Oral rehydration therapy
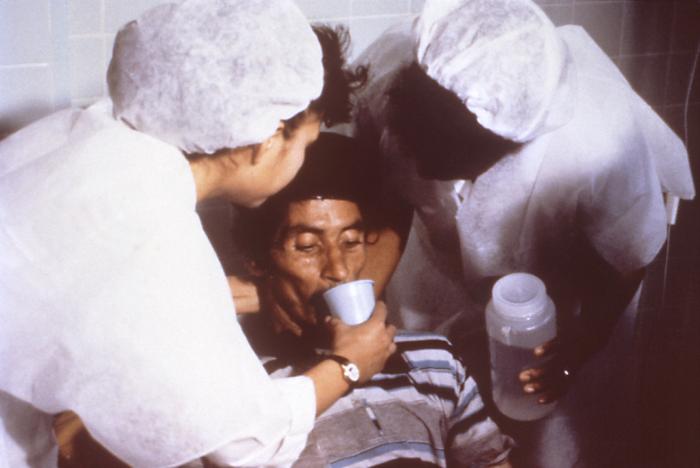
Courtesy:Centers for Disease Control and Prevention
Oral rehydration therapy, (also called ORT, oral rehydration salts or solutions (ORS), oral electrolyte, or drinking), is a simple, cheap, and effective treatment for diarrhea-related dehydration, for example due to cholera or rotavirus. It consists of a solution of salts and other substances such as glucose, sucrose, citrates or molasses, which is administered orally. It is used around the world, but is most important in the Third World, where it saves millions of children from diarrhea—still their leading cause of death.
History
Since ancient times, caregivers substituted cholera patient's water loss with rice water, coconut juice, carrot soup etc.[citation needed] Before the practice of ORT was known, modern doctors used intravenous fluid therapy to compensate for fluid loss in diarrhea.
Physiologists noted in the 1950s that sodium and glucose were cotransported along the gastrointestinal epithelium. Using histological and other techniques it was shown that the epithelium was not disrupted in cholera. These notions provided a physiological basis for the use of ORT in clinical medicine. ORT was developed in the late 1960s by researchers in India and International Centre for Diarrhoeal Disease Research, Bangladesh (then East Pakistan), for the treatment of cholera.
Smaller clinical trials in the late 1960s (like those of Hirschhorn, Nalin, Pierce etc.) confirmed the effectivity of adding glucose to sodium chloride solutions for ORT.
The Indo-Pakistani War of 1971 provoked a public health emergency in the refugee camps set up to house those fleeing the violence. With cholera spreading rapidly and death rates rising, medical teams ran out of intravenous fluids. Dr. Mahalanabis, the head of a medical centre in one of the camps (accommodating 350,000 refugees) instructed his staff to distribute Oral Rehydration Salts (ORS). In the refugee camps where ORS was being used to treat over 3000 patients, the death rate was only 3%, compared to 20–30% in those camps using only intravenous fluid therapy. Others replicated these findings and found ORT can be used in babies.
Meanwhile, further studies demonstrated the mechanism by which cholera caused fluid loss, i.e. because the cholera toxin constitutively activates the enzyme adenylate cyclase in the cells of the intestine. Research at the International Centre for Diarrhoeal Disease Research, Bangladesh (ICDDR,B) contributed much to these discoveries.
In 2002, Drs. Norbert Hirschhorn, Dilip Mahalanabis, David R. Nalin, and Nathaniel F. Pierce were awarded the first Pollin Prize for Pediatric Research, in recognition of their work in developing ORT[1].
In 1978 the World Health Organisation launched a worldwide campaign to reduce mortality related to diarrhea, with ORT as one of the principal elements of that program.
Between 1980 and 2000, ORT decreased the number of children under five dying of diarrhea from 4.6 million worldwide to 1.8 million—a 60% reduction. According to The Lancet (1978), ORT is "potentially the most important medical discovery of the 20th century".
Today, the total production is around 500 million ORS sachets per year, with the children's rights agency UNICEF distributing them to children in around 60 developing countries. ORS represents a cheap and effective way of reducing the millions of deaths caused each year by diarrhea.
Physiology
Oral rehydration therapy is widely considered to be the best method for combating the dehydration caused by diarrhea and/or vomiting.
Various diseases cause damage to the intestine, allowing water to flow from the blood into the intestine, depleting the body of both fluid and electrolytes. This may be
- a direct destruction of the cells lining the intestine (the enterocytes),
- a toxic effect causing them to lose their microvilli (the brush border),
- a toxic effect (by an enterotoxin) causing them to secrete water.
In the human body, water is absorbed and secreted passively; it follows the movement of salts, based on a principle called osmosis. So, in many cases, diarrhea is caused by intestine cells secreting salts (primarily sodium) and water following passively along.
Simply drinking water is ineffective for 2 reasons: (1) the large intestine is usually secreting instead of absorbing water, and (2) electrolyte losses also need compensating. As such, the standard treatment is to restore fluids intravenously with water and salts. This requires trained personnel and materials which are not sufficiently available in the Third World.
However, it was discovered that the body can absorb a simple solution containing both sugar and salt. The dry ingredients can be mixed and packaged, and then the solution can be prepared and delivered by people with minimal training. One diarrhea mechanism (like in cholera, which is a very dangerous form of profuse diarrhea), is an enterotoxin interfering with enterocyte cAMP and G-proteins. However, water can still be absorbed by cAMP-independent mechanisms, like the SGLT-transporter (sodium and glucose transporter, of which two types exist). This is achieved by combining salts and glucose.
Oral rehydration can be accomplished by drinking frequent small amounts of an oral rehydration salt solution.
It is important to rehydrate with solutions that contain electrolytes, especially sodium and potassium, so that electrolyte disturbances may be avoided. Sugar is absolutely essential to improve adequate absorption of electrolytes and water, but the presence of sugar in ORS solutions does tend to cause diarrhea to worsen. Although oral rehydration with a sugar solution does not stop diarrhea, and the diarrhea contributes to further loss of fluids, oral rehydration helps replace these fluids. It thus keeps the body hydrated and gives the patient a greatly improved chance of surviving the diarrhea. If a broth can be prepared from simple carbohydrates and substituted for sugar in the solution, diarrhea can sometimes be reduced while oral rehydration remains effective.
Often sodium bicarbonate or sodium citrate is also added to formulas in an attempt to revert metabolic acidosis.
Recipe
There are several commercially available products but an inexpensive home-made solution consists of 8 level teaspoons of sugar and 1 level teaspoon of table salt mixed in 1 liter of water (Rehydration Project: Home made recipe). Fructose (fruit sugar) or artificial sweeteners should not be used instead of sugar as they may increase diarrhea and/or not provide sufficient energy. A half cup of orange juice or half of a mashed banana can be added to each liter both to add potassium and to improve taste. If commercial solutions are used, true rehydration solutions should be used and sports drinks should be avoided (especially in younger children) as these solutions contain too much sugar and not enough electrolytes.
One standard remedy is the WHO/UNICEF glucose-based Oral Rehydration Salts (ORS) solution. WHO/UNICEF ORS solution contains
| Reduced osmolarity ORS | grams/litre |
|---|---|
| Sodium chloride | 2.6 |
| Anhydrous Glucose | 13.5 |
| Potassium chloride | 1.5 |
| Trisodium citrate, dihydrate | 2.9 |
| Reduced osmolarity ORS | mmol/litre |
|---|---|
| Sodium | 75 |
| Anhydrous Glucose | 75 |
| Chloride | 65 |
| Potassium | 20 |
| Citrate | 10 |
| Total Osmolarity | 245 |
In the human body, the plasma osmolarity is about 285 mOsm/l.
The amount of rehydration that is needed depends on the size of the individual and the degree of dehydration. Rehydration is generally adequate when the person no longer feels thirsty and has a normal urine output. A rough guide to the amount of ORS solution needed in the first 4-6 hours of treatment for a mildly dehydrated person is:
- Up to 5 kg (11 lb): 200 – 400 ml
- 5-10 kg (11-22 lb): 400 – 600 ml
- 10-15 kg (22-33 lb): 600 – 800 ml
- 15-20 kg (33–44 lb): 800 – 1000 ml
- 20-30 kg (44-66 lb: 1000 – 1500 ml
- 30-40 kg (66-88 lb): 1500 – 2000 ml
- 40 plus kg (88 lb): 2000-4000 ml
Technique
Adults and children with dehydration who are not vomiting can be allowed to drink these solutions in addition to their normal diet. People who are vomiting should be fed small frequent amounts of ORS solution until dehydration is resolved. Once they are rehydrated, they may resume eating normal foods when nausea passes.
Vomiting itself does not mean that oral rehydration cannot be given. As long as more fluid enters than exits, rehydration will be accomplished. It is only when the volume of fluid and electrolyte loss in vomit and stool exceeds what is taken in that dehydration will continue.
See also
- Electrolyte
- Sports drink
- CeraLyte, a commercially available rice-based oral rehydration solution (ORS).
References
History
- Guerrant RL, Carneiro-Filho BA, Dillingham RA. Cholera, diarrhea, and oral rehydration therapy: triumph and indictment. Clin Infect Dis 2003; 37(3): 398-405. PMID 12884165
- Bhattacharya SK. History of development of oral rehydration therapy. Indian J Public Health 1994; 38(2): 39-43. PMID 7530695
Footnotes
- ↑ World Health Organisation, Child and Adolescent Health Development. The first Pollin Prize for Paediatric Research awarded to Oral Rehydration Therapy. Issued November 2002, accessed August 21, 2006
External links
- Rehydration Project
- "Reducing deaths from diarrhoea through oral rehydration therapy", Bulletin of the World Health Organization, 2000: 78 (10); 1246-1255.
- New formulation of Oral Rehydration Salts (ORS) with reduced osmolarity - Technical Bulletin from UNICEF, describing the user of a weaker solution, with the aim of reducing stool output.
- Rainbow Pediatrics Knowledgebase: The Oral Rehydration Therapy
- A Simple Solution - Time, Sunday, Oct. 08, 2006.
- Diarrhea: why is a simple and inexpensive treatment not more widely used? IRC, Updated: Monday 06 November 2006. Accessed 21 November 2006.
- Ceralyte
de:Physiologische Kochsalzlösung nl:Oraal rehydratiemiddel sv:Vätskeersättning