Chondromyxoid fibroma: Difference between revisions
No edit summary |
(→Causes) |
||
| (35 intermediate revisions by 2 users not shown) | |||
| Line 2: | Line 2: | ||
{{SI}} | {{SI}} | ||
{{CMG}}; {{AE}} | {{CMG}}; {{AE}} {{Rohan}} | ||
{{SK}} | |||
==Overview== | ==Overview== | ||
Chondromyxoid fibroma is a rare [[benign]] [[Bone tumors|bone tumor]] accounting for approximately 1% of all [[benign]] [[bone tumors]]. Chondromyxoid fibroma affects all age groups. It is more commonly seen during the second and third decades of life. [[Male|Men]] are more commonly affected than [[Female|women]]. Chondromyxoid fibroma arising from the [[Growth plate|physeal]] remnant is the commonly proposed theory in the [[pathogenesis]] of this [[tumor]]. It is predominantly found in the [[Metaphysis|metaphyses]] of the [[Long bone|long bones]]. The [[Bone|bones]] involved include [[tibia]], [[distal]] [[femur]], [[pelvis]], [[feet]] and [[hands]]. [[Chromosome 6]] appears to be involved in chondromyxoid fibroma. Over expression of the [[Glutamic acid|glutamate]] [[Receptor (biochemistry)|receptor]] [[gene]] GRM1 in [[Patient|patients]] with chondromyxoid fibroma via [[promoter]] swapping and [[Fusion gene|gene fusion]] has been observed. The [[hallmark]] of chondromyxoid fibroma is [[pain]], [[Edema|swelling]], and [[Bone fracture|pathological fracture]]. The mainstay of treatment for chondromyxoid fibroma is [[surgery]] ([[curettage]] and [[bone grafting]]). | |||
==Historical Perspective== | |||
In 1948, Jaffe and Lichtenstein described chondromyxoid fibroma for the first time.<ref name="pmid18891025">{{cite journal| author=JAFFE HL, LICHTENSTEIN L| title=Chondromyxoid fibroma of bone; a distinctive benign tumor likely to be mistaken especially for chondrosarcoma. | journal=Arch Pathol (Chic) | year= 1948 | volume= 45 | issue= 4 | pages= 541-51 | pmid=18891025 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18891025 }} </ref> | |||
==Classification== | |||
Chondromyxoid fibroma can be [[Classification|classified]] based on [[imaging]] findings. | |||
===Enneking (MSTS) Staging System=== | |||
*The Enneking [[Surgery|surgical]] [[Cancer staging|staging]] system (also known as the MSTS system) for [[benign]] [[Musculoskeletal system|musculoskeletal]] [[Tumor|tumors]] is based on [[radiographic]] characteristics of the [[tumor]] host margin.<ref name="pmid20333492">{{cite journal| author=Jawad MU, Scully SP| title=In brief: classifications in brief: enneking classification: benign and malignant tumors of the musculoskeletal system. | journal=Clin Orthop Relat Res | year= 2010 | volume= 468 | issue= 7 | pages= 2000-2 | pmid=20333492 | doi=10.1007/s11999-010-1315-7 | pmc=2882012 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20333492 }} </ref> | |||
*It is widely accepted and routinely used [[classification]]. | |||
{| style="border: 0px; font-size: 90%; margin: 3px; width: 1000px" align="center" | |||
| valign="top" | | |||
|- | |||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Stages}} | |||
! style="background: #4479BA; width: 300px;" | {{fontcolor|#FFF|Description}} | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold; text-align:center;" |1 | |||
| style="padding: 5px 5px; background: #F5F5F5;" | Latent: Well demarcated borders | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold; text-align:center;" |2 | |||
| style="padding: 5px 5px; background: #F5F5F5;" | Active: Indistinct borders | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold; text-align:center;" |3 | |||
| style="padding: 5px 5px; background: #F5F5F5;" | Aggressive: Indistinct borders | |||
|} | |||
==Pathophysiology== | |||
*The exact [[etiology]] of chondromyxoid fibroma is unknown.<ref>{{cite book | last = Peabody | first = Terrance | title = Orthopaedic oncology : primary and metastatic tumors of the skeletal system | publisher = Springer | location = Cham | year = 2014 | isbn = 9783319073224 }}</ref> | |||
*Chondromyxoid fibroma arising from the [[Growth plate|physeal]] remnant is the commonly proposed theory in the [[pathogenesis]] of chondromyxoid fibroma.<ref name="pmid9229417">{{cite journal| author=Brien EW, Mirra JM, Kerr R| title=Benign and malignant cartilage tumors of bone and joint: their anatomic and theoretical basis with an emphasis on radiology, pathology and clinical biology. I. The intramedullary cartilage tumors. | journal=Skeletal Radiol | year= 1997 | volume= 26 | issue= 6 | pages= 325-53 | pmid=9229417 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9229417 }} </ref> | |||
*It is predominantly found in the [[Metaphysis|metaphyses]] of the [[Long bone|long bones]].<ref name="pmid498016">{{cite journal| author=Cuvelier CA, Roels HJ| title=Cytophotometric studies of the nuclear DNA content in cartilaginous tumors. | journal=Cancer | year= 1979 | volume= 44 | issue= 4 | pages= 1363-74 | pmid=498016 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=498016 }} </ref> | |||
*The bones involved by chondromyxoid fibroma includes [[tibia]], [[Anatomical terms of location|distal]] [[femur]], [[pelvis]], [[feet]] and [[Hand|hands]].<ref name="pmid9648559">{{cite journal| author=Halbert AR, Harrison WR, Hicks MJ, Davino N, Cooley LD| title=Cytogenetic analysis of a scapular chondromyxoid fibroma. | journal=Cancer Genet Cytogenet | year= 1998 | volume= 104 | issue= 1 | pages= 52-6 | pmid=9648559 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9648559 }} </ref> | |||
===Genetics=== | |||
*[[Chromosome 6]] appears to be involved in chondromyxoid fibroma.<ref name="pmid498016" /><ref name="pmid12606137">{{cite journal| author=Buddingh EP, Naumann S, Nelson M, Neffa JR, Birch N, Bridge JA| title=Cytogenetic findings in benign cartilaginous neoplasms. | journal=Cancer Genet Cytogenet | year= 2003 | volume= 141 | issue= 2 | pages= 164-8 | pmid=12606137 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12606137 }} </ref> | |||
*The non-random clonal abnormalities involves 6p25, 6q13 and 6q23.<ref name="pmid498016">{{cite journal| author=Cuvelier CA, Roels HJ| title=Cytophotometric studies of the nuclear DNA content in cartilaginous tumors. | journal=Cancer | year= 1979 | volume= 44 | issue= 4 | pages= 1363-74 | pmid=498016 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=498016 }} </ref> | |||
*[[Shotgun sequencing|Whole-genome mate-pair sequencing]] and [[RNA]] sequencing showed over expression of the [[glutamate receptor]] [[gene]] GRM1 in [[Patient|patients]] with chondromyxoid fibroma via [[promoter]] swapping and [[Fusion gene|gene fusion]].<ref name="pmid24658000">{{cite journal| author=Nord KH, Lilljebjörn H, Vezzi F, Nilsson J, Magnusson L, Tayebwa J et al.| title=GRM1 is upregulated through gene fusion and promoter swapping in chondromyxoid fibroma. | journal=Nat Genet | year= 2014 | volume= 46 | issue= 5 | pages= 474-7 | pmid=24658000 | doi=10.1038/ng.2927 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24658000 }} </ref> | |||
==Causes== | |||
There are no established causes of chondromyxoid fibroma.<ref name="pmid6337162">{{cite journal| author=Gherlinzoni F, Rock M, Picci P| title=Chondromyxoid fibroma. The experience at the Istituto Ortopedico Rizzoli. | journal=J Bone Joint Surg Am | year= 1983 | volume= 65 | issue= 2 | pages= 198-204 | pmid=6337162 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=6337162 }} </ref> | |||
==Differentiating Chondromyxoid Fibroma from Other Diseases== | |||
Chondromyxoid fibroma must be differentiated from the following [[bone]] disorders:<ref name="pmid19846816">{{cite journal| author=Bergman S, Madden CR, Geisinger KR| title=Fine-needle aspiration biopsy of chondromyxoid fibroma: an investigation of four cases. | journal=Am J Clin Pathol | year= 2009 | volume= 132 | issue= 5 | pages= 740-5 | pmid=19846816 | doi=10.1309/AJCPFJZ8AKMFUAFP | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19846816 }} </ref> | |||
{| | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Disease | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |'''Bubbly lytic lesion on x-ray''' | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |'''Lakes of Blood on histology''' | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Diagnosis | |||
! align="center" style="background:#4479BA; color: #FFFFFF;" + |Treatment is curretage and bone grafting | |||
|- | |||
! align="center" style="background:#DCDCDC;" + |Chondromyxoid Fibroma | |||
| align="center" style="background:#F5F5F5;" + | - | |||
| align="center" style="background:#F5F5F5;" + | - | |||
| align="center" style="background:#F5F5F5;" + |[[Radiology]] and [[biopsy]] | |||
| align="center" style="background:#F5F5F5;" + | + | |||
|- | |||
! align="center" style="background:#DCDCDC;" + |[[Unicameral bone cyst]] | |||
| align="center" style="background:#F5F5F5;" + | + | |||
| align="center" style="background:#F5F5F5;" + | - | |||
| align="center" style="background:#F5F5F5;" + |[[Radiology]] and [[biopsy]] | |||
| align="center" style="background:#F5F5F5;" + | - | |||
|- | |||
! align="center" style="background:#DCDCDC;" + |[[Non ossifying fibroma]] | |||
| align="center" style="background:#F5F5F5;" + | + | |||
| align="center" style="background:#F5F5F5;" + | - | |||
| align="center" style="background:#F5F5F5;" + |[[Radiology]] and [[biopsy]] | |||
| align="center" style="background:#F5F5F5;" + | - | |||
|- | |||
! align="center" style="background:#DCDCDC;" + |[[Giant cell tumor of bone|Giant cell tumor]] | |||
| align="center" style="background:#F5F5F5;" + | - | |||
| align="center" style="background:#F5F5F5;" + | - | |||
| align="center" style="background:#F5F5F5;" + |[[Radiology]] and [[Biopsy]] | |||
| align="center" style="background:#F5F5F5;" + | + | |||
|- | |||
! align="center" style="background:#DCDCDC;" + |[[Chondroblastoma]] | |||
| align="center" style="background:#F5F5F5;" + | - | |||
| align="center" style="background:#F5F5F5;" + | - | |||
| align="center" style="background:#F5F5F5;" + |[[Biopsy]] | |||
| align="center" style="background:#F5F5F5;" + | + | |||
|- | |||
! align="center" style="background:#DCDCDC;" + |[[Aneurysmal bone cyst]] | |||
| align="center" style="background:#F5F5F5;" + | + | |||
| align="center" style="background:#F5F5F5;" + | + | |||
| align="center" style="background:#F5F5F5;" + |[[Radiology]] and [[biopsy]] | |||
| align="center" style="background:#F5F5F5;" + | + | |||
|- | |||
! align="center" style="background:#DCDCDC;" + |[[Osteoblastoma]] | |||
| align="center" style="background:#F5F5F5;" + | - | |||
| align="center" style="background:#F5F5F5;" + | - | |||
| align="center" style="background:#F5F5F5;" + |[[Radiology]] and [[biopsy]] | |||
| align="center" style="background:#F5F5F5;" + | + | |||
|- | |||
! align="center" style="background:#DCDCDC;" + |Telangiectatic [[osteosarcoma]] | |||
| align="center" style="background:#F5F5F5;" + | - | |||
| align="center" style="background:#F5F5F5;" + | + | |||
| align="center" style="background:#F5F5F5;" + |[[Radiology]] and [[biopsy]] | |||
| align="center" style="background:#F5F5F5;" + | - | |||
|} | |||
==Epidemiology and Demographics== | |||
*Chondromyxoid fibroma is a rare [[benign]] [[Bone tumors|bone tumor]] accounting for approximately 1% of all [[benign]] [[bone tumors]].<ref name="pmid26981481">{{cite journal| author=Pintor F, Bahamondes C, Campos O, Zivov A| title=Chondromyxoid fibroma of zygoma in an elderly patient: A rare presentation. | journal=Ann Maxillofac Surg | year= 2015 | volume= 5 | issue= 2 | pages= 244-8 | pmid=26981481 | doi=10.4103/2231-0746.175755 | pmc=4772571 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26981481 }} </ref> | |||
*Chondromyxoid fibroma affects all age groups. | |||
*It is more commonly seen during the second and third decades of life. | |||
*[[Male|Men]] are more commonly affected than [[Female|women]]. | |||
*There is no racial predilection to chondromyxoid fibroma. | |||
==Risk Factors== | |||
There are no established [[Risk factor|risk factors]] for chondromyxoid fibroma. | |||
==Screening== | |||
There is insufficient evidence to recommend routine [[Screening (medicine)|screening]] for chondromyxoid fibroma. | |||
==Natural History, Complications, and Prognosis== | |||
Common [[Complication (medicine)|complications]] of chondromyxoid fibroma include: | |||
*[[Bone fracture|Pathological fracture]] | |||
*[[Premature]] [[Epiphyseal plate|epiphyseal]] closure | |||
*Limb-length discrepancy | |||
*Angular deformity | |||
[[Prognosis]] is generally good for chondromyxoid fibroma. | |||
*[[Prognostic]] variables include: | |||
**[[Children]] | |||
**When the [[Tumor]] is more lobulated with abundant myxoid material | |||
==Diagnosis== | |||
{| align="right" | |||
| | |||
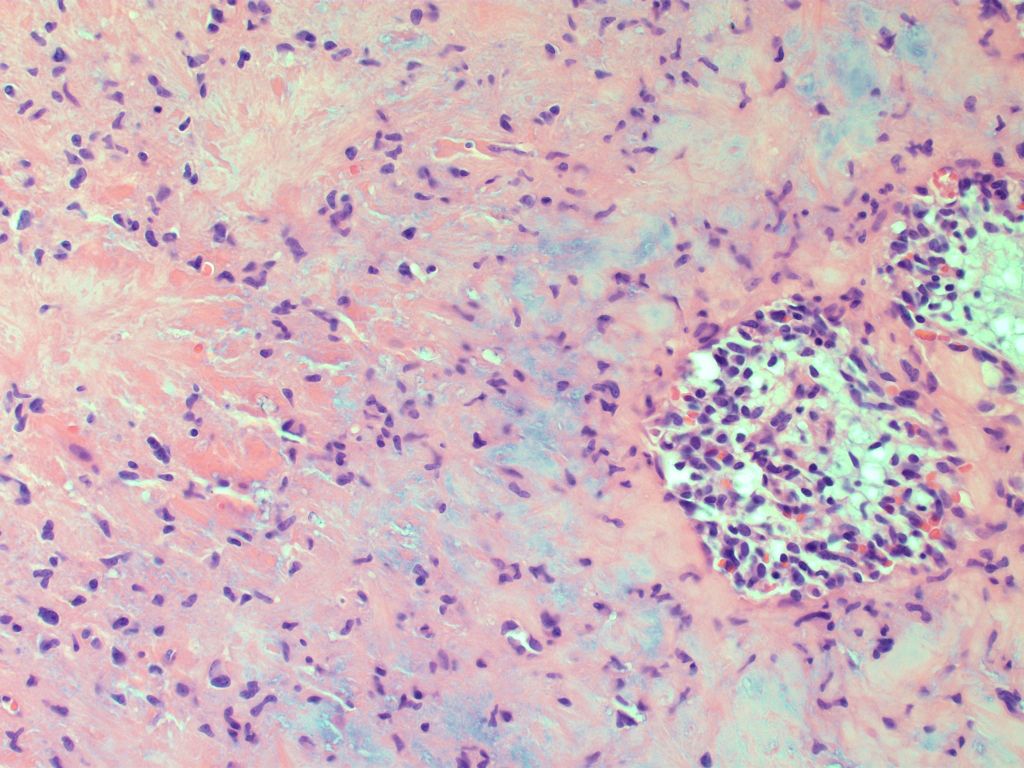
[[File:CMF HISTO.jpg|300px|thumb|Histology of chondromyxoid fibroma showing stellate cells in a myxoid stroma..[https://upload.wikimedia.org/wikipedia/commons/0/05/Bone_ChondromyxoidFibroma_MP3_CTR.jpg Source: Case courtesy of Sarahkayb [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)], from Wikimedia Commons]]] | |||
|} | |||
===Diagnostic Study of Choice=== | |||
*[[Biopsy]] is the [[diagnostic study of choice]] for chondromyxoid fibroma. | |||
*[[Biopsy]] findings under low and high power fields are given below:<ref name="pmid11793371">{{cite journal| author=Tallini G, Dorfman H, Brys P, Dal Cin P, De Wever I, Fletcher CD et al.| title=Correlation between clinicopathological features and karyotype in 100 cartilaginous and chordoid tumours. A report from the Chromosomes and Morphology (CHAMP) Collaborative Study Group. | journal=J Pathol | year= 2002 | volume= 196 | issue= 2 | pages= 194-203 | pmid=11793371 | doi=10.1002/path.1023 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11793371 }} </ref><ref name="pmid15612014">{{cite journal| author=Desai SS, Jambhekar NA, Samanthray S, Merchant NH, Puri A, Agarwal M| title=Chondromyxoid fibromas: a study of 10 cases. | journal=J Surg Oncol | year= 2005 | volume= 89 | issue= 1 | pages= 28-31 | pmid=15612014 | doi=10.1002/jso.20113 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15612014 }} </ref> | |||
====== Under Low Power field: ====== | |||
*It has a biphasic appearance | |||
*It has [[lobules]] and pseudolobules of fibromyxoid [[Tissue (biology)|tissue]] with hypercellular area. | |||
*The [[Cell (biology)|cells]] are [[spindle]]-shaped or [[Stellate cell|stellate]]-shaped and contain [[Hyperchromicity|hyperchromatic]] [[Cell nucleus|nuclei]]. | |||
*[[Multinucleate|Multinucleated]] [[giant cells]] and fibrovascular [[Tissue (biology)|tissue]] may be present between the [[lobules]]. | |||
*Hypocellular area with chondroid material is seen. | |||
====== Under High Power Field: ====== | |||
*The [[tumor]] shows [[Stroma|myxoid stroma]] mixed with [[Stellate cell|stellate cells]]. | |||
*In addition, an area of [[Pleomorphism|pleiomorphic]] [[Cell (biology)|cells]] with bizarre [[Cell nucleus|nuclei]] may be seen. | |||
===History and Symptoms=== | |||
*The majority of [[Patient|patients]] with chondromyxoid fibroma have a positive history of: | |||
**[[Pain]] | |||
**[[Swelling]] | |||
**[[Stiffness]] | |||
**[[Bone fracture|Pathological fracture]] | |||
{| align="right" | |||
| | |||
[[File:XRAY CMF.gif|300px|thumb|X-ray of ulna showing chondromyxoid fibroma.[https://radiopaedia.org/cases/chondromyxoid-fibroma-ulna?lang=us Source: Case courtesy of A.Prof Frank Gaillard, Radiopaedia.org, rID: 6172]]] | |||
|} | |||
===Physical Examination=== | |||
Common [[physical examination]] findings of chondromyxoid fibroma include: | |||
* [[Deformity]] | |||
*[[Swelling]] | |||
*Decreased [[range of motion]] | |||
*[[Warmth receptors|Warmth]] over the affected area | |||
===Laboratory Findings=== | |||
There are no [[Diagnosis|diagnostic]] [[Medical laboratory|laboratory]] findings associated with chondromyxoid fibroma. | |||
===Electrocardiogram=== | |||
There are no [[The electrocardiogram|ECG]] findings associated with chondromyxoid fibroma. | |||
===X-ray=== | |||
[[X-rays|X-ray]] findings include:<ref name="pmid9428071">{{cite journal| author=Marin C, Gallego C, Manjón P, Martinez-Tello FJ| title=Juxtacortical chondromyxoid fibroma: imaging findings in three cases and a review of the literature. | journal=Skeletal Radiol | year= 1997 | volume= 26 | issue= 11 | pages= 642-9 | pmid=9428071 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9428071 }} </ref><ref name="pmid2732329">{{cite journal| author=Merine D, Fishman EK, Rosengard A, Tolo V| title=Chondromyxoid fibroma of the fibula. | journal=J Pediatr Orthop | year= 1989 | volume= 9 | issue= 4 | pages= 468-71 | pmid=2732329 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2732329 }} </ref> | |||
* The [[tumor]] appears as a [[lytic]], eccentric [[Metaphyseal|metaphyse]]<nowiki/>[[Metaphyseal|a]]<nowiki/>l [[lesion]]. | |||
*Size of the [[lesion]] may vary from 2 to 10 cm. | |||
*It has a sharply demarcated border from the adjacent [[bone]]. | |||
{| align="right" | |||
| | |||
[[File:CT CMF.gif|thumb|CT of proximal ulna showing chondromyxoid fibroma.[https://radiopaedia.org/cases/chondromyxoid-fibroma-ulna?lang=us Source: Case courtesy of A.Prof Frank Gaillard, Radiopaedia.org, rID: 6172]]] | |||
|} | |||
*It may show scalloped and [[Sclerosis|sclerotic]] rim | |||
*[[Calcification]] is usually not seen | |||
*The [[tumor]] may show [[Cortical bone|cortical expansion.]] | |||
===Echocardiography or Ultrasound=== | |||
There are no [[echocardiography]]/[[ultrasound]] findings associated with chondromyxoid fibroma. | |||
===CT scan=== | |||
*[[Computed tomography|CT scan]] confirms the [[X-rays|x-ray]] findings.<ref name="pmid27226218">{{cite journal| author=Cappelle S, Pans S, Sciot R| title=Imaging features of chondromyxoid fibroma: report of 15 cases and literature review. | journal=Br J Radiol | year= 2016 | volume= | issue= | pages= 20160088 | pmid=27226218 | doi=10.1259/bjr.20160088 | pmc=5124884 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27226218 }} </ref> | |||
*It is superior to [[X-rays|x-ray]] for analyzing the expansion of the [[lesion]] and [[Cortical bone|cortical]] breach. | |||
===MRI=== | |||
[[MRI]] findings of chondromyxoid fibroma include:<ref name="pmid21835889">{{cite journal| author=Kim HS, Jee WH, Ryu KN, Cho KH, Suh JS, Cho JH et al.| title=MRI of chondromyxoid fibroma. | journal=Acta Radiol | year= 2011 | volume= 52 | issue= 8 | pages= 875-80 | pmid=21835889 | doi=10.1258/ar.2011.110180 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21835889 }} </ref><ref>Campanacci M. Bone and soft tissue tumours. 2nd edn. Wien, Austria: Springer; 1999. pp. 265–71.</ref> | |||
{| align="right" | |||
| | |||
[[File:MRI CMF.gif|thumb|MRI of proximal ulna showing chondromyxoid fibroma.[https://radiopaedia.org/cases/chondromyxoid-fibroma-ulna?lang=us Source: Case courtesy of A.Prof Frank Gaillard, Radiopaedia.org, rID: 6172]]] | |||
|} | |||
*T1 image: Chondroid and myxoid [[Tissue (biology)|tissues]] produce low signals. | |||
*T2 image: Chondroid and myxoid [[tissues]] produce high signals. | |||
== | ===Other Imaging Findings=== | ||
===Bone Scan=== | |||
*Increased uptake is seen in chondromyxoid fibroma. | |||
===Other Diagnostic Studies=== | |||
There are no other [[Diagnosis|diagnostic]] studies associated with chondromyxoid fibroma. | |||
== | ==Treatment== | ||
===Medical Therapy=== | |||
There is no treatment for chondromyxoid fibroma; the mainstay of therapy is [[surgery]]. | |||
===Surgery=== | |||
[[Surgery]] is the mainstay of treatment for chondromyxoid fibroma.<ref name="pmid2793160">{{cite journal| author=Zillmer DA, Dorfman HD| title=Chondromyxoid fibroma of bone: thirty-six cases with clinicopathologic correlation. | journal=Hum Pathol | year= 1989 | volume= 20 | issue= 10 | pages= 952-64 | pmid=2793160 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2793160 }} </ref><ref name="pmid10653103">{{cite journal| author=Dürr HR, Lienemann A, Nerlich A, Stumpenhausen B, Refior HJ| title=Chondromyxoid fibroma of bone. | journal=Arch Orthop Trauma Surg | year= 2000 | volume= 120 | issue= 1-2 | pages= 42-7 | pmid=10653103 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10653103 }} </ref> | |||
'''Types''' | |||
== | '''1. Intralesional Curettage''' | ||
*It is the mainstay of treatment for chondromyxoid fibroma.<ref name="pmid10653103">{{cite journal| author=Dürr HR, Lienemann A, Nerlich A, Stumpenhausen B, Refior HJ| title=Chondromyxoid fibroma of bone. | journal=Arch Orthop Trauma Surg | year= 2000 | volume= 120 | issue= 1-2 | pages= 42-7 | pmid=10653103 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10653103 }} </ref> | |||
*The defect is filled with [[bone graft]] or [[bone cement]] in form of polymethlymethacrylate(PMMA). | |||
'''2. En Bloc Excision''' | |||
*It usually reserved for recurrent cases.<ref name="pmid29403178">{{cite journal| author=Dey B, Deshpande AH, Brar RK, Ray A| title=Chondromyxoid Fibroma of the Metatarsal Bone: A Diagnosis Using Fine Needle Aspiration Biopsy. | journal=J Cytol | year= 2018 | volume= 35 | issue= 1 | pages= 67-68 | pmid=29403178 | doi=10.4103/JOC.JOC_48_17 | pmc=5795736 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29403178 }} </ref> | |||
'''Recurrence Rate''' | |||
*The recurrence rate is about 25% for chondromyxoid fibroma.<ref name="pmid9596266">{{cite journal| author=Wu CT, Inwards CY, O'Laughlin S, Rock MG, Beabout JW, Unni KK| title=Chondromyxoid fibroma of bone: a clinicopathologic review of 278 cases. | journal=Hum Pathol | year= 1998 | volume= 29 | issue= 5 | pages= 438-46 | pmid=9596266 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9596266 }} </ref> | |||
== | ===Primary Prevention=== | ||
There are no established measures for the [[Prevention (medical)|primary prevention]] of chondromyxoid fibroma. | |||
===Secondary Prevention=== | |||
There are no established measures for the [[Prevention (medical)|secondary prevention]] of chondromyxoid fibroma. | |||
==References== | ==References== | ||
{{reflist | {{reflist|2}} | ||
{{WikiDoc Help Menu}} | |||
{{WikiDoc Sources}} | |||
Latest revision as of 16:35, 30 April 2019
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Rohan A. Bhimani, M.B.B.S., D.N.B., M.Ch.[2]
Synonyms and keywords:
Overview
Chondromyxoid fibroma is a rare benign bone tumor accounting for approximately 1% of all benign bone tumors. Chondromyxoid fibroma affects all age groups. It is more commonly seen during the second and third decades of life. Men are more commonly affected than women. Chondromyxoid fibroma arising from the physeal remnant is the commonly proposed theory in the pathogenesis of this tumor. It is predominantly found in the metaphyses of the long bones. The bones involved include tibia, distal femur, pelvis, feet and hands. Chromosome 6 appears to be involved in chondromyxoid fibroma. Over expression of the glutamate receptor gene GRM1 in patients with chondromyxoid fibroma via promoter swapping and gene fusion has been observed. The hallmark of chondromyxoid fibroma is pain, swelling, and pathological fracture. The mainstay of treatment for chondromyxoid fibroma is surgery (curettage and bone grafting).
Historical Perspective
In 1948, Jaffe and Lichtenstein described chondromyxoid fibroma for the first time.[1]
Classification
Chondromyxoid fibroma can be classified based on imaging findings.
Enneking (MSTS) Staging System
- The Enneking surgical staging system (also known as the MSTS system) for benign musculoskeletal tumors is based on radiographic characteristics of the tumor host margin.[2]
- It is widely accepted and routinely used classification.
| Stages | Description |
|---|---|
| 1 | Latent: Well demarcated borders |
| 2 | Active: Indistinct borders |
| 3 | Aggressive: Indistinct borders |
Pathophysiology
- The exact etiology of chondromyxoid fibroma is unknown.[3]
- Chondromyxoid fibroma arising from the physeal remnant is the commonly proposed theory in the pathogenesis of chondromyxoid fibroma.[4]
- It is predominantly found in the metaphyses of the long bones.[5]
- The bones involved by chondromyxoid fibroma includes tibia, distal femur, pelvis, feet and hands.[6]
Genetics
- Chromosome 6 appears to be involved in chondromyxoid fibroma.[5][7]
- The non-random clonal abnormalities involves 6p25, 6q13 and 6q23.[5]
- Whole-genome mate-pair sequencing and RNA sequencing showed over expression of the glutamate receptor gene GRM1 in patients with chondromyxoid fibroma via promoter swapping and gene fusion.[8]
Causes
There are no established causes of chondromyxoid fibroma.[9]
Differentiating Chondromyxoid Fibroma from Other Diseases
Chondromyxoid fibroma must be differentiated from the following bone disorders:[10]
| Disease | Bubbly lytic lesion on x-ray | Lakes of Blood on histology | Diagnosis | Treatment is curretage and bone grafting |
|---|---|---|---|---|
| Chondromyxoid Fibroma | - | - | Radiology and biopsy | + |
| Unicameral bone cyst | + | - | Radiology and biopsy | - |
| Non ossifying fibroma | + | - | Radiology and biopsy | - |
| Giant cell tumor | - | - | Radiology and Biopsy | + |
| Chondroblastoma | - | - | Biopsy | + |
| Aneurysmal bone cyst | + | + | Radiology and biopsy | + |
| Osteoblastoma | - | - | Radiology and biopsy | + |
| Telangiectatic osteosarcoma | - | + | Radiology and biopsy | - |
Epidemiology and Demographics
- Chondromyxoid fibroma is a rare benign bone tumor accounting for approximately 1% of all benign bone tumors.[11]
- Chondromyxoid fibroma affects all age groups.
- It is more commonly seen during the second and third decades of life.
- Men are more commonly affected than women.
- There is no racial predilection to chondromyxoid fibroma.
Risk Factors
There are no established risk factors for chondromyxoid fibroma.
Screening
There is insufficient evidence to recommend routine screening for chondromyxoid fibroma.
Natural History, Complications, and Prognosis
Common complications of chondromyxoid fibroma include:
- Pathological fracture
- Premature epiphyseal closure
- Limb-length discrepancy
- Angular deformity
Prognosis is generally good for chondromyxoid fibroma.
- Prognostic variables include:
Diagnosis
 |
Diagnostic Study of Choice
- Biopsy is the diagnostic study of choice for chondromyxoid fibroma.
- Biopsy findings under low and high power fields are given below:[12][13]
Under Low Power field:
- It has a biphasic appearance
- It has lobules and pseudolobules of fibromyxoid tissue with hypercellular area.
- The cells are spindle-shaped or stellate-shaped and contain hyperchromatic nuclei.
- Multinucleated giant cells and fibrovascular tissue may be present between the lobules.
- Hypocellular area with chondroid material is seen.
Under High Power Field:
- The tumor shows myxoid stroma mixed with stellate cells.
- In addition, an area of pleiomorphic cells with bizarre nuclei may be seen.
History and Symptoms
- The majority of patients with chondromyxoid fibroma have a positive history of:
 |
Physical Examination
Common physical examination findings of chondromyxoid fibroma include:
- Swelling
- Decreased range of motion
- Warmth over the affected area
Laboratory Findings
There are no diagnostic laboratory findings associated with chondromyxoid fibroma.
Electrocardiogram
There are no ECG findings associated with chondromyxoid fibroma.
X-ray
X-ray findings include:[14][15]
- Size of the lesion may vary from 2 to 10 cm.
- It has a sharply demarcated border from the adjacent bone.
 |
- It may show scalloped and sclerotic rim
- Calcification is usually not seen
- The tumor may show cortical expansion.
Echocardiography or Ultrasound
There are no echocardiography/ultrasound findings associated with chondromyxoid fibroma.
CT scan
- CT scan confirms the x-ray findings.[16]
- It is superior to x-ray for analyzing the expansion of the lesion and cortical breach.
MRI
MRI findings of chondromyxoid fibroma include:[17][18]
 |
- T1 image: Chondroid and myxoid tissues produce low signals.
- T2 image: Chondroid and myxoid tissues produce high signals.
Other Imaging Findings
Bone Scan
- Increased uptake is seen in chondromyxoid fibroma.
Other Diagnostic Studies
There are no other diagnostic studies associated with chondromyxoid fibroma.
Treatment
Medical Therapy
There is no treatment for chondromyxoid fibroma; the mainstay of therapy is surgery.
Surgery
Surgery is the mainstay of treatment for chondromyxoid fibroma.[19][20]
Types
1. Intralesional Curettage
- It is the mainstay of treatment for chondromyxoid fibroma.[20]
- The defect is filled with bone graft or bone cement in form of polymethlymethacrylate(PMMA).
2. En Bloc Excision
- It usually reserved for recurrent cases.[21]
Recurrence Rate
- The recurrence rate is about 25% for chondromyxoid fibroma.[22]
Primary Prevention
There are no established measures for the primary prevention of chondromyxoid fibroma.
Secondary Prevention
There are no established measures for the secondary prevention of chondromyxoid fibroma.
References
- ↑ JAFFE HL, LICHTENSTEIN L (1948). "Chondromyxoid fibroma of bone; a distinctive benign tumor likely to be mistaken especially for chondrosarcoma". Arch Pathol (Chic). 45 (4): 541–51. PMID 18891025.
- ↑ Jawad MU, Scully SP (2010). "In brief: classifications in brief: enneking classification: benign and malignant tumors of the musculoskeletal system". Clin Orthop Relat Res. 468 (7): 2000–2. doi:10.1007/s11999-010-1315-7. PMC 2882012. PMID 20333492.
- ↑ Peabody, Terrance (2014). Orthopaedic oncology : primary and metastatic tumors of the skeletal system. Cham: Springer. ISBN 9783319073224.
- ↑ Brien EW, Mirra JM, Kerr R (1997). "Benign and malignant cartilage tumors of bone and joint: their anatomic and theoretical basis with an emphasis on radiology, pathology and clinical biology. I. The intramedullary cartilage tumors". Skeletal Radiol. 26 (6): 325–53. PMID 9229417.
- ↑ 5.0 5.1 5.2 Cuvelier CA, Roels HJ (1979). "Cytophotometric studies of the nuclear DNA content in cartilaginous tumors". Cancer. 44 (4): 1363–74. PMID 498016.
- ↑ Halbert AR, Harrison WR, Hicks MJ, Davino N, Cooley LD (1998). "Cytogenetic analysis of a scapular chondromyxoid fibroma". Cancer Genet Cytogenet. 104 (1): 52–6. PMID 9648559.
- ↑ Buddingh EP, Naumann S, Nelson M, Neffa JR, Birch N, Bridge JA (2003). "Cytogenetic findings in benign cartilaginous neoplasms". Cancer Genet Cytogenet. 141 (2): 164–8. PMID 12606137.
- ↑ Nord KH, Lilljebjörn H, Vezzi F, Nilsson J, Magnusson L, Tayebwa J; et al. (2014). "GRM1 is upregulated through gene fusion and promoter swapping in chondromyxoid fibroma". Nat Genet. 46 (5): 474–7. doi:10.1038/ng.2927. PMID 24658000.
- ↑ Gherlinzoni F, Rock M, Picci P (1983). "Chondromyxoid fibroma. The experience at the Istituto Ortopedico Rizzoli". J Bone Joint Surg Am. 65 (2): 198–204. PMID 6337162.
- ↑ Bergman S, Madden CR, Geisinger KR (2009). "Fine-needle aspiration biopsy of chondromyxoid fibroma: an investigation of four cases". Am J Clin Pathol. 132 (5): 740–5. doi:10.1309/AJCPFJZ8AKMFUAFP. PMID 19846816.
- ↑ Pintor F, Bahamondes C, Campos O, Zivov A (2015). "Chondromyxoid fibroma of zygoma in an elderly patient: A rare presentation". Ann Maxillofac Surg. 5 (2): 244–8. doi:10.4103/2231-0746.175755. PMC 4772571. PMID 26981481.
- ↑ Tallini G, Dorfman H, Brys P, Dal Cin P, De Wever I, Fletcher CD; et al. (2002). "Correlation between clinicopathological features and karyotype in 100 cartilaginous and chordoid tumours. A report from the Chromosomes and Morphology (CHAMP) Collaborative Study Group". J Pathol. 196 (2): 194–203. doi:10.1002/path.1023. PMID 11793371.
- ↑ Desai SS, Jambhekar NA, Samanthray S, Merchant NH, Puri A, Agarwal M (2005). "Chondromyxoid fibromas: a study of 10 cases". J Surg Oncol. 89 (1): 28–31. doi:10.1002/jso.20113. PMID 15612014.
- ↑ Marin C, Gallego C, Manjón P, Martinez-Tello FJ (1997). "Juxtacortical chondromyxoid fibroma: imaging findings in three cases and a review of the literature". Skeletal Radiol. 26 (11): 642–9. PMID 9428071.
- ↑ Merine D, Fishman EK, Rosengard A, Tolo V (1989). "Chondromyxoid fibroma of the fibula". J Pediatr Orthop. 9 (4): 468–71. PMID 2732329.
- ↑ Cappelle S, Pans S, Sciot R (2016). "Imaging features of chondromyxoid fibroma: report of 15 cases and literature review". Br J Radiol: 20160088. doi:10.1259/bjr.20160088. PMC 5124884. PMID 27226218.
- ↑ Kim HS, Jee WH, Ryu KN, Cho KH, Suh JS, Cho JH; et al. (2011). "MRI of chondromyxoid fibroma". Acta Radiol. 52 (8): 875–80. doi:10.1258/ar.2011.110180. PMID 21835889.
- ↑ Campanacci M. Bone and soft tissue tumours. 2nd edn. Wien, Austria: Springer; 1999. pp. 265–71.
- ↑ Zillmer DA, Dorfman HD (1989). "Chondromyxoid fibroma of bone: thirty-six cases with clinicopathologic correlation". Hum Pathol. 20 (10): 952–64. PMID 2793160.
- ↑ 20.0 20.1 Dürr HR, Lienemann A, Nerlich A, Stumpenhausen B, Refior HJ (2000). "Chondromyxoid fibroma of bone". Arch Orthop Trauma Surg. 120 (1–2): 42–7. PMID 10653103.
- ↑ Dey B, Deshpande AH, Brar RK, Ray A (2018). "Chondromyxoid Fibroma of the Metatarsal Bone: A Diagnosis Using Fine Needle Aspiration Biopsy". J Cytol. 35 (1): 67–68. doi:10.4103/JOC.JOC_48_17. PMC 5795736. PMID 29403178.
- ↑ Wu CT, Inwards CY, O'Laughlin S, Rock MG, Beabout JW, Unni KK (1998). "Chondromyxoid fibroma of bone: a clinicopathologic review of 278 cases". Hum Pathol. 29 (5): 438–46. PMID 9596266.