Epididymoorchitis pathophysiology
|
Epididymoorchitis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Epididymoorchitis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Epididymoorchitis pathophysiology |
|
Risk calculators and risk factors for Epididymoorchitis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Dima Nimri, M.D. [2]
Overview
Epididymoorchitis refers to the inflammation of the epididymis and/or testes, with or without infection. While the pathogenesis is not fully understood, infectious epididymoorchitis is thought to be due to retrograde reflux of infected urine into the epididymis, which then spreads to the testes.[1][2]
Pathophysiology
Pathogenesis
Epididymoorchitis refers to the inflammation of the epididymis and/or testes, with or without infection. While the pathogenesis is not fully understood, the following are the proposed mechanisms behind epididymoorchitis:[1][2]
- The retrograde ascent of infectious pathogens is the usual route of infection. Most cases of epididymoorchitis start with inflammation of the epididymis (i.e., epididymitis), which then spread to the adjacent testicle (i.e., orchitis). Because orchitis tends to occur in patients with concurrent epididymitis, cases are mostly referred to as epididymoorchitis.
- Isolated cases of orchitis are usually due to mumps virus and in isolated cases of orchitis, blood-borne dissemination is the usual route of infection.
- Retrograde flow of infected urine into the ejaculatory duct is thought to cause epididymoorchitis.
- For infectious cases of epididymoorchitis that are not associated with an STD or UTI, it is believed that these cases may be related a post-infectious inflammatory reaction. When taking viral cultures of throat, stool and urine, it was found that patients with epididymoorchitis had elevated titers to certain pathogens, as compared to controls. Most notably, patients with epididymoorchitis had elevated titers to M. pneumonia and adenovirus.
- The mechanism behind non-infectious epididymoorchitis remains unclear.
Gross Pathology
-
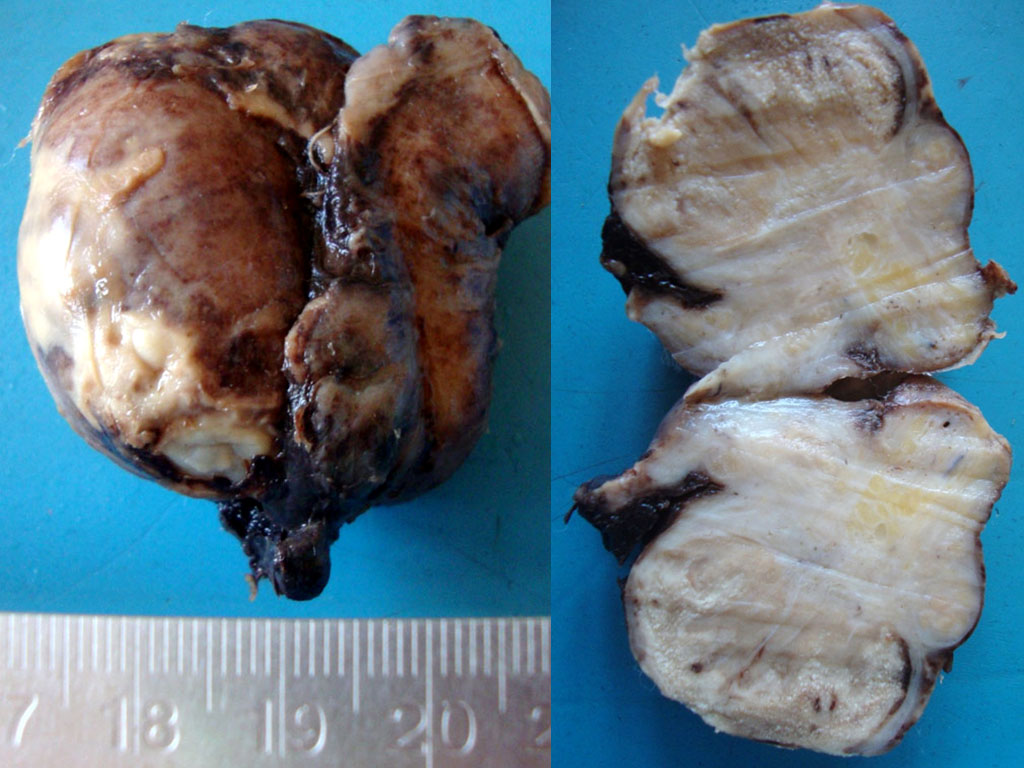
Image on the left shows evidence of acute inflammation and exudates on the surface of the testicle. Image to the right is a cut section showing exudates and dense fibrosis in the epididymis. Adapted from https://commons.wikimedia.org/wiki/Category:Gross_pathology_of_epididymo-orchitis#/media/File:Acute_epidydimoorchitis_Gross_Pathology.jpg. Accessed on Jan 3rd, 2017.
-
Cut-section through the testicle following orchidectomy showing a lesion in the epidydimis with fibrosis and caseous necrosis, following chronic epididymoorchitis caused by Mycobacterium tuberculosis. Adapted from https://commons.wikimedia.org/wiki/Category:Gross_pathology_of_tuberculous_epididymo-orchitis#/media/File:Tuberculous_epididymoorchitis_gross_pathology.jpg. Accessed on Jan 3rd, 2017.
Microscopic Pathology
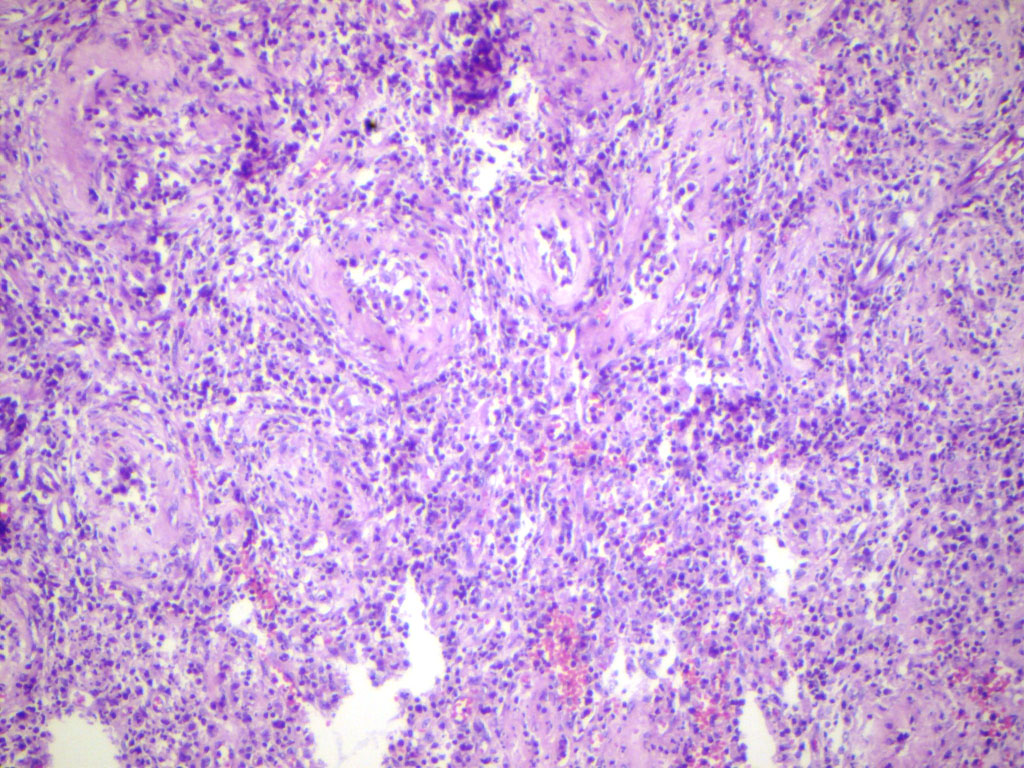
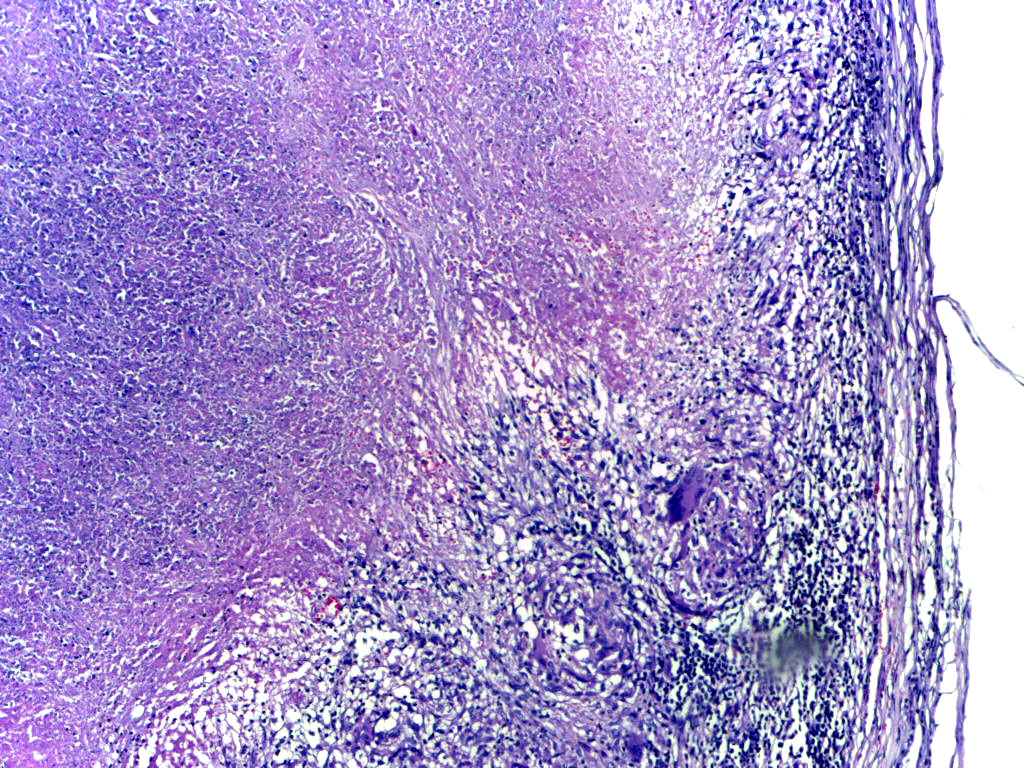
Acute epididymoorchitis is characterized by infiltration of neutrophils. Chronic cases of epididymoorchitis, such as in sarcoidosis or tuberculosis, are characterized by granulomatous inflammation.
-
Microscopy showing hyalinised residual seminiferous tubules and dense infilitrate of neutrophils. Adapted from https://commons.wikimedia.org/wiki/Category:Histopathology_of_epididymo-orchitis#/media/File:Suppurative_epidydimo_orchitis_histopathology.jpg. Accessed on Jan 3rd, 2017.
-
Low-power microscopy showing tuberculous epididymitis; caseous necrosis surrounded by epithelioid cells and giant cells with a mantle of lymphocytes. Adapted from https://commons.wikimedia.org/wiki/Category:Histopathology_of_tuberculous_epididymitis#/media/File:Tuberculous_epididymitis_Low_Power.jpg. Accessed on Jan 3rd, 2017.
Associated Conditions
The following conditions may be associated with epididymoorchitis:[1]
- Sexually transmitted diseases, such as N. gonorrhea and C. trachomatis
- Mumps infection may be associated with isolated cases of orchitis
- Anatomic abnormalities of the urinary tract, such as prostatic obstruction in older men (e.g., benign prostatic hyperplasia (BPH), prostatic cancer, urethral strictures)[2] and posterior urethral valves or meatal stenosis in young, prepubertal boys
References
- ↑ 1.0 1.1 1.2 Trojian TH, Lishnak TS, Heiman D (2009). "Epididymitis and orchitis: an overview". Am Fam Physician. 79 (7): 583–7. PMID 19378875.
- ↑ 2.0 2.1 2.2 Tracy CR, Steers WD, Costabile R (2008). "Diagnosis and management of epididymitis". Urol. Clin. North Am. 35 (1): 101–8, vii. doi:10.1016/j.ucl.2007.09.013. PMID 18061028.