Sofosbuvir / velpatasvir
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Yashasvi Aryaputra[2];
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
RISK OF HEPATITIS B VIRUS REACTIVATION IN PATIENTS CO-INFECTED WITH HCV AND HBV
See full prescribing information for complete Boxed Warning.
*Test all patients for evidence of current or prior hepatitis B virus (HBV) infection before initiating treatment with Sofosbuvir/Velpatasvir. HBV reactivation has been reported in HCV/HBV coinfected patients who were undergoing or had completed treatment with HCV direct acting antivirals and were not receiving HBV antiviral therapy. Some cases have resulted in fulminant hepatitis, hepatic failure, and death. Monitor HCV/HBV coinfected patients for hepatitis flare or HBV reactivation during HCV treatment and post-treatment follow-up. Initiate appropriate patient management for HBV infection as clinically indicated.
|
Overview
Sofosbuvir / velpatasvir is a fixed-dose combination of Sofosbuvir, a hepatitis C virus (HCV) nucleotide analog NS5B polymerase inhibitor, and Velpatasvir, an HCV NS5A inhibitor that is FDA approved for the treatment of adult patients with chronic HCV genotype 1, 2, 3, 4, 5, or 6 infection (1) without cirrhosis or with compensated cirrhosis or with decompensated cirrhosis for use in combination with ribavirin. There is a Black Box Warning for this drug as shown here. Common adverse reactions include fatigue, anemia, nausea, headache, insomnia, and diarrhea.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indications:
- Sofosbuvir/Velpatasvir is indicated for the treatment of adult patients with chronic hepatitis C virus (HCV) genotype 1, 2, 3, 4, 5, or 6 infection:
- without cirrhosis or with compensated cirrhosis.
- with decompensated cirrhosis for use in combination with ribavirin.
Recommended Dosage:
- The recommended dosage of Sofosbuvir/Velpatasvir is one tablet taken orally once daily with or without food. One tablet of Sofosbuvir/Velpatasvir contains 400 mg of Sofosbuvir and 100 mg of Velpatasvir. Table 1 shows the recommended treatment regimen and duration based on patient population.
- For patients with HCV/HIV-1 coinfection, follow the dosage recommendations in Table 1. Refer to Drug Interactions (7) for dosage recommendations for concomitant HIV-1 antiviral drugs.
No Dosage Recommendations in Severe Renal Impairment and End Stage Renal Disease
- No dosage recommendation can be given for patients with severe renal impairment (estimated Glomerular Filtration Rate [eGFR] less than 30 mL/min/1.73 m2) or with end stage renal disease (ESRD), due to higher exposures (up to 20-fold) of the predominant Sofosbuvir metabolite.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Sofosbuvir/Velpatasvir Off-Label Guideline-Supported Use and Dosage (Adult) in the drug label.
Non–Guideline-Supported Use
There is limited information regarding Sofosbuvir/Velpatasvir Off-Label Non-Guideline-Supported Use and Dosage (Adult) in the drug label.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding Sofosbuvir / velpatasvir FDA-Labeled Indications and Dosage (Pediatric) in the drug label.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Sofosbuvir/Velpatasvir Off-Label Guideline-Supported Use and Dosage (Pediatric) in the drug label.
Non–Guideline-Supported Use
There is limited information regarding Sofosbuvir/Velpatasvir Off-Label Non-Guideline-Supported Use and Dosage (Pediatric) in the drug label.
Contraindications
- Sofosbuvir/Velpatasvir and ribavirin combination regimen is contraindicated in patients for whom ribavirin is contraindicated. Refer to the ribavirin prescribing information for a list of contraindications for ribavirin.
Warnings
|
RISK OF HEPATITIS B VIRUS REACTIVATION IN PATIENTS CO-INFECTED WITH HCV AND HBV
See full prescribing information for complete Boxed Warning.
*Test all patients for evidence of current or prior hepatitis B virus (HBV) infection before initiating treatment with Sofosbuvir/Velpatasvir. HBV reactivation has been reported in HCV/HBV coinfected patients who were undergoing or had completed treatment with HCV direct acting antivirals and were not receiving HBV antiviral therapy. Some cases have resulted in fulminant hepatitis, hepatic failure, and death. Monitor HCV/HBV coinfected patients for hepatitis flare or HBV reactivation during HCV treatment and post-treatment follow-up. Initiate appropriate patient management for HBV infection as clinically indicated.
|
Risk of Hepatitis B Virus Reactivation in Patients Coinfected with HCV and HBV
- Hepatitis B virus (HBV) reactivation has been reported in HCV/HBV coinfected patients who were undergoing or had completed treatment with HCV direct acting antivirals, and who were not receiving HBV antiviral therapy. Some cases have resulted in fulminant hepatitis, hepatic failure, and death. Cases have been reported in patients who are HBsAg positive and also in patients with serologic evidence of resolved HBV infection (i.e., HBsAg negative and anti-HBc positive). HBV reactivation has also been reported in patients receiving certain immunosuppressants or chemotherapeutic agents; the risk of HBV reactivation associated with treatment with HCV direct-acting antivirals may be increased in these patients.
- HBV reactivation is characterized as an abrupt increase in HBV replication manifesting as a rapid increase in serum HBV DNA level. In patients with resolved HBV infection, reappearance of HBsAg can occur. Reactivation of HBV replication may be accompanied by hepatitis, i.e., increases in aminotransferase levels and, in severe cases, increases in bilirubin levels, liver failure, and death can occur.
- Test all patients for evidence of current or prior HBV infection by measuring HBsAg and anti-HBc before initiating HCV treatment with Sofosbuvir/Velpatasvir. In patients with serologic evidence of HBV infection, monitor for clinical and laboratory signs of hepatitis flare or HBV reactivation during HCV treatment with Sofosbuvir/Velpatasvir and during post-treatment follow-up. Initiate appropriate patient management for HBV infection as clinically indicated.
Serious Symptomatic Bradycardia When Coadministered with Amiodarone
- Postmarketing cases of symptomatic bradycardia and cases requiring pacemaker intervention have been reported when amiodarone is coadministered with a Sofosbuvir containing regimen. A fatal cardiac arrest was reported in a patient taking amiodarone who was coadministered a Sofosbuvir-containing regimen. Bradycardia has generally occurred within hours to days, but cases have been observed up to 2 weeks after initiating HCV treatment. Patients also taking beta blockers, or those with underlying cardiac comorbidities and/or advanced liver disease may be at increased risk for symptomatic bradycardia with coadministration of amiodarone. Bradycardia generally resolved after discontinuation of HCV treatment. The mechanism for this effect is unknown.
- Coadministration of amiodarone with Sofosbuvir/Velpatasvir is not recommended. For patients taking amiodarone who have no other alternative viable treatment options and who will be coadministered Sofosbuvir/Velpatasvir:
- Counsel patients about the risk of symptomatic bradycardia.
- Cardiac monitoring in an in-patient setting for the first 48 hours of coadministration is recommended, after which outpatient or self-monitoring of the heart rate should occur on a daily basis through at least the first 2 weeks of treatment.
- Patients who are taking Sofosbuvir/Velpatasvir who need to start amiodarone therapy due to no other alternative viable treatment options should undergo similar cardiac monitoring as outlined above.
- Due to amiodarone’s long half-life, patients discontinuing amiodarone just prior to starting Sofosbuvir/Velpatasvir should also undergo similar cardiac monitoring as outlined above.
- Patients who develop signs or symptoms of bradycardia should seek medical evaluation immediately. Symptoms may include near-fainting or fainting, dizziness or lightheadedness, malaise, weakness, excessive tiredness, shortness of breath, chest pains, confusion, or memory problems.
Risk of Reduced Therapeutic Effect Due to Concomitant Use of Sofosbuvir/Velpatasvir with Inducers of P-gp and/or Moderate to Potent Inducers of CYP
- Drugs that are inducers of P-gp and/or moderate to potent inducers of CYP2B6, CYP2C8, or CYP3A4 (e.g., rifampin, St. John’s wort, carbamazepine) may significantly decrease plasma concentrations of Sofosbuvir and/or Velpatasvir, leading to potentially reduced therapeutic effect of Sofosbuvir/Velpatasvir. The use of these agents with Sofosbuvir/Velpatasvir is not recommended.
Risks Associated with Ribavirin and Sofosbuvir/Velpatasvir Combination Treatment
- If Sofosbuvir/Velpatasvir is administered with ribavirin, the warnings and precautions for ribavirin apply to this combination regimen. Refer to the ribavirin prescribing information for a full list of the warnings and precautions for ribavirin.
Adverse Reactions
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
- If Sofosbuvir/Velpatasvir is administered with ribavirin, refer to the prescribing information for ribavirin for a description of ribavirin-associated adverse reactions.
Adverse Reactions in Subjects without Cirrhosis or with Compensated Cirrhosis
- The adverse reactions data for Sofosbuvir/Velpatasvir in patients without cirrhosis or with compensated cirrhosis were derived from three Phase 3 clinical trials (ASTRAL-1, ASTRAL-2, and ASTRAL-3) which evaluated a total of 1035 subjects infected with genotype 1, 2, 3, 4, 5, or 6 HCV, without cirrhosis or with compensated cirrhosis, who received Sofosbuvir/Velpatasvir for 12 weeks. Sofosbuvir/Velpatasvir was studied in placebo- and activecontrolled trials.
- The proportion of subjects who permanently discontinued treatment due to adverse events was 0.2% for subjects who received Sofosbuvir/Velpatasvir for 12 weeks.
- The most common adverse reactions (adverse events assessed as causally related by the investigator and at least 10%) were headache and fatigue in subjects treated with Sofosbuvir/Velpatasvir for 12 weeks.
- Adverse reactions, all grades, observed in greater than or equal to 5% of subjects receiving 12 weeks of treatment with Sofosbuvir/Velpatasvir in ASTRAL-1 include headache (22%), fatigue (15%), nausea (9%), asthenia (5%), and insomnia (5%). Of subjects receiving Sofosbuvir/Velpatasvir who experienced these adverse reactions, 79% had an adverse reaction of mild severity (Grade 1). With the exception of asthenia, each of these adverse reactions occurred at a similar frequency or more frequently in subjects treated with placebo compared to subjects treated with Sofosbuvir/Velpatasvir (asthenia: 3% versus 5% for the placebo and Sofosbuvir/Velpatasvir groups, respectively).
- The adverse reactions observed in subjects treated with Sofosbuvir/Velpatasvir in ASTRAL-2 and ASTRAL-3 were consistent with those observed in ASTRAL-1. Irritability was also observed in greater than or equal to 5% of subjects treated with Sofosbuvir/Velpatasvir in ASTRAL-3.
Adverse Reactions in Subjects Coinfected with HCV and HIV-1
- The safety assessment of Sofosbuvir/Velpatasvir in subjects with HCV/HIV-1 coinfection was based on an open-label clinical trial (ASTRAL-5) in 106 subjects who were on stable antiretroviral therapy. The safety profile in HCV/HIV-1 coinfected subjects was similar to that observed in HCV mono-infected subjects. The most common adverse reactions occurring in at least 10% of subjects were fatigue (22%) and headache (10%).
Adverse Reactions in Subjects with Decompensated Cirrhosis
- The safety assessment of Sofosbuvir/Velpatasvir in subjects infected with genotype 1, 2, 3, 4, or 6 HCV with decompensated cirrhosis was based on one Phase 3 trial (ASTRAL-4) including 87 subjects who received Sofosbuvir/Velpatasvir with ribavirin for 12 weeks. All 87 subjects had Child-Pugh B cirrhosis at screening. On the first day of treatment with Sofosbuvir/Velpatasvir with ribavirin, 6 subjects and 4 subjects were assessed to have Child-Pugh A and Child-Pugh C cirrhosis, respectively.
- The most common adverse reactions (adverse events assessed as causally related by the investigator, all grades with frequency of 10% or greater) in the 87 subjects who
received Sofosbuvir/Velpatasvir with ribavirin for 12 weeks were fatigue (32%), anemia (26%), nausea (15%), headache (11%), insomnia (11%), and diarrhea (10%). Of subjects who experienced these adverse reactions, 98% had adverse reactions of mild to moderate severity.
- A total of 4 (5%) subjects permanently discontinued Sofosbuvir/Velpatasvir with ribavirin due to an adverse event; there was no adverse event leading to discontinuation that occurred in more than 1 subject.
- Decreases in hemoglobin to less than 10 g/dL and 8.5 g/dL during treatment were observed in 23% and 7% of subjects treated with Sofosbuvir/Velpatasvir with ribavirin for 12 weeks, respectively. Ribavirin was permanently discontinued in 17% of subjects treated with Sofosbuvir/Velpatasvir with ribavirin for 12 weeks, due to adverse reactions.
Less Common Adverse Reactions Reported in Clinical Trials
- The following adverse reactions occurred in less than 5% of subjects without cirrhosis or with compensated cirrhosis treated with Sofosbuvir/Velpatasvir for 12 weeks and are included because of a potential causal relationship.
- Rash: In the ASTRAL-1 study, rash occurred in 2% of subjects treated with Sofosbuvir/Velpatasvir and in 1% of subjects treated with placebo. No serious adverse reactions of rash occurred and all rashes were mild or moderate in severity.
- Depression: In the ASTRAL-1 study, depressed mood occurred in 1% of subjects treated with Sofosbuvir/Velpatasvir and was not reported by any subject taking placebo. No serious adverse reactions of depressed mood occurred and all events were mild or moderate in severity.
- The following adverse reactions occurred in less than 10% of subjects with decompensated cirrhosis (ASTRAL-4) treated with Sofosbuvir/Velpatasvir with ribavirin for 12 weeks and are included because of a potential causal relationship.
- Rash: Rash occurred in 5% of subjects treated with Sofosbuvir/Velpatasvir with ribavirin. No serious adverse reactions of rash occurred and all rashes were mild or moderate in severity.
Laboratory Abnormalities
- Lipase Elevations: In ASTRAL-1, isolated, asymptomatic lipase elevations of greater than 3xULN were observed in 3% and 1% of subjects treated with Sofosbuvir/Velpatasvir and placebo for 12 weeks, respectively; and in 6% and 3% of subjects treated with Sofosbuvir/Velpatasvir in ASTRAL-2 and ASTRAL-3, respectively.
- In the Phase 3 trial of subjects with decompensated cirrhosis (ASTRAL-4), lipase was assessed when amylase values were greater than or equal to 1.5xULN. Isolated, asymptomatic lipase elevations of greater than 3xULN were observed in 2% of subjects treated with Sofosbuvir/Velpatasvir with ribavirin for 12 weeks.
- Creatine Kinase: In ASTRAL-1, isolated, asymptomatic creatine kinase elevations greater than or equal to 10xULN were reported in 1% and 0% of subjects treated with Sofosbuvir/Velpatasvir and placebo for 12 weeks, respectively; and in 2% and 1% of subjects treated with Sofosbuvir/Velpatasvir in ASTRAL-2 and ASTRAL-3, respectively.
- In the Phase 3 trial with decompensated cirrhosis (ASTRAL-4), isolated, asymptomatic creatine kinase elevations greater than or equal to 10xULN were reported in 1% of subjects treated with Sofosbuvir/Velpatasvir with ribavirin for 12 weeks.
- Indirect Bilirubin: Increases in indirect bilirubin up to 3 mg/dL above baseline were noted among HIV-1/HCV coinfected subjects treated with Sofosbuvir/Velpatasvir and an atazanavir/ritonavir-based antiretroviral regimen. The elevated indirect bilirubin values were not associated with clinical adverse events and all subjects completed 12 weeks of Sofosbuvir/Velpatasvir without dose adjustment or treatment interruption of either Sofosbuvir/Velpatasvir or HIV antiretroviral agents.
Postmarketing Experience
- The following adverse reactions have been identified during post approval use of Sofosbuvir. Because postmarketing reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Cardiac Disorders
- Serious symptomatic bradycardia has been reported in patients taking amiodarone who initiate treatment with a Sofosbuvir-containing regimen.
Skin and Subcutaneous Tissue Disorders
- Skin rashes, sometimes with blisters or angioedema-like swelling Angioedema.
Drug Interactions
- Potential for Other Drugs to Affect Sofosbuvir/Velpatasvir
- Potential for Sofosbuvir/Velpatasvir to Affect Other Drugs
- Established and Potentially Significant Drug Interactions
- Drugs without Clinically Significant Interactions with Sofosbuvir/Velpatasvir
Potential for Other Drugs to Affect Sofosbuvir/Velpatasvir
- Sofosbuvir and Velpatasvir are substrates of drug transporters P-gp and BCRP while GS-331007 (the predominant circulating metabolite of Sofosbuvir) is not. In vitro, slow metabolic turnover of Velpatasvir by CYP2B6, CYP2C8, and CYP3A4 was observed.
- Drugs that are inducers of P-gp and/or moderate to potent inducers of CYP2B6, CYP2C8, or CYP3A4 (e.g., rifampin, St. John’s wort, carbamazepine) may decrease plasma concentrations of Sofosbuvir and/or Velpatasvir, leading to reduced therapeutic effect of Sofosbuvir/Velpatasvir. The use of these agents with Sofosbuvir/Velpatasvir is not recommended. Sofosbuvir/Velpatasvir may be coadministered with P-gp, BCRP, and CYP inhibitors.
Potential for Sofosbuvir/Velpatasvir to Affect Other Drugs
- Velpatasvir is an inhibitor of drug transporters P-gp, breast cancer resistance protein (BCRP), OATP1B1, OATP1B3, and OATP2B1. Coadministration of Sofosbuvir/Velpatasvir with drugs that are substrates of these transporters may increase the exposure of such drugs.
Established and Potentially Significant Drug Interactions
- Table 2 provides a listing of established or potentially clinically significant drug interactions. The drug interactions described are based on studies conducted with either Sofosbuvir/Velpatasvir, the components of Sofosbuvir/Velpatasvir as individual agents, or are predicted drug interactions that may occur with Sofosbuvir/Velpatasvir.
Drugs without Clinically Significant Interactions with Sofosbuvir/Velpatasvir
- Based on drug interaction studies conducted with the components of Sofosbuvir/Velpatasvir or Sofosbuvir/Velpatasvir, no clinically significant drug interactions have been observed with the following drugs:
- Sofosbuvir/Velpatasvir: atazanavir/ritonavir, cyclosporine, darunavir/ritonavir, dolutegravir, elvitegravir/cobicistat/emtricitabine/tenofovir alafenamide, emtricitabine, raltegravir, or rilpivirine.
- Sofosbuvir: ethinyl estradiol/norgestimate, methadone, or tacrolimus.
- Velpatasvir: ethinyl estradiol/norgestimate, ketoconazole, or pravastatin. See Table 2 for use of Sofosbuvir/Velpatasvir with certain HIV antiretroviral regimens.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): Risk Summary
- If Sofosbuvir/Velpatasvir is administered with ribavirin, the combination regimen is contraindicated in pregnant women and in men whose female partners are pregnant. Refer to the ribavirin prescribing information for more information on ribavirin-associated risks of use during pregnancy.
- No adequate human data are available to establish whether or not Sofosbuvir/Velpatasvir poses a risk to pregnancy outcomes. In animal reproduction studies, no evidence of adverse developmental outcomes was observed with the components of Sofosbuvir/Velpatasvir at exposures greater than those in humans at the recommended human dose (RHD). During organogenesis in the mouse, rat, and rabbit, systemic exposures (AUC) to Velpatasvir were approximately 31 (mice), 6 (rats), and 0.4 (rabbits) times the exposure in humans at the RHD, while exposures to the predominant circulating metabolite of Sofosbuvir (GS-331007) were approximately 4 (rats) and 10 (rabbits) times the exposure in humans at the RHD. In rat pre/postnatal development studies, maternal systemic exposures (AUC) to Velpatasvir and GS-331007 were approximately 5 times the exposures of each component in humans at the RHD.
- The background risk of major birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2–4% and 15–20%, respectively.
Data
- Sofosbuvir: Sofosbuvir was administered orally to pregnant rats (up to 500 mg/kg/day) and rabbits (up to 300 mg/kg/day) on gestation days 6 to 18 and 6 to 19, respectively, and also to rats (oral doses up to 500 mg/kg/day) on gestation day 6 to lactation/postpartum day 20. No significant effects on embryo-fetal (rats and rabbits) or pre/postnatal (rats) development were observed at the highest doses tested. The systemic exposures (AUC) of the predominant circulating metabolite of Sofosbuvir (GS-331007) during gestation were approximately 4 (rats) and 10 (rabbits) times the exposure in humans at the RHD.
- Velpatasvir: Velpatasvir was administered orally to pregnant mice (up to 1000 mg/kg/day), rats (up to 200 mg/kg/day) and rabbits (up to 300 mg/kg/day) on gestation days 6 to 15, 6 to 17, and 7 to 20, respectively, and also to rats (oral doses up to 200 mg/kg) on gestation day 6 to lactation/post-partum day 20. No significant effects on embryo-fetal (mice, rats, and rabbits) or pre/postnatal (rats) development were observed at the highest doses tested. The systemic exposures (AUC) of Velpatasvir during gestation were approximately 31 (mice), 6 (rats), and 0.4 (rabbits) times the exposure in humans at the RHD.
Risk Summary
- It is not known whether the components of Sofosbuvir/Velpatasvir and its metabolites are present in human breast milk, affect human milk production, or have effects on the breastfed infant. The predominant circulating metabolite of Sofosbuvir (GS-331007) was the primary component observed in the milk of lactating rats administered Sofosbuvir, without effect on nursing pups. When administered to lactating rats, Velpatasvir was detected in the milk of lactating rats and in the plasma of nursing pups without effects on the nursing pups.
- The development and health benefits of breastfeeding should be considered along with the mother’s clinical need for Sofosbuvir/Velpatasvir and any potential adverse effects on the breastfed child from Sofosbuvir/Velpatasvir or from the underlying maternal condition.
- If Sofosbuvir/Velpatasvir is administered with ribavirin, the nursing mother’s information for ribavirin also applies to this combination regimen. Refer to the ribavirin prescribing information for more information on use during lactation.
Data
- Sofosbuvir: No effects of Sofosbuvir on growth and postnatal development were observed in nursing pups at the highest dose tested in rats. Maternal systemic exposure (AUC) to the predominant circulating metabolite of Sofosbuvir (GS-331007) was approximately 5 times the exposure in humans at the RHD, with exposure of approximately 2% that of maternal exposure observed in nursing pups on lactation day 10. In a lactation study, Sofosbuvir metabolites (primarily GS-331007) were excreted into the milk of lactating rats following administration of a single oral dose of Sofosbuvir (20 mg/kg) on lactation day 2, with milk concentrations of approximately 10% that of maternal plasma concentrations observed 1 hour post-dose.
- Velpatasvir: No effects of Velpatasvir on growth and postnatal development were observed in nursing pups at the highest dose tested in rats. Maternal systemic exposure (AUC) to Velpatasvir was approximately 5 times the exposure in humans at the RHD. Velpatasvir was present in the milk (approximately 173% that of maternal plasma concentrations) of lactating rats following a single oral dose of Velpatasvir (30 mg/kg), and systemic exposure (AUC) in nursing pups was approximately 4% that of maternal exposure on lactation day 10.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Sofosbuvir / velpatasvir in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Sofosbuvir / velpatasvir during labor and delivery.
Nursing Mothers
(Description)g
Pediatric Use
- Safety and effectiveness of Sofosbuvir/Velpatasvir have not been established in pediatric patients.
Geriatic Use
- Clinical trials of Sofosbuvir/Velpatasvir included 156 subjects aged 65 and over (12% of total number of subjects in the Phase 3 clinical trials). No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. No dosage adjustment of Sofosbuvir/Velpatasvir is warranted in geriatric patients.
Gender
There is no FDA guidance on the use of Sofosbuvir / velpatasvir with respect to specific gender populations.
Race
There is no FDA guidance on the use of Sofosbuvir / velpatasvir with respect to specific racial populations.
Renal Impairment
- No dosage adjustment of Sofosbuvir/Velpatasvir is required for patients with mild or moderate renal impairment. The safety and efficacy of Sofosbuvir/Velpatasvir have not been established in patients with severe renal impairment (eGFR less than 30 mL/min/1.73 m2) or ESRD requiring hemodialysis. No dosage recommendation can be given for patients with severe renal impairment or ESRD. Refer to ribavirin prescribing information regarding use of ribavirin in patients with renal impairment.
Hepatic Impairment
- No dosage adjustment of Sofosbuvir/Velpatasvir is required for patients with mild, moderate, or severe hepatic impairment (Child-Pugh Class A, B, or C).
- Clinical and hepatic laboratory monitoring (including direct bilirubin), as clinically indicated, is recommended for patients with decompensated cirrhosis receiving treatment with Sofosbuvir/Velpatasvir and ribavirin.
Females of Reproductive Potential and Males
- If Sofosbuvir/Velpatasvir is administered with ribavirin, the information for ribavirin with regard to pregnancy testing, contraception, and infertility also applies to this combination regimen. Refer to ribavirin prescribing information for additional information.
Immunocompromised Patients
There is no FDA guidance one the use of Sofosbuvir / velpatasvir in patients who are immunocompromised.
Administration and Monitoring
Administration
Oral
- Take with or without food.
Monitoring
- Hepatitis C virus genotype: Prior to initiation of therapy.
- Reduction in HCV-RNA viral load and improvement in signs/symptoms of chronic hepatitis C genotype 1 infection may indicate efficacy.
- Hepatitis B virus (HBV) current or prior infection: Prior to initiation.
- Hepatic function; as appropriate in patients with decompensated cirrhosis who are co-administered ribavirin.
- Clinical and laboratory signs of hepatitis flare or HBV reactivation, in patients with evidence or current or prior HBV infection: During treatment and post-treatment follow-up.
IV Compatibility
There is limited information regarding the compatibility of Sofosbuvir / velpatasvir and IV administrations.
Overdosage
- No specific antidote is available for overdose with Sofosbuvir/Velpatasvir. If overdose occurs the patient must be monitored for evidence of toxicity. Treatment of overdose with Sofosbuvir/Velpatasvir consists of general supportive measures including monitoring of vital signs as well as observation of the clinical status of the patient. Hemodialysis can efficiently remove the predominant circulating metabolite of Sofosbuvir, GS-331007, with an extraction ratio of 53%. Hemodialysis is unlikely to result in significant removal of Velpatasvir since Velpatasvir is highly bound to plasma protein.
Pharmacology
Mechanism of Action
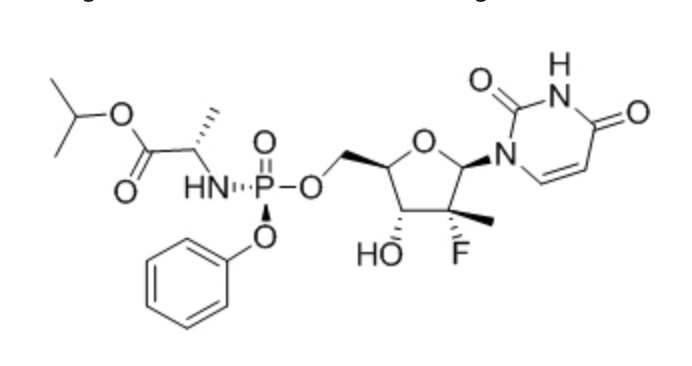
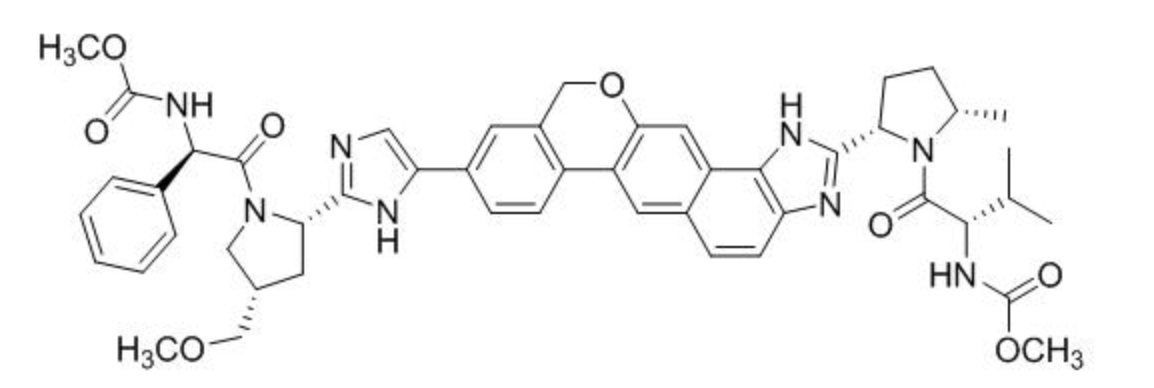
- Sofosbuvir/Velpatasvir is a fixed-dose combination of Sofosbuvir and Velpatasvir which are directacting antiviral agents against the hepatitis C virus.
Structure
Pharmacodynamics
Cardiac Electrophysiology
- The effect of Sofosbuvir 400 mg (recommended dosage) and 1200 mg (3 times the recommended dosage) on QTc interval was evaluated in an active-controlled (moxifloxacin 400 mg) thorough QT trial. At a dose 3 times the recommended dose, Sofosbuvir does not prolong QTc to any clinically relevant extent.
- The effect of Velpatasvir 500 mg (5 times the recommended dosage) was evaluated in an active-controlled (moxifloxacin 400 mg) thorough QT trial. At a dose 5 times the recommended dose, Velpatasvir does not prolong QTc interval to any clinically relevant extent.
Pharmacokinetics
- The pharmacokinetic properties of the components of Sofosbuvir/Velpatasvir are provided in Table 3. The multiple dose pharmacokinetic parameters of Sofosbuvir and its metabolite, GS-331007, and Velpatasvir are provided in Table 4.
- Sofosbuvir and GS-331007 AUC0-24 and Cmax were similar in healthy adult subjects and subjects with HCV infection. Relative to healthy subjects (N=331), Velpatasvir AUC0-24 and Cmax were 37% lower and 42% lower, respectively, in HCV-infected subjects.
- Velpatasvir AUC increases in a greater than proportional manner from 5 to 50 mg and in a less than proportional manner from 50 to 450 mg in healthy volunteers. However, Velpatasvir exhibited more than or near dose-proportional increase in exposures 25 mg to 150 mg in HCV-infected patients when coadministered with Sofosbuvir. Sofosbuvir and GS-331007 AUCs are near dose-proportional over the dose range of 200 mg to 1200 mg.
Specific Populations
- Pediatric Patients: The pharmacokinetics of Sofosbuvir or Velpatasvir in pediatric patients has not been established.
- Geriatric Patients: Population pharmacokinetic analysis in HCV-infected subjects showed that within the age range (18 to 82 years) analyzed, age did not have a clinically relevant effect on the exposure to Sofosbuvir, GS-331007, or Velpatasvir.
- Patients with Renal Impairment: The pharmacokinetics of Sofosbuvir were studied in HCV negative subjects with mild (eGFR between 50 to less than 80 mL/min/1.73 m2 ), moderate (eGFR between 30 to less than 50 mL/min/1.73 m2 ), severe renal impairment (eGFR less than 30 mL/min/1.73 m2 ), and subjects with ESRD requiring hemodialysis following a single 400 mg dose of Sofosbuvir. Relative to subjects with normal renal function (eGFR greater than 80 mL/min/1.73 m2 ), the Sofosbuvir AUC0-inf was 61%,
107%, and 171% higher in subjects with mild, moderate, and severe renal impairment, while the GS-331007 AUC0-inf was 55%, 88%, and 451% higher, respectively.
- In subjects with ESRD, relative to subjects with normal renal function, Sofosbuvir and GS-331007 AUC0-inf was 28% and 1280% higher when Sofosbuvir was dosed 1 hour before hemodialysis compared with 60% and 2070% higher when Sofosbuvir was dosed 1 hour after hemodialysis, respectively. A 4 hour hemodialysis session removed approximately 18% of administered dose.
- The pharmacokinetics of Velpatasvir were studied with a single dose of 100 mg Velpatasvir in HCV negative subjects with severe renal impairment (eGFR less than 30 mL/min by Cockcroft-Gault). No clinically relevant differences in Velpatasvir pharmacokinetics were observed between healthy subjects and subjects with severe renal impairment.
- Patients with Hepatic Impairment: The pharmacokinetics of Sofosbuvir were studied following 7-day dosing of 400 mg Sofosbuvir in HCV-infected subjects with moderate and severe hepatic impairment (Child-Pugh Class B and C, respectively). Relative to subjects with normal hepatic function, the Sofosbuvir AUC0-24 were 126% and 143% higher in moderate and severe hepatic impairment, while the GS-331007 AUC0-24 were 18% and 9% higher, respectively. Population pharmacokinetics analysis in HCV-infected subjects indicated that cirrhosis (including decompensated cirrhosis) had no clinically relevant effect on the exposure of Sofosbuvir and GS-331007.
- The pharmacokinetics of Velpatasvir were studied with a single dose of 100 mg Velpatasvir in HCV negative subjects with moderate and severe hepatic impairment (Child-Pugh Class B and C). Velpatasvir plasma exposure (AUCinf) was similar in subjects with moderate hepatic impairment, severe hepatic impairment, and control subjects with normal hepatic function. Population pharmacokinetics analysis in HCVinfected subjects indicated that cirrhosis (including decompensated cirrhosis) had no clinically relevant effect on the exposure of Velpatasvir.
- Race: Population pharmacokinetics analysis in HCV-infected subjects indicated that race had no clinically relevant effect on the exposure of Sofosbuvir, GS-331007, or Velpatasvir.
- Gender: Population pharmacokinetics analysis in HCV-infected subjects indicated that gender had no clinically relevant effect on the exposure of Sofosbuvir, GS-331007, or Velpatasvir.
Drug Interaction Studies
- After oral administration of Sofosbuvir/Velpatasvir, Sofosbuvir is rapidly absorbed and subject to extensive first-pass hepatic extraction (hydrolysis followed by sequential phosphorylation) to form the pharmacologically active triphosphate. In clinical pharmacology studies, both Sofosbuvir and the primary circulating metabolite GS-331007 (dephosphorylated nucleotide metabolite) were monitored for purposes of pharmacokinetic analyses.
- Sofosbuvir and Velpatasvir are substrates of drug transporters P-gp and BCRP while GS-331007 is not. Velpatasvir is also transported by OATP1B1 and OATP1B3. In vitro, slow metabolic turnover of Velpatasvir by CYP2B6, CYP2C8, and CYP3A4 was observed. Inducers of P-gp and/or moderate to potent inducers of CYP2B6, CYP2C8, or CYP3A4 (e.g., rifampin, St. John’s wort, carbamazepine) may decrease plasma concentrations of Sofosbuvir and/or Velpatasvir, leading to reduced therapeutic effect of Sofosbuvir/Velpatasvir. Coadministration with drugs that inhibit P-gp and/or BCRP may increase Sofosbuvir and/or Velpatasvir plasma concentrations without increasing GS-331007 plasma concentration. Drugs that inhibit CYP2B6, CYP2C8, or CYP3A4 may increase plasma concentration of Velpatasvir.
- Velpatasvir is an inhibitor of drug transporter P-gp, BCRP, OATP1B1, OATP1B3, and OATP2B1, and its involvement in drug interactions with these transporters is primarily limited to the process of absorption. At clinically relevant concentration, Velpatasvir is not an inhibitor of hepatic transporters OATP1A2 or OCT1, renal transporters OCT2, OAT1, OAT3 or MATE1, or CYP or UGT1A1 enzymes.
- Sofosbuvir and GS-331007 are not inhibitors of drug transporters P-gp, BCRP, OATP1B1, OATP1B3, and OCT1 and GS-331007 is not an inhibitor of OAT1, OAT3, OCT2, and MATE1. Sofosbuvir and GS-331007 are not inhibitors or inducers of CYP or UGT1A1 enzymes.
- The effects of coadministered drugs on the exposure of Sofosbuvir, GS-331007, and Velpatasvir are shown in Table 5. The effects of Sofosbuvir/Velpatasvir on the exposure of coadministered drugs are shown in Table 6.
- No effect on the pharmacokinetic parameters of Sofosbuvir, GS-331007, or Velpatasvir was observed with dolutegravir; the combination of emtricitabine, rilpivirine, and tenofovir DF; emtricitabine; raltegravir; or tenofovir DF.
- No effect on the pharmacokinetic parameters of the following coadministered drugs was observed with Sofosbuvir/Velpatasvir (dolutegravir or lopinavir/ritonavir) or its components Sofosbuvir (cyclosporine or methadone) or Velpatasvir (cyclosporine).
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis and Mutagenesis
- Sofosbuvir: Sofosbuvir was not genotoxic in a battery of in vitro or in vivo assays, including bacterial mutagenicity, chromosome aberration using human peripheral blood lymphocytes and in vivo mouse micronucleus assays.
- Sofosbuvir was not carcinogenic in a 2-year mouse study (up to 200 mg/kg/day in males and 600 mg/kg/day in females) and in a 2-year rat study (up to 750 mg/kg/day), resulting in exposures of the predominant circulating metabolite GS-331007 of approximately 3 and 15 times (in mice) and 7 and 9 times (in rats), in males and females, respectively, the exposure in humans at the recommended human dose (RHD).
- Velpatasvir: Velpatasvir was not genotoxic in a battery of in vitro or in vivo assays, including bacterial mutagenicity, chromosome aberration using human peripheral blood lymphocytes, and in vivo rat micronucleus assays.
- Velpatasvir was not carcinogenic in a 6-month rasH2 transgenic mouse study (up to 1000 mg/kg/day). A 2-year rat carcinogenicity study with Velpatasvir is ongoing.
Impairment of Fertility
- Sofosbuvir: Sofosbuvir had no effects on embryo-fetal viability or on fertility when evaluated in rats. At the highest dose tested, AUC exposure to the predominant circulating metabolite GS-331007 was approximately 4 times the exposure in humans at the RHD.
- Velpatasvir: Velpatasvir had no effects on embryo-fetal viability or on fertility when evaluated in rats. At the highest dose tested, Velpatasvir exposure was approximately 6 times the exposure in humans at the RHD.
Clinical Studies
Description of Clinical Trials
- Table 9 presents the clinical trial design including different treatment groups that were conducted with Sofosbuvir/Velpatasvir with and without ribavirin in subjects with chronic hepatitis C (HCV) genotype 1, 2, 3, 4, 5, and 6 infection. For detailed description of trial design and recommended regimen and duration.
- The ribavirin dosage was weight-based (1000 mg daily administered in two divided doses for subjects less than 75 kg and 1200 mg for those greater than or equal to 75 kg) and administered in two divided doses when used in combination with Sofosbuvir in the ASTRAL-2 and ASTRAL-3 trials or in combination with Sofosbuvir/Velpatasvir in the ASTRAL-4 trial. Ribavirin dosage adjustments were performed according to the ribavirin prescribing information. Serum HCV RNA values were measured during the clinical trials using the COBAS AmpliPrep/COBAS Taqman HCV test (version 2.0) with a lower limit of quantification (LLOQ) of 15 IU/mL. Sustained virologic response (SVR12), defined as HCV RNA less than LLOQ at 12 weeks after the cessation of treatment, was the primary endpoint in all the trials. Relapse is defined as HCV RNA greater than or equal to LLOQ during the post treatment period after having achieved HCV RNA less than LLOQ at the end of treatment. On-treatment virologic failure is defined as breakthrough, rebound, or non-response.
Clinical Trials in Subjects without Cirrhosis and Subjects with Compensated Cirrhosis
Genotype 1, 2, 4, 5, and 6 HCV Infected Adults (ASTRAL-1)
- ASTRAL-1 was a randomized, double-blind, placebo-controlled trial that evaluated 12 weeks of treatment with Sofosbuvir/Velpatasvir compared with 12 weeks of placebo in subjects with genotype 1, 2, 4, 5, or 6 HCV infection without cirrhosis or with compensated cirrhosis. Subjects with genotype 1, 2, 4, or 6 HCV infection were randomized in a 5:1 ratio to treatment with Sofosbuvir/Velpatasvir or placebo for 12 weeks. Subjects with genotype 5 HCV infection were enrolled to the Sofosbuvir/Velpatasvir group. Randomization was stratified by HCV genotype (1, 2, 4, 6, and indeterminate) and the presence or absence of compensated cirrhosis.
- Demographics and baseline characteristics were balanced between the Sofosbuvir/Velpatasvir and placebo group. Of the 740 treated subjects, the median age was 56 years (range: 18 to 82); 60% of the subjects were male; 79% were White, 9% were Black; 21% had a baseline body mass index at least 30 kg/m2 ; the proportions of subjects with genotype
1, 2, 4, 5, or 6 HCV infection were 53%, 17%, 19%, 5%, and 7%, respectively; 69% had non-CC IL28B alleles (CT or TT); 74% had baseline HCV RNA levels at least 800,000 IU/mL; 19% had compensated cirrhosis; and 32% were treatment-experienced.
- Table 10 presents SVR12 and other virologic outcomes in Sofosbuvir/Velpatasvir-treated subjects in the ASTRAL-1 trial by HCV genotype. No subjects in the placebo group achieved SVR12.
Genotype 2 HCV Infected Adults (ASTRAL-2)
- ASTRAL-2 was a randomized, open-label trial that evaluated 12 weeks of treatment with Sofosbuvir/Velpatasvir compared with 12 weeks of treatment with SOF with ribavirin in subjects with genotype 2 HCV infection. Subjects were randomized in a 1:1 ratio to the treatment groups. Randomization was stratified by the presence or absence of compensated cirrhosis and prior treatment experience (treatment-naïve vs treatment-experienced).
- Demographics and baseline characteristics were balanced across the two treatment groups. Of the 266 treated subjects, the median age was 58 years (range: 23 to 81); 59% of the subjects were male; 88% were White; 7% were Black; 33% had a baseline body mass index at least 30 kg/m2 ; 62% had non-CC IL28B alleles (CT or TT); 80% had baseline HCV RNA levels at least 800,000 IU/mL; 14% had compensated cirrhosis; and 15% were treatment-experienced.
- Table 11 presents SVR12 and other virologic outcomes from the ASTRAL-2 trial.
Genotype 3 HCV Infected Adults (ASTRAL-3)
- ASTRAL-3 was a randomized, open-label trial that evaluated 12 weeks of treatment with Sofosbuvir/Velpatasvir compared with 24 weeks of treatment with SOF with ribavirin in subjects with genotype 3 HCV infection. Subjects were randomized in a 1:1 ratio to the treatment groups. Randomization was stratified by the presence or absence of compensated cirrhosis and prior treatment experience (treatment-naïve vs treatment-experienced).
- Demographics and baseline characteristics were balanced across the treatment groups. Of the 552 treated subjects, the median age was 52 years (range: 19 to 76); 62% of the subjects were male; 89% were White; 9% were Asian; 20% had a baseline body mass index at least 30 kg/m2 ; 61% had non-CC IL28B alleles (CT or TT); 70% had baseline HCV RNA levels at least 800,000 IU/mL; 30% had compensated cirrhosis; and 26% were treatment-experienced.
- Table 12 presents SVR12 and other virologic outcomes from the ASTRAL-3 trial.
- SVR12 for selected subgroups are presented in Table 13.
Clinical Trial in Subjects Coinfected with HCV and HIV-1
- ASTRAL-5 was an open-label trial that evaluated 12 weeks of treatment with Sofosbuvir/Velpatasvir in subjects with genotype 1, 2, 3, 4, 5 or 6 HCV infection who were coinfected with HIV1. Subjects were on a stable HIV-1 antiretroviral therapy that included emtricitabine/tenofovir disoproxil fumarate or abacavir/lamivudine administered with atazanavir/ritonavir, darunavir/ritonavir, lopinavir/ritonavir, rilpivirine, raltegravir or elvitegravir/cobicistat.
- Of the 106 treated subjects, the median age was 57 years (range: 25 to 72); 86% of the subjects were male; 51% were White; 45% were Black; 22% had a baseline body mass
index at least 30 kg/m2 ; the proportions of patients with genotype 1, 2, 3, or 4 HCV infection were 74%; 10%; 11%, and 5% respectively; no subjects with genotype 5 or 6 HCV were treated with Sofosbuvir/Velpatasvir; 77% had non- CC IL28B alleles (CT or TT); 74% had baseline HCV RNA levels of at least 800,000 IU/mL; 18% had compensated cirrhosis; and 29% were treatment experienced. The overall mean CD4+ count was 598 cells/µL (range: 183−1513 cells/µL) and 57% of subjects had CD4+ counts > 500 cells/μL.
- Table 14 presents the SVR12 for the ASTRAL-5 trial by HCV genotype.
- No subject had HIV-1 rebound during treatment and CD4+ counts were stable during treatment.
Clinical Trials in Subjects with Decompensated Cirrhosis
- ASTRAL-4 was a randomized, open-label trial in subjects with genotype 1, 2, 3, 4, 5, or 6 HCV infection and Child-Pugh B cirrhosis at screening. Subjects were randomized in a 1:1:1 ratio to treatment with Sofosbuvir/Velpatasvir for 12 weeks (N=90), Sofosbuvir/Velpatasvir with ribavirin for 12 weeks (N=87), or Sofosbuvir/Velpatasvir for 24 weeks (N=90). Randomization was stratified by HCV genotype (1, 2, 3, 4, 5, 6, and indeterminate).
- Demographics and baseline characteristics were balanced across the treatment groups. Of the 267 treated subjects, the median age was 59 years (range: 40 to 73); 70% of the subjects were male; 90% were White, 6% were Black; 42% had a baseline body mass index at least 30 kg/m2. The proportions of subjects with genotype 1, 2, 3, 4, or 6 HCV were 78%, 4%, 15%, 3%, and less than 1% (1 subject), respectively. No subjects with genotype 5 HCV infection were enrolled. 76% had non-CC IL28B alleles (CT or TT); 56% had baseline HCV RNA levels at least 800,000 IU/mL; 55% were treatmentexperienced; and 95% of subjects had Model for End Stage Liver Disease (MELD) score less than or equal to 15 at baseline. Although all subjects had Child-Pugh B cirrhosis at screening, 6% and 4% of subjects were assessed to have Child-Pugh A and Child-Pugh C cirrhosis, respectively, on the first day of treatment.
- Treatment with Sofosbuvir/Velpatasvir with ribavirin for 12 weeks resulted in numerically higher SVR12 rates than treatment with Sofosbuvir/Velpatasvir for 12 weeks or 24 weeks. Because Sofosbuvir/Velpatasvir with ribavirin for 12 weeks is the recommended dosage regimen, the results of the 12- and 24-week Sofosbuvir/Velpatasvir treatment groups are not presented.
- Table 15 presents the SVR12 for subjects treated with Sofosbuvir/Velpatasvir with ribavirin for 12 weeks in the ASTRAL-4 trial by HCV genotype. No subjects with genotype 5 or 6 HCV were treated with Sofosbuvir/Velpatasvir with ribavirin for 12 weeks.
- All subjects with genotype 2 (N=4) and genotype 4 (N=2) HCV infection treated with Sofosbuvir/Velpatasvir and ribavirin achieved SVR12.
How Supplied
- Each Sofosbuvir/Velpatasvir tablet contains 400 mg of Sofosbuvir and 100 mg of Velpatasvir, is pink, diamond-shaped, film-coated, debossed with “GSI” on one side and “7916” on the other. Each bottle contains 28 tablets (NDC 61958-2201-1), polyester coil, and is closed with a child-resistant closure.
Storage
- Store below 30 °C (86 ºF). Dispense only in original container.
Images
Drug Images
{{#ask: Page Name::Sofosbuvir / velpatasvir |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Sofosbuvir / velpatasvir |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Risk of Hepatitis B Virus Reactivation in Patients Coinfected with HCV and HBV
- Inform patients that HBV reactivation can occur in patients coinfected with HBV during or after treatment of HCV infection. Advise patients to tell their healthcare provider if they have a history of HBV infection.
Serious Symptomatic Bradycardia When Coadministered with Amiodarone
- Advise patients to seek medical evaluation immediately for symptoms of bradycardia such as near-fainting or fainting, dizziness or lightheadedness, malaise, weakness, excessive tiredness, shortness of breath, chest pain, confusion or memory problems.
Drug Interactions
- Inform patients that Sofosbuvir/Velpatasvir may interact with other drugs. Advise patients to report to their healthcare provider the use of any other prescription or nonprescription medication or herbal products including St. John’s wort.
Administration
- Advise patients to take Sofosbuvir/Velpatasvir once daily on a regular dosing schedule with or without food. Inform patients that it is important not to miss or skip doses and to take Sofosbuvir/Velpatasvir for the duration that is recommended by the physician.
Pregnancy
- Advise patients to avoid pregnancy during combination treatment with Sofosbuvir/Velpatasvir and ribavirin and for 6 months after completion of treatment. Inform patients to notify their healthcare provider immediately in the event of a pregnancy.
Precautions with Alcohol
Alcohol-Sofosbuvir / velpatasvir interaction has not been established. Talk to your doctor regarding the effects of taking alcohol with this medication.
Brand Names
- Epclusa
Look-Alike Drug Names
There is limited information regarding Sofosbuvir / velpatasvir Look-Alike Drug Names in the drug label.
Drug Shortage
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ Invalid
<ref>tag; no text was provided for refs namedAHFS2016 - ↑ "Epclusa (sofosbuvir and velpatasvir) Tablets, for Oral Use. Full Prescribing Information" (PDF). Gilead Sciences, Inc. Foster City, CA 94404. Retrieved 1 August 2016.