Tracheobronchial injury
| Tracheobronchial injury | |
 | |
|---|---|
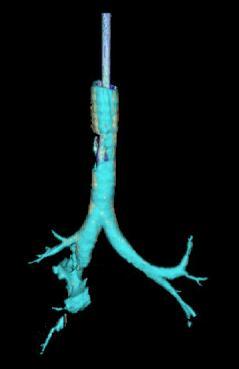
| Reconstruction of the trachea and bronchi with CT scanning showing disruption of the right main bronchus[1] | |
| ICD-10 | S27.4, S27.5 |
| eMedicine | radio/706 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Tracheobronchial injury (TBI) is damage to the tracheobronchial tree (the structure of airways involving the trachea and bronchi).[2] It can result from blunt or penetrating neck or chest trauma. The airways may also be injured by inhaling harmful fumes, or aspirating liquids or objects.[3]
Though rare, TBI is potentially fatal. TBI can cause the airway to be blocked and can restrict breathing.[2] Other injuries accompany TBI in about half of cases.[4] Most people with the injury who die do so before receiving emergency care, due to other injuries to vital organs, profuse bleeding, and insufficient airway.[5] Of those who do reach a hospital, the mortality rate is about 30%.
Early diagnosis is important to prevent complications, which include narrowing of the airway, respiratory infections, and damage to the lung tissue. Diagnosis involves bronchoscopy to visualize the airways, and X-ray can be used as well. Signs and symptoms include difficulty breathing, hoarseness, coughing, and abnormal breath sounds; however they vary based on the location and severity of the injury. In the emergency setting, intubation with an endotracheal tube can be used to ensure that the airway remains open so the patient can breathe. Surgery to repair a tracheobronchial tear is usually considered standard; however in less severe cases TBI may be managed conservatively and allowed to heal without surgery.[6]
Anatomy
The trachea and bronchi form the tracheobronchial tree. An arbitrary division can be made between the intrathoracic and cervical trachea at the at the thoracic inlet.[7] The carina is the ridge where the trachea splits into two bronchi. Anatomical structures that surround and protect the tracheobronchial tree include the lungs, the esophagous, large blood vessels, and the sternum.[7]
Classification
Lesions can be transverse, occurring between the rings of the trachea, or longitudinal or spiral, occurring along the membranous part of the trachea, the main bronchi, or both.[2] In 8% of ruptures, lesions are complex, occurring in more than one location or with more than one type of lesion on both main bronchi and the trachea.[2] Transverse tears are more common than longitudinal or complex ones.[7] Another way to classify tracheal lesions is to divide them into complete and incomplete lacerations.[3]
Bronchial injuries are divided into those that are accompanied by a disruption of the pleura and those that are not; in the former, air can leak from the hole in the airway and a pneumothorax can form.[8] The latter type is associated with more minor signs; pneumothorax is small if it occurs at all, and though function is lost in the part of the lung which receives air from the injured bronchus, the rest of the lungs may be able to compensate.[8]
Most TBIs that result from blunt trauma occur within the chest.[9] The most common tracheal injury is a tear near the carina or in the membranous wall of the trachea.[8] In blunt chest trauma, TBI occurs within 2.5 cm of the carina 40–80% of the time.[2] The injury is more common in the right main bronchus than the left, possibly because the former is near vertebrae, which may injure it.[2] Also, the aorta and other tissues in the mid chest that surround the left main bronchus may protect it.[10] Another possibility is that people with left main bronchus injuries are more likely to also have other deadly injuries and therefore die before reaching hospital, making them less likely to be included in studies that determine rates of injuries.[5]
Signs and symptoms
Signs and symptoms vary depending on what part of the tracheobronchial tree is injured and how severely it is damaged.[5] There are no direct signs of TBI, but certain signs suggest the injury and raise a clinician's suspicion that it has occurred.[11] Many of the signs and symptoms are also present in injuries with similar injury mechanisms such as pneumothorax.[12] Dyspnea (difficulty breathing) and respiratory distress are found in 76–100% of people with TBI, and hemoptysis (coughing up blood) has been found in up to a quarter.[9] However, TBI does not usually cause profuse bleeding; thus, such bleeding that does occur is likely to be due to another injury such as one to a large blood vessel.[2] The patient may be hoarse or have diminished breath sounds, and rapid breathing is common.[6] Coughing may be present,[13] and stridor, an abnormal, high pitched breath sound indicating obstruction of the upper airway can also occur.[14]
Damage to the airways can cause subcutaneous emphysema (air trapped in the subcutaneous tissue of the skin) in the abdomen, chest, neck, and head.[2] Subcutaneous emphysema, present in up to 85% of people with TBI,[9] is particularly indicative of the injury when it is only in the neck.[15] Air is trapped in the chest cavity outside the lungs (pneumothorax) in about 70% of tracheobronchial tears.[3][9] Particularly strong evidence that TBI has occurred is failure of a pneumothorax to go away even when a chest tube is placed to rid the chest cavity of the air; it may indicate that air is continually leaking into the chest cavity from the site of the tear.[13] Air can also be trapped in the mediastinum, the center of the chest cavity (pneumomediastinum).[3] If air escapes from a penetrating injury to the neck, a definite diagnosis of TBI can be made.[9] Hamman's sign, a sound of crunching or clicking that occurs in time with the heartbeat, also occasionally accompanies TBI.[2]
Causes
Injuries to the tracheobronchial tree within the chest may occur in gunshot wounds, but are more often the result of blunt trauma.[5] In blunt trauma, high-energy impacts such as falls from height and vehicle collisions are the usual mechanism for TBI; the injury is rare in low-impact mechanisms.[2] Injuries of the trachea cause about 1% of traffic-related deaths.[3] Other potential causes are falls from high places and injuries in which the chest is crushed.[8]
When the injury is due to penetrating trauma, gunshots are the usual cause,[8] but knives and shrapnel from car accidents can also penetrate the airways.[5] Most injuries to the trachea occur in the neck,[6] because the airways within the chest are deep and therefore well protected; however, a quarter of TBIs resulting from penetrating trauma do occur within the chest.[9] Injury to the cervical trachea usually affects the anterior (front) part of the trachea.[7]
Certain medical procedures can also injure the airways; these include endotracheal intubation, endoscopy, and tracheostomy.[3] When an endotracheal tube tears the trachea, it typically does so at the posterior (back) membranous wall.[7] Excessive pressure from the cuff of an endotracheal tube can reduce blood supply to the tissues of the trachea, leading to ischemia and potentially causing it to become ulcerated, infected, and, later, narrowed.[3]
The inner lining of the trachea may also be injured by inhaling hot gasses or harmful fumes such as chlorine gas.[7] This can damage the mucosal lining of the airways and lead to edema (swelling), necrosis (death of the tissue), scar formation, and ultimately stenosis (a narrowing of the airway).[7] However, TBI due to inhalation, foreign body aspiration, and medical procedures is uncommon.[7]
Mechanism
The structures in the tracheobronchial tree are well protected, so it normally takes a large amount of force to injure them.[5] In blunt trauma, TBI is usually the result of violent compression of the chest.[9][4]
Although the mechanism is not well understood, TBI due to blunt trauma is widely thought to be caused by any combination of three possible mechanisms: an increase in pressure within the airways, shearing, and pulling apart.[13] The first type of injury, sometimes called an "explosive rupture", may occur when the chest is violently compressed, for example when a driver strikes the steering wheel in a vehicle accident.[3] As a result of the compression, the pressure in the airways, especially the larger airways (the trachea and bronchi), quickly and sharply rises[10] because the glottis reflexively closes off the airways.[2] When this pressure exceeds the elasticity of the tissues, they burst.[10] The membranous part of the trachea is more commonly affected by this mechanism of injury than cartilaginous portions.[10][7]
The second mechanism may occur when the chest is suddenly decelerated, as occurs in vehicle accidents, producing a shearing force.[10] The lungs have mobility in the pleural space but their movement is more restricted near the carina.[10] Areas near the cricoid and carina are fixed to the thyroid cartilage and the pericardium respectively; thus if the airways move, they can tear at these points of fixation.[2]
The third mechanism occurs when the chest is compressed from front to back, causing it to widen from side to side.[9] The lungs adhere to the chest wall because of the negative pressure between them and the pleural membranes that line the inside of the chest cavity; thus when the chest widens, they are pulled apart.[9] This creates tension at the carina; the airway tears if this tensile force exceeds its elasticity.[9] This mechanism may be the cause of injury when the chest is crushed.[10] Most TBIs are probably due to a combination of these three mechanisms.[5]
When airways are damaged, air can escape from them and be trapped in the surrounding tissues; it can build up there to pressures high enough to compress the airways.[2] Blood and other fluids can build up in the airways, and the injury can interfere with the patency of the airway and interfere with its continuity.[2] However, even if the trachea is completely transected, the tissues surrounding it may hold it together enough for adequate air exchange to occur, at least at first.[3]
Diagnosis
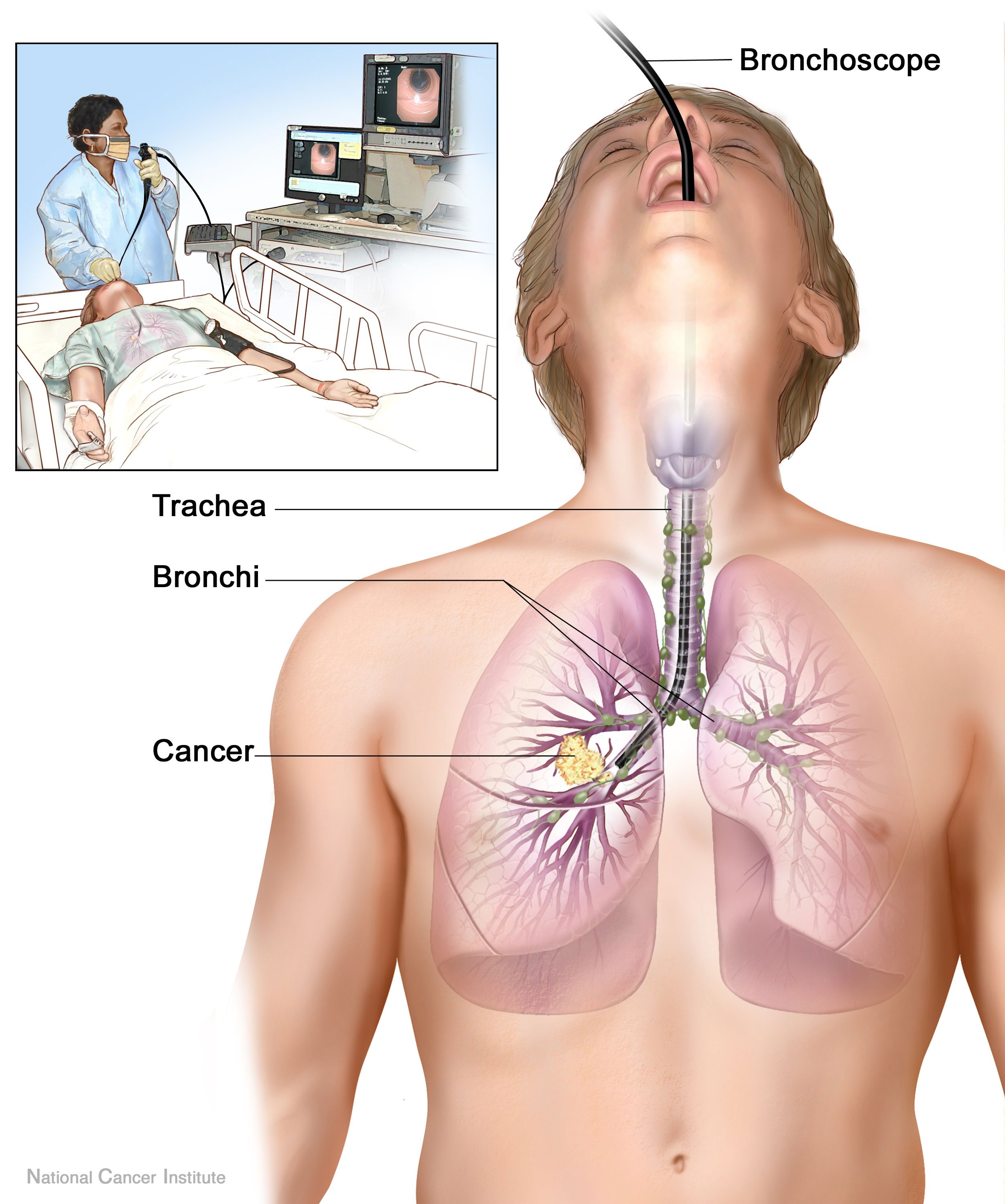
Rapid diagnosis and treatment are important in the care of TBI;[5] if the injury is not diagnosed shortly after the injury, the risk of complications is higher.[13] Bronchoscopy is the most effective method to diagnose, locate, and determine the severity of TBI.[9][5] Diagnosis with a flexible bronchoscope, which allows the injury to be visualized directly, is the fastest and most reliable technique.[11] In people with TBI, bronchoscopy may reveal that the airway is torn, or that the airways are blocked by blood, or that a bronchus has collapsed, obscuring more distal bronchi from view.[6]
Chest X-ray is the initial imaging technique used to diagnose TBI.[7] The film may not have any signs in an otherwise asymptomatic patient.[8] Indications of TBI seen on X-ray include a deformity in the trachea and a defect in the tracheal wall.[7] Radiography may also show cervical emphysema, air in the tissues of the neck.[2] X-rays may also show accompanying injuries and signs such as fractures and subcutaneous emphysema.[2] If subcutaneous emphysema occurs and the hyoid bone appears in an X-ray to be sitting unusually high in the throat, it may be an indication that the trachea has been severed.[3] TBI is also suspected if an endotracheal tube appears in an X-ray to be out of place, or if its cuff appears to be more full than normal or to protrude through a tear in the airway.[7] If a bronchus is torn all the way around, the lung may collapse outward toward the chest wall (rather than inward, as it usually does in pneumothorax) because it loses the attachment to the bronchus which normally holds it toward the center.[5] This sign, described in 1969, is called fallen lung sign and is pathognomonic of TBI (that is, it is diagnostic for TBI because it does not occur in other conditions); however it occurs only rarely.[5] CT scanning detects over 90% of TBIs that result from blunt trauma,[6] but neither X-ray nor CT are a replacement for bronchoscopy.[5]
At least 30% of tracheobronchial injuries are not discovered at first.[3] In about 10% of cases, TBI has no specific signs either clinically or on chest radiography, and its detection may be further complicated by concurrent injuries, since TBI tends to occur after high-energy accidents.[2] It is not uncommon for weeks or months go by before the injury is diagnosed, even though the injury is better known than it was in the past.[10]
Treatment
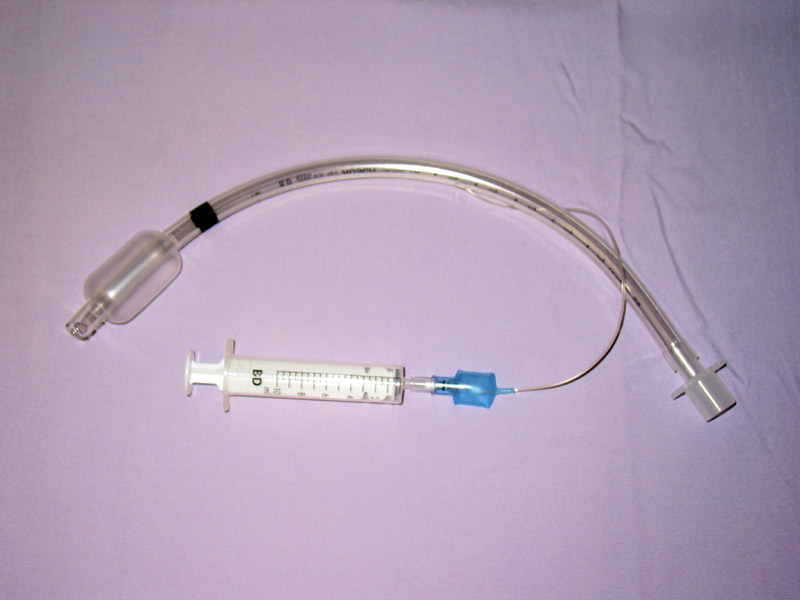
Treatment of TBI varies based on the location and severity of injury and whether the patient is stable or having trouble breathing,[2] but ensuring that the airway is patent so that the patient can breathe is always of paramount importance.[9] Intubation, one method to secure the airway, can be used to bypass the tear in the airway in order to send air to the lungs.[6] Intubation through the mouth is the most common method of securing an airway.[6] If necessary, a tube can be placed into the uninjured bronchus, and a single lung can be ventilated.[6] If there is a penetrating injury to the neck through which air is escaping, the patient may be intubated through the wound.[9] Multiple unsuccessful attempts to intubate may threaten the airway, so techniques that allow healthcare providers to visualize the airway may be used to facilitate intubation.[9] Clinicians can visualize the airway with a bronchoscope, and a fiberoptic endotracheal tube can also be used.[9] Tube thoracostomy may be used, and cricothyroidotomy or tracheostomy may be needed in order to ensure an open airway.[5] However, cricothyroidotomy may not be useful in TBI because the tear may be more distal to (below) the site of the artificial airway.[9] Tracheostomy is used sparingly because it can cause complications such as infections and narrowing of the trachea and larynx.[16] When it is impossible to establish a sufficient airway, or when complicated surgery must be performed, cardiopulmonary bypass may be used—blood is pumped out of the body, oxygenated by a machine, and pumped back in.[16]
Supplemental oxygen is provided.[15] Mechanical ventilation may be needed, but can worsen a tear by forcing air through it.[2] Positive end expiratory pressure, while helpful in maintaining adequate oxygenation, can increase leakage of air through a tear, and can stress the sutures in a tear that has been surgically repaired.[6] Therefore, healthcare providers try to use the lowest possible airway pressures that still maintain oxygenation.[6] Mechanical ventilation can cause barotrauma to the lung when excessive pressure results from the patient "fighting the ventilator"; airway pressure release ventilation, which allows breathing at any point in the respiratory cycle, reduces the likelihood of this problem.[6] Techniques such as pulmonary toilet (removal of secretions), fluid management, and treatment of pneumonia are employed to improve pulmonary compliance (the elasticity of the lungs).[16]
While TBI may be managed without surgery, surgical repair of the tear is considered standard in the treatment of most TBI.[6] It is required if a tear interferes with ventilation, if mediastinitis (inflammation of the tissues in the mid-chest) occurs, or if subcutaneous or mediastinal emphysema progresses rapidly.[6] Other indications for surgery are a tear more than one third the circumference of the airway, tears with loss of tissue, and a need for positive pressure ventilation.[16] Surgery to repair the tear can be successful even when it is performed months after the trauma, as can occur when TBI is not noticed right away.[6] Damaged tissue around a rupture (e.g. torn or scarred tissue) may be removed in order to get clean edges that can be surgically repaired.[10] When lung tissue is destroyed as a result of TBI complications, pneumonectomy or lobectomy (removal of a lung or of one lobe, respectively) may be required.[17]
Prognosis and complications
Most people who die do so within minutes of the injury, due to complications such as pneumothorax and insufficient airway and to other injuries that occurred at the same time.[4] Most late deaths that occur in TBI are attributed to sepsis or multi-organ dysfunction syndrome.[2] If the condition is not recognized and treated early, serious complications are more likely occur; for example,[17] pneumonia and bronchiectasis may occur as late complications.[6] Years can pass before the condition is recognized.[12][17] Some TBIs are so small that they do not have significant clinical manifestations; they may never be noticed or diagnosed and may heal without intervention.[17]
If granulation tissue grows over the injured site, it can cause a stenosis, a narrowing of the airway, after a week to a month.[3] The granulation tissue must be surgically excised.[16] People with a narrowed airway may suffer dyspnea, coughing, wheezing, respiratory infections, and difficulty with clearing secretions.[9] If the bronchiole is completely obstructed, atelectasis occurs: the alveoli of the lung collapse.[3] Lung tissue distal to a completely obstructed bronchiole often does not become infected because it is filled with mucus; this tissue remains functional.[10] When the secretions are removed, the lung is commonly able to function almost normally.[17] However, infection is common in lungs distal to a stenosis,[10] and infected lung tissue distal to a stricture can be damaged, and wheezing and coughing may develop due to the narrowing.[8] In addition to pneumonia, the stenosis may cause bronchiectasis, in which bronchi are dilated, to develop.[10] Even after an airway with a stricture is widened back out, the resulting loss of lung function may remain.[10]
Complications may also occur with treatment; for example a granuloma can form at the suture site.[2] Also, the sutured wound can tear again, as occurs when there is excessive pressure in the airways from ventilation.[2] However, for people who do receive surgery soon after the injury to repair the lesion, outcome is usually good; the long-term outcome is good for over 90% of people who have tracheobronchial tears surgically repaired early in treatment.[9] Even when surgery is performed years after the injury, the outlook is good, with low rates of death and disability and good chances of preserving lung function.[17]
Epidemiology
Rupture of the trachea or bronchus is the most common type of blunt injury to the airway.[10] It is difficult to determine the incidence of TBI because in as many as 30–80% of cases, death occurs before the person reaches a hospital, and these people may not be included in studies.[6] On the other hand, some TBIs are so small that they do not cause significant symptoms and are therefore never noticed.[17] In addition, the injury sometimes is not associated with symptoms until complications develop later, further hindering estimation of the true incidence.[5] However, autopsy studies have revealed TBI in 2.5–3.2% of people who died after trauma.[6] Of all neck and chest traumas, including people that died immediately, TBI is estimated to occur in 0.5–2%.[17] An estimated 0.5% of polytrauma patients treated in trauma centers have TBI.[9] The incidence is estimated at 2% in blunt chest and neck trauma and 1–2% in penetrating chest trauma.[9] Laryngotracheal injuries occur in 8% of patients with penetrating injury to the neck, and TBI occurs in 2.8% of blunt chest trauma deaths.[5] In people with blunt trauma who do reach a hospital alive, reports have found incidences of 2.1% and 5.3%.[2] Another study of blunt chest trauma revealed an incidence of only 0.3%, but a mortality rate of 67% (possibly due in part to associated injuries).[5]
The death rate (mortality) for people who reach a hospital alive is about 30%.[2] The number of people reaching a hospital alive has increased, perhaps due to improved prehospital care or specialized treatment centers.[9] Of those who reach the hospital alive but then die, most do so within the first two hours of arrival.[12] The sooner a TBI is diagnosed, the higher the mortality rate; this is likely because of other accompanying injuries that prove fatal.[10]
Associated injuries
Accompanying injuries often play a key role in the outcome.[9] Injuries that may accompany TBI include pulmonary contusion and laceration; and fractures of the sternum, ribs and clavicles.[2] Spinal cord injury, facial trauma, traumatic aortic injury, injuries to the abdomen, lung, and head are present in 40–100% of the time.[7] The most common accompanying injury is esophageal injury, which occurs in as many as 43% of the penetrating injuries to the neck that cause tracheal injury.[5]
History
Throughout most of history the mortality rate of TBI was thought to be 100%.[4] However, in 1871 a healed TBI was noted in a duck that had been killed by a hunter, thus demonstrating that the injury could be survived, at least in the general sense.[5] This report, made by Winslow, was the first record in the medical literature of a bronchus injury.[10] In 1873, Seuvre made one of the earliest reports of TBI in the medical literature: a 74-year-old woman whose chest was crushed by a wagon wheel was found on autopsy to have an avulsion of the right bronchus.[10] Long-term survival of the injury was unknown in humans until 1927, when a report was made of a person who survived.[4][5] In 1931, a report made by Nissen described successful removal of a lung in a 12-year-old girl who had had narrowing of the bronchus due to the injury.[10] Repair of TBI was probably first attempted in 1945, when the first documented case of a successful suturing of a lacerated bronchus was made.[5] Prior to 1950, the mortality rate was 36%; it had fallen to 9% by 2001.[10]
References
- Riley RD, Miller PR, Meredith JW (2004). "Injury to the esophagus, trachea, and bronchus". In Moore EJ, Feliciano DV, Mattox KL. Trauma. New York: McGraw-Hill, Medical Pub. Division. pp. 544–52. ISBN 0-07-137069-2. Retrieved 2008-06-15.
Notes
- ↑ 1.0 1.1 1.2 Le Guen M, Beigelman C, Bouhemad B, Wenjïe Y, Marmion F, Rouby JJ (2007). "Chest computed tomography with multiplanar reformatted images for diagnosing traumatic bronchial rupture: A case report". Crit Care. 11 (5): R94. doi:10.1186/cc6109. PMID 17767714.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 2.19 2.20 2.21 2.22 2.23 2.24
Chu CP, Chen PP (2002). "Tracheobronchial injury secondary to blunt chest trauma: Diagnosis and management". Anaesth Intensive Care. 30 (2): 145–52. PMID 12002920. Unknown parameter
|month=ignored (help) - ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 Stark P (1995). "Imaging of tracheobronchial injuries". J Thorac Imaging. 10 (3): 206-19. PMID 7674433.
- ↑ 4.0 4.1 4.2 4.3 4.4
Barmada H, Gibbons JR (1994). "Tracheobronchial injury in blunt and penetrating chest trauma" (pdf). Chest. 106 (1): 74–8. PMID 8020323. Unknown parameter
|month=ignored (help) - ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 5.12 5.13 5.14 5.15 5.16 5.17 5.18 5.19 5.20 Riley et al. (2004). pp. 544–7.
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 6.11 6.12 6.13 6.14 6.15 6.16 Johnson SB (2008). "Tracheobronchial injury". Seminars in Thoracic and Cardiovascular Surgery. 20 (1): 52&ndash, 57. doi:10.1053/j.semtcvs.2007.09.001. PMID 18420127.
- ↑ 7.00 7.01 7.02 7.03 7.04 7.05 7.06 7.07 7.08 7.09 7.10 7.11 7.12
Euathrongchit J, Thoongsuwan N, Stern EJ (2006). "Nonvascular mediastinal trauma". Radiol Clin North Am. 44 (2): 251–8, viii. doi:10.1016/j.rcl.2005.10.001. PMID 16500207. Unknown parameter
|month=ignored (help) - ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6
Smith M, Ball V (1998). Cardiovascular/respiratory physiotherapy. St. Louis: Mosby. p. 217. ISBN 0-7234-2595-7. Retrieved 2008-06-12. Unknown parameter
|Chapter=ignored (|chapter=suggested) (help) - ↑ 9.00 9.01 9.02 9.03 9.04 9.05 9.06 9.07 9.08 9.09 9.10 9.11 9.12 9.13 9.14 9.15 9.16 9.17 9.18 9.19 9.20 9.21 9.22
Karmy-Jones R, Wood DE (2007). "Traumatic injury to the trachea and bronchus". Thorac Surg Clin. 17 (1): 35–46. doi:10.1016/j.thorsurg.2007.03.005. PMID 17650695. Unknown parameter
|month=ignored (help) - ↑ 10.00 10.01 10.02 10.03 10.04 10.05 10.06 10.07 10.08 10.09 10.10 10.11 10.12 10.13 10.14 10.15 10.16 10.17 10.18
Kiser AC, O'Brien SM, Detterbeck FC (2001). "Blunt tracheobronchial injuries: treatment and outcomes". Ann Thorac Surg. 71 (6): 2059–65. doi:10.1016/S0003-4975(00)02453-X. PMID 11426809. Unknown parameter
|month=ignored (help) - ↑ 11.0 11.1
Rico FR, Cheng JD, Gestring ML, Piotrowski ES (2007). "Mechanical ventilation strategies in massive chest trauma". Crit Care Clin. 23 (2): 299–315, xi. doi:10.1016/j.ccc.2006.12.007. PMID 17368173. Unknown parameter
|month=ignored (help) - ↑ 12.0 12.1 12.2 Nakayama DK, Rowe MI (1988). "Intrathoracic tracheobronchial injuries in childhood". Int Anesthesiol Clin. 26 (1): 42–9. PMID 3283046.
- ↑ 13.0 13.1 13.2 13.3 Hwang JCF, Hanowell LH, Grande CM (1996). "Peri-operative concerns in thoracic trauma". Baillière's Clinical Anaesthesiology. 10 (1): 123–153. doi:10.1016/S0950-3501(96)80009-2.
- ↑ Atluri P, Karakousis GC, Porrett PM, Kaiser LR (2005). The Surgical Review: An Integrated Basic and Clinical Science Study Guide. Hagerstown, MD: Lippincott Williams & Wilkins. ISBN 0-7817-5641-3.
- ↑ 15.0 15.1 Paidas CN. (September 15, 2006) "Thoracic Trauma". Template:Emedicine Retrieved on June 13, 2007.
- ↑ 16.0 16.1 16.2 16.3 16.4 Riley et al. (2004). pp. 548–9.
- ↑ 17.0 17.1 17.2 17.3 17.4 17.5 17.6 17.7 Glazer ES, Meyerson SL (2008). "Delayed presentation and treatment of tracheobronchial injuries due to blunt trauma". J Surg Educ. 65 (4): 302–8. doi:10.1016/j.jsurg.2008.06.006. PMID 18707665.