Flucytosine: Difference between revisions
Adeel Jamil (talk | contribs) No edit summary |
m Protected "Flucytosine": Bot: Protecting all pages from category Drug ([Edit=Allow only administrators] (indefinite) [Move=Allow only administrators] (indefinite)) |
||
| (2 intermediate revisions by one other user not shown) | |||
| Line 5: | Line 5: | ||
|drugClass=antifungal , anti-Infective agent | |drugClass=antifungal , anti-Infective agent | ||
|indicationType=treatment | |indicationType=treatment | ||
|indication=[[candidiasis]] and [[cryptococcosis]] | |indication=[[candidiasis]] and [[cryptococcosis]] | ||
|hasBlackBoxWarning=Yes | |hasBlackBoxWarning=Yes | ||
|adverseReactions=[[abdominal pain]], [[diarrhea]], [[nausea]], [[vomiting]], [[confusion]], [[headache]] and [[hallucinations]] | |adverseReactions=[[abdominal pain]], [[diarrhea]], [[nausea]], [[vomiting]], [[confusion]], [[headache]] and [[hallucinations]] | ||
| Line 12: | Line 12: | ||
<!--FDA-Labeled Indications and Dosage (Adult)--> | <!--FDA-Labeled Indications and Dosage (Adult)--> | ||
|fdaLIADAdult=* Ancobon is indicated only in the treatment of serious | |fdaLIADAdult=* Ancobon is indicated only in the treatment of serious [[infection]]s caused by susceptible strains of [[Candida]] and/or [[Cryptococcus]]. | ||
* Candida: Septicemia, endocarditis and urinary system | * [[Candida]]: [[Septicemia]], [[endocarditis]] and [[urinary system]] [[infection]]s have been effectively treated with flucytosine. Limited trials in [[pulmonary infection]]s justify the use of flucytosine. | ||
* Cryptococcus: Meningitis and pulmonary infections have been treated effectively. Studies in septicemias and urinary tract infections are limited, but good responses have been reported. | * [[Cryptococcus]]: [[Meningitis]] and [[pulmonary]] [[infections]] have been treated effectively. Studies in [[septicemias]] and [[urinary tract infections]] are limited, but good responses have been reported. | ||
* Ancobon should be used in combination with amphotericin B for the treatment of systemic candidiasis and cryptococcosis because of the emergence of resistance to Ancobon. | * Ancobon should be used in combination with [[amphotericin B]] for the treatment of systemic [[candidiasis]] and [[cryptococcosis]] because of the emergence of resistance to Ancobon. | ||
====Dosing Information==== | ====Dosing Information==== | ||
* The usual dosage of Ancobon is 50 to 150 mg/kg/day administered in divided doses at 6-hour intervals. Nausea or vomiting may be reduced or avoided if the capsules are given a few at a time over a 15-minute period. If the BUN or the serum creatinine is elevated, or if there are other signs of renal impairment, the initial dose should be at the lower level | * The usual dosage of Ancobon is 50 to 150 mg/kg/day administered in divided doses at 6-hour intervals. Nausea or vomiting may be reduced or avoided if the capsules are given a few at a time over a 15-minute period. If the [[BUN]] or the [[serum creatinine]] is elevated, or if there are other signs of [[renal impairment]], the initial dose should be at the lower level. | ||
* Ancobon should be used in combination with amphotericin B for the treatment of systemic candidiasis and cryptococcosis because of the emergence of resistance to Ancobon. | * Ancobon should be used in combination with [[amphotericin B]] for the treatment of systemic [[candidiasis]] and [[cryptococcosis]] because of the emergence of resistance to Ancobon. | ||
|offLabelAdultGuideSupport=There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of {{PAGENAME}} in adult patients. | |offLabelAdultGuideSupport=There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of {{PAGENAME}} in adult patients. | ||
| Line 49: | Line 49: | ||
<!--Warnings--> | <!--Warnings--> | ||
|warnings=* Ancobon must be given with extreme caution to patients with [[impaired renal function]]. Since Ancobon is excreted primarily by the [[kidney]]s, [[renal impairment]] may lead to accumulation of the drug. Ancobon serum concentrations should be monitored to determine the adequacy of renal excretion in such patients. Dosage adjustments should be made in patients with [[renal insufficiency]] to prevent progressive accumulation of active drug. | |warnings=* Ancobon must be given with extreme caution to patients with [[impaired renal function]]. Since Ancobon is excreted primarily by the [[kidney]]s, [[renal impairment]] may lead to accumulation of the drug. Ancobon [[serum]] concentrations should be monitored to determine the adequacy of renal excretion in such patients. Dosage adjustments should be made in patients with [[renal insufficiency]] to prevent progressive accumulation of active drug. | ||
* Ancobon must be given with extreme caution to patients with bone marrow depression. Patients may be more prone to [[depression of bone marrow]] function if they: 1) have a [[hematologic]] disease, 2) are being treated with radiation or drugs which [[depress bone marrow]], or 3) have a history of treatment with such drugs or radiation. [[Bone marrow]] [[toxicity]] can be irreversible and may lead to death in [[immunosuppressed]] patients. Frequent monitoring of [[hepatic]] function and of the [[hematopoietic]] system is indicated during therapy. | * Ancobon must be given with extreme caution to patients with [[bone marrow depression]]. Patients may be more prone to [[depression of bone marrow]] function if they: 1) have a [[hematologic]] disease, 2) are being treated with radiation or drugs which [[depress bone marrow]], or 3) have a history of treatment with such drugs or radiation. [[Bone marrow]] [[toxicity]] can be irreversible and may lead to death in [[immunosuppressed]] patients. Frequent monitoring of [[hepatic]] function and of the [[hematopoietic]] system is indicated during therapy. | ||
====PRECAUTIONS==== | ====PRECAUTIONS==== | ||
| Line 57: | Line 57: | ||
=====General===== | =====General===== | ||
* Before therapy with Ancobon is instituted, electrolytes (because of [[hypokalemia]]) and the [[hematologic]] and [[renal]] status of the patient should be determined. Close monitoring of the patient during therapy is essential. | * Before therapy with Ancobon is instituted, [[electrolytes]] (because of [[hypokalemia]]) and the [[hematologic]] and [[renal]] status of the patient should be determined. Close monitoring of the patient during therapy is essential. | ||
|clinicalTrials=* The adverse reactions which have occurred during treatment with Ancobon are grouped according to organ system affected. | |clinicalTrials=* The adverse reactions which have occurred during treatment with Ancobon are grouped according to organ system affected. | ||
=====Cardiovascular:===== | =====[[Cardiovascular]]:===== | ||
* Cardiac arrest, myocardial toxicity, ventricular dysfunction. | * [[Cardiac arrest]], [[myocardial]] [[toxicity]], [[ventricular dysfunction]]. | ||
=====Respiratory:===== | =====[[Respiratory]]:===== | ||
* Respiratory arrest, chest pain, dyspnea. | * [[Respiratory arrest]], [[chest pain]], [[dyspnea]]. | ||
=====Dermatologic:===== | =====[[Dermatologic]]:===== | ||
* Rash, pruritus, urticaria, photosensitivity. | * [[Rash]], [[pruritus]], [[urticaria]], [[photosensitivity]]. | ||
=====Gastrointestinal:===== | =====[[Gastrointestinal]]:===== | ||
* Nausea, emesis, abdominal pain, diarrhea, anorexia, dry mouth, duodenal ulcer, gastrointestinal hemorrhage, acute hepatic injury including hepatic necrosis with possible fatal outcome in debilitated patients, hepatic dysfunction, jaundice, ulcerative colitis, enterocolitis, bilirubin elevation, increased hepatic enzymes. | * [[Nausea]], [[emesis]], [[abdominal pain]], [[diarrhea]], [[anorexia]], dry mouth, [[duodenal ulcer]], gastrointestinal hemorrhage, acute hepatic injury including hepatic necrosis with possible fatal outcome in debilitated patients, hepatic dysfunction, [[jaundice]], [[ulcerative colitis]], enterocolitis, bilirubin elevation, increased hepatic enzymes. | ||
=====Genitourinary:===== | =====Genitourinary:===== | ||
* Azotemia, creatinine and BUN elevation, crystalluria, renal failure. | * [[Azotemia]], creatinine and BUN elevation, [[crystalluria]], renal failure. | ||
=====Hematologic:===== | =====Hematologic:===== | ||
* Anemia, agranulocytosis, aplastic anemia, eosinophilia, leukopenia, pancytopenia, thrombocytopenia, and fatal cases of bone marrow aplasia. | * [[Anemia]], [[agranulocytosis]], [[aplastic anemia]], [[eosinophilia]], leukopenia, pancytopenia, [[thrombocytopenia]], and fatal cases of bone marrow aplasia. | ||
=====Neurologic:===== | =====Neurologic:===== | ||
* Ataxia, hearing loss, headache, paresthesia, parkinsonism, peripheral neuropathy, pyrexia, vertigo, sedation, convulsions. | * [[Ataxia]], hearing loss, headache, paresthesia, parkinsonism, peripheral neuropathy, pyrexia, vertigo, sedation, [[convulsions]]. | ||
=====Psychiatric:===== | =====Psychiatric:===== | ||
| Line 108: | Line 108: | ||
* Measurement of serum creatinine levels should be determined by the Jaffé reaction, since Ancobon does not interfere with the determination of creatinine values by this method. Most automated equipment for measurement of creatinine makes use of the Jaffé reaction. | * Measurement of serum creatinine levels should be determined by the Jaffé reaction, since Ancobon does not interfere with the determination of creatinine values by this method. Most automated equipment for measurement of creatinine makes use of the Jaffé reaction. | ||
|FDAPregCat=C | |FDAPregCat=C | ||
|useInPregnancyFDA=* Flucytosine was shown to be teratogenic (vertebral fusions) in the rat at doses of 40 mg/kg/day (298 mg/M2/day or 0.051 times the human dose) administered on days 7 to 13 of gestation. At higher doses (700 mg/kg/day; 5208 mg/M2/day or 0.89 times the human dose administered on days 9 to 12 of gestation), cleft lip and palate and micrognathia were reported. Flucytosine was not teratogenic in rabbits up to a dose of 100 mg/kg/day (1423 mg/M2/day or 0.243 times the human dose) administered on days 6 to 18 of gestation. In mice, 400 mg/kg/day of flucytosine (1380 mg/M2/day or 0.236 times the human dose) administered on days 7 to 13 of gestation was associated with a low incidence of cleft palate that was not statistically significant. Studies in pregnant rats have shown that flucytosine injected intraperitoneally crosses the placental barrier. There are no adequate and well-controlled studies in pregnant women. Ancobon should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. | |useInPregnancyFDA=* Flucytosine was shown to be [[teratogenic]] ([[vertebral fusions]]) in the rat at doses of 40 mg/kg/day (298 mg/M2/day or 0.051 times the human dose) administered on days 7 to 13 of gestation. At higher doses (700 mg/kg/day; 5208 mg/M2/day or 0.89 times the human dose administered on days 9 to 12 of gestation), cleft lip and palate and [[micrognathia]] were reported. Flucytosine was not [[teratogenic]] in rabbits up to a dose of 100 mg/kg/day (1423 mg/M2/day or 0.243 times the human dose) administered on days 6 to 18 of gestation. In mice, 400 mg/kg/day of flucytosine (1380 mg/M2/day or 0.236 times the human dose) administered on days 7 to 13 of gestation was associated with a low incidence of cleft palate that was not statistically significant. Studies in pregnant rats have shown that flucytosine injected intraperitoneally crosses the placental barrier. There are no adequate and well-controlled studies in [[pregnant]] women. Ancobon should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. | ||
|useInPregnancyAUS=* '''Australian Drug Evaluation Committee (ADEC) Pregnancy Category''' | |useInPregnancyAUS=* '''Australian Drug Evaluation Committee (ADEC) Pregnancy Category''' | ||
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of {{PAGENAME}} in women who are pregnant. | There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of {{PAGENAME}} in women who are pregnant. | ||
|useInLaborDelivery=There is no FDA guidance on use of {{PAGENAME}} during labor and delivery. | |useInLaborDelivery=There is no FDA guidance on use of {{PAGENAME}} during labor and delivery. | ||
|useInNursing=* It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from Ancobon, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother. | |useInNursing=* It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing [[infants]] from Ancobon, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother. | ||
|useInPed=* The efficacy and safety of Ancobon have not been systematically studied in pediatric patients. A small number of neonates have been treated with 25 to 200 mg/kg/day of flucytosine, with and without the addition of amphotericin B, for systemic candidiasis. No unexpected adverse reactions were reported in these patients. It should be noted, however, that hypokalemia and acidemia were reported in one patient who received flucytosine in combination with amphotericin B, and anemia was observed in a second patient who received flucytosine alone. Transient thrombocytopenia was noted in two additional patients, one of whom also received amphotericin B. | |useInPed=* The efficacy and safety of Ancobon have not been systematically studied in pediatric patients. A small number of neonates have been treated with 25 to 200 mg/kg/day of flucytosine, with and without the addition of [[amphotericin B]], for systemic [[candidiasis]]. No unexpected adverse reactions were reported in these patients. It should be noted, however, that [[hypokalemia]] and acidemia were reported in one patient who received flucytosine in combination with amphotericin B, and anemia was observed in a second patient who received flucytosine alone. [[Transient thrombocytopenia]] was noted in two additional patients, one of whom also received [[amphotericin B]]. | ||
|useInGeri=There is no FDA guidance on the use of {{PAGENAME}} with respect to geriatric patients. | |useInGeri=There is no FDA guidance on the use of {{PAGENAME}} with respect to geriatric patients. | ||
|useInGender=There is no FDA guidance on the use of {{PAGENAME}} with respect to specific gender populations. | |useInGender=There is no FDA guidance on the use of {{PAGENAME}} with respect to specific gender populations. | ||
| Line 125: | Line 125: | ||
<!--Administration and Monitoring--> | <!--Administration and Monitoring--> | ||
|administration=* Oral | |administration=* Oral | ||
|monitoring= | |monitoring=* Ancobon must be given with extreme caution to patients with impaired renal function. Since Ancobon is excreted primarily by the kidneys, renal impairment may lead to accumulation of the drug. Ancobon serum concentrations should be monitored to determine the adequacy of renal excretion in such patients. Dosage adjustments should be made in patients with renal insufficiency to prevent progressive accumulation of active drug. | ||
* | * Ancobon must be given with extreme caution to patients with bone marrow depression. Patients may be more prone to depression of bone marrow function if they: 1) have a hematologic disease, 2) are being treated with radiation or drugs which depress bone marrow, or 3) have a history of treatment with such drugs or radiation. Bone marrow toxicity can be irreversible and may lead to death in immunosuppressed patients. Frequent monitoring of hepatic function and of the hematopoietic system is indicated during therapy. | ||
* Before therapy with Ancobon is instituted, electrolytes (because of hypokalemia) and the hematologic and renal status of the patient should be determined. Close monitoring of the patient during therapy is essential. | |||
=====Laboratory Tests===== | |||
* Since renal impairment can cause progressive accumulation of the drug, blood concentrations and kidney function should be monitored during therapy. Hematologic status ([[leucocyte]] and [[thrombocyte]] count) and liver function ([[alkaline phosphatase]], [[SGOT]] and [[SGPT]]) should be determined at frequent intervals during treatment as indicated. | |||
<!--IV Compatibility--> | <!--IV Compatibility--> | ||
| Line 133: | Line 139: | ||
<!--Overdosage--> | <!--Overdosage--> | ||
|overdose=* There is no experience with intentional overdosage. It is reasonable to expect that overdosage may produce pronounced manifestations of the known clinical adverse reactions. Prolonged serum concentrations in excess of 100 µg/mL may be associated with an increased incidence of toxicity, especially gastrointestinal (diarrhea, nausea, vomiting), hematologic (leukopenia, thrombocytopenia) and hepatic (hepatitis). | |overdose=* There is no experience with intentional overdosage. It is reasonable to expect that overdosage may produce pronounced manifestations of the known clinical adverse reactions. Prolonged serum concentrations in excess of 100 µg/mL may be associated with an increased incidence of [[toxicity]], especially gastrointestinal (diarrhea, nausea, vomiting), [[hematologic]] ([[leukopenia]], [[thrombocytopenia]]) and [[hepatic]] ([[hepatitis]]). | ||
* In the management of overdosage, prompt gastric lavage or the use of an emetic is recommended. Adequate fluid intake should be maintained, by the intravenous route if necessary, since Ancobon is excreted unchanged via the renal tract. The hematologic parameters should be monitored frequently; liver and kidney function should be carefully monitored. Should any abnormalities appear in any of these parameters, appropriate therapeutic measures should be instituted. | * In the management of overdosage, prompt gastric lavage or the use of an emetic is recommended. Adequate fluid intake should be maintained, by the intravenous route if necessary, since Ancobon is excreted unchanged via the renal tract. The hematologic parameters should be monitored frequently; liver and kidney function should be carefully monitored. Should any abnormalities appear in any of these parameters, appropriate therapeutic measures should be instituted. | ||
| Line 144: | Line 150: | ||
|structure=* Ancobon (flucytosine), an [[antifungal]] agent, is available as 250 mg and 500 mg capsules for oral administration. Each capsule also contains corn starch, lactose and talc. [[Gelatin]] capsule shells contain parabens (butyl, methyl, propyl) and sodium propionate, with the following dye systems: 250 mg capsules — black iron oxide, FD&C Blue No. 1, FD&C Yellow No. 6, D&C Yellow No. 10 and titanium dioxide; 500 mg capsules — black iron oxide and titanium dioxide. Chemically, flucytosine is 5-fluorocytosine, a fluorinated pyrimidine which is related to fluorouracil and floxuridine. It is a white to off-white crystalline powder with a molecular weight of 129.09 and the following structural formula: | |structure=* Ancobon (flucytosine), an [[antifungal]] agent, is available as 250 mg and 500 mg capsules for oral administration. Each capsule also contains corn starch, lactose and talc. [[Gelatin]] capsule shells contain parabens (butyl, methyl, propyl) and sodium propionate, with the following dye systems: 250 mg capsules — black iron oxide, FD&C Blue No. 1, FD&C Yellow No. 6, D&C Yellow No. 10 and titanium dioxide; 500 mg capsules — black iron oxide and titanium dioxide. Chemically, flucytosine is 5-fluorocytosine, a fluorinated pyrimidine which is related to fluorouracil and floxuridine. It is a white to off-white crystalline powder with a molecular weight of 129.09 and the following structural formula: | ||
[[File: | [[File:Flucytosine structure.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | ||
<!--Pharmacodynamics--> | <!--Pharmacodynamics--> | ||
| Line 176: | Line 182: | ||
:* Quantitative methods are used to determine antimicrobial minimum inhibitory concentrations (MICs). These MICs provide estimates of the susceptibility of Candida spp. to antimicrobial compounds. The MICs should be determined using a standardized procedure. Standardized procedures are based on a dilution method (broth)1 with standardized inoculum concentrations and standardized concentrations of flucytosine powder. The MIC values should be interpreted according to the criteria in Table 1. | :* Quantitative methods are used to determine antimicrobial minimum inhibitory concentrations (MICs). These MICs provide estimates of the susceptibility of Candida spp. to antimicrobial compounds. The MICs should be determined using a standardized procedure. Standardized procedures are based on a dilution method (broth)1 with standardized inoculum concentrations and standardized concentrations of flucytosine powder. The MIC values should be interpreted according to the criteria in Table 1. | ||
[[File:Flucytosine microbiology.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | |||
* A report of “Susceptible” indicates that the pathogen is likely to be inhibited if the antimicrobial compound in the blood reaches the concentration usually achievable. A report of "Intermediate" indicates that the result should be considered equivocal, and, if the microorganism is not fully susceptible to alternative, clinically feasible drugs, the test should be repeated. This category implies possible clinical applicability in body sites where the drug is physiologically concentrated or in situations where a high dosage of drug can be used. This category also provides a buffer zone which prevents small uncontrolled technical factors from causing major discrepancies in interpretation. A report of "Resistant" indicates that the pathogen is not likely to be inhibited if the antimicrobial compound in the blood reaches the concentration usually achievable; other therapy should be selected. Because of other significant host factors, in vitro susceptibility may not correlate with clinical outcomes. | * A report of “Susceptible” indicates that the pathogen is likely to be inhibited if the antimicrobial compound in the blood reaches the concentration usually achievable. A report of "Intermediate" indicates that the result should be considered equivocal, and, if the microorganism is not fully susceptible to alternative, clinically feasible drugs, the test should be repeated. This category implies possible clinical applicability in body sites where the drug is physiologically concentrated or in situations where a high dosage of drug can be used. This category also provides a buffer zone which prevents small uncontrolled technical factors from causing major discrepancies in interpretation. A report of "Resistant" indicates that the pathogen is not likely to be inhibited if the antimicrobial compound in the blood reaches the concentration usually achievable; other therapy should be selected. Because of other significant host factors, in vitro susceptibility may not correlate with clinical outcomes. | ||
| Line 182: | Line 188: | ||
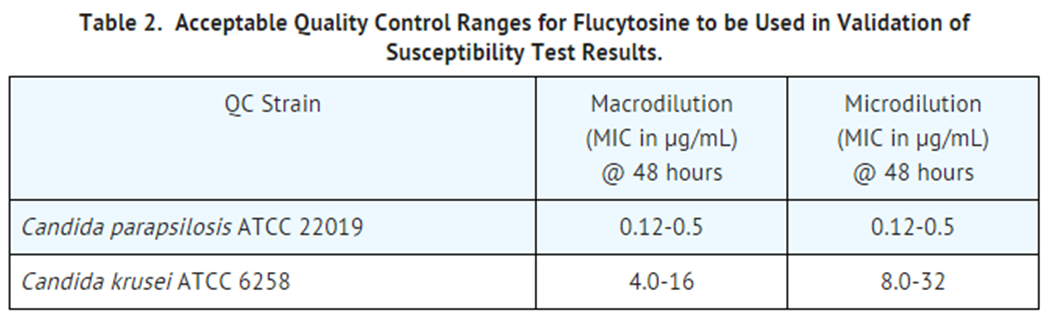
* Standardized susceptibility test procedures require the use of laboratory control microorganisms to control the technical aspects of the laboratory procedures. Standard flucytosine powder should provide the range of MIC values noted in Table 2. NOTE: Quality control microorganisms are specific strains of organisms with intrinsic biological properties relating to resistance mechanisms and their genetic expression within fungi; the specific strains used for microbiological control are not clinically significant. | * Standardized susceptibility test procedures require the use of laboratory control microorganisms to control the technical aspects of the laboratory procedures. Standard flucytosine powder should provide the range of MIC values noted in Table 2. NOTE: Quality control microorganisms are specific strains of organisms with intrinsic biological properties relating to resistance mechanisms and their genetic expression within fungi; the specific strains used for microbiological control are not clinically significant. | ||
[[File:Flucytosine microbiology2.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | |||
=====Drug Resistance===== | =====Drug Resistance===== | ||
| Line 213: | Line 219: | ||
Capsules, 500 mg (gray and white), imprinted ANCOBON® 500 ICN, bottles of 100 (NDC 0187-3555-10). | Capsules, 500 mg (gray and white), imprinted ANCOBON® 500 ICN, bottles of 100 (NDC 0187-3555-10). | ||
|storage=Store at 25°C (77°F); excursions permitted to 15°C - 30°C (59°F - 86°F). | |storage=Store at 25°C (77°F); excursions permitted to 15°C - 30°C (59°F - 86°F). | ||
|packLabel======PRINCIPAL DISPLAY PANEL - 250 MG CAPSULE BOTTLE LABEL===== | |packLabel======PRINCIPAL DISPLAY PANEL - 250 MG CAPSULE BOTTLE LABEL===== | ||
| Line 235: | Line 239: | ||
Pharmaceuticals North America LLC | Pharmaceuticals North America LLC | ||
image | [[File:Flucytosine drug lable01.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | ||
| Line 256: | Line 260: | ||
VALEANT | VALEANT | ||
Pharmaceuticals North America LLC | Pharmaceuticals North America LLC | ||
[[File:Flucytosine drug lable02.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | |||
|fdaPatientInfo=There is limited information regarding <i>Patient Counseling Information</i> of {{PAGENAME}} in the drug label. | |fdaPatientInfo=There is limited information regarding <i>Patient Counseling Information</i> of {{PAGENAME}} in the drug label. | ||
Latest revision as of 21:01, 18 August 2015
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Adeel Jamil, M.D. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
WARNING
See full prescribing information for complete Boxed Warning.
* Use with extreme caution in patients with impaired renal function. Close monitoring of hematologic, renal and hepatic status of all patients is essential. These instructions should be thoroughly reviewed before administration of Ancobon.
|
Overview
Flucytosine is a antifungal , anti-Infective agent that is FDA approved for the treatment of candidiasis and cryptococcosis. There is a Black Box Warning for this drug as shown here. Common adverse reactions include abdominal pain, diarrhea, nausea, vomiting, confusion, headache and hallucinations.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
- Ancobon is indicated only in the treatment of serious infections caused by susceptible strains of Candida and/or Cryptococcus.
- Candida: Septicemia, endocarditis and urinary system infections have been effectively treated with flucytosine. Limited trials in pulmonary infections justify the use of flucytosine.
- Cryptococcus: Meningitis and pulmonary infections have been treated effectively. Studies in septicemias and urinary tract infections are limited, but good responses have been reported.
- Ancobon should be used in combination with amphotericin B for the treatment of systemic candidiasis and cryptococcosis because of the emergence of resistance to Ancobon.
Dosing Information
- The usual dosage of Ancobon is 50 to 150 mg/kg/day administered in divided doses at 6-hour intervals. Nausea or vomiting may be reduced or avoided if the capsules are given a few at a time over a 15-minute period. If the BUN or the serum creatinine is elevated, or if there are other signs of renal impairment, the initial dose should be at the lower level.
- Ancobon should be used in combination with amphotericin B for the treatment of systemic candidiasis and cryptococcosis because of the emergence of resistance to Ancobon.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Flucytosine in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Flucytosine in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding FDA-Labeled Use of Flucytosine in pediatric patients.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Flucytosine in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Flucytosine in pediatric patients.
Contraindications
- Ancobon should not be used in patients with a known hypersensitivity to the drug.
Warnings
|
WARNING
See full prescribing information for complete Boxed Warning.
* Use with extreme caution in patients with impaired renal function. Close monitoring of hematologic, renal and hepatic status of all patients is essential. These instructions should be thoroughly reviewed before administration of Ancobon.
|
- Ancobon must be given with extreme caution to patients with impaired renal function. Since Ancobon is excreted primarily by the kidneys, renal impairment may lead to accumulation of the drug. Ancobon serum concentrations should be monitored to determine the adequacy of renal excretion in such patients. Dosage adjustments should be made in patients with renal insufficiency to prevent progressive accumulation of active drug.
- Ancobon must be given with extreme caution to patients with bone marrow depression. Patients may be more prone to depression of bone marrow function if they: 1) have a hematologic disease, 2) are being treated with radiation or drugs which depress bone marrow, or 3) have a history of treatment with such drugs or radiation. Bone marrow toxicity can be irreversible and may lead to death in immunosuppressed patients. Frequent monitoring of hepatic function and of the hematopoietic system is indicated during therapy.
PRECAUTIONS
General
- Before therapy with Ancobon is instituted, electrolytes (because of hypokalemia) and the hematologic and renal status of the patient should be determined. Close monitoring of the patient during therapy is essential.
Adverse Reactions
Clinical Trials Experience
- The adverse reactions which have occurred during treatment with Ancobon are grouped according to organ system affected.
Cardiovascular:
Respiratory:
Dermatologic:
Gastrointestinal:
- Nausea, emesis, abdominal pain, diarrhea, anorexia, dry mouth, duodenal ulcer, gastrointestinal hemorrhage, acute hepatic injury including hepatic necrosis with possible fatal outcome in debilitated patients, hepatic dysfunction, jaundice, ulcerative colitis, enterocolitis, bilirubin elevation, increased hepatic enzymes.
Genitourinary:
- Azotemia, creatinine and BUN elevation, crystalluria, renal failure.
Hematologic:
- Anemia, agranulocytosis, aplastic anemia, eosinophilia, leukopenia, pancytopenia, thrombocytopenia, and fatal cases of bone marrow aplasia.
Neurologic:
- Ataxia, hearing loss, headache, paresthesia, parkinsonism, peripheral neuropathy, pyrexia, vertigo, sedation, convulsions.
Psychiatric:
- Confusion, hallucinations, psychosis.
Miscellaneous:
- Fatigue, hypoglycemia, hypokalemia, weakness, allergic reactions, Lyell’s syndrome.
Postmarketing Experience
There is limited information regarding Postmarketing Experience of Flucytosine in the drug label.
Drug Interactions
Drug Interactions
- Cytosine arabinoside, a cytostatic agent, has been reported to inactivate the antifungal activity of Ancobon by competitive inhibition. Drugs which impair glomerular filtration may prolong the biological half-life of flucytosine.
Laboratory Tests
- Since renal impairment can cause progressive accumulation of the drug, blood concentrations and kidney function should be monitored during therapy. Hematologic status (leucocyte and thrombocyte count) and liver function (alkaline phosphatase, SGOT and SGPT) should be determined at frequent intervals during treatment as indicated.
Drug/Laboratory Test Interactions
- Measurement of serum creatinine levels should be determined by the Jaffé reaction, since Ancobon does not interfere with the determination of creatinine values by this method. Most automated equipment for measurement of creatinine makes use of the Jaffé reaction.
Use in Specific Populations
Pregnancy
- Flucytosine was shown to be teratogenic (vertebral fusions) in the rat at doses of 40 mg/kg/day (298 mg/M2/day or 0.051 times the human dose) administered on days 7 to 13 of gestation. At higher doses (700 mg/kg/day; 5208 mg/M2/day or 0.89 times the human dose administered on days 9 to 12 of gestation), cleft lip and palate and micrognathia were reported. Flucytosine was not teratogenic in rabbits up to a dose of 100 mg/kg/day (1423 mg/M2/day or 0.243 times the human dose) administered on days 6 to 18 of gestation. In mice, 400 mg/kg/day of flucytosine (1380 mg/M2/day or 0.236 times the human dose) administered on days 7 to 13 of gestation was associated with a low incidence of cleft palate that was not statistically significant. Studies in pregnant rats have shown that flucytosine injected intraperitoneally crosses the placental barrier. There are no adequate and well-controlled studies in pregnant women. Ancobon should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
- Australian Drug Evaluation Committee (ADEC) Pregnancy Category
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Flucytosine in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Flucytosine during labor and delivery.
Nursing Mothers
- It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from Ancobon, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
- The efficacy and safety of Ancobon have not been systematically studied in pediatric patients. A small number of neonates have been treated with 25 to 200 mg/kg/day of flucytosine, with and without the addition of amphotericin B, for systemic candidiasis. No unexpected adverse reactions were reported in these patients. It should be noted, however, that hypokalemia and acidemia were reported in one patient who received flucytosine in combination with amphotericin B, and anemia was observed in a second patient who received flucytosine alone. Transient thrombocytopenia was noted in two additional patients, one of whom also received amphotericin B.
Geriatic Use
There is no FDA guidance on the use of Flucytosine with respect to geriatric patients.
Gender
There is no FDA guidance on the use of Flucytosine with respect to specific gender populations.
Race
There is no FDA guidance on the use of Flucytosine with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Flucytosine in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Flucytosine in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Flucytosine in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Flucytosine in patients who are immunocompromised.
Administration and Monitoring
Administration
- Oral
Monitoring
- Ancobon must be given with extreme caution to patients with impaired renal function. Since Ancobon is excreted primarily by the kidneys, renal impairment may lead to accumulation of the drug. Ancobon serum concentrations should be monitored to determine the adequacy of renal excretion in such patients. Dosage adjustments should be made in patients with renal insufficiency to prevent progressive accumulation of active drug.
- Ancobon must be given with extreme caution to patients with bone marrow depression. Patients may be more prone to depression of bone marrow function if they: 1) have a hematologic disease, 2) are being treated with radiation or drugs which depress bone marrow, or 3) have a history of treatment with such drugs or radiation. Bone marrow toxicity can be irreversible and may lead to death in immunosuppressed patients. Frequent monitoring of hepatic function and of the hematopoietic system is indicated during therapy.
- Before therapy with Ancobon is instituted, electrolytes (because of hypokalemia) and the hematologic and renal status of the patient should be determined. Close monitoring of the patient during therapy is essential.
Laboratory Tests
- Since renal impairment can cause progressive accumulation of the drug, blood concentrations and kidney function should be monitored during therapy. Hematologic status (leucocyte and thrombocyte count) and liver function (alkaline phosphatase, SGOT and SGPT) should be determined at frequent intervals during treatment as indicated.
IV Compatibility
There is limited information regarding IV Compatibility of Flucytosine in the drug label.
Overdosage
- There is no experience with intentional overdosage. It is reasonable to expect that overdosage may produce pronounced manifestations of the known clinical adverse reactions. Prolonged serum concentrations in excess of 100 µg/mL may be associated with an increased incidence of toxicity, especially gastrointestinal (diarrhea, nausea, vomiting), hematologic (leukopenia, thrombocytopenia) and hepatic (hepatitis).
- In the management of overdosage, prompt gastric lavage or the use of an emetic is recommended. Adequate fluid intake should be maintained, by the intravenous route if necessary, since Ancobon is excreted unchanged via the renal tract. The hematologic parameters should be monitored frequently; liver and kidney function should be carefully monitored. Should any abnormalities appear in any of these parameters, appropriate therapeutic measures should be instituted.
- Since hemodialysis has been shown to rapidly reduce serum concentrations in anuric patients, this method may be considered in the management of overdosage.
Pharmacology
There is limited information regarding Flucytosine Pharmacology in the drug label.
Mechanism of Action
- Flucytosine is taken up by fungal organisms via the enzyme cytosine permease. Inside the fungal cell, flucytosine is rapidly converted to fluorouracil by the enzyme cytosine deaminase. Fluorouracil exerts its antifungal activity through the subsequent conversion into several active metabolites, which inhibit protein synthesis by being falsely incorporated into fungal RNA or interfere with the biosynthesis of fungal DNA through the inhibition of the enzyme thymidylate synthetase.
Structure
- Ancobon (flucytosine), an antifungal agent, is available as 250 mg and 500 mg capsules for oral administration. Each capsule also contains corn starch, lactose and talc. Gelatin capsule shells contain parabens (butyl, methyl, propyl) and sodium propionate, with the following dye systems: 250 mg capsules — black iron oxide, FD&C Blue No. 1, FD&C Yellow No. 6, D&C Yellow No. 10 and titanium dioxide; 500 mg capsules — black iron oxide and titanium dioxide. Chemically, flucytosine is 5-fluorocytosine, a fluorinated pyrimidine which is related to fluorouracil and floxuridine. It is a white to off-white crystalline powder with a molecular weight of 129.09 and the following structural formula:

Pharmacodynamics
Microbiology
Activity In Vitro
- Flucytosine has been shown to be active against most strains of the following microorganisms both in vitro and in clinical infections.
Candida albicansCryptococcus neoformans
- The following in vitro data are available, but their clinical significance is unknown.
- Flucytosine exhibits in vitro minimum inhibitory concentrations (MIC values) of 4 μg/mL, or less against most (≥90%) strains of the following microorganisms, however, the safety and effectiveness of flucytosine in treating clinical infections due to these microorganisms have not been established in adequate and well control trials.
- Candida dubliniensisCandida glabrataCandida guilliermondiiCandida lusitaniaeCandida parapsilosisCandida tropicalis
- Candida krusei should be considered to be resistant to flucytosine.
- In vitro activity of flucytosine is affected by the test conditions. It is essential to follow the approved standard method guidelines.1
Susceptibility Testing Methods
Cryptococcus neoformans:
- No interpretive criteria have been established for Cryptococcus neoformans.
Candida species:
- Broth Dilution Techniques:
- Quantitative methods are used to determine antimicrobial minimum inhibitory concentrations (MICs). These MICs provide estimates of the susceptibility of Candida spp. to antimicrobial compounds. The MICs should be determined using a standardized procedure. Standardized procedures are based on a dilution method (broth)1 with standardized inoculum concentrations and standardized concentrations of flucytosine powder. The MIC values should be interpreted according to the criteria in Table 1.

- A report of “Susceptible” indicates that the pathogen is likely to be inhibited if the antimicrobial compound in the blood reaches the concentration usually achievable. A report of "Intermediate" indicates that the result should be considered equivocal, and, if the microorganism is not fully susceptible to alternative, clinically feasible drugs, the test should be repeated. This category implies possible clinical applicability in body sites where the drug is physiologically concentrated or in situations where a high dosage of drug can be used. This category also provides a buffer zone which prevents small uncontrolled technical factors from causing major discrepancies in interpretation. A report of "Resistant" indicates that the pathogen is not likely to be inhibited if the antimicrobial compound in the blood reaches the concentration usually achievable; other therapy should be selected. Because of other significant host factors, in vitro susceptibility may not correlate with clinical outcomes.
- Standardized susceptibility test procedures require the use of laboratory control microorganisms to control the technical aspects of the laboratory procedures. Standard flucytosine powder should provide the range of MIC values noted in Table 2. NOTE: Quality control microorganisms are specific strains of organisms with intrinsic biological properties relating to resistance mechanisms and their genetic expression within fungi; the specific strains used for microbiological control are not clinically significant.
Drug Resistance
- Flucytosine resistance may arise from a mutation of an enzyme necessary for the cellular uptake or metabolism of flucytosine or from an increased synthesis of pyrimidines, which compete with the active metabolites of flucytosine (fluorinated antimetabolites). Resistance to flucytosine has been shown to develop during monotherapy after prolonged exposure to the drug.
- Candida krusei should be considered to be resistant to flucytosine.
Drug Combination
- Antifungal synergism between flucytosine and polyene antibiotics, particularly amphotericin B has been reported in vitro. Ancobon is usually administered in combination with amphotericin B due to lack of cross-resistance and reported synergistic activity of both drugs.
Pharmacokinetics
- Flucytosine is rapidly and virtually completely absorbed following oral administration. Ancobon is not metabolized significantly when given orally to man. Bioavailability estimated by comparing the area under the curve of serum concentrations after oral and intravenous administration showed 78% to 89% absorption of the oral dose. Peak serum concentrations of 30 to 40 µg/mL were reached within 2 hours of administration of a 2 g oral dose to normal subjects. Other studies revealed mean serum concentrations of approximately 70 to 80 μg/mL 1 to 2 hours after a dose in patients with normal renal function receiving a 6-week regimen of flucytosine (150 mg/kg/day given in divided doses every 6 hours) in combination with amphotericin B. The half-life in the majority of healthy subjects ranged between 2.4 and 4.8 hours. Flucytosine is excreted via the kidneys by means of glomerular filtration without significant tubular reabsorption. More than 90% of the total radioactivity after oral administration was recovered in the urine as intact drug. Flucytosine is deaminated (probably by gut bacteria) to 5-fluorouracil. The area under the curve (AUC) ratio of 5-fluorouracil to flucytosine is 4%. Approximately 1% of the dose is present in the urine as the α-fluoro-β-ureido-propionic acid metabolite. A small portion of the dose is excreted in the feces.
- The half-life of flucytosine is prolonged in patients with renal insufficiency; the average half-life in nephrectomized or anuric patients was 85 hours (range: 29.9 to 250 hours). A linear correlation was found between the elimination rate constant of flucytosine and creatinine clearance.
- In vitro studies have shown that 2.9% to 4% of flucytosine is protein-bound over the range of therapeutic concentrations found in the blood. Flucytosine readily penetrates the blood-brain barrier, achieving clinically significant concentrations in cerebrospinal fluid.
Pharmacokinetics in Pediatric Patients
- Limited data are available regarding the pharmacokinetics of Ancobon administered to neonatal patients being treated for systemic candidiasis. After five days of continuous therapy, median peak levels in infants were 19.6 µg/mL, 27.7 µg/mL, and 83.9 µg/mL at doses of 25 mg/kg (N=3), 50 mg/kg (N=4), and 100 mg/kg (N=3), respectively. Mean time to peak serum levels was of 2.5 ± 1.3 hours, similar to that observed in adult patients. A good deal of interindividual variability was noted, which did not correlate with gestational age. Some patients had serum levels > 100 µg/mL, suggesting a need for drug level monitoring during therapy. In another study, serum concentrations were determined during flucytosine therapy in two patients (total assays performed =10). Median serum flucytosine concentrations at steady state were calculated to be 57 ± 10 µg/mL (doses of 50 to 125 mg/kg/day, normalized to 25 mg/kg per dose for comparison). In three infants receiving flucytosine 25 mg/kg/day (four divided doses), a median flucytosine half-life of 7.4 hours was observed, approximately double that seen in adult patients. The concentration of flucytosine in the cerebrospinal fluid of one infant was 43 µg/mL 3 hours after a 25 mg oral dose, and ranged from 20 to 67 mg/L in another neonate receiving oral doses of 120 to 150 mg/kg/day.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- Flucytosine has not undergone adequate animal testing to evaluate carcinogenic potential. The mutagenic potential of flucytosine was evaluated in Ames-type studies with five different mutants of S. typhimurium and no mutagenicity was detected in the presence or absence of activating enzymes. Flucytosine was nonmutagenic in three different repair assay systems (i.e., rec, uvr and pol).
- There have been no adequate trials in animals on the effects of flucytosine on fertility or reproductive performance. The fertility and reproductive performance of the offspring (F1 generation) of mice treated with 100 mg/kg/day (345 mg/M2/day or 0.059 times the human dose), 200 mg/kg/day (690 mg/M2/day or 0.118 times the human dose) or 400 mg/kg/day (1380 mg/M2/day or 0.236 times the human dose) of flucytosine on days 7 to 13 of gestation was studied; the in utero treatment had no adverse effect on the fertility or reproductive performance of the offspring.
Clinical Studies
There is limited information regarding Clinical Studies of Flucytosine in the drug label.
How Supplied
Capsules, 250 mg (gray and green), imprinted ANCOBON® 250 ICN, bottles of 100 (NDC 0187-3554-10).
Capsules, 500 mg (gray and white), imprinted ANCOBON® 500 ICN, bottles of 100 (NDC 0187-3555-10).
Storage
Store at 25°C (77°F); excursions permitted to 15°C - 30°C (59°F - 86°F).
Images
Drug Images
{{#ask: Page Name::Flucytosine |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
PRINCIPAL DISPLAY PANEL - 250 MG CAPSULE BOTTLE LABEL
NDC 0187-3554-10 Rx Only
Ancobon® (flucytosine)
250 mg
Each capsule contains 250 mg flucytosine
100 Capsules
VALEANT Pharmaceuticals North America LLC

PRINCIPAL DISPLAY PANEL - 500 MG CAPSULE BOTTLE LABEL
NDC 0187-3555-10 Rx Only
Ancobon® (flucytosine)
500 mg
Each capsule contains 500 mg flucytosine
100 Capsules
VALEANT Pharmaceuticals North America LLC

{{#ask: Label Page::Flucytosine |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
There is limited information regarding Patient Counseling Information of Flucytosine in the drug label.
Precautions with Alcohol
- Alcohol-Flucytosine interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- Ancobon®
Look-Alike Drug Names
There is limited information regarding Flucytosine Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
{{#subobject:
|Page Name=Flucytosine
|Pill Name=No image.jpg
|Drug Name=
|Pill Ingred=|+sep=;
|Pill Imprint=
|Pill Dosage={{{dosageValue}}} {{{dosageUnit}}}
|Pill Color=|+sep=;
|Pill Shape=
|Pill Size (mm)=
|Pill Scoring=
|Pill Image=
|Drug Author=
|NDC=
}}
{{#subobject:
|Label Page=Flucytosine |Label Name=Flucytosine11.png
}}
{{#subobject:
|Label Page=Flucytosine |Label Name=Flucytosine11.png
}}