Ludwig's angina
| Ludwig's angina | |
| Classification and external resources | |
| |
|---|---|
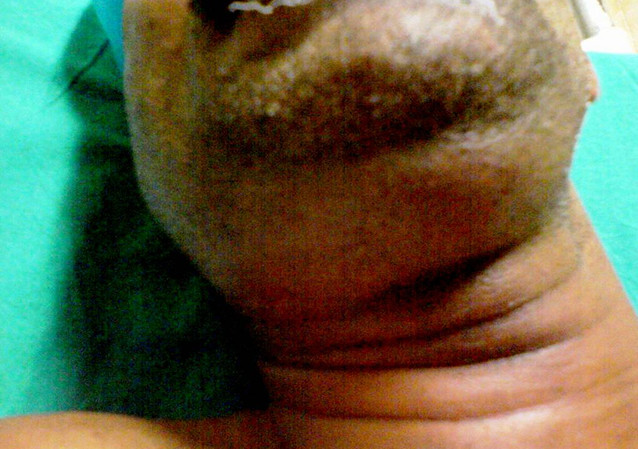
| Swelling in the submandibular area in a patient with Ludwig's angina. |
|
WikiDoc Resources for Ludwig's angina |
|
Articles |
|---|
|
Most recent articles on Ludwig's angina Most cited articles on Ludwig's angina |
|
Media |
|
Powerpoint slides on Ludwig's angina |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Ludwig's angina at Clinical Trials.gov Trial results on Ludwig's angina Clinical Trials on Ludwig's angina at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Ludwig's angina NICE Guidance on Ludwig's angina
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Ludwig's angina Discussion groups on Ludwig's angina Patient Handouts on Ludwig's angina Directions to Hospitals Treating Ludwig's angina Risk calculators and risk factors for Ludwig's angina
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Ludwig's angina |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Template:Seealso Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Ludwig's angina, otherwise known as angina ludovici, is a serious, potentially life-threatening cellulitis,[1] or connective tissue infection, of the floor of the mouth characterized by bilateral lower facial swelling around the lower jaw and upper neck. Ludwig's angina usually occurs in adults with concomitant dental infections and if left untreated, may obstruct the airways, necessitating tracheotomy. Symptoms of Ludwig's angina include malaise, fever, dysphagia (difficulty swallowing), odynophagia (pain during swallowing) and, in severe cases, stridor or difficulty breathing. The mainstay of therapy for Ludwig's angina includes surgery along with antimicrobial therapy.
It is named after the German physician, Wilhelm Friedrich von Ludwig who first described this condition in 1836.[2][3]. Other names include "angina Maligna" and "Morbus Strangularis". Ludwig's angina should not be confused with angina pectoris, which is also otherwise commonly known as "angina". The word "angina" comes from the Greek word ankhon, meaning "strangling", so in this case, Ludwig's angina refers to the feeling of strangling, not the feeling of chest pain, though there may be chest pain in Ludwig's angina if the infection spreads into the retrosternal space.
Causes
Dental infections account for approximately 80% of cases of Ludwig's angina.[4] Mixed infections, due to both aerobes and anaerobes, are of the cellulitis associated with Ludwig's angina. Typically, these include alpha-hemolytic streptococci, staphylococci and bacteroides groups.[4]
The route of infection in most cases is from infected lower molars or from pericoronitis, which is an infection of the gums surrounding the partially erupted lower (usually third) molars. Although the widespread involvement seen in Ludwig's usually develops in immunocompromised persons, it can also develop in otherwise healthy individuals. Thus, it is very important to obtain dental consultation for lower-third molars at the first sign of any pain, bleeding from the gums, sensitivity to heat/cold or swelling at the angle of the jaw.
There has been a single case reported where Ludwig's angina was thought to be caused by a recent tongue piercing.[5][6][7] In addition, Filipino boxer Pancho Villa died after contracting Ludwig's Angina following a bout with Jimmy McLarnin.[8]
Symptoms and signs
True Ludwig's Angina is a cellulitic facial infection. The signs are bilateral lower facial swelling around the lower jaw and upper neck. This is because the infection has spread to involve the Submandibular, Sublingual and Submental spaces of the face.
Swelling of the Submandibular space, while externally is concerning, the true danger lies in the fact that the swelling has also spread inwardly - compromising, or in effect narrowing the airway. Dysphagia (difficulty swallowing), Odynophagia (pain during swallowing) are symptoms that are typically seen and demand immediate attention.
The Sublingual and Submental spaces are anterior (beneath the middle and chin areas of the lower jaw) to the Submandibular space. Swelling in these areas can often push the floor of the mouth, including the tongue upwards and backwards - further compromising the airway.
Localisation of infection to the sublingual space is accompanied by swelling of structures in the floor of the mouth as well as the tongue being pushed upwards and backwards.[4]
Spread of infection to the submandibular spaces is usually accompanied by signs of cellulitis rather than those of an abscess. Submental and submandibular regions are swollen and tender.
Additional symptoms include malaise, fever, dysphagia (difficulty swallowing), odynophagia (pain during swallowing)[4] and, in severe cases, stridor or difficulty breathing. There may also be varying degrees of trismus. Swelling of the submandibular and/or sublingual space is imminent.
Treatment
Treatment involves appropriate antibiotic medications, monitoring and protection of the airway in severe cases, and, where appropriate, urgent maxillo-facial surgery and/or dental consultation to incise and drain the collections. The antibiotic of choice is from the penicillin group.
Incision and drainage of the abscess may be either intraoral or external. An intraoral incision and drainage procedure is indicated if the infection is localized to the sublingual space. External incision and drainage is performed if infection involves the perimandibular spaces.[4]
A nasotracheal tube is sometimes warranted for ventilation if the tissues of the mouth make insertion of an oral airway difficult or impossible.
In cases where the patency of the airway is compromised, skilled airway management is mandatory. Fiberoptic intubation is common.
Ludwig's angina is a life-threatening condition, and carries a fatality rate of about 5%.[9]
- Preferred regimen (immunocompetent host) (1): (Penicillin G 2–4 MU IV q4–6h AND Tobramycin 2 mg/kg IV q8h)
- Preferred regimen (immunocompetent host) (2): Ampicillin-Sulbactam 2 g IV q4h
- Preferred regimen (immunocompetent host) (3): Clindamycin 600 mg IV q6h
- Preferred regimen (immunocompetent host) (4): Doxycycline 200 mg IV q12h
- Preferred regimen (immunocompetent host) (5): Cefoxitin 2 g IV q6h
- Preferred regimen (immunocompetent host) (6): Cefotetan 2 g IV q12h
- Preferred regimen (immunocomppromised host) (1): Cefotaxime 2 g IV q6h
- Preferred regimen (immunocomppromised host) (2): Ceftizoxime 4 g IV q8h
- Preferred regimen (immunocomppromised host) (3): Piperacillin 3 g IV q4h
- Preferred regimen (immunocomppromised host) (4): Imipenem 500 mg IV q6h
- Preferred regimen (immunocomppromised host) (5): Meropenem 1 g IV q8h
- Preferred regimen (immunocomppromised host) (6): Gatifloxacin 200 mg IV q24h
References
- ↑ Template:DorlandsDict[dead link]
- ↑ Template:WhoNamedIt
- ↑ W. F. Von Ludwig. Über eine in neuerer Zeit wiederholt hier vorgekommene Form von Halsentzündung. Medicinisches Correspondenzblatt des Württembergischen ärztlichen Vereins, Stuttgart, 1836, 6: 21-25.
- ↑ 4.0 4.1 4.2 4.3 4.4 Dhingra, PL; Dhingra, Shruti (2010) [1992]. Nasim, Shabina, ed. Diseases of Ear, Nose and Throat. Dhingra, Deeksha (5 ed.). New Delhi: Elsevier. pp. 277–278. ISBN 978-81-312-2364-2.
- ↑ Body Piercing: To What Depths? An Unusual Case and Review of Associated Problems. Plastic & Reconstructive Surgery. 115(3):50e-54e, March 2005. Williams, Andrew M. M.A., M.R.C.S.(Ed.); Southern, Stephen J. F.R.C.S.(Plast.)
- ↑ Koenig, Laura M.; Carnes, Molly (1999). "Body Piercing: Medical Concerns with Cutting Edge-Fashion". Journal of General Internal Medicine. 14 (6): 379–385. doi:10.1046/j.1525-1497.1999.00357.x. PMC 1496593. PMID 10354260.
- ↑ Zadik Yehuda, Becker Tal, Levin Liran (January 2007). "Intra-oral and peri-oral piercing". J Isr Dent Assoc. 24 (1): 29–34, 83. PMID 17615989.
- ↑ http://www.ibhof.com/pages/about/inductees/oldtimer/villa.html
- ↑ Newlands C, Kerawala C (2010). Oral and maxillofacial surgery. Oxford: Oxford University Press. pp. 374–375. ISBN 9780199204830.