ankle fracture classification (or Danis-Weber classification) can b used to classify the lateral malleolar fractures.
The Lauge-Hansen classification system is also for the ankle injuries based on injury mechanisms. This classification system uses two words:
- The first word describes the position of the foot during the injury such as: supination and pronation.
- The second word describes the direction of the deforming force such as abduction, adduction, or external rotation.
Accordingly, at least 13 different patterns have been described:
| Grade | Sequence |
|---|---|
| Supination-Adduction | Stage 1: With no medial malleolar fracture (Weber A)
Stage 2: With oblique or vertical medial malleolar fracture |
| Supination-External rotation
(40-70% of injuries) |
Stage 1: Tear or avulsion of the anteroinferior tibiofibular ligament is torn or avulsed
Stage 2: The talus displaces and fractures the fibula in an oblique or spiral fracture, starting at the joint (Weber B) Stage 3: Tear of the posteroinferior tibiofibular ligament or fracture posterior malleolus Stage 4: Tear of the deltoid ligament or transverse avulsion fracture medial malleolus |
| Pronation-Abduction | stage 1: Deltoid ligament disruption or transverse medial malleolus fracture
stage 2: Posterior malleolus fracture stage 3: Oblique fibular fracture (Weber C) |
| Pronation-External rotation | stage 1: Deltoid ligament rupture, which may appear occult or as medial mortise widening, or transverse avulsion fracture of the medial malleolus
stage 2: Involvement of the AITFL with extension into the interosseous membrane results in widening of the distal tibiofibular distance stage 3: A spiral or oblique fibular fracture (>6 cm) at the level or above the talotibial joint (Weber C) stage 4: Involvement of the posterior inferior tibiofibular ligament (PITFL), or posterior malleolus fracture |
AO/OTA classification of tibial malleolar fractures
| Infrasyndesmotic | 44-A1
44-A2 44-A3 |
isolated fibula fracture
fibula fracture with a medial malleolar involvement fibular fracturewith a posteromedial involvement |
| Transsyndesmotic | 44-B1
44-B2 44-B3 |
isolated fibula fracture
fibula fracture with a medial involvement fibula fracture with a medial injury and the posterolateral rim involvement (Volkmann’s fragment) |
| Suprasyndesmotic | 44-C1
44-C2 44-C3 |
simple diaphyseal fibula fracture
wedge or multifragmentary diaphyseal fibula involvement proximal fibula fracture |
Screening[21]
Osteoporosis is an important risk factor for human affecting human bone especially in men with the age of older than 50 years old and postmenopausal and women.
Based on the US Preventive Services Task Force (USPSTF) there are three groups of patients need to be screened for the osteoporosis:
- · Men with no history of osteoporosis
- · Women with the age of 65≤ year old, with no previous history of pathological fracture due to the osteoporosis
- · Women with the age of <65 years, with 10-year fracture risk of not less than a 65-year-old white woman (who has not any other risk factor)
Accordingly women older than age of 50 are the main target for the osteoporosis screening. There is no specific recommendation to screen men for the osteoporosis.
The USPSTF recommendations from 2002 included:
Meanwhile, there are two major modalities for the osteoporosis screening:
- · Dual energy x-ray absorptiometry (DXA) of the hip and lumbar spine bones
- · Quantitative ultrasonography of the calcaneus
*It should be noted of the two above mentioned modalities for screening the ultrasonograhy is preferred to the DXA due to its lower cost, lower ionizing radiation, more availability.
After the primary evaluation of the osteoporosis, the further evaluation are required in some cases such as:
· Women with normal bone density or mild osteopenia: T-score of greater than −1.50 – should have screening for 15 years.
· Women with moderate osteopenia: T-score of −1.50 to −1.99 – should have screening for 5 years.
· Women with advanced osteopenia: T-score of −2.00 to −2.49 - should have screening for 1 year.
Natural History, Complications and Prognosis [22][23]
Natural History[24]
In cases with untreated Ankle fracture the malunion and deformity of arm can be occurred.
Complications [25]
The overall complication rate in the treatment of Ankle fracture were found in around 40% of cases:
- Neurovascular compromise: such as Ulna nerve damage
- Compartment syndrome
- Chronic disability of the DRUJ
- Physeal Injury
- Malunion of the radius
- Nonunion
- Infection
- Refracture following plate removal
- Neural injury
- Instability of the DRUJ
- Loss of Motion (Stiffness)
- Posttraumatic Arthritis
- Heterotopic Ossification
Prognosis [26]
Successful treatment of Ankle fracture depends on the on-time interventions such as: accurate diagnosis and appropriate treatment and referral. Complex open fractures with soft-tissue injuries have a worse prognosis than isolated closed ankle fractures.
Diagnosis[25]
The diagnosis of a Ankle fracture should be confirmed using a radiographic examination.
History and Symptoms [27]
The related signs and symptoms include:
- Deformity
- Skin lacerations
- Open fractures
- Erythema
- Edema
- Stiffness
- Decreased range of motion
- Tenderness
- Loss of function of the leg
- Difficulties in detection of pulses
- Nerve damage
In the physical exam the orthopedic surgeon should check the vascular status and amount of swelling in the ankle. In MULTI-trauma patients or in comatose or obtunded patients a tense compartment with neurological signs or stretch pain should be considered as the compartment syndrome, and the compartment pressures should be measured and monitored. Normally the pain and soft-tissue swelling are found at the injury site. This injury should be confirmed using a radiographic evaluations.
Physical Examination[28][29][30]
The related signs and symptoms include:
- Edema of the ankle
- Most of the time the edema will be a non-pitting edema
- Depends on the edema extent, it may even lead to compartment syndrome in the anterior and internal compartment of the ankle
- Bruising
- As a manifestation of internal injury to the local vessels by trauma or fractures bone
- Decrease in range of motion of the ankle
- Movement of the ankle will be painful if possible at all
- Tenderness
- Deformity
- Fractured bone deformity may be touchable in the internal side of the ankle if the fracture is displaced
In the physical exam the orthopedic surgeon should check the vascular status and amount of swelling in the ankle. In polytrauma patients or in comatose or obtunded patients a tense compartment with neurological signs or stretch pain should be considered as the compartment syndrome, and the compartment pressures should be measured and monitored.
Physical examination of patients with Ankle fracture is usually remarkable for swelling, tenderness, bruises, ecchymosis, deformity and restricted range of motion of the ankle.
Appearance of the Patient
- Patients with Ankle fracture usually appears normal unless the patients had a high energy trauma causing the open wound fracture.
Vital Signs
- Weak pulse may be seen when associated with polytrauma.
- Low blood pressure with normal pulse pressure may be present due to compound fracture with blood loss.
Skin
- Skin examination of patients with Ankle fracture includes:
HEENT
- HEENT examination of patients with Ankle fracture usually normal.
Neck
- Neck examination of patients with Ankle fracture is usually normal
Lungs
- Pulmonary examination of patients with Ankle fracture usually normal
Heart
- Cardiovascular examination of patients with Ankle fracture usually normal
Abdomen
- Abdominal examination of patients with Ankle fracture usually normal
Back
- Back examination of patients with Ankle fracture usually normal
Genitourinary
- Genitourinary examination of patients with Ankle fracture usually normal
Neuromuscular
- Neuromuscular examination of patients with Ankle fracture is usually normal
- However, some patients may develop neuropraxia of the branch of the Ulnar nerve resulting in decreased sensation of thumb, index and middle finger.
Laboratory Findings[31]
There is a limited laboratory tests useful in the diagnosis of bone fractures such as the Ankle fracture. Meanwhile, aged men and women may have some abnormalities in their laboratory findings suggestive of osteoporosis.
Laboratory tests for the diagnosis of osteoporosis are:
- Complete blood count (CBC)
- Serum total calcium level
- Serum Ionized calcium level
- Serum phosphate level
- Serum alkaline phosphatase level
- Serum 25-(OH)-vitamin D level
X Ray[32]
The orthopedic surgeon should consider to have at least two radiographic projections (ie, anteroposterior [AP] and lateral) of the ankle. These show the fracture, the extent of displacement, and the extent of comminution. The orthopedic surgeon should pay serious attention toward finding any foreign bodies in open fractures and gunshot injuries. Also imperative is to include the elbow and wrist joint in the radiographs of Ankle fracture to ensure that the distal radioulnar joint injuries are not missed.
-
Mortise Three views of the ankle demonstrate a horizontal fracture through the lateral malleolus, below the level of the ankle joint, consistent with a Weber A fracture.
-
Lateral Three views of the ankle demonstrate a horizontal fracture through the lateral malleolus, below the level of the ankle joint, consistent with a Weber A fracture.
-
Frontal Three views of the ankle demonstrate a horizontal fracture through the lateral malleolus, below the level of the ankle joint, consistent with a Weber A fracture.
CT [33][20]
- CT-scan in the case of the Ankle fractureis the best modality if you can not have an exclusive diagnosis by X-ray itself can not be made.
-
Sagittal bone window Displaced distal fibular fracture with mild posterior angulation/ displacement. Comminuted and moderately displaced posterior malleolus fracture with a large articular surface step. Medial malleolus avulsion fracture involving the deltoid ligament. Anterior subluxation of the tibia on the talus also with lateral talar shift. Associated soft tissue swelling.
-
Coronal bone window Displaced distal fibular fracture with mild posterior angulation/ displacement. Comminuted and moderately displaced posterior malleolus fracture with a large articular surface step. Medial malleolus avulsion fracture involving the deltoid ligament. Anterior subluxation of the tibia on the talus also with lateral talar shift. Associated soft tissue swelling.
MRI [34]
- Magnetic resonance imaging (MRI) is an expensive technique that should not be used routinely.
- MRI is a powerful diagnostic tool to assess the abnormalities of the bone, ligaments and soft tissues associated with the Ankle fracture, but it is known as a limited utility in radioulnar injuries and is not indicated in uncomplicated ankle fractures.
- Meanwhile, the MRI can be useful in in following mentioned evaluations:
- Evaluation of occult fractures
- Evaluation of the post-traumatic or avascular necrosis of carpal bones
- Evaluation of tendons
- Evaluation of nerve
- Evaluation of carpal tunnel syndrome
-
PD Subchondral fracture of the talar dome. Note the intact overlying cartilage.
-
T2 fat sat Subchondral fracture of the talar dome. Note the intact overlying cartilage.
Other Imaging Findings[35]
There are no other imaging findings associated with Ankle fracture
Other Diagnostic Studies[35]
There are no other Diagnostic studies associated with Ankle fracture
Treatment [36]
Immediate stabilization of patients is the first step. Then the radial fracture and the DRUJ stabilization is recommended in these cases. Open ankle fractures considered as a surgical emergency. Ankle fracture occurs in younger patients who are skeletally immature; the normally they treated using a closed reduction and casting. Since closed reduction and cast application have led to unsatisfactory results. Then, Almost always the open reduction are necessary for the Ankle fracture. There are controversies regarding the indications for intramedullary nailing of ankle fractures.
Non-Operative Treatment [37][38]
- The first step in managing a patient with a fracture is to stabilize the patient if he/she is unstable due to blood loss, etc by giving them intravenous fluids and giving them some painkillers if the pain is severe.
- In children, the usual plan is to attempt closed reduction followed by cast immobilization. In adults, treatment with immobilization in a molded long arm cast can be used in those rare occasions of a non-displaced fracture of the ankle joint. If the fracture shifts in position, it may require surgery to put the bones back together.
- Rigid immobilization is suggested in preference to removable splints in nonoperative treatment for the management of the Ankle fracture
- For all patients with Ankle fracture, a post-reduction true lateral radiograph is suggested.
- Operative fixation is suggested in preference to cast fixation for fractures with post-reduction radial shortening greater than 3 mm, dorsal tilt greater than 10º, or intra-articular displacement or step-off greater than 2 mm.
- Patients probably do not need to begin early wrist motion routinely after stable fracture fixation.
- Adjuvant treatment of Ankle fracture with vitamin C is suggested for the prevention of disproportionate pain
- Lateral epicondylar fractures should be immobilized for 7 days with patients elbow flexed at 90º, with the supinated ankle , and the extended wrist for relaxing the extensor muscles.
Complications of Non-surgical therapy[37]
Failure of non-surgical therapy is common:
- Re-displacement to its original position even in a cast
- Stiffness
- Post traumatic osteoarthritis leading to wrist pain and loss of function
- Other risks specific to cast treatment include:
- Compression of the swollen arm causing compartment syndrome
- Reflex sympathetic dystrophy is a serious complication
- Stiffness is universal following a prolonged period of immobilization and swelling
Surgery [39][40][41]
Returning to the normal physical activity after Ankle fracturecan take weeks to months of therapy under supervision an orthopedist. Meanwhile, a physiotherapy can be helpful for patient to achieve the normal wrist and elbow function caused by the immobilisation. All adult Ankle fracture should be considered to be treated with open reduction and internal fixation (ORIF).
External fixation: For severe open fractures Open reduction and internal fixation: For distal Ankle fracture which depending on each patients condition the following may be needed:
Nerve placement Bone grafting Osteotomy Arthrodesis
-
Screw-plate stabilization of the fibular fracture and trans-syndesmotic screw stabilizing the ankle mortise.
-
Plate and screw internal fixation of distal fibular fracture. Lateral talar shift has been reduced with reduction of the fibula - distal syndesmosis must have been obviously stable at surgery and thus no diastasis screw was used.
Operation [42][43]
- There are a variety of methods and implants useful to stabilize the Ankle fracturee, ranging from closed reduction and percutaneous pin fixation to the use of intra-medullary devices.
- However, the most common fixation methods to treat complex Ankle fracture include external fixation, and open reduction and internal fixation.
External Fixation With or Without Percutaneous Pin Fixation
- Ankle spanning external fixation employs ligamentotaxis to restore and maintain length, alignment, and rotation of bone.
- Reduction is typically obtained through closed or minimally open methods and preserves the fracture biology.
- The addition of percutaneous pins enhances the ability to reduce and stabilize fracture fragments.
Complications of External Fixation
- Pin tract infection
- Injury to the Superficial branch of the nerve
- Complex regional pain syndrome
Open reduction and internal fixation with plates and screws
- This is the most common type of surgical repair for Ankle fracture
- During this type of procedure, the bone fragments are first repositioned (reduced) into their normal alignment.
- The bones held together with special screws and metal plates attached to the outer surface of the bone.
Complications of open reduction and internal fixation with plates and screws =
- Infection
- Damage to nerves and blood vessels
- Synostosis
- Nonunion
Pain Management [44][45]
Pain after an injury or surgery is a natural part of the healing process.
Medications are often prescribed for short-term pain relief after surgery or an injury such as:
- opioids
- non-steroidal anti-inflammatory drugs (NSAIDs)
- local anesthetics
Be aware that although opioids help relieve pain after surgery or an injury, they are a narcotic and can be addictive. It is important to use opioids only as directed by doctor.
Interventions [46]
The following options can be helpful for patients to rehabilitate after their fracture :
- Joints mobilization
- compression bandage
- Soft tissue massage
- Exercises and Activity modification
Postoperative Rehabilitation [47]
- Complex Ankle fracture warrant individualized immobilization and rehabilitation strategies.
- Because most multifragmentary Ankle fracture are the result of high-energy injuries, a prolonged period of wrist immobilization and soft-tissue rest may be beneficial and has not been shown to affect clinical outcomes.
- The ankle is typically immobilized for 6 weeks post-operatively in a splint with Full weight bearing commences at approximately 3 months post-operatively after consolidation of the fracture is noted on radiographs.
- The presence of varying degrees of ankle stiffness is inevitable and may result from poor pain control, lack of effort in controlled mobilization, edema, concomitant ipsilateral lower extremity fractures, or peripheral nerve injuries. Early stretching and mobilization of the intrinsic and extrinsic tendons of the hand is important to prevent finger stiffness. Edema control can be initiated with compression gloves, digital massage, and active and passive ROM of the ankle. A home exercise program or outpatient occupational therapy is started immediately post-operatively to maintain full range of motion of the ankle and limit the development of intrinsic muscle tightnes
Primary Prevention [48][49]
There are various preventive options to reduce the incidence of the Ankle fracture
- Using ankle guards during practicing sports (skating, biking)
- Using ankle guards during driving motorbikes
- Avoid falls in elderly individuals
- Prevention and/or treatment of osteoporosis
- Healthy diet
Secondary Prevention [50]
It should be noted that the Post-menopausal women specially older than the age of 65 are at the higher risk of osteoporosis consequently these type of patients at greater risk for the pathological fractures .
So the Calcium and vitamin D supplementation play important role in increasing the bone mineral density (BMD) consequently decrease the risk of fracture in these type of patients. Also, avoiding excessive alcohol and quitting smoking play important role in this regard.
Detecting osteoporosis
- DEXA(dual-energy x-ray absorptiometry) scan
- Serum calcium and vitamin D levels
- Ultrasonography of the calcaneus
Pharmacological therapy [51]
- The primary goal for the treatment of osteoporosis is to reduce longtime fracture risk in patients. Increasing bone mineral density (BMD) in response to the treatment is far less important than improvement of clinical aspects of osteoporosis, i.e., osteoporoticfracture. Therefore, most of the drugs efficacy is measured by the extent they improve the fracture risk instead of increasing BMD.
- During the treatment, if a single fracture happens, it does not necessarily indicate treatment failure or the need to be started on an alternative treatment or patient referral to a specialist.
- Calcium and vitamin D supplementation have been found to be effective in reducing the long term fracture risk, significantly. In order to suggest the people to use vitamin D and calcium supplements, the physician needs to make sure that patient is not able to obtain the nutrients through the daily intake. The available supplemental ions of calcium include calcium carbonate, calcium citrate, and vitamin D3 in various dosage forms.
Life style modifications[52]
- Exercise: Exercise promotes the mineralization of bone and bone accumulation particularly during growth. High impact exercise, in particular, has been shown to prevent the development of osteoporosis. However, it can have a negative effect on bone mineralization in cases of poor nutrition, such as anorexia nervosa and celiac disease.
- Nutrition: A diet high in calcium and vitamin D prevents bone loss. Patients at risk for osteoporosis, such as persons with chronic steroid use are generally treated with vitamin D and calcium supplementation. In renal disease, more active forms of vitamin D, such as 1,25-dihydroxycholecalciferol or calcitriol are used; as the kidney cannot adequately generate calcitriol from calcidiol (25-hydroxycholecalciferol), which is the storage form of vitamin D.
- By quitting smoking, osteoporosis as well as other diseases can be prevented.
- Avoiding excessive alcohol intake or drinking only in moderation.
See also
- triplane fracture
- Tillaux fracture
- Bosworth fracture
- pilon fracture
- Wagstaffe-Le Forte fracture
- Maisonneuve Fracture
References
- ↑ Mason LW, Marlow WJ, Widnall J, Molloy AP (November 2017). "Pathoanatomy and Associated Injuries of Posterior Malleolus Fracture of the Ankle". Foot Ankle Int. 38 (11): 1229–1235. doi:10.1177/1071100717719533. PMID 28758439.
- ↑ Mittal R, Harris IA, Adie S, Naylor JM (March 2017). "Surgery for Type B Ankle Fracture Treatment: a Combined Randomised and Observational Study (CROSSBAT)". BMJ Open. 7 (3): e013298. doi:10.1136/bmjopen-2016-013298. PMC 5372107. PMID 28348185.
- ↑ Winge R, Bayer L, Gottlieb H, Ryge C (August 2017). "Compression therapy after ankle fracture surgery: a systematic review". Eur J Trauma Emerg Surg. 43 (4): 451–459. doi:10.1007/s00068-017-0801-y. PMID 28624992.
- ↑ Guo CJ, Li XC, Hu M, Xu Y, Xu XY (February 2017). "Realignment Surgery for Malunited Ankle Fracture". Orthop Surg. 9 (1): 49–53. doi:10.1111/os.12312. PMID 28276651.
- ↑ Jonckheer P, Willems T, De Ridder R, Paulus D, Holdt Henningsen K, San Miguel L, De Sutter A, Roosen P (2016). "Evaluating fracture risk in acute ankle sprains: Any news since the Ottawa Ankle Rules? A systematic review". Eur J Gen Pract. 22 (1): 31–41. doi:10.3109/13814788.2015.1102881. PMID 26691309.
- ↑ Elmajee M, Rafee A, Williams T (2017). "Ankle Fracture Associated With Rupture of the Achilles Tendon: Case Report and Review of the Literature". J Foot Ankle Surg. 56 (6): 1320–1322. doi:10.1053/j.jfas.2017.05.043. PMID 29079241.
- ↑ González-Lucena G, Pérez-Prieto D, López-Alcover A, Ginés-Cespedosa A (2018). "Ankle fracture controversies: Do the foot and ankle specialists have a different vision?". Rev Esp Cir Ortop Traumatol. 62 (1): 27–34. doi:10.1016/j.recot.2017.10.001. PMID 29162365.
- ↑ Ortiz CA, Wagner P, Wagner E (June 2016). "State-of-the-Art in Ankle Fracture Management in Chile". Foot Ankle Clin. 21 (2): 367–89. doi:10.1016/j.fcl.2016.01.008. PMID 27261811.
- ↑ Cuzmar-Grimalt D, Escudero-Heldt M, Aldunate-González JT, Plaza-Guzmán N (2016). "[Ankle fracture in adolescents: triplanar injury associated to fracture of leg]". Acta Ortop Mex (in Spanish; Castilian). 30 (3): 144–146. PMID 27984688.
- ↑ Stull JD, Bhat SB, Kane JM, Raikin SM (September 2017). "Economic Burden of Inpatient Admission of Ankle Fractures". Foot Ankle Int. 38 (9): 997–1004. doi:10.1177/1071100717709576. PMID 28639869.
- ↑ Hong X, Bao CS, Zheng WL (October 2018). "Inference on Injury Mechanism of Ankle Fracture by Lauge-Hansen Classification". Fa Yi Xue Za Zhi. 34 (5): 512–515. doi:10.12116/j.issn.1004-5619.2018.05.015. PMID 30468054.
- ↑ Ashton F, Hamid K, Sulieman S, Eardley W, Baker P (April 2017). "Factors Influencing patient experience and satisfaction following surgical management of ankle fractures". Injury. 48 (4): 960–965. doi:10.1016/j.injury.2017.02.017. PMID 28249677.
- ↑ Woo SH, Bae SY, Chung HJ (January 2018). "Short-Term Results of a Ruptured Deltoid Ligament Repair During an Acute Ankle Fracture Fixation". Foot Ankle Int. 39 (1): 35–45. doi:10.1177/1071100717732383. PMID 29078057.
- ↑ Thakore RV, Hooe BS, Considine P, Sathiyakumar V, Onuoha G, Hinson JK, Obremskey WT, Sethi MK (2015). "Ankle fractures and employment: a life-changing event for patients". Disabil Rehabil. 37 (5): 417–22. doi:10.3109/09638288.2014.923525. PMID 24856790.
- ↑ Krishna SV, Pilar A, Pai SN, Issac T (2016). "Traumatic Rupture of Posterior Tibial Tendon Following Closed Supination-Adduction Ankle Fracture: A Case Report". JBJS Case Connect. 6 (3): e75. doi:10.2106/JBJS.CC.15.00273. PMID 29252652.
- ↑ van Zuuren WJ, Schepers T, Beumer A, Sierevelt I, van Noort A, van den Bekerom M (September 2017). "Acute syndesmotic instability in ankle fractures: A review". Foot Ankle Surg. 23 (3): 135–141. doi:10.1016/j.fas.2016.04.001. PMID 28865579. Vancouver style error: initials (help)
- ↑ Juto H, Möller M, Wennergren D, Edin K, Apelqvist I, Morberg P (November 2016). "Substantial accuracy of fracture classification in the Swedish Fracture Register: Evaluation of AO/OTA-classification in 152 ankle fractures". Injury. 47 (11): 2579–2583. doi:10.1016/j.injury.2016.05.028. PMID 27645617.
- ↑ Boszczyk A, Fudalej M, Kwapisz S, Klimek U, Maksymowicz M, Kordasiewicz B, Rammelt S (January 2018). "Ankle fracture - Correlation of Lauge-Hansen classification and patient reported fracture mechanism". Forensic Sci. Int. 282: 94–100. doi:10.1016/j.forsciint.2017.11.023. PMID 29182957.
- ↑ Briet JP, Houwert RM, Smeeing D, Dijkgraaf M, Verleisdonk EJ, Leenen L, Hietbrink F (2017). "Differences in Classification Between Mono- and Polytrauma and Low- and High-Energy Trauma Patients With an Ankle Fracture: A Retrospective Cohort Study". J Foot Ankle Surg. 56 (4): 793–796. doi:10.1053/j.jfas.2017.04.012. PMID 28633779. Vancouver style error: initials (help)
- ↑ 20.0 20.1 Gong XF, Lyu YW, Wang JH, Wang Y, Wu Y, Wang MY (April 2017). "[A correlation analysis of the ankle CT and ankle fracture classification]". Beijing Da Xue Xue Bao (in Chinese). 49 (2): 281–285. PMID 28416839.
- ↑ Walsh AS, Sinclair V, Watmough P, Henderson AA (March 2018). "Ankle fractures: Getting it right first time". Foot (Edinb). 34: 48–52. doi:10.1016/j.foot.2017.11.013. PMID 29287221.
- ↑ Neilly D, Baliga S, Munro C, Johnston A (October 2015). "Acute compartment syndrome of the foot following open reduction and internal fixation of an ankle fracture". Injury. 46 (10): 2064–8. doi:10.1016/j.injury.2015.06.006. PMID 26190633.
- ↑ Denning JR (January 2017). "Complications of Pediatric Foot and Ankle Fractures". Orthop. Clin. North Am. 48 (1): 59–70. doi:10.1016/j.ocl.2016.08.010. PMID 27886683.
- ↑ Hinds RM, Garner MR, Lazaro LE, Warner SJ, Loftus ML, Birnbaum JF, Burket JC, Lorich DG (February 2015). "Ankle fracture spur sign is pathognomonic for a variant ankle fracture". Foot Ankle Int. 36 (2): 159–64. doi:10.1177/1071100714553470. PMID 25278340.
- ↑ 25.0 25.1 Toth MJ, Yoon RS, Liporace FA, Koval KJ (October 2017). "What's new in ankle fractures". Injury. 48 (10): 2035–2041. doi:10.1016/j.injury.2017.08.016. PMID 28826651.
- ↑ Goost H, Wimmer MD, Barg A, Kabir K, Valderrabano V, Burger C (May 2014). "Fractures of the ankle joint: investigation and treatment options". Dtsch Arztebl Int. 111 (21): 377–88. doi:10.3238/arztebl.2014.0377. PMC 4075279. PMID 24939377.
- ↑ Young KW, Kim JS, Cho JH, Kim HS, Cho HK, Lee KT (March 2015). "Paratrooper's ankle fracture: posterior malleolar fracture". Clin Orthop Surg. 7 (1): 15–21. doi:10.4055/cios.2015.7.1.15. PMC 4329528. PMID 25729514.
- ↑ Ovaska M, Madanat R, Mäkinen T, Lindahl J (2015). "[Complications in ankle fracture surgery]". Duodecim (in Finnish). 131 (16): 1451–9. PMID 26485938.
- ↑ Hsu RY, Lee Y, Hayda R, DiGiovanni CW, Mor V, Bariteau JT (November 2015). "Morbidity and Mortality Associated with Geriatric Ankle Fractures: A Medicare Part A Claims Database Analysis". J Bone Joint Surg Am. 97 (21): 1748–55. doi:10.2106/JBJS.O.00095. PMID 26537162.
- ↑ Beckenkamp PR, Lin CW, Chagpar S, Herbert RD, van der Ploeg HP, Moseley AM (November 2014). "Prognosis of physical function following ankle fracture: a systematic review with meta-analysis". J Orthop Sports Phys Ther. 44 (11): 841–51, B2. doi:10.2519/jospt.2014.5199. PMID 25269609.
- ↑ Yousri T, Jackson M (February 2015). "Ankle fractures: When can I drive, doctor? A simulation study". Injury. 46 (2): 399–404. doi:10.1016/j.injury.2014.10.041. PMID 25554425.
- ↑ Boszczyk A, Fudalej M, Kwapisz S, Błoński M, Kiciński M, Kordasiewicz B, Rammelt S (October 2018). "X-ray features to predict ankle fracture mechanism". Forensic Sci. Int. 291: 185–192. doi:10.1016/j.forsciint.2018.08.042. PMID 30216844.
- ↑ Golshani A, Zhu L, Cai C, Beckmann NM (February 2017). "Incidence and Association of CT Findings of Ankle Tendon Injuries in Patients Presenting With Ankle and Hindfoot Fractures". AJR Am J Roentgenol. 208 (2): 373–379. doi:10.2214/AJR.16.16657. PMID 28112555.
- ↑ Park YH, Yoon MA, Choi WS, Choi GW, Hong SJ, Kim HJ (April 2018). "The predictive value of MRI in the syndesmotic instability of ankle fracture". Skeletal Radiol. 47 (4): 533–540. doi:10.1007/s00256-017-2821-4. PMID 29196821.
- ↑ 35.0 35.1 McDonald MR, Bulka CM, Thakore RV, Obremskey WT, Ehrenfeld JM, Jahangir AA, Sethi MK (September 2014). "Ankle radiographs in the early postoperative period: do they matter?". J Orthop Trauma. 28 (9): 538–41. doi:10.1097/BOT.0000000000000052. PMID 24375274.
- ↑ Shen MS, Dodd AC, Lakomkin N, Mousavi I, Bulka C, Jahangir AA, Sethi MK (December 2017). "Open treatment of ankle fracture as inpatient increases risk of complication". J Orthop Traumatol. 18 (4): 431–438. doi:10.1007/s10195-017-0472-9. PMC 5685990. PMID 29071495.
- ↑ 37.0 37.1 Drakos MC, Murphy CI (November 2014). "Bracing versus casting in ankle fractures". Phys Sportsmed. 42 (4): 60–70. doi:10.3810/psm.2014.11.2092. PMID 25419889.
- ↑ Qin C, Dekker RG, Helfrich MM, Kadakia AR (January 2018). "Outpatient Management of Ankle Fractures". Orthop. Clin. North Am. 49 (1): 103–108. doi:10.1016/j.ocl.2017.08.012. PMID 29145978.
- ↑ Gonzalez TA, Macaulay AA, Ehrlichman LK, Drummond R, Mittal V, DiGiovanni CW (May 2016). "Arthroscopically Assisted Versus Standard Open Reduction and Internal Fixation Techniques for the Acute Ankle Fracture". Foot Ankle Int. 37 (5): 554–62. doi:10.1177/1071100715620455. PMID 26660864.
- ↑ Ostrum RF, Avery MC (August 2016). "Open Reduction Internal Fixation of a Bimalleolar Ankle Fracture With Syndesmotic Injury". J Orthop Trauma. 30 Suppl 2: S43–4. doi:10.1097/BOT.0000000000000588. PMID 27441940.
- ↑ Sung KH, Kwon SS, Yun YH, Park MS, Lee KM, Nam M, Jung JH, Lee SY (2018). "Short-Term Outcomes and Influencing Factors After Ankle Fracture Surgery". J Foot Ankle Surg. 57 (6): 1096–1100. doi:10.1053/j.jfas.2018.03.045. PMID 30146336.
- ↑ Jung HG, Kim JI, Park JY, Park JT, Eom JS, Lee DO (2016). "Is Hardware Removal Recommended after Ankle Fracture Repair?". Biomed Res Int. 2016: 5250672. doi:10.1155/2016/5250672. PMC 5081426. PMID 27819005.
- ↑ Chan KB, Lui TH (November 2016). "Role of Ankle Arthroscopy in Management of Acute Ankle Fracture". Arthroscopy. 32 (11): 2373–2380. doi:10.1016/j.arthro.2016.08.016. PMID 27816101.
- ↑ Saper D, Litrenta J, Otlans P, Daley J, Tornetta P (August 2015). "Factors affecting pain in acute ankle fractures: A prospective evaluation". Injury. 46 (8): 1641–4. doi:10.1016/j.injury.2015.05.009. PMID 26021663.
- ↑ Lovy AJ, Dowdell J, Keswani A, Koehler S, Kim J, Weinfeld S, Joseph D (March 2017). "Nonoperative Versus Operative Treatment of Displaced Ankle Fractures in Diabetics". Foot Ankle Int. 38 (3): 255–260. doi:10.1177/1071100716678796. PMID 27923219.
- ↑ Olsen LL, Møller AM, Brorson S, Hasselager RB, Sort R (February 2017). "The impact of lifestyle risk factors on the rate of infection after surgery for a fracture of the ankle". Bone Joint J. 99-B (2): 225–230. doi:10.1302/0301-620X.99B2.BJJ-2016-0344.R1. PMID 28148665.
- ↑ Nortunen S, Leskelä HV, Haapasalo H, Flinkkilä T, Ohtonen P, Pakarinen H (March 2017). "Dynamic Stress Testing Is Unnecessary for Unimalleolar Supination-External Rotation Ankle Fractures with Minimal Fracture Displacement on Lateral Radiographs". J Bone Joint Surg Am. 99 (6): 482–487. doi:10.2106/JBJS.16.00450. PMID 28291180.
- ↑ KARNAUKHOV AK (1964). "[POINTED PIN FOR OSTEOSYNTHESIS OF ANKLE FRACTURES]". Voen Med Zh (in Russian). 51: 76. PMID 14291935.
- ↑ Gee CW, Dahal L, Rogers BA, Harry LE (October 2015). "Ankle fractures in the elderly: an overlooked burden". Br J Hosp Med (Lond). 76 (10): 564–9. doi:10.12968/hmed.2015.76.10.564. PMID 26457936.
- ↑ Zwipp H, Amlang M (April 2014). "[Treatment of fractures of the ankle in the elderly]". Orthopade (in German). 43 (4): 332–8. doi:10.1007/s00132-013-2168-z. PMID 24676720.
- ↑ Ovaska M (February 2015). "Complications in ankle fracture surgery". Acta Orthop Suppl. 86 (358): 1–32. doi:10.3109/17453674.2014.100227. PMID 25586467.
- ↑ Cordova CB, Dunn JC, Kusnezov N, Bader JM, Waterman BR, Orr JD (February 2018). "Comparing clinician use of three ankle fracture classifications". JAAPA. 31 (2): 36–39. doi:10.1097/01.JAA.0000529773.90897.9f. PMID 29369927.