Interstitial nephritis pathophysiology
|
Interstitial nephritis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Interstitial nephritis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Interstitial nephritis pathophysiology |
|
Risk calculators and risk factors for Interstitial nephritis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] ; Associate Editor(s)-in-Chief: Mohsen Basiri M.D.
Overview
It is thought that acute interstitial nephritis is mediated by hypersensitivity reaction to endogenous or exogenous antigens expressed by tubular cells. Numerous drugs such as antibiotics, NSAIDS, sulfa-containing drugs, etc, as well as systemic diseases, and Infections may lead injury to renal cells. the cascade activation owing to cellular injury toward inflammatory cell infiltration, and activation of cytokines causes an immunologic reaction in acute or chronic process.
In acute interstitial nephritis, this cascade activation can cause renal tubular dysfunction, whereas in chronic interstitial nephritis an insidious interstitial fibrosis,scarring, and tubular atrophy spreads gradually and causes progressive chronic renal insufficiency.
Pathophysiology
In acute interstitial nephritis, espacially in acute drug-induced tubulointerstitial nephritis (TIN) an adverse reaction to any of an increasing number of drugs such as penicillins, rifampin, diuretics (thiazides), nonsteroidal anti-inflammatory agents, and numerous other drugs like phenindione, cimetidine occurs.[1]
Pathogenesis
Many features of the disease suggest an immune mechanism. Clinical evidence of hypersensitivity includes latent period, eosinophilia and rash, the idiosyncratic drug reaction (i.e., the lack of dose dependency), and the recurrence of hypersensitivity after reexposure to the same drug or others that are similar in structure. Serum IgE levels are increased in some persons, suggesting type I hypersensitivity.
In other cases the nature of the inflammatory infiltrate and the presence of positive skin tests to drugs suggest a T cell–mediated (type IV) hypersensitivity reaction.[2]
The most likely sequence of pathogenic events is as follows: The drugs act as haptens that, during secretion by tubules, covalently bind to some cytoplasmic or extracellular component of tubular cells and become immunogenic. The resultant tubulointerstitial injury is then caused by IgE- and cell mediated immune reactions to tubular cells or their basement membranes.
The development of drug-induced AIN is not dose-dependent, and recurrence or exacerbation can occur with a second exposure to the same or a related drug.[3]
Since the majority cases of TIN are due to bacterial infection, and the renal pelvis is deeply involved, therefore pyelonephritis is term describes this condition. And In general, the term interstitial nephritis is used for TIN that are owing to nonbacterial causes of tubular injury.
bacterial infection in accompanied with obstruction or reflux such as Legionella, Leptospira, can primarily invade organs remote from the kidney and exerted an inflammatory response in the kidney without invading the kidney.[4] [5]
However, more recent reports describe the identification of organism-specific antigens or DNA in kidney proximal tubule cells of patients with TIN, a histologic variant of TIN that is characterized by granuloma formation has been associated with Mycobacterium, fungi (histoplasmosis, coccidiomycosis), bacteria (Brucella, Chlamydia), spirochetes (Francisella, Treponema), and parasites (Leishmania, Toxoplasma).[6]
Associated Conditions
Common conditions associated with interstitial nephritis include:
Gross Pathology
On gross pathology, [feature1], [feature2], and [feature3] are characteristic findings of [disease name].
Microscopic Pathology
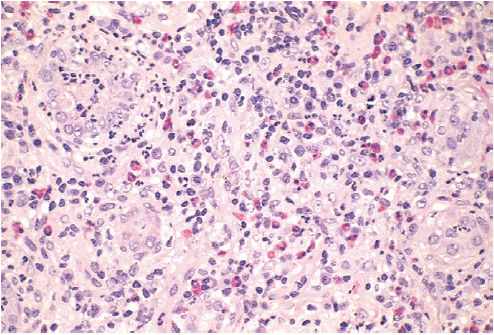
The abnormalities in acute drug-induced nephritis are in the interstitium which shows pronounced edema and infiltration by mononuclear cells, principally lymphocytes and macrophages. Eosinophils and neutrophils may be present, often in large numbers. Interstitial non-necrotizing granulomas with giant cells may be seen with some Medications such as methicillin, thiazides, and rifampin. The glomeruli are normal except in some cases caused by nonsteroidal antiinflammatory agents, in which the hypersensitivity reaction also leads to podocyte foot process effacement and the nephrotic syndrome.
References
- ↑ Kelly C, Tomaszewski J, Neilson E. Immunopathogenic mechanisms of tubulointerstitial injury. In: Tisher C, Brenner B, eds, Renal Pathology: With Clinical and Functional Correlations, 2nd Edn., Vol. 1. J. B. Lippincott & Co, Philadelphia, PA, 1994; 699–722
- ↑ Sabnis, Sharda G.; Koss, Michael N.; Ross, W.B.; Pavlova, Zdena (2009). "Non-Neoplastic Kidney": 979–1042. doi:10.1016/B978-1-4160-3966-2.00029-1.
- ↑ Schubert C, Bates WD, Moosa MR. Acute tubulointerstitial nephritis related to antituberculous drug therapy. Clin Nephrol 2010; 73:413
- ↑ Ellis D, Fried WA, Yunis EJ, Blau EB. Acute interstitial nephritis in children: a report of 13 cases and review of the literature. Pediatrics 1981; 67:862
- ↑ Dharmarajan TS, Yoo J, Russell RO, Boateng YA. Acute post streptococcal interstitial nephritis in an adult and review of the literature. Int Urol Nephrol 1999; 31:145
- ↑ Agrawal V, Crisi GM, D'Agati VD, Freda BJ. Renal sarcoidosis presenting as acute kidney injury with granulomatous interstitial nephritis and vasculitis. Am J Kidney Dis 2012; 59:303