Systemic lupus erythematosus electrocardiogram: Difference between revisions
No edit summary |
|||
| (7 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Systemic lupus erythematosus}} | {{Systemic lupus erythematosus}} | ||
{{CMG}} | {{CMG}} {{AE}} {{MIR}} | ||
==Overview== | ==Overview== | ||
| Line 7: | Line 7: | ||
==Electrocardiogram== | ==Electrocardiogram== | ||
The most common and important [[ECG]] findings associated with systemic lupus erythematosus (SLE) include [[sinus tachycardia]], [[ST segment changes]], and [[Ventricular arrhythmias|ventricular conduction disturbances]]. SLE can affect [[cardiopulmonary]] system in different ways including [[Pulmonary embolism|pulmonary emboli development]], [[Libman-Sacks disease|Libman sacks endocarditis]], and conduction problems. <ref name="pmid24838943">{{cite journal |vauthors=Bourré-Tessier J, Urowitz MB, Clarke AE, Bernatsky S, Krantz MJ, Huynh T, Joseph L, Belisle P, Bae SC, Hanly JG, Wallace DJ, Gordon C, Isenberg D, Rahman A, Gladman DD, Fortin PR, Merrill JT, Romero-Diaz J, Sanchez-Guerrero J, Fessler B, Alarcón GS, Steinsson K, Bruce IN, Ginzler E, Dooley MA, Nived O, Sturfelt G, Kalunian K, Ramos-Casals M, Petri M, Zoma A, Pineau CA |title=Electrocardiographic findings in systemic lupus erythematosus: data from an international inception cohort |journal=Arthritis Care Res (Hoboken) |volume=67 |issue=1 |pages=128–35 |year=2015 |pmid=24838943 |doi=10.1002/acr.22370 |url=}}</ref><ref name="pmid8331790">{{cite journal |vauthors=Tsunakawa H, Miyamoto N, Kawabata M, Mashima S |title=[Electrocardiogram in heart failure] |language=Japanese |journal=Nippon Rinsho |volume=51 |issue=5 |pages=1222–32 |year=1993 |pmid=8331790 |doi= |url=}}</ref><ref name="pmid20435842">{{cite journal| author=Maganti K, Rigolin VH, Sarano ME, Bonow RO| title=Valvular heart disease: diagnosis and management. | journal=Mayo Clin Proc | year= 2010 | volume= 85 | issue= 5 | pages= 483-500 | pmid=20435842 | doi=10.4065/mcp.2009.0706 | pmc=2861980 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20435842 }}</ref><ref name="pmid14916061">{{cite journal| author=TROUNCE JR| title=The electrocardiogram in mitral stenosis. | journal=Br Heart J | year= 1952 | volume= 14 | issue= 2 | pages= 185-92 | pmid=14916061 | doi= | pmc=479442 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14916061 }}</ref><ref name="pmid7849377">{{cite journal |vauthors=Nakashima H, Honda Y, Katayama T |title=Serial electrocardiographic findings in acute myocarditis |journal=Intern. Med. |volume=33 |issue=11 |pages=659–66 |year=1994 |pmid=7849377 |doi= |url=}}</ref><ref name="pmid110701052">{{cite journal| author=Feldman AM, McNamara D|title=Myocarditis. | journal=N Engl J Med | year= 2000 | volume= 343 | issue= 19 | pages= 1388-98 | pmid=11070105 |doi=10.1056/NEJM200011093431908 | pmc= | url= }}</ref><ref name="troughton">{{cite journal | author= Troughton RW, Asher CR, Klein AL | title= Pericarditis | journal= Lancet| year=2004| pages=717–27 | volume=363 | issue=9410 | pmid=15001332 | doi= 10.1016/S0140-6736(04)15648-1}}</ref><ref name="spodick">{{cite journal | author= Spodick DH | title= Acute pericarditis: current concepts and practice | journal= JAMA | year=2003 | pages=1150–3 | volume=289 | issue=9 | pmid=12622586 | doi= 10.1001/jama.289.9.1150}}</ref> | The most common and important [[ECG]] findings associated with systemic lupus erythematosus (SLE) include [[sinus tachycardia]], [[ST segment changes]], and [[Ventricular arrhythmias|ventricular conduction disturbances]]. SLE can affect [[cardiopulmonary]] system in different ways including [[Pulmonary embolism|pulmonary emboli development]], [[Libman-Sacks disease|Libman sacks endocarditis]], and conduction problems.<ref name="pmid24838943">{{cite journal |vauthors=Bourré-Tessier J, Urowitz MB, Clarke AE, Bernatsky S, Krantz MJ, Huynh T, Joseph L, Belisle P, Bae SC, Hanly JG, Wallace DJ, Gordon C, Isenberg D, Rahman A, Gladman DD, Fortin PR, Merrill JT, Romero-Diaz J, Sanchez-Guerrero J, Fessler B, Alarcón GS, Steinsson K, Bruce IN, Ginzler E, Dooley MA, Nived O, Sturfelt G, Kalunian K, Ramos-Casals M, Petri M, Zoma A, Pineau CA |title=Electrocardiographic findings in systemic lupus erythematosus: data from an international inception cohort |journal=Arthritis Care Res (Hoboken) |volume=67 |issue=1 |pages=128–35 |year=2015 |pmid=24838943 |doi=10.1002/acr.22370 |url=}}</ref><ref name="pmid8331790">{{cite journal |vauthors=Tsunakawa H, Miyamoto N, Kawabata M, Mashima S |title=[Electrocardiogram in heart failure] |language=Japanese |journal=Nippon Rinsho |volume=51 |issue=5 |pages=1222–32 |year=1993 |pmid=8331790 |doi= |url=}}</ref><ref name="pmid20435842">{{cite journal| author=Maganti K, Rigolin VH, Sarano ME, Bonow RO| title=Valvular heart disease: diagnosis and management. | journal=Mayo Clin Proc | year= 2010 | volume= 85 | issue= 5 | pages= 483-500 | pmid=20435842 | doi=10.4065/mcp.2009.0706 | pmc=2861980 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20435842 }}</ref><ref name="pmid14916061">{{cite journal| author=TROUNCE JR| title=The electrocardiogram in mitral stenosis. | journal=Br Heart J | year= 1952 | volume= 14 | issue= 2 | pages= 185-92 | pmid=14916061 | doi= | pmc=479442 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14916061 }}</ref><ref name="pmid7849377">{{cite journal |vauthors=Nakashima H, Honda Y, Katayama T |title=Serial electrocardiographic findings in acute myocarditis |journal=Intern. Med. |volume=33 |issue=11 |pages=659–66 |year=1994 |pmid=7849377 |doi= |url=}}</ref><ref name="pmid110701052">{{cite journal| author=Feldman AM, McNamara D|title=Myocarditis. | journal=N Engl J Med | year= 2000 | volume= 343 | issue= 19 | pages= 1388-98 | pmid=11070105 |doi=10.1056/NEJM200011093431908 | pmc= | url= }}</ref><ref name="troughton">{{cite journal | author= Troughton RW, Asher CR, Klein AL | title= Pericarditis | journal= Lancet| year=2004| pages=717–27 | volume=363 | issue=9410 | pmid=15001332 | doi= 10.1016/S0140-6736(04)15648-1}}</ref><ref name="spodick">{{cite journal | author= Spodick DH | title= Acute pericarditis: current concepts and practice | journal= JAMA | year=2003 | pages=1150–3 | volume=289 | issue=9 | pmid=12622586 | doi= 10.1001/jama.289.9.1150}}</ref> | ||
=== Important ECG findings in SLE patients based on cardiac complication: === | === Important ECG findings in SLE patients based on cardiac complication: === | ||
| Line 13: | Line 13: | ||
| colspan="2" align="center" style="background: #4479BA; color: #FFFFFF; " |Cardiac complication | | colspan="2" align="center" style="background: #4479BA; color: #FFFFFF; " |Cardiac complication | ||
| align="center" style="background: #4479BA; color: #FFFFFF; " |ECG findings | | align="center" style="background: #4479BA; color: #FFFFFF; " |ECG findings | ||
| align="center" style="background: #4479BA; color: #FFFFFF; " |ECG examples | |||
|- | |- | ||
| colspan="2" style="background: #DCDCDC; " |[[Cardiomegaly]] | | colspan="2" style="background: #DCDCDC; " |[[Cardiomegaly]] | ||
| Line 20: | Line 21: | ||
* [[Left Atrial Enlargement|Left atrial enlargement]] | * [[Left Atrial Enlargement|Left atrial enlargement]] | ||
* [[Left axis deviation]] | * [[Left axis deviation]] | ||
|[[File:LA.gif|200px|thumb|'''http://ecg.utah.edu/img_index''' Courtesy dedicated to ecg.utah.edu]] | |||
|- | |- | ||
| rowspan="2" style="background: #DCDCDC; " |[[Libman-Sacks endocarditis|Libman sacks endocarditis]] | | rowspan="2" style="background: #DCDCDC; " |[[Libman-Sacks endocarditis|Libman sacks endocarditis]] | ||
| Line 28: | Line 30: | ||
** Primary increase | ** Primary increase | ||
** Decrease after progression | ** Decrease after progression | ||
|[[File:Jjj.gif|200px|thumb|'''http://ecg.utah.edu/img_index''' Courtesy dedicated to ecg.utah.edu]] | |||
|- | |- | ||
| style="background: #DCDCDC; " |[[Myocardial infarction]] | | style="background: #DCDCDC; " |[[Myocardial infarction]] | ||
| Line 36: | Line 39: | ||
**[[ST depression]] in several leads plus [[ST elevation]] in lead aVR (suggestive of occlusion of the left main or proximal [[LAD artery]]) | **[[ST depression]] in several leads plus [[ST elevation]] in lead aVR (suggestive of occlusion of the left main or proximal [[LAD artery]]) | ||
**New [[left bundle branch block]] ([[LBBB]]) | **New [[left bundle branch block]] ([[LBBB]]) | ||
|[[File:84 Acute inf STEMI.jpg|200px|thumb|'''http://ecg.utah.edu/img_index''' Courtesy dedicated to ecg.utah.edu]] | |||
|- | |- | ||
| rowspan="2" style="background: #DCDCDC; " |[[Valvular Diseases|Valvular involvement]] | | rowspan="2" style="background: #DCDCDC; " |[[Valvular Diseases|Valvular involvement]] | ||
| Line 41: | Line 45: | ||
| | | | ||
* [[ECG]] findings suggestive of [[left atrial enlargement]] include: | * [[ECG]] findings suggestive of [[left atrial enlargement]] include: | ||
**Broad | **Broad and biphasic [[P wave]] in lead II ([[P mitrale]]) | ||
**Enlargement of the terminal negative portion of the [[P wave]] in VI | **Enlargement of the terminal negative portion of the [[P wave]] in VI | ||
**[[P wave]] amplitude >2.5 mm in inferior leads (II, III, AVF) or >1.5 mm in V1/V2 ([[P pulmonale]]) | **[[P wave]] amplitude >2.5 mm in inferior leads (II, III, AVF) or >1.5 mm in V1/V2 ([[P pulmonale]]) | ||
|[[File:LA.gif|200px|thumb|'''http://ecg.utah.edu/img_index''' Courtesy dedicated to ecg.utah.edu]] | |||
|- | |- | ||
| style="background: #DCDCDC; " |[[Mitral regurgitation]] | | style="background: #DCDCDC; " |[[Mitral regurgitation]] | ||
| | | | ||
* [[ECG]] findings suggestive of [[left atrial enlargement]] include: | * [[ECG]] findings suggestive of [[left atrial enlargement]] include: | ||
**Broad | **Broad and biphasic [[P wave]] in lead II [[P mitrale|(P mitrale)]] | ||
**Enlargement of the terminal negative portion of the [[P wave]] in V1 | **Enlargement of the terminal negative portion of the [[P wave]] in V1 | ||
**[[P wave]] amplitude >2.5 mm in inferior leads (II, III, AVF) or >1.5 mm in V1/V2 (P pulmonale) | **[[P wave]] amplitude >2.5 mm in inferior leads (II, III, AVF) or >1.5 mm in V1/V2 (P pulmonale) | ||
| Line 55: | Line 60: | ||
**Strain pattern | **Strain pattern | ||
**Inverted check mark pattern to the [[T wave]] in the lateral leads | **Inverted check mark pattern to the [[T wave]] in the lateral leads | ||
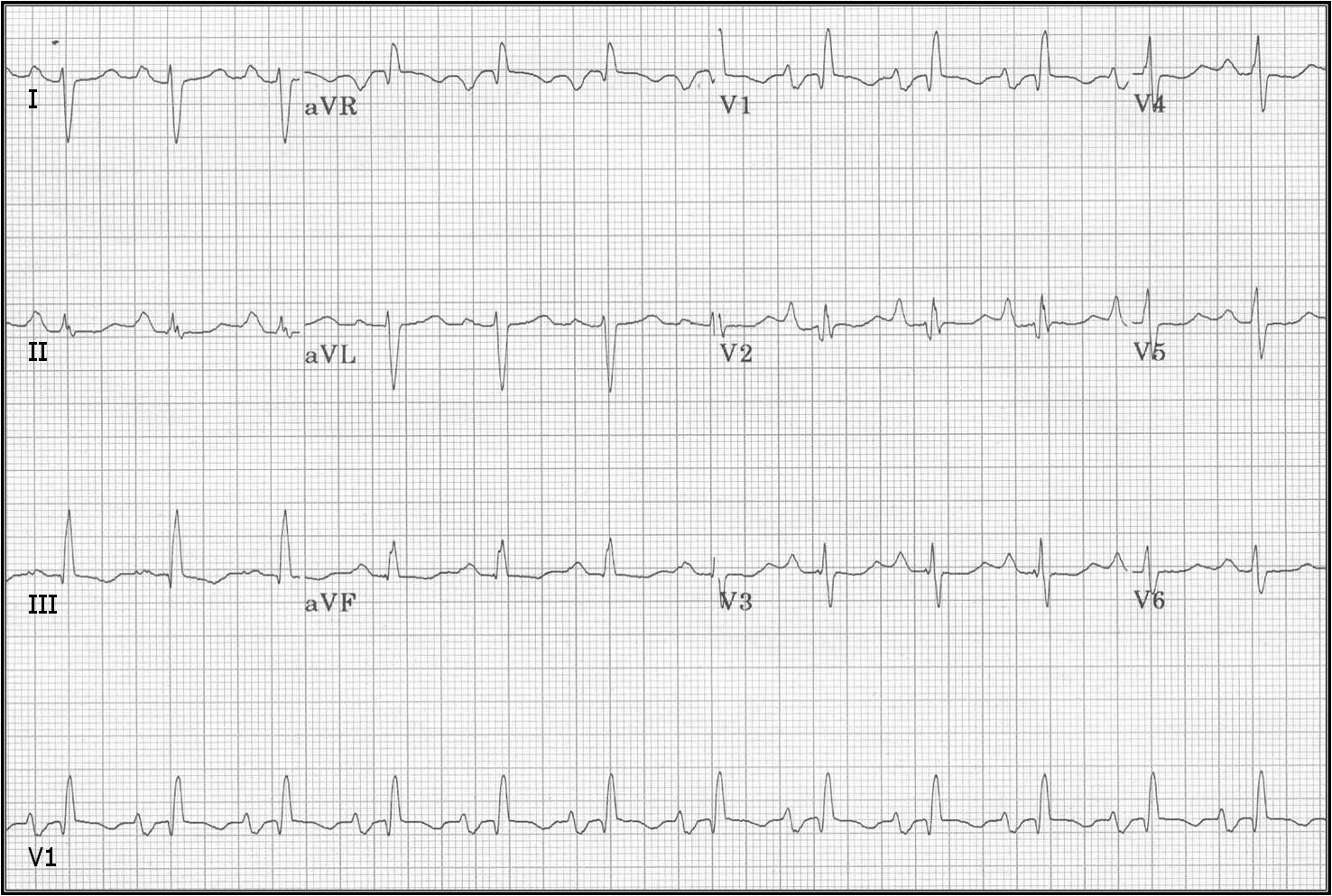
|[[File:80 RVH and LAE in mitral stenosis.jpg|200px|thumb|'''http://ecg.utah.edu/img_index''' Courtesy dedicated to ecg.utah.edu]] | |||
|- | |- | ||
| rowspan="2" style="background: #DCDCDC; " |[[Arrythmias|Arrhythmias]] | | rowspan="2" style="background: #DCDCDC; " |[[Arrythmias|Arrhythmias]] | ||
| style="background: #DCDCDC; " |[[ | | style="background: #DCDCDC; " |[[Atrioventricular block|AV Blocks]] | ||
| | | | ||
* Incomplete [[bundle branch block]] | * Incomplete [[bundle branch block]] | ||
| Line 64: | Line 70: | ||
* [[Left anterior fascicular block]] | * [[Left anterior fascicular block]] | ||
* [[Left posterior fascicular block]] | * [[Left posterior fascicular block]] | ||
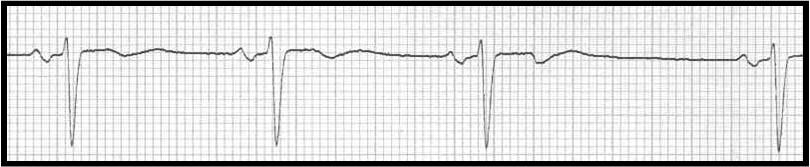
|[[File:Ggddh.gif|200px|thumb|'''http://ecg.utah.edu/img_index''' Courtesy dedicated to ecg.utah.edu]]<br> | |||
[[File:80 RVH and LAcxE in mitral stenosis.jpg|200px|thumb|'''http://ecg.utah.edu/img_index''' Courtesy dedicated to ecg.utah.edu]] | |||
|- | |- | ||
| style="background: #DCDCDC; " |[[Supraventricular arrhythmias]] | | style="background: #DCDCDC; " |[[Supraventricular arrhythmias]] | ||
| Line 70: | Line 78: | ||
* [[Atrial fibrillation]] | * [[Atrial fibrillation]] | ||
* [[Atrial flutter]] | * [[Atrial flutter]] | ||
|[[File:Pac.jpg|200px|thumb|'''http://ecg.utah.edu/img_index''' Courtesy dedicated to ecg.utah.edu]] | |||
|- | |- | ||
| rowspan="2" style="background: #DCDCDC; " |[[Pericardial disease]] | | rowspan="2" style="background: #DCDCDC; " |[[Pericardial disease]] | ||
| Line 81: | Line 90: | ||
*Reduced voltage with quasi-specific ST-T waves due to increase in [[scar tissue]], fluid and [[fibrin]] | *Reduced voltage with quasi-specific ST-T waves due to increase in [[scar tissue]], fluid and [[fibrin]] | ||
*The [[EKG]] abnormalities vary depending on the stage/severity of the [[pericarditis]] | *The [[EKG]] abnormalities vary depending on the stage/severity of the [[pericarditis]] | ||
|[[File:Ecg 12lead006z.gif|200px|thumb|'''http://ecg.utah.edu/img_index''' Courtesy dedicated to ecg.utah.edu]] | |||
|- | |- | ||
| style="background: #DCDCDC; " |[[Pericardial effusion]] | | style="background: #DCDCDC; " |[[Pericardial effusion]] | ||
| Line 86: | Line 96: | ||
* [[Electrical alternans]] | * [[Electrical alternans]] | ||
** An [[Electrocardiogram|electrocardiographic]] phenomenon of alternation of [[QRS complex]] amplitude or [[axis]] between beats | ** An [[Electrocardiogram|electrocardiographic]] phenomenon of alternation of [[QRS complex]] amplitude or [[axis]] between beats | ||
|[[File:Electrical Alternans.jpg|200px|thumb|'''https://en.wikipedia.org/wiki/Pericardial_effusion''' Courtesy dedicated to wikipedia]] | |||
|- | |- | ||
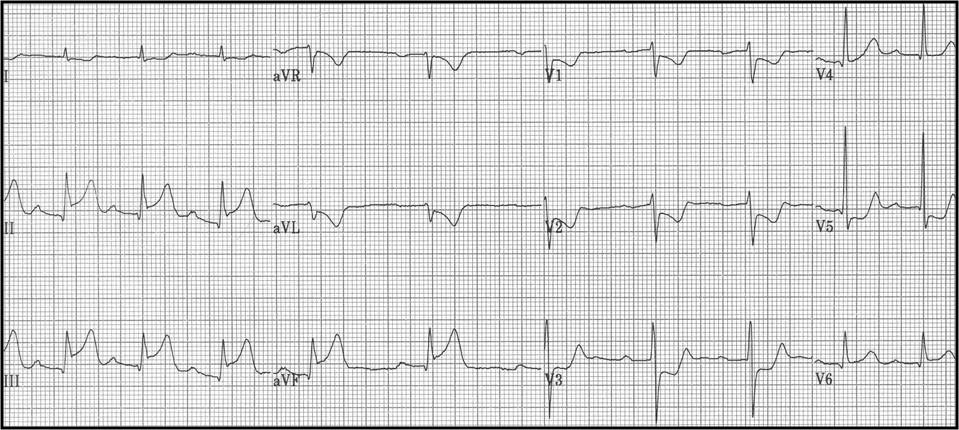
| colspan="2" style="background: #DCDCDC; " |[[Myocarditis]] | | colspan="2" style="background: #DCDCDC; " |[[Myocarditis]] | ||
| | | | ||
The [[Electrocardiogram|ECG]] findings most commonly seen in [[myocarditis]] are: | The [[Electrocardiogram|ECG]] findings most commonly seen in [[myocarditis]] are: | ||
| Line 96: | Line 106: | ||
*Low voltage of the [[QRS]] complexes | *Low voltage of the [[QRS]] complexes | ||
*[[Arrhythmias]] such as [[atrial]] or [[ventricular]] ectopic beats, [[atrial]] or [[Ventricular Tachycardia|ventricular tachycardias]], and [[atrial fibrillation]] | *[[Arrhythmias]] such as [[atrial]] or [[ventricular]] ectopic beats, [[atrial]] or [[Ventricular Tachycardia|ventricular tachycardias]], and [[atrial fibrillation]] | ||
|[[File:PericarditisMyocarditis.jpg|200px|thumb|'''https://en.wikipedia.org/wiki/Myocarditis''' Courtesy dedicated to wikipedia]] | |||
|- | |- | ||
| colspan="2" style="background: #DCDCDC; " |[[Coronary heart disease|Coronary artery disease]] | | colspan="2" style="background: #DCDCDC; " |[[Coronary heart disease|Coronary artery disease]] | ||
| Line 103: | Line 114: | ||
** Exercise induced [[ventricular arrhythmia]] | ** Exercise induced [[ventricular arrhythmia]] | ||
** [[Hemodynamics|Hemodynamic]] changes during the test | ** [[Hemodynamics|Hemodynamic]] changes during the test | ||
|[[File:Jkhhk.jpg|200px|thumb|'''http://ecg.utah.edu/img_index''' Courtesy dedicated to ecg.utah.edu]] | |||
|} | |} | ||
Latest revision as of 16:23, 1 February 2018
|
Systemic lupus erythematosus Microchapters |
|
Differentiating Systemic lupus erythematosus from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Systemic lupus erythematosus electrocardiogram On the Web |
|
American Roentgen Ray Society Images of Systemic lupus erythematosus electrocardiogram |
|
Directions to Hospitals Treating Systemic lupus erythematosus |
|
Risk calculators and risk factors for Systemic lupus erythematosus electrocardiogram |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Mahshid Mir, M.D. [2]
Overview
The most common and important ECG findings associated with systemic lupus erythematosus (SLE) include sinus tachycardia, ST segment changes, and ventricular conduction disturbances. Other ECG findings are related to late complications of SLE and may range based on the complication.
Electrocardiogram
The most common and important ECG findings associated with systemic lupus erythematosus (SLE) include sinus tachycardia, ST segment changes, and ventricular conduction disturbances. SLE can affect cardiopulmonary system in different ways including pulmonary emboli development, Libman sacks endocarditis, and conduction problems.[1][2][3][4][5][6][7][8]
Important ECG findings in SLE patients based on cardiac complication:
| Cardiac complication | ECG findings | ECG examples | |
| Cardiomegaly |
|
 | |
| Libman sacks endocarditis | Heart failure |  | |
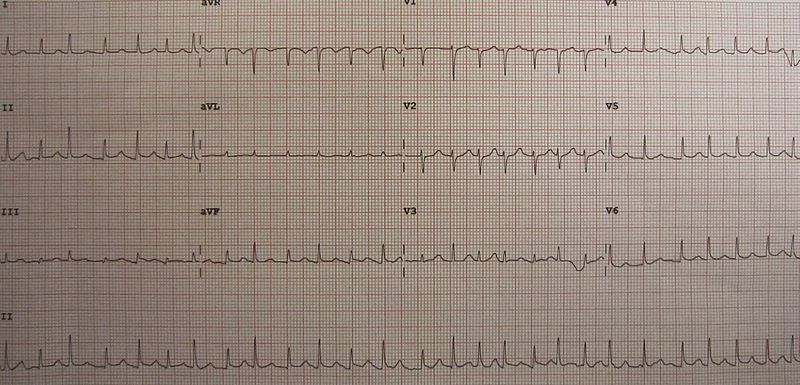
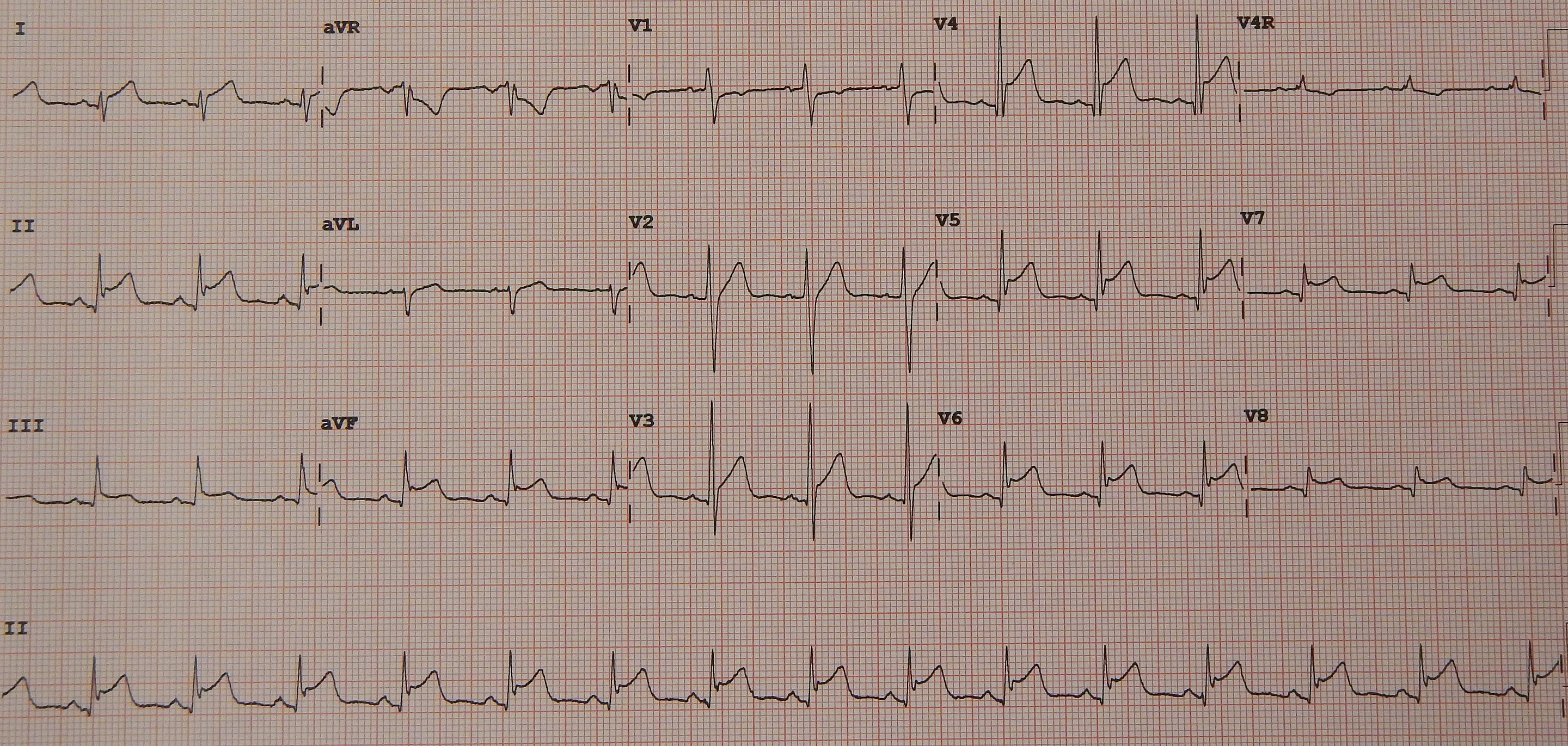
| Myocardial infarction |
|
 | |
| Valvular involvement | Mitral valve stenosis |
|
 |
| Mitral regurgitation |
|
 | |
| Arrhythmias | AV Blocks |  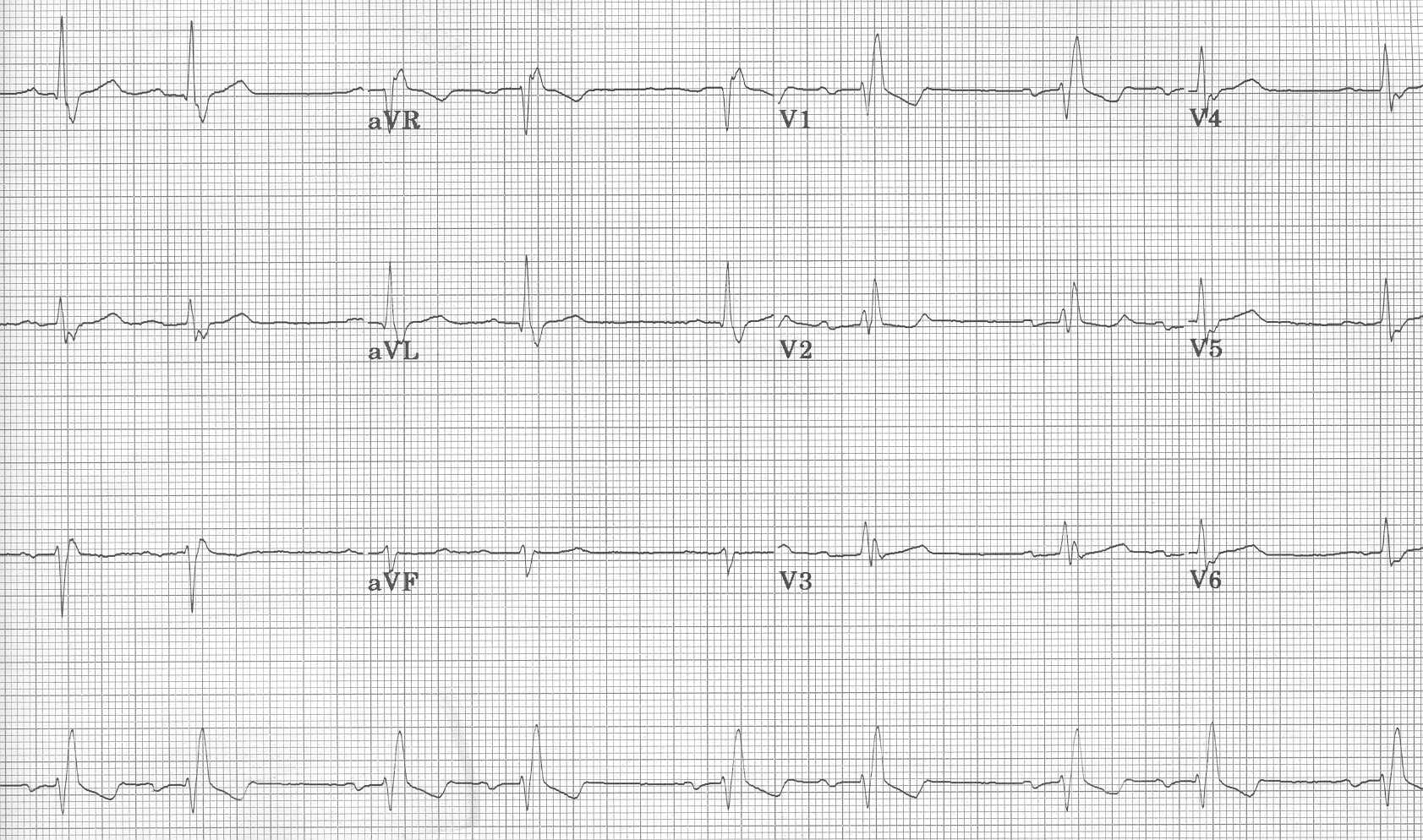 | |
| Supraventricular arrhythmias | |||
| Pericardial disease | Acute pericarditis |
|
 |
| Pericardial effusion |
|
 | |
| Myocarditis |
The ECG findings most commonly seen in myocarditis are:
|
 | |
| Coronary artery disease |
|
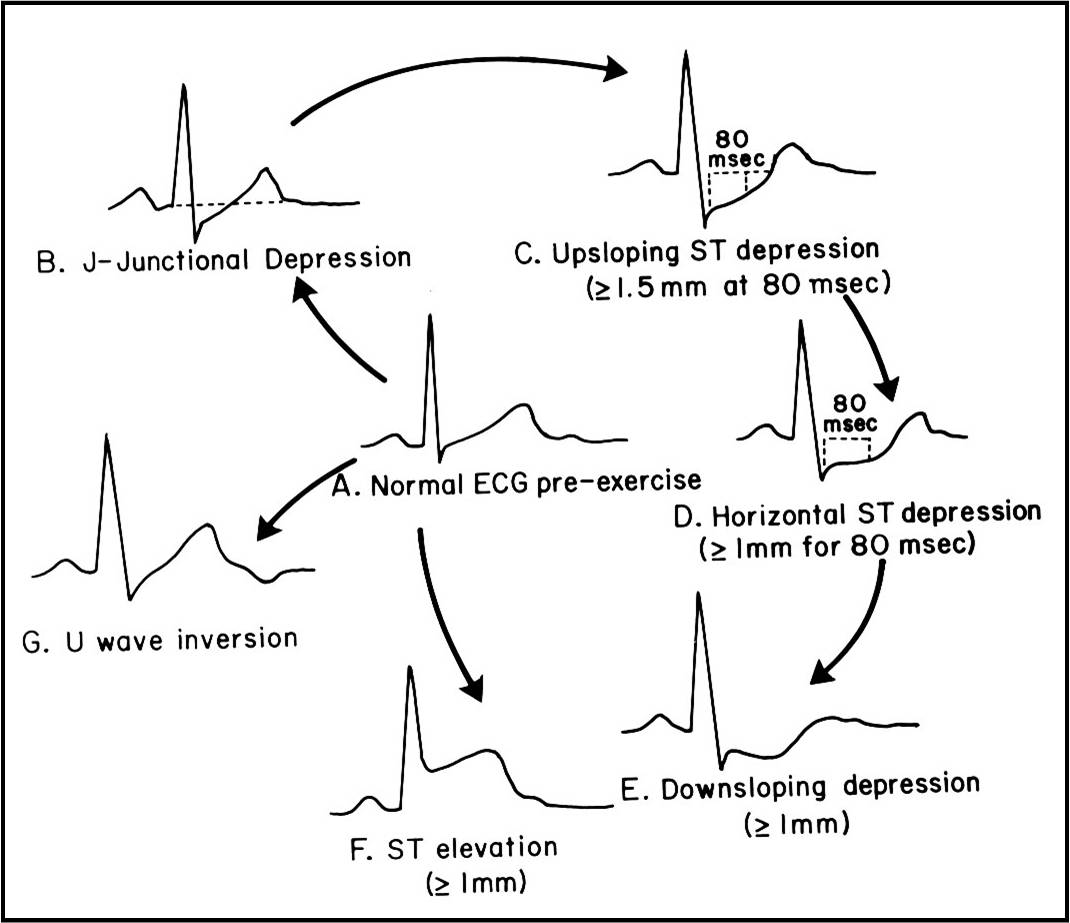 | |
References
- ↑ Bourré-Tessier J, Urowitz MB, Clarke AE, Bernatsky S, Krantz MJ, Huynh T, Joseph L, Belisle P, Bae SC, Hanly JG, Wallace DJ, Gordon C, Isenberg D, Rahman A, Gladman DD, Fortin PR, Merrill JT, Romero-Diaz J, Sanchez-Guerrero J, Fessler B, Alarcón GS, Steinsson K, Bruce IN, Ginzler E, Dooley MA, Nived O, Sturfelt G, Kalunian K, Ramos-Casals M, Petri M, Zoma A, Pineau CA (2015). "Electrocardiographic findings in systemic lupus erythematosus: data from an international inception cohort". Arthritis Care Res (Hoboken). 67 (1): 128–35. doi:10.1002/acr.22370. PMID 24838943.
- ↑ Tsunakawa H, Miyamoto N, Kawabata M, Mashima S (1993). "[Electrocardiogram in heart failure]". Nippon Rinsho (in Japanese). 51 (5): 1222–32. PMID 8331790.
- ↑ Maganti K, Rigolin VH, Sarano ME, Bonow RO (2010). "Valvular heart disease: diagnosis and management". Mayo Clin Proc. 85 (5): 483–500. doi:10.4065/mcp.2009.0706. PMC 2861980. PMID 20435842.
- ↑ TROUNCE JR (1952). "The electrocardiogram in mitral stenosis". Br Heart J. 14 (2): 185–92. PMC 479442. PMID 14916061.
- ↑ Nakashima H, Honda Y, Katayama T (1994). "Serial electrocardiographic findings in acute myocarditis". Intern. Med. 33 (11): 659–66. PMID 7849377.
- ↑ Feldman AM, McNamara D (2000). "Myocarditis". N Engl J Med. 343 (19): 1388–98. doi:10.1056/NEJM200011093431908. PMID 11070105.
- ↑ Troughton RW, Asher CR, Klein AL (2004). "Pericarditis". Lancet. 363 (9410): 717–27. doi:10.1016/S0140-6736(04)15648-1. PMID 15001332.
- ↑ Spodick DH (2003). "Acute pericarditis: current concepts and practice". JAMA. 289 (9): 1150–3. doi:10.1001/jama.289.9.1150. PMID 12622586.