Nipple discharge
|
WikiDoc Resources for Nipple discharge |
|
Articles |
|---|
|
Most recent articles on Nipple discharge Most cited articles on Nipple discharge |
|
Media |
|
Powerpoint slides on Nipple discharge |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Nipple discharge at Clinical Trials.gov Trial results on Nipple discharge Clinical Trials on Nipple discharge at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Nipple discharge NICE Guidance on Nipple discharge
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Nipple discharge Discussion groups on Nipple discharge Patient Handouts on Nipple discharge Directions to Hospitals Treating Nipple discharge Risk calculators and risk factors for Nipple discharge
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Nipple discharge |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Synonyms and Related keywords: Discharge from breasts; Milk secretions; Lactation - abnormal; Witches milk; Galactorrhea
Nipple discharge is the abnormal release of fluid from the nipples of the breasts. It is the third major reason, involving the breasts, for which women seek medical attention, after lumps and breast pain. The risk of nipple discharge increases with both age and number of pregnancies, but is also known to occur in adolescent boys and girls going through puberty. Discharge often is the result of stimulation of the breasts or by irritation through clothing.
Types of discharge
There are many different types of discharges. Some associations include:
- cloudy white color -- most common, can be galactorrhea
- clear or light white -- pregnancy
- red -- contains blood -- most often due to breast infection or intraductal papillomas, but can be breast cancer
- whitish-yellow or yellow or even green -- pus due to infection
Epidemiology and Demographics
- Most often benign: overall incidence cancer ~ 3-5%
- Risk of malignancy much increased if concurrent mass (~ 60%)
- Reported in 10-15% of women with benign breast disease
- Reported in 2.5-3% of women with breast cancer
Pathophysiology & Etiology
- Physiologic
- Discharge only with compression
- Multiple duct involvement
- Bilateral
- Fluid may be clear, yellow, white or dark green
- Pathologic
- Spontaneous discharge
- Bloody
- Unilateral
- Associated with a mass
- Physiologic / Endocrinologic Discharge
- Lactation
- Milk produced in presence of postpartum exocrin, parathyrin, thyroxine, cortisol, growth hormone and placental lactogen
- Milk secreted via stimulation of lobular and ductal epithelium by PRL
- Milk ejected via stimulation of muscular walls of lactiferous ducts by oxytocin
- Oxytocin and PRL secreted by pituitary in response to nipple stimulation
- Galactorrhea:
- Milk secretion unrelated to pregnancy/lactation
- Usually due to hyperprolactin state, though can be idiopathic with normal prolactin (PRL)
- Can occur via:
- Chronic breast stimulation (nipple manipulation, rubbing on bra)
- Oral Contraceptive Pills (OCPs) – E can stimulate PRL secretion
- Drugs that inhibit dopamine (loss of tonic inhibition of PRL)
- Hypothalamic/pituitary disease interfering with DA release
- Prolactinoma
- Hypothyroidism
- Chronic renal failure
- Chest wall injury – healing wound stimulates PRL release
- Pathologic Discharge
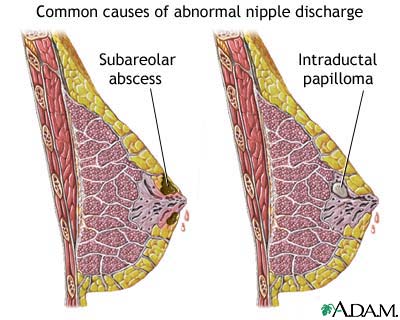
- Intraductal papilloma: monotonous proliferation of papillary cells growing into the lumen
- Fluid typically straw-colored, transparent, sticky
- Duct ectasia: distention of subareolar ducts
- Fibrocystic disease: associated irritation within the duct
- Papillomatosis: formation of multiple papillomas
- Associated with small increase in breast cancer risk
- Intraductal hyperplasia: increased number of epithelial cells lining the ducts
- Cells appear benign but associated with small increase in breast cancer risk
- Breast cancer: risk much increased if mass associated with abnormal discharge
History and Symptoms
- Description of Discharge
- Unilateral vs. bilateral (bilateral almost always due to endocrinologic cause)
- Spontaneous vs. provoked
- Bloody vs. non-bloody
- Endocrine Symptoms
- Irregular menses,
- thyroid symptoms,
- endo review of symptoms (& visual fields) if prolactinoma suspected
- Medical Conditions
- Renal failure,
- thyroid disease
- Medications
- Potential causes of hyperprolactinemia
Physical Examination
- Thorough breast exam to rule out palpable mass
- Skin exam for superficial lesions that might produce discharge mimicking nipple discharge
- (Eczema, Paget’s disease, local infections or irritation)
- Expression of discharge: firm pressure applied at base of areola of each breast
- Close observation to determine if discharge from > 1 nipple duct
- Guaiac testing for blood
- Cytology for bloody or G+ discharge:
- Express fluid along surface of glass slide
- Spray immediately with Pap smear fixative
- Prepare 4-6 slides for evaluation
- Low sensitivity, but high specificity for cancer
Other Imaging Findings
Mammogram
- Mammogram in all patients with pathologic discharge
- Mammogram in patients > 35 years old with physiologic or endocrinologic discharge:
- If negative mammogram, exam and endocrine evaluation, avoidance of nipple stimulation will often lead to resolution of discharge
Risk Stratification and Prognosis
Referral
- Unilateral, bloody or spontaneous discharge: all should be referred to breast surgeon
- Terminal duct excision diagnostic; may also be therapeutic if benign lesion
- Bilateral, non-bloody discharge with negative endocrine work-up: referral to breast surgeon if fails to resolve
See also
External links
Template:Diseases of the pelvis, genitals and breasts