Insulin lispro
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Alonso Alvarado, M.D. [2]
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Insulin lispro is an insulin analog that is FDA approved for the {{{indicationType}}} of improve glycemic control in adults and children with diabetes mellitus. Common adverse reactions include injection site reaction, hypoglycemia, hypokalemia, lipodystrophy.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Dosage Considerations
- When given subcutaneously, insulin lispro has a more rapid onset of action and a shorter duration of action than regular human insulin.
- The dosage of insulin lispro must be individualized. Blood glucose monitoring is essential in all patients receiving insulin therapy.
- The total daily insulin requirement may vary and is usually between 0.5 to 1 unit/kg/day. Insulin requirements may be altered during stress, major illness, or with changes in exercise, meal patterns, or coadministered drugs.
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
Subcutaneous Administration
- Insulin lispro should be given within 15 minutes before a meal or immediately after a meal.
- Insulin lispro given by subcutaneous injection should generally be used in regimens with an intermediate- or long-acting insulin.
- Insulin lispro administered by subcutaneous injection should be given in the abdominal wall, thigh, upper arm, or buttocks. Injection sites should be rotated within the same region (abdomen, thigh, upper arm, or buttocks) from one injection to the next to reduce the risk of lipodystrophy.
Continuous Subcutaneous Infusion (Insulin Pump)
- Insulin lispro may be administered by continuous subcutaneous infusion by an external insulin pump. Do not use diluted or mixed insulins in external insulin pumps. Infusion sites should be rotated within the same region to reduce the risk of lipodystrophy. Change the insulin lispro in the reservoir at least every 7 days, change the infusion sets and the infusion set insertion site at least every 3 days.
- The initial programming of the external insulin infusion pump should be based on the total daily insulin dose of the previous regimen. Although there is significant variability among patients, approximately 50% of the total dose is usually given as meal-related boluses of insulin lispro and the remainder is given as a basal infusion. Insulin lispro is recommended for use in pump systems suitable for insulin infusion such as MiniMed, Disetronic, and other equivalent pumps.
Intravenous Administration
- Insulin lispro can be administered intravenously under medical supervision with close monitoring of blood glucose and potassium levels to avoid hypoglycemia and hypokalemia. Insulin lispro should be used at concentrations from 0.1 unit/mL to 1.0 unit/mL in infusion systems containing 0.9% sodium chloride.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Insulin lispro in adult patients.
Non–Guideline-Supported Use
Prophylaxis of Cardiovascular System Disorder in Patients with Type 1 Diabetes Mellitus
- Dosing Information
- Administer insulin through external pump or ≥ 3 daily injections.[1]
Prophylaxis of Cardiovascular System Disorder in Patients with Type 2 Diabetes Mellitus
- Dosing Information
- Administer stepped treatment:[2]
- Administer one injection at night, with or without glipizide during daytime
- Administer insulin injections twice daily
- Administer ≥ 3 daily injections
Diabetic Nephropathy Prophylaxis
- Dosing Information
- Diabetes mellitus type 1: ≥ 3 daily injections.[3]
- Diabetes mellitus type 2: ≥ 3 daily injections.[4]
Diabetic Neuropathy Prophylaxis
- Dosing Information
Diabectic Retinopathy Prophylaxis
- Dosing Information
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
- When given subcutaneously, insulin lispro has a more rapid onset of action and a shorter duration of action than regular human insulin.
- The dosage of insulin lispro must be individualized. Blood glucose monitoring is essential in all patients receiving insulin therapy.
- The total daily insulin requirement may vary and is usually between 0.5 to 1 unit/kg/day. Insulin requirements may be altered during stress, major illness, or with changes in exercise, meal patterns, or coadministered drugs.
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
Subcutaneous Administration
- Insulin lispro should be given within 15 minutes before a meal or immediately after a meal.
- Insulin lispro given by subcutaneous injection should generally be used in regimens with an intermediate- or long-acting insulin.
- Insulin lispro administered by subcutaneous injection should be given in the abdominal wall, thigh, upper arm, or buttocks. Injection sites should be rotated within the same region (abdomen, thigh, upper arm, or buttocks) from one injection to the next to reduce the risk of lipodystrophy.
Continuous Subcutaneous Infusion (Insulin Pump)
- Insulin lispro may be administered by continuous subcutaneous infusion by an external insulin pump. Do not use diluted or mixed insulins in external insulin pumps. Infusion sites should be rotated within the same region to reduce the risk of lipodystrophy. Change the insulin lispro in the reservoir at least every 7 days, change the infusion sets and the infusion set insertion site at least every 3 days.
- The initial programming of the external insulin infusion pump should be based on the total daily insulin dose of the previous regimen. Although there is significant variability among patients, approximately 50% of the total dose is usually given as meal-related boluses of insulin lispro and the remainder is given as a basal infusion. Insulin lispro is recommended for use in pump systems suitable for insulin infusion such as MiniMed, Disetronic, and other equivalent pumps.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Insulin lispro in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Insulin lispro in pediatric patients.
Contraindications
Insulin lispro is contraindicated:
- During episodes of hypoglycemia
- In patients who are hypersensitive to insulin lispro or to any of its excipients.
Warnings
Dose Adjustment and Monitoring
- Glucose monitoring is essential for patients receiving insulin therapy. Changes to an insulin regimen should be made cautiously and only under medical supervision. Changes in insulin strength, manufacturer, type, or method of administration may result in the need for a change in insulin dose. Concomitant oral antidiabetic treatment may need to be adjusted.
- As with all insulin preparations, the time course of action for insulin lispro may vary in different individuals or at different times in the same individual and is dependent on many conditions, including the site of injection, local blood supply, or local temperature. Patients who change their level of physical activity or meal plan may require adjustment of insulin dosages.
Hypoglycemia
- Hypoglycemia is the most common adverse effect associated with insulins, including insulin lispro. The risk of hypoglycemia increases with tighter glycemic control. Patients must be educated to recognize and manage hypoglycemia. Hypoglycemia can happen suddenly and symptoms may be different for each person and may change from time to time. Severe hypoglycemia can cause seizures and may be life-threatening or cause death.
- The timing of hypoglycemia usually reflects the time-action profile of the administered insulin formulations. Other factors such as changes in food intake (e.g., amount of food or timing of meals), injection site, exercise, and concomitant medications may also alter the risk of hypoglycemia.
- As with all insulins, use caution in patients with hypoglycemia unawareness and in patients who may be predisposed to hypoglycemia (e.g., the pediatric population and patients who fast or have erratic food intake). The patient's ability to concentrate and react may be impaired as a result of hypoglycemia. This may present a risk in situations where these abilities are especially important, such as driving or operating other machinery.
- Rapid changes in serum glucose levels may induce symptoms similar to hypoglycemia in persons with diabetes, regardless of the glucose value. Early warning symptoms of hypoglycemia may be different or less pronounced under certain conditions, such as longstanding diabetes, diabetic nerve disease, use of medications such as beta-blockers, or intensified diabetes control. These situations may result in severe hypoglycemia (and, possibly, loss of consciousness) prior to the patient's awareness of hypoglycemia.
Hypersensitivity and Allergic Reactions
- Severe, life-threatening, generalized allergy, including anaphylaxis, can occur with insulin products, including insulin lispro.
Hypokalemia
- All insulin products, including insulin lispro, cause a shift in potassium from the extracellular to intracellular space, possibly leading to hypokalemia. Untreated hypokalemia may cause respiratory paralysis, ventricular arrhythmia, and death. Use caution in patients who may be at risk for hypokalemia (e.g., patients using potassium-lowering medications, patients taking medications sensitive to serum potassium concentrations and patients receiving intravenously administered insulin).
Renal or Hepatic Impairment
- Frequent glucose monitoring and insulin dose reduction may be required in patients with renal or hepatic impairment.
Mixing of Insulins
- Insulin lispro for subcutaneous injection should not be mixed with insulin preparations other than NPH insulin. If insulin lispro is mixed with NPH insulin, insulin lispro should be drawn into the syringe first. Injection should occur immediately after mixing.
- Do not mix insulin lispro with other insulins for use in an external subcutaneous infusion pump.
Subcutaneous Insulin Infusion Pumps
- When used in an external insulin pump for subcutaneous infusion, insulin lispro should not be diluted or mixed with any other insulin. Change the insulin lispro in the reservoir at least every 7 days, change the infusion sets and the infusion set insertion site at least every 3 days. Insulin lispro should not be exposed to temperatures greater than 98.6°F (37°C).
- Malfunction of the insulin pump or infusion set or insulin degradation can rapidly lead to hyperglycemia and ketosis. Prompt identification and correction of the cause of hyperglycemia or ketosis is necessary. Interim subcutaneous injections with insulin lispro may be required. Patients using continuous subcutaneous insulin infusion pump therapy must be trained to administer insulin by injection and have alternate insulin therapy available in case of pump failure.
Drug Interactions
- Some medications may alter insulin requirements and the risk for hypoglycemia or hyperglycemia.
Fluid Retention and Heart Failure with Concomitant Use of PPAR-gamma Agonists
- Thiazolidinediones (TZDs), which are peroxisome proliferator-activated receptor (PPAR)-gamma agonists, can cause dose-related fluid retention, particularly when used in combination with insulin. Fluid retention may lead to or exacerbate heart failure. Patients treated with insulin, including , and a PPAR-gamma agonist should be observed for signs and symptoms of heart failure. If heart failure develops, it should be managed according to current standards of care, and discontinuation or dose reduction of the PPAR-gamma agonist must be considered.
Adverse Reactions
Clinical Trials Experience
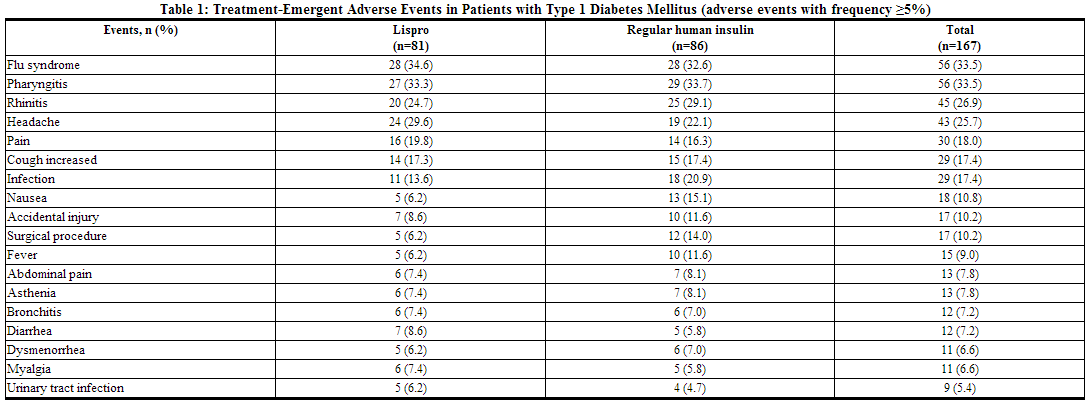
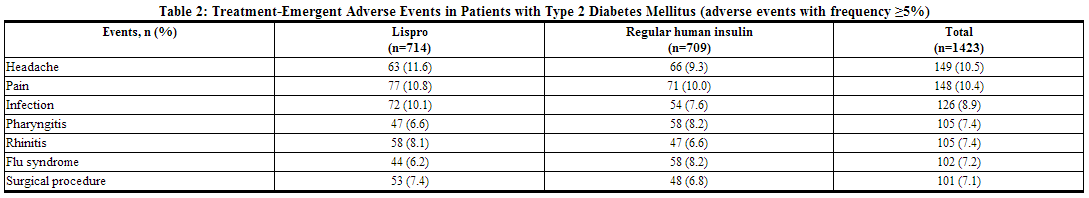
- Because clinical trials are conducted under widely varying designs, the adverse reaction rates reported in one clinical trial may not be easily compared with those rates reported in another clinical trial, and may not reflect the rates actually observed in clinical practice.
- The frequencies of Treatment-Emergent Adverse Events during insulin lispro clinical trials in patients with type 1 diabetes mellitus and type 2 diabetes mellitus are listed in the tables below.
Insulin initiation and intensification of glucose control
- Intensification or rapid improvement in glucose control has been associated with a transitory, reversible ophthalmologic refraction disorder, worsening of diabetic retinopathy, and acute painful peripheral neuropathy. However, long-term glycemic control decreases the risk of diabetic retinopathy and peripheral neuropathy.
Lipodystrophy
- Long-term use of insulin, including insulin lispro, can cause lipodystrophy at the site of repeated insulin injections or infusion. Lipodystrophy includes lipohypertrophy (thickening of adipose tissue) and lipoatrophy (thinning of adipose tissue), and may affect insulin absorption. Rotate insulin injection or infusion sites within the same region to reduce the risk of lipodystrophy.
Weight gain
- Weight gain can occur with insulin therapy, including insulin lispro, and has been attributed to the anabolic effects of insulin and the decrease in glucosuria.
Peripheral Edema
- Insulin, including insulin lispro, may cause sodium retention and edema, particularly if previously poor metabolic control is improved by intensified insulin therapy.
- Adverse Reactions with Continuous Subcutaneous Insulin Infusion (CSII)
- In a 12-week, randomized, crossover study in adult patients with type 1 diabetes (n=39), the rates of catheter occlusions and infusion site reactions were similar for insulin lispro and regular human insulin treated patients (see Table 3).

- In a randomized, 16-week, open-label, parallel design study of children and adolescents with type 1 diabetes, adverse event reports related to infusion-site reactions were similar for insulin lispro and insulin aspart (21% of 100 patients versus 17% of 198 patients, respectively). In both groups, the most frequently reported infusion site adverse events were infusion site erythema and infusion site reaction.
Allergic Reactions
- Local Allergy: As with any insulin therapy, patients taking insulin lispro may experience redness, swelling, or itching at the site of the injection. These minor reactions usually resolve in a few days to a few weeks, but in some occasions, may require discontinuation of insulin lispro. In some instances, these reactions may be related to factors other than insulin, such as irritants in a skin cleansing agent or poor injection technique.
- Systemic Allergy: Severe, life-threatening, generalized allergy, including anaphylaxis, may occur with any insulin, including insulin lispro. Generalized allergy to insulin may cause whole body rash (including pruritus), dyspnea, wheezing, hypotension, tachycardia, or diaphoresis.
- In controlled clinical trials, pruritus (with or without rash) was seen in 17 patients receiving regular human insulin (n=2969) and 30 patients receiving insulin lispro (n=2944).
- Localized reactions and generalized myalgias have been reported with injected metacresol, which is an excipient in insulin lispro.
Antibody Production
- In large clinical trials with patients with type 1 (n=509) and type 2 (n=262) diabetes mellitus, anti-insulin antibody (insulin lispro-specific antibodies, insulin-specific antibodies, cross-reactive antibodies) formation was evaluated in patients receiving both regular human insulin and insulin lispro (including patients previously treated with human insulin and naive patients). As expected, the largest increase in the antibody levels occurred in patients new to insulin therapy. The antibody levels peaked by 12 months and declined over the remaining years of the study. These antibodies do not appear to cause deterioration in glycemic control or necessitate an increase in insulin dose. There was no statistically significant relationship between the change in the total daily insulin dose and the change in percent antibody binding for any of the antibody types.
Postmarketing Experience
The following additional adverse reactions have been identified during post-approval use of insulin lispro. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. Medication errors in which other insulins have been accidentally substituted for insulin lispro have been identified during postapproval use.
Drug Interactions
A number of drugs affect glucose metabolism and may require insulin dose adjustment and particularly close monitoring. Following are some of the examples:
- Drugs That May Increase the Blood-Glucose-Lowering Effect of Insulin Lispro and Susceptibility to Hypoglycemia: Oral antidiabetic agents, salicylates, sulfonamide antibiotics, monoamine oxidase inhibitors, fluoxetine, pramlintide, disopyramide, fibrates, propoxyphene, pentoxifylline, ACE inhibitors, angiotensin II receptor blocking agents, and somatostatin analogs (e.g., octreotide).
- Drugs That May Reduce the Blood-Glucose-Lowering Effect of Insulin Lispro: Corticosteroids, isoniazid, niacin, estrogens, oral contraceptives, phenothiazines, danazol, diuretics, sympathomimetic agents (e.g., epinephrine, albuterol, terbutaline), somatropin, atypical antipsychotics, glucagon, protease inhibitors, and thyroid hormones.
- Drugs That May Increase or Reduce the Blood-Glucose-Lowering Effect of Insulin Lispro: Beta-blockers, clonidine, lithium salts, and alcohol. Pentamidine may cause hypoglycemia, which may sometimes be followed by hyperglycemia.
- Drugs That May Reduce the Signs of Hypoglycemia: Beta-blockers, clonidine, guanethidine, and reserpine.
Use in Specific Populations
Pregnancy
- All pregnancies have a background risk of birth defects, loss, or other adverse outcome regardless of drug exposure. This background risk is increased in pregnancies complicated by hyperglycemia and may be decreased with good metabolic control. It is essential for patients with diabetes or history of gestational diabetes to maintain good metabolic control before conception and throughout pregnancy. In patients with diabetes or gestational diabetes insulin requirements may decrease during the first trimester, generally increase during the second and third trimesters, and rapidly decline after delivery. Careful monitoring of glucose control is essential in these patients. Therefore, female patients should be advised to tell their physicians if they intend to become, or if they become pregnant while taking insulin lispro.
- Although there are limited clinical studies of the use of insulin lispro in pregnancy, published studies with human insulins suggest that optimizing overall glycemic control, including postprandial control, before conception and during pregnancy improves fetal outcome.
- In a combined fertility and embryo-fetal development study, female rats were given subcutaneous insulin lispro injections of 5 and 20 units/kg/day (0.8 and 3 times the human subcutaneous dose of 1 unit/kg/day, based on units/body surface area, respectively) from 2 weeks prior to cohabitation through Gestation Day 19. There were no adverse effects on female fertility, implantation, or fetal viability and morphology. However, fetal growth retardation was produced at the 20 units/kg/day-dose as indicated by decreased fetal weight and an increased incidence of fetal runts/litter.
- In an embryo-fetal development study in pregnant rabbits, insulin lispro doses of 0.1, 0.25, and 0.75 unit/kg/day (0.03, 0.08, and 0.24 times the human subcutaneous dose of 1 unit/kg/day, based on units/body surface area, respectively) were injected subcutaneously on Gestation days 7 through 19. There were no adverse effects on fetal viability, weight, and morphology at any dose.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Insulin lispro in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Insulin lispro during labor and delivery.
Nursing Mothers
It is unknown whether insulin lispro is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when insulin lispro is administered to a nursing woman. Use of insulin lispro is compatible with breastfeeding, but women with diabetes who are lactating may require adjustments of their insulin doses.
Pediatric Use
- Insulin lispro is approved for use in children for subcutaneous daily injections and for subcutaneous continuous infusion by external insulin pump. Insulin lispro has not been studied in pediatric patients younger than 3 years of age. insulin lispro has not been studied in pediatric patients with type 2 diabetes.
- As in adults, the dosage of insulin lispro must be individualized in pediatric patients based on metabolic needs and results of frequent monitoring of blood glucose.
Geriatic Use
Of the total number of subjects (n=2834) in eight clinical studies of insulin lispro, twelve percent (n=338) were 65 years of age or over. The majority of these had type 2 diabetes. HbA1c values and hypoglycemia rates did not differ by age. Pharmacokinetic/pharmacodynamic studies to assess the effect of age on the onset of insulin lispro action have not been performed.
Gender
There is no FDA guidance on the use of Insulin lispro with respect to specific gender populations.
Race
There is no FDA guidance on the use of Insulin lispro with respect to specific racial populations.
Renal Impairment
Frequent glucose monitoring and insulin dose reduction may be required in patients with renal impairment.
Hepatic Impairment
Frequent glucose monitoring and insulin dose reduction may be required in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Insulin lispro in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Insulin lispro in patients who are immunocompromised.
Administration and Monitoring
Administration
- Subcutaneous Administration (single dose)
- Continuous Subcutaneous Infusion (Insulin Pump)
- Intravenous Administration
Monitoring
- Glucose monitoring is essential for patients receiving insulin therapy. Changes to an insulin regimen should be made cautiously and only under medical supervision. Changes in insulin strength, manufacturer, type, or method of administration may result in the need for a change in insulin dose. Concomitant oral antidiabetic treatment may need to be adjusted.
- As with all insulin preparations, the time course of action for insulin lispro may vary in different individuals or at different times in the same individual and is dependent on many conditions, including the site of injection, local blood supply, or local temperature. Patients who change their level of physical activity or meal plan may require adjustment of insulin dosages.
IV Compatibility
There is limited information regarding the compatibility of Insulin lispro and IV administrations.
Overdosage
Excess insulin administration may cause hypoglycemia and hypokalemia. Mild episodes of hypoglycemia usually can be treated with oral glucose. Adjustments in drug dosage, meal patterns, or exercise may be needed. More severe episodes with coma, seizure, or neurologic impairment may be treated with intramuscular/subcutaneous glucagon or concentrated intravenous glucose. Sustained carbohydrate intake and observation may be necessary because hypoglycemia may recur after apparent clinical recovery. Hypokalemia must be corrected appropriately.
Pharmacology
| |
Insulin lispro
| |
| Systematic (IUPAC) name | |
| ? | |
| Identifiers | |
| CAS number | |
| ATC code | A10 |
| PubChem | |
| DrugBank | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 5813.63 g/mol |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Metabolism | ? |
| Half life | ? |
| Excretion | ? |
| Therapeutic considerations | |
| Pregnancy cat. |
? |
| Legal status | |
| Routes | ? |
Mechanism of Action
Regulation of glucose metabolism is the primary activity of insulins and insulin analogs, including insulin lispro. Insulins lower blood glucose by stimulating peripheral glucose uptake by skeletal muscle and fat, and by inhibiting hepatic glucose production. Insulins inhibit lipolysis and proteolysis, and enhance protein synthesis.
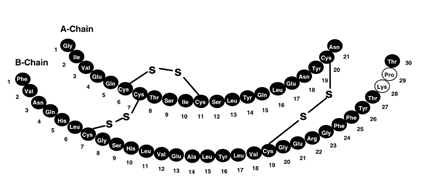
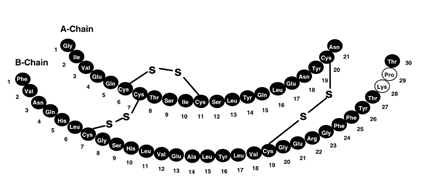
Structure
Insulin lispro injection, USP [rDNA origin] is a rapid-acting human insulin analog used to lower blood glucose. Insulin lispro is produced by recombinant DNA technology utilizing a non-pathogenic laboratory strain of Escherichia coli. Insulin lispro differs from human insulin in that the amino acid proline at position B28 is replaced by lysine and the lysine in position B29 is replaced by proline. Chemically, it is Lys(B28), Pro(B29) human insulin analog and has the empirical formula C257H383N65O77S6 and a molecular weight of 5808, both identical to that of human insulin. Insulin lispro has the following primary structure:
Insulin lispro is a sterile, aqueous, clear, and colorless solution. Each milliliter of insulin lispro contains insulin lispro 100 units, 16 mg glycerin, 1.88 mg dibasic sodium phosphate, 3.15 mg Metacresol, zinc oxide content adjusted to provide 0.0197 mg zinc ion, trace amounts of phenol, and Water for Injection. Insulin lispro has a pH of 7.0 to 7.8. The pH is adjusted by addition of aqueous solutions of hydrochloric acid 10% and/or sodium hydroxide 10%.
Pharmacodynamics
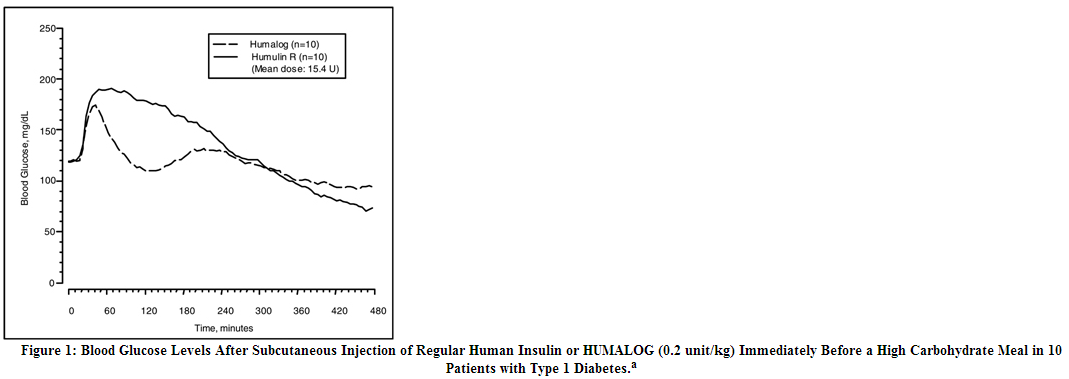
Insulin lispro has been shown to be equipotent to human insulin on a molar basis. One unit of insulin lispro has the same glucose-lowering effect as one unit of regular human insulin. Studies in normal volunteers and patients with diabetes demonstrated that insulin lispro has a more rapid onset of action and a shorter duration of activity than regular human insulin when given subcutaneously. The time course of action of insulin and insulin analogs, such as insulin lispro, may vary considerably in different individuals or within the same individual. The parameters of insulin lispro activity (time of onset, peak time, and duration) as designated in Figure 1 should be considered only as general guidelines. The rate of insulin absorption, and consequently the onset of activity are known to be affected by the site of injection, exercise, and other variables
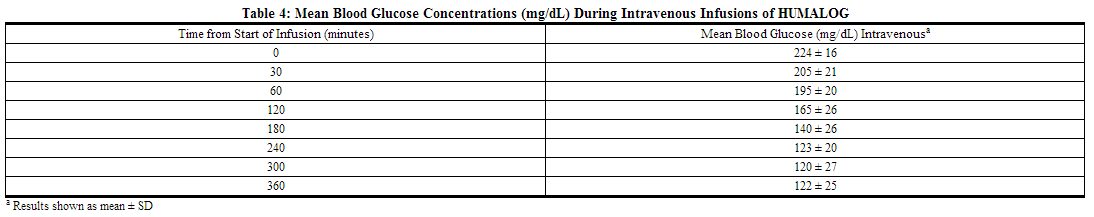
a Baseline insulin concentration was maintained by infusion of 0.2 mU/min/kg human insulin. Intravenous Administration of insulin lispro: The glucose lowering effect of intravenously administered insulin lispro was tested in 21 patients with type 1 diabetes. For the study, the patients' usual doses of insulin were held and blood glucose concentrations were allowed to reach a stable range of 200 to 260 mg/dL during a one to three hours run-in phase. The run-in phase was followed by a 6-hour assessment phase. During the assessment phase, patients received intravenous insulin lispro at an initial infusion rate of 0.5 units/hour. The infusion rate of insulin lispro could be adjusted at regular timed intervals to achieve and maintain blood glucose concentrations between 100 to 160 mg/dL. The mean blood glucose levels during the assessment phase for patients on insulin lispro therapy are summarized below in Table 4. All patients achieved the targeted glucose range at some point during the 6-hour assessment phase. At the endpoint, blood glucose was within the target range (100 to 160 mg/dL) for 17 of 20 patients treated with insulin lispro. The average time (±SE) required to attain near normoglycemia was 129 ± 14 minutes for insulin lispro.
Pharmacokinetics
Absorption and Bioavailability
Studies in healthy volunteers and patients with diabetes demonstrated that insulin lispro is absorbed more quickly than regular human insulin. In healthy volunteers given subcutaneous doses of insulin lispro ranging from 0.1 to 0.4 unit/kg, peak serum levels were seen 30 to 90 minutes after dosing. When healthy volunteers received equivalent doses of regular human insulin, peak insulin levels occurred between 50 to 120 minutes after dosing. Similar results were seen in patients with type 1 diabetes (see Figure 2).
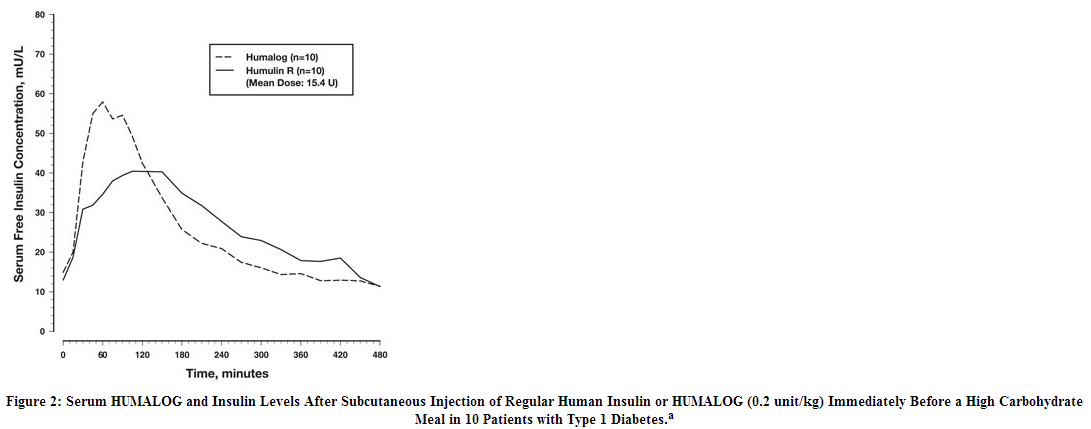
a Baseline insulin concentration was maintained by infusion of 0.2 mU/min/kg human insulin. insulin lispro was absorbed at a consistently faster rate than regular human insulin in healthy male volunteers given 0.2 unit/kg at abdominal, deltoid, or femoral subcutaneous sites. After insulin lispro was administered in the abdomen, serum drug levels were higher and the duration of action was slightly shorter than after deltoid or thigh administration. Bioavailability of insulin lispro is similar to that of regular human insulin. The absolute bioavailability after subcutaneous injection ranges from 55% to 77% with doses between 0.1 to 0.2 unit/kg, inclusive.
Distribution
When administered intravenously as bolus injections of 0.1 and 0.2 U/kg dose in two separate groups of healthy subjects, the mean volume of distribution of insulin lispro appeared to decrease with increase in dose (1.55 and 0.72 L/kg, respectively) in contrast to that of regular human insulin for which, the volume of distribution was comparable across the two dose groups (1.37 and 1.12 L/kg for 0.1 and 0.2 U/kg dose, respectively).
Metabolism
Human metabolism studies have not been conducted. However, animal studies indicate that the metabolism of insulin lispro is identical to that of regular human insulin.
Elimination
After subcutaneous administration of insulin lispro, the t1/2 is shorter than that of regular human insulin (1 versus 1.5 hours, respectively). When administered intravenously, insulin lispro and regular human insulin demonstrated similar dose-dependent clearance, with a mean clearance of 21.0 mL/min/kg and 21.4 mL/min/kg, respectively (0.1 unit/kg dose), and 9.6 mL/min/kg and 9.4 mL/min/kg, respectively (0.2 unit/kg dose). Accordingly, insulin lispro demonstrated a mean t1/2 of 0.85 hours (51 minutes) and 0.92 hours (55 minutes), respectively for 0.1 unit/kg and 0.2 unit/kg doses, and regular human insulin mean t1/2 was 0.79 hours (47 minutes) and 1.28 hours (77 minutes), respectively for 0.1 unit/kg and 0.2 unit/kg doses.
Specific Populations
Age
The effect of age on the pharmacokinetics of insulin lispro has not been studied. However, in large clinical trials, sub-group analysis based on age did not indicate any difference in postprandial glucose parameters between vand regular human insulin.
Gender
The effect of gender on the pharmacokinetics of insulin lispro has not been studied. However, in large clinical trials, sub-group analysis based on gender did not indicate any difference in postprandial glucose parameters between insulin lispro and regular human insulin.
Renal Impairment
Type 2 diabetic patients with varying degree of renal impairment showed no difference in pharmacokinetics of regular insulin and insulin lispro. However, the sensitivity of the patients to insulin did change, with an increased response to insulin as the renal function declined. Some studies with human insulin have shown increased circulating levels of insulin in patients with renal impairment. Careful glucose monitoring and dose adjustments of insulin, including insulin lispro, may be necessary in patients with renal dysfunction.
Hepatic Impairment
Type 2 diabetic patients with impaired hepatic function showed no effect on the pharmacokinetics of insulin lispro as compared to patients with no hepatic dysfunction. However, some studies with human insulin have shown increased circulating levels of insulin in patients with liver failure. Careful glucose monitoring and dose adjustments of insulin, including insulin lispro, may be necessary in patients with hepatic dysfunction.
Race
The effects of race on the pharmacokinetics and pharmacodynamics of insulin lispro have not been studied.
Obesity
The effect of obesity on the pharmacokinetics and pharmacodynamics of insulin lispro has not been studied.
Pregnancy
The effect of pregnancy on the pharmacokinetics and pharmacodynamics of insulin lispro has not been studied.
Smoking
The effect of smoking on the pharmacokinetics and pharmacodynamics of insulin lispro has not been studied.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- Standard 2-year carcinogenicity studies in animals have not been performed. In Fischer 344 rats, a 12-month repeat-dose toxicity study was conducted with insulin lispro at subcutaneous doses of 20 and 200 units/kg/day (approximately 3 and 32 times the human subcutaneous dose of 1 unit/kg/day, based on units/body surface area). Insulin lispro did not produce important target organ toxicity including mammary tumors at any dose.
- Insulin lispro was not mutagenic in the following genetic toxicity assays: bacterial mutation, unscheduled DNA synthesis, mouse lymphoma, chromosomal aberration and micronucleus assays.
- Male fertility was not compromised when male rats given subcutaneous insulin lispro injections of 5 and 20 units/kg/day (0.8 and 3 times the human subcutaneous dose of 1 unit/kg/day, based on units/body surface area) for 6 months were mated with untreated female rats. In a combined fertility, perinatal, and postnatal study in male and female rats given 1, 5, and 20 units/kg/day subcutaneously (0.16, 0.8, and 3 times the human subcutaneous dose of 1 unit/kg/day, based on units/body surface area), mating and fertility were not adversely affected in either gender at any dose.
Animal Toxicology and/or Pharmacology
In standard biological assays in fasted rabbits, 0.2 unit/kg of insulin lispro injected subcutaneously had the same glucose-lowering effect and had a more rapid onset of action as 0.2 unit/kg of regular human insulin.
Clinical Studies
The safety and efficacy of HUMALOG were studied in children, adolescent, and adult patients with type 1 diabetes (n=789) and adult patients with type 2 diabetes (n=722).
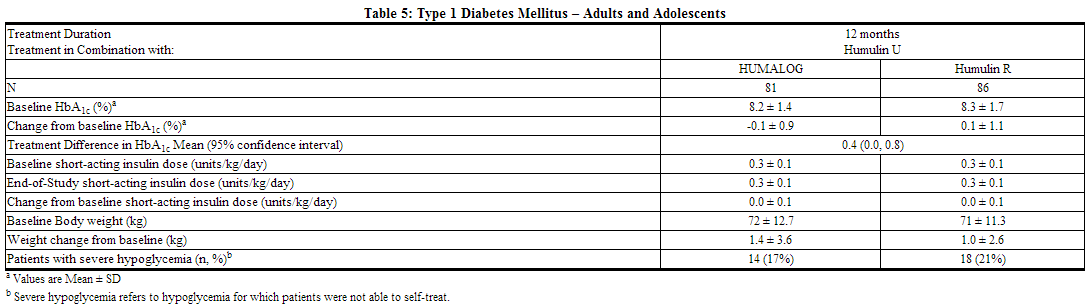
Type 1 Diabetes – Adults and Adolescents
A 12-month, randomized, parallel, open-label, active-controlled study was conducted in patients with type 1 diabetes to assess the safety and efficacy of insulin lispro (n=81) compared with regular human insulin injection, USP (rDNA origin) (n=86). Insulin lispro was administered by subcutaneous injection immediately prior to meals and regular human insulin was administered 30 to 45 minutes before meals. Long acting human insulin (rDNA origin) extended zinc suspension was administered once or twice daily as the basal insulin. There was a 2- to 4-week run-in period with reguar human insulin and long acting human insulin before randomization. Most patients were Caucasian (97%). Forty-seven percent of the patients were male. The mean age was 31 years (range 12 to 70 years). Glycemic control, the total daily doses of insulin lispro and regular human insulin, and the incidence of severe hypoglycemia (as determined by the number of events that were not self-treated) were similar in the two treatment groups. There were no episodes of diabetic ketoacidosis in either treatment group.
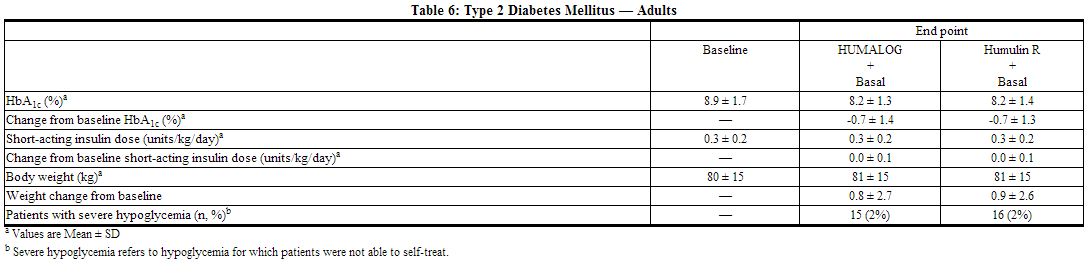
Type 2 Diabetes – Adults
A 6-month randomized, crossover, open-label, active-controlled study was conducted in insulin-treated patients with type 2 diabetes (n=722) to assess the safety and efficacy of insulin lispro for 3 months followed by reguar human insulin for 3 months or the reverse sequence. Insulin lispro was administered by subcutaneous injection immediately before meals and reguar human insulin was administered 30 to 45 minutes before meals. NPH human insulin (rDNA origin) isophane suspension or long acting human insulin was administered once or twice daily as the basal insulin. All patients participated in a 2- to 4-week run-in period with reguar human insulin and NPH human insulin or long acting human insulin. Most of the patients were Caucasian (88%), and the numbers of men and women in each group were approximately equal. The mean age was 58.6 years (range 23.8 to 85 years). The average body mass index (BMI) was 28.2 kg/m2. During the study, the majority of patients used NPH human insulin (84%) compared with long acting human insulin (16%) as their basal insulin. The reductions from baseline in HbA1c and the incidence of severe hypoglycemia (as determined by the number of events that were not self-treated) were similar between the two treatments from the combined groups (see Table 6).
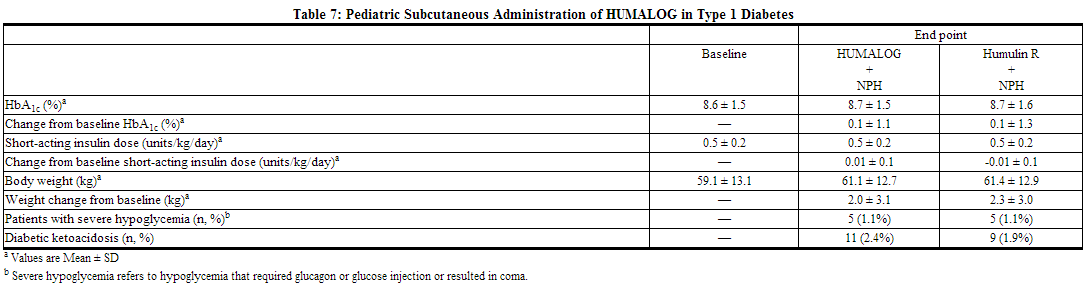
Type 1 Diabetes – Pediatric and Adolescents
An 8-month, crossover study of adolescents with type 1 diabetes (n=463), aged 9 to 19 years, compared two subcutaneous multiple-dose treatment regimens: insulin lispro or reguar human insulin, both administered with NPH human insulin as the basal insulin. Insulin lispro achieved glycemic control comparable to reguar human insulin, as measured by HbA1c (see Table 7), and both treatment groups had a comparable incidence of hypoglycemia. In a 9-month, crossover study of prepubescent children (n=60) with type 1 diabetes, aged 3 to 11 years, insulin lispro administered immediately before meals, insulin lispro administered immediately after meals and reguar human insulin administered 30 minutes before meals resulted in similar glycemic control, as measured by HbA1c, and incidence of hypoglycemia, regardless of treatment group.
Type 1 Diabetes – Adults Continuous Subcutaneous Insulin Infusion
To evaluate the administration of insulin lispro via external insulin pumps, two open-label, crossover design studies were performed in patients with type 1 diabetes. One study involved 39 patients, ages 19 to 58 years, treated for 24 weeks with insulin lispro or regular human insulin. After 12 weeks of treatment, the mean HbA1c values decreased from 7.8% to 7.2% in the insulin lispro-treated patients and from 7.8% to 7.5% in the regular human insulin-treated patients. Another study involved 60 patients (mean age 39, range 15 to 58 years) treated for 24 weeks with either insulin lispro or buffered regular human insulin. After 12 weeks of treatment, the mean HbA1c values decreased from 7.7% to 7.4% in the insulin lispro-treated patients and remained unchanged from 7.7% in the buffered regular human insulin-treated patients. Rates of hypoglycemia were comparable between treatment groups in both studies.
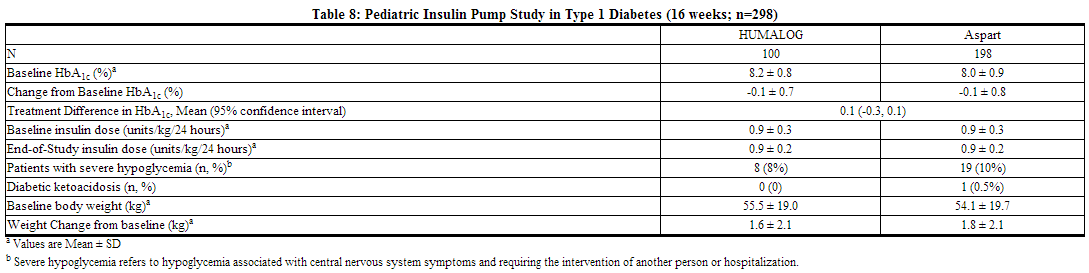
Type 1 Diabetes – Pediatric Continuous Subcutaneous Insulin Infusion
A randomized, 16-week, open-label, parallel design, study of children and adolescents with type 1 diabetes (n=298) aged 4 to 18 years compared two subcutaneous infusion regimens administered via an external insulin pump: insulin aspart (n=198) or insulin lispro (n=100). These two treatments resulted in comparable changes from baseline in HbA1c and comparable rates of hypoglycemia after 16 weeks of treatment (see Table 8). Infusion site reactions were similar between groups.
How Supplied
HUMALOG 100 units per mL (U-100) is available as:
- 10 mL vials, NDC 0002-7510-01 (VL-7510)
- 3 mL vials, NDC 0002-7510-17 (VL-7533)
- 5 x 3 mL cartridges1, NDC 0002-7516-59 (VL-7516)
- 5 x 3 mL Humalog KwikPen (prefilled), NDC 0002-8799-59 (HP-8799)
Storage
Do not use after the expiration date
Unopened insulin lispro should be stored in a refrigerator (36° to 46°F [2° to 8°C]), but not in the freezer. Do not use insulin lispro if it has been frozen. In-use insulin lispro vials, cartridges, and insulin lispro KwikPen should be stored at room temperature, below 86°F (30°C) and must be used within 28 days or be discarded, even if they still contain insulin lispro. Protect from direct heat and light. See table below:
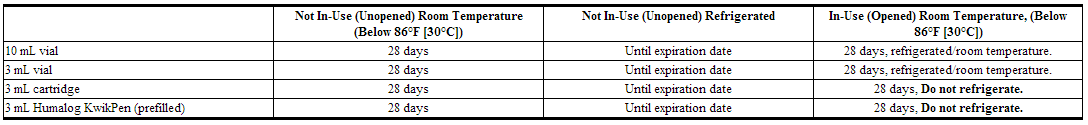
Use in an External Insulin Pump
Change the insulin lispro in the reservoir at least every 7 days, change the infusion sets and the infusion set insertion site at least every 3 days or after exposure to temperatures that exceed 98.6°F (37°C). A insulin lispro 3 mL cartridge used in the D-Tron pumps should be discarded after 7 days, even if it still contains insulin lispro. However, as with other external insulin pumps, the infusion set should be replaced and a new infusion set insertion site should be selected at least every 3 days.
Diluted Insulin Lispro for Subcutaneous Injection
Diluted insulin lispro may remain in patient use for 28 days when stored at 41°F (5°C) and for 14 days when stored at 86°F (30°C). Do not dilute insulin lispro contained in a cartridge or insulin lispro used in an external insulin pump.
Preparation and Handling
Diluted Lnsulin Lispro for Subcutaneous Injection: Insulin lispro may be diluted with Sterile Diluent for insulin lispro for subcutaneous injection. Diluting one part insulin lispro to nine parts diluent will yield a concentration one-tenth that of insulin lispro (equivalent to U-10). Diluting one part HUMALOG to one part diluent will yield a concentration one-half that of HUMALOG (equivalent to U-50).
Admixture for Intravenous Administration
Infusion bags prepared with insulin lispro are stable when stored in a refrigerator (2° to 8°C [36° to 46°F]) for 48 hours and then may be used at room temperature for up to an additional 48 hours.
Images
Drug Images
{{#ask: Page Name::Insulin lispro |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Insulin lispro |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Instructions for All Patients
Patients should be instructed on self-management procedures including glucose monitoring, proper injection technique, and management of hypoglycemia and hyperglycemia. Patients must be instructed on handling of special situations such as intercurrent conditions (illness, stress, or emotional disturbances), an inadequate or skipped insulin dose, inadvertent administration of an increased insulin dose, inadequate food intake, and skipped meals. Refer patients to the insulin lispro Patient Information Leaflet for additional information.
Women with diabetes should be advised to inform their doctor if they are pregnant or are contemplating pregnancy.
Accidental mix-ups between insulin lispro and other insulins have been reported. To avoid medication errors between insulin lispro and other insulins, patients should be instructed to always check the insulin label before each injection.
For Patients Using Continuous Subcutaneous Insulin Pumps
Patients using external pump infusion therapy should be trained appropriately. The following insulin pumps have been tested in insulin lispro clinical trials conducted by Eli Lilly and Company.
- Disetronic® H-Tron® plus V100, D-Tron® and D-Tronplus® with Disetronic Rapid infusion sets2
- MiniMed® Models 506, 507 and 508 and Polyfin® infusion sets3
Insulin lispro is recommended for use in pump systems suitable for insulin infusion such as MiniMed, Disetronic, and other equivalent pumps. Before using insulin lispro in a pump system, read the pump label to make sure the pump is indicated for continuous delivery of fast-acting insulin. insulin lispro is recommended for use in any reservoir and infusion sets that are compatible with insulin and the specific pump. Please see recommended reservoir and infusion sets in the pump manual.
To avoid insulin degradation, infusion set occlusion, and loss of the preservative (metacresol), insulin in the reservoir should be replaced at least every 7 days; infusion sets and infusion set insertion sites should be changed at least every 3 days.
Insulin exposed to temperatures higher than 98.6°F (37°C) should be discarded. The temperature of the insulin may exceed ambient temperature when the pump housing, cover, tubing or sport case is exposed to sunlight or radiant heat. Infusion sites that are erythematous, pruritic, or thickened should be reported to the healthcare professional, and a new site selected because continued infusion may increase the skin reaction or alter the absorption of insulin lispro.
Pump or infusion set malfunctions or insulin degradation can lead to rapid hyperglycemia and ketosis. This is especially pertinent for rapid acting insulin analogs that are more rapidly absorbed through skin and have a shorter duration of action. Prompt identification and correction of the cause of hyperglycemia or ketosis is necessary. Problems include pump malfunction, infusion set occlusion, leakage, disconnection or kinking, and degraded insulin. Less commonly, hypoglycemia from pump malfunction may occur. If these problems cannot be promptly corrected, patients should resume therapy with subcutaneous insulin injection and contact their healthcare professionals.
Precautions with Alcohol
Alcohol may increase or reduce the blood-glucose-lowering effect of insulin lispro.
Brand Names
- Humalog
- Lispro-PFC
Look-Alike Drug Names
- Humalog - Humuin
- Humalog - Novolog
- Humapen - Humira Pen
Drug Shortage
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ Nathan DM, Cleary PA, Backlund JY, Genuth SM, Lachin JM, Orchard TJ; et al. (2005). "Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes". N Engl J Med. 353 (25): 2643–53. doi:10.1056/NEJMoa052187. PMC 2637991. PMID 16371630. Review in: ACP J Club. 2006 May-Jun;144(3):63
- ↑ Abraira C, Colwell J, Nuttall F, Sawin CT, Henderson W, Comstock JP; et al. (1997). "Cardiovascular events and correlates in the Veterans Affairs Diabetes Feasibility Trial. Veterans Affairs Cooperative Study on Glycemic Control and Complications in Type II Diabetes". Arch Intern Med. 157 (2): 181–8. PMID 9009975.
- ↑ 3.0 3.1 3.2 Ohkubo Y, Kishikawa H, Araki E, Miyata T, Isami S, Motoyoshi S; et al. (1995). "Intensive insulin therapy prevents the progression of diabetic microvascular complications in Japanese patients with non-insulin-dependent diabetes mellitus: a randomized prospective 6-year study". Diabetes Res Clin Pract. 28 (2): 103–17. PMID 7587918.
- ↑ 4.0 4.1 4.2 Shichiri M, Kishikawa H, Ohkubo Y, Wake N (2000). "Long-term results of the Kumamoto Study on optimal diabetes control in type 2 diabetic patients". Diabetes Care. 23 Suppl 2: B21–9. PMID 10860187.
{{#subobject:
|Label Page=Insulin lispro |Label Name=InsulinLisproPackage1.png
}}
{{#subobject:
|Label Page=Insulin lispro |Label Name=InsulinLisproPackage2.png
}}
{{#subobject:
|Label Page=Insulin lispro |Label Name=InsulinLisproPackage3.png
}}