Hereditary elliptocytosis pathophysiology
|
Hereditary elliptocytosis Microchapters |
|
Differentiating Hereditary elliptocytosis from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Hereditary elliptocytosis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Hereditary elliptocytosis pathophysiology |
|
Risk calculators and risk factors for Hereditary elliptocytosis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Niyousha Danesh M.D., M.P.H
Overview
Hereditary elliptocytosis (HE) includes inherited a spectrum of red blood cell (RBC) disorders, that present heterogeneity in clinical symptoms, biochemistry and genetics. All of the Hereditary elliptocytosis subtypes have the elliptical morphologic shape RBCs in common, which leads to reduced RBC survival.[1]
Quality and quantity defects of the cytoskeletal proteins are responsible in Hereditary elliptocytosis. These cytoskeletal proteins are necessary for maintenance of RBCs structure, specially their biconcave morphology.[2]
Pathophysiology
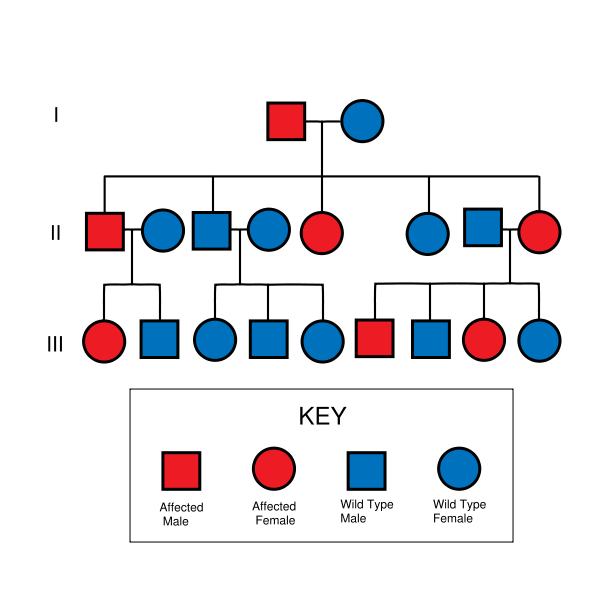
Hereditary elliptocytosis is commonly inherited as autosomal dominant. The only exception is autosomal recessive inheritance of hereditary pyropoikilocytosis (HPP). The spontaneous mutations occurs rarely. [3]
As we mentioned hereditary elliptocytosis is caused by cytoskeletal proteins defects. In this disease the protein scaffolding in the inner side of RBC is influenced and results in defective RBCs membrane
The RBC membrane consists of a lipid bilayer and a protein cytoskeleton, which increase RBC resistance, Spectrin is one of the main part of this scaffold and has 2 chains, alpha and beta. Separate genes encode alpha and beta chains and after being twisted together, they create an elongated heterodimer. These heterodimers build tetramers in the head part and they are linked to other cytoskeletal proteins at the tail regien,protein 4.1 and actin. Then protein 4.1 and actin bind to glycophorin A, band 3, and glycophorin C, the transmembrane proteins, connecting the scaffold to the lipid bilayer.
Mutations involved in the pathogenesis of HE can occur in each one of the cytoskeletal proteins,such as spectrins, band 4.1 or glycophorin C. [4]
These mutations affect mainly alpha- and beta-spectrin,impairing of the spectrin heterodimer formation. The combination of heterodimer and the lipid anchoring complex can also be influenced.
Some mutations alter the quantity of glycophorin C, namely Leach phenotype.
Various point mutations have been reported in some families, which present clinical variation of HE.
Normal erythrocytes are 7 microns, biconcave and have central pallor. They remain in the blood circulation for 120 days and they can maintain their elastic recoil and their discoid shape after passing through the capillaries in microcirculation , yet the elliptical shape of RBCs reduces the elasticity of RBCs, so their discoid shape is damaged and their ability to pass through 2 micron capillaries is reduced, so they are trapped and removed by the spleen. The reduction in surface to volume ratio of RBCs and their premature destruction leads to extravascular hemolysis and the clinical signs and symptoms of these disease.[5]
References
- ↑ Da Costa L, Galimand J, Fenneteau O, Mohandas N (2013). "Hereditary spherocytosis, elliptocytosis, and other red cell membrane disorders". Blood Rev. 27 (4): 167–78. doi:10.1016/j.blre.2013.04.003. PMID 23664421.
- ↑ Mohandas N, Gallagher PG (2008). "Red cell membrane: past, present, and future". Blood. 112 (10): 3939–48. doi:10.1182/blood-2008-07-161166. PMC 2582001. PMID 18988878.
- ↑ Harper SL, Sriswasdi S, Tang HY, Gaetani M, Gallagher PG, Speicher DW (2013). "The common hereditary elliptocytosis-associated α-spectrin L260P mutation perturbs erythrocyte membranes by stabilizing spectrin in the closed dimer conformation". Blood. 122 (17): 3045–53. doi:10.1182/blood-2013-02-487702. PMC 3811177. PMID 23974198.
- ↑ Mohandas N, Gallagher PG (2008). "Red cell membrane: past, present, and future". Blood. 112 (10): 3939–48. doi:10.1182/blood-2008-07-161166. PMC 2582001. PMID 18988878.
- ↑ Christensen RD, Nussenzveig RH, Reading NS, Agarwal AM, Prchal JT, Yaish HM (2014). "Variations in both α-spectrin (SPTA1) and β-spectrin ( SPTB ) in a neonate with prolonged jaundice in a family where nine individuals had hereditary elliptocytosis". Neonatology. 105 (1): 1–4. doi:10.1159/000354884. PMID 24193021.