Eluxadoline
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Martin Nino [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Eluxadoline is a mu-opioid receptor agonist that is FDA approved for the treatment of adults with irritable bowel syndrome with diarrhea (IBS-D). Common adverse reactions include constipation, nausea and abdominal pain (>5%)..
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indications
Eluxadoline is indicated in adults for the treatment of irritable bowel syndrome with diarrhea (IBS-D).
Dosage
The recommended dosage of Eluxadoline is 100 mg taken orally twice daily with food.
The recommended dosage of Eluxadoline is 75 mg taken orally twice daily with food in patients who:
- do not have a gallbladder.
- are unable to tolerate the 100 mg dose of Eluxadoline.
- are receiving concomitant OATP1B1 inhibitors.
- have mild (Child-Pugh Class A) or moderate (Child-Pugh Class B) hepatic impairment.
Discontinue Eluxadoline in patients who develop severe constipation for more than 4 days.
Instruct patients if they miss a dose, take the next dose at the regular time and not to take 2 doses at the same time to make up for a missed dose.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Eluxadoline in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Eluxadoline in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Safety and effectiveness in pediatric patients have not been established.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Eluxadoline in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Eluxadoline in pediatric patients.
Contraindications
Eluxadoline is contraindicated in patients with:
- Known or suspected biliary duct obstruction; or sphincter of Oddi disease or dysfunction. These patients are at increased risk for sphincter of Oddi spasm.
- Alcoholism, alcohol abuse or alcohol addiction, or in patients who drink more than 3 alcoholic beverages per day. These patients are at increased risk for acute pancreatitis.
- A history of pancreatitis; or structural diseases of the pancreas, including known or suspected pancreatic duct obstruction. These patients are at increased risk for acute pancreatitis.
- Severe hepatic impairment (Child-Pugh Class C). These patients are at risk for significantly increased plasma concentrations of Eluxadoline.
- A history of chronic or severe constipation or sequelae from constipation, or known or suspected mechanical gastrointestinal obstruction. These patients may be at risk for severe complications of bowel obstruction.
Warnings
Given the mu-opioid receptor agonism of Eluxadoline, there is a potential for increased risk of sphincter of Oddi spasm, resulting in pancreatitis or hepatic enzyme elevation associated with acute abdominal pain (e.g., biliary-type pain) with Eluxadoline.
In clinical trials, sphincter of Oddi spasm occurred in less than 1% of patients receiving Eluxadoline. The majority of these patients presented within the first week of treatment and the event resolved on discontinuation of Eluxadoline. Patients without a gallbladder are at increased risk.
Consider alternative therapies before using Eluxadoline in patients without a gallbladder and evaluate the benefits and risks of Eluxadoline in these patients in the context of their symptom severity. The recommended dosage of Eluxadoline is 75 mg twice daily in patients without a gallbladder. If Eluxadoline is used in such a patient, inform them that they may be at increased risk for adverse reactions and monitor them for symptoms of sphincter of Oddi spasm, such as elevated liver transaminases associated with abdominal pain or pancreatitis, especially during the first few weeks of treatment.
Instruct patients to stop Eluxadoline and seek medical attention if they experience symptoms suggestive of sphincter of Oddi spasm such as acute worsening of abdominal pain, (e.g. acute epigastric or biliary [i.e., right upper quadrant] pain), that may radiate to the back or shoulder with or without nausea and vomiting, associated with elevations of pancreatic enzymes or liver transaminases. Do not restart Eluxadoline in patients who developed biliary duct obstruction or sphincter of Oddi spasm while taking Eluxadoline.
There is a potential for increased risk of pancreatitis, not associated with sphincter of Oddi spasm, when taking Eluxadoline. Additional cases of pancreatitis, not associated with sphincter of Oddi spasm, were reported in less than 1% of patients receiving Eluxadoline in clinical trials. The majority were associated with excessive alcohol intake. All pancreatic events, whether or not associated with sphincter of Oddi spasm, resolved upon discontinuation of Eluxadoline; patients did not have organ failure or local or systemic complications.
Instruct patients to avoid chronic or acute excessive alcohol use while taking Eluxadoline. Monitor for new or worsening abdominal pain that may radiate to the back or shoulder, with or without nausea and vomiting. Instruct patients to stop Eluxadoline and seek medical attention if they experience symptoms suggestive of pancreatitis such as acute abdominal or epigastric pain radiating to the back associated with elevations of pancreatic enzymes.
Adverse Reactions
Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Over 1700 patients with IBS-D have been treated with 75 or 100 mg of Eluxadoline twice daily in controlled trials. Exposures from placebo-controlled clinical trials in adult patients with IBS-D included 1391 exposed for 3 months, 1001 exposed for 6 months and 488 exposed for one year.
Demographic characteristics were comparable between the treatment groups. Data described below represent pooled data compared to placebo across the randomized trials.
In clinical trials, sphincter of Oddi spasm occurred in 0.2% (2/807) of patients receiving 75 mg and 0.8% (8/1032) of patients receiving 100 mg Eluxadoline twice daily.
- Among patients receiving 75 mg, 1/807 (0.1%) patient experienced a sphincter of Oddi spasm presenting with abdominal pain but with lipase elevation less than 3 times the upper limit of normal (ULN) and 1/ 807 (0.1%) patient experienced a sphincter of Oddi spasm manifested as elevated hepatic enzymes associated with abdominal pain.
- Among patients receiving 100 mg, 1/1032 (0.1%) patient experienced a sphincter of Oddi spasm manifested as pancreatitis and 7/1032 (0.7%) patients experienced sphincter of Oddi spasm manifested as elevated hepatic enzymes associated with abdominal pain.
In patients without a gallbladder, 2/165 (1.2%) and 8/184 (4.3%) of patients receiving 75 mg and 100 mg, respectively, experienced a sphincter of Oddi spasm vs 0/1317 (0%) in patients with a gallbladder who had received either 75 mg or 100 mg treatment.
Of those patients who experienced a sphincter of Oddi spasm, 80% (8/10) reported their first onset of symptoms within the first week of treatment. The case of sphincter of Oddi spasm-induced pancreatitis occurred within minutes of taking the first dose of Eluxadoline. No cases of sphincter of Oddi spasm occurred greater than 1 month after treatment onset. All events resolved upon discontinuation of Eluxadoline, with symptoms typically improved by the following day.
Additional cases of pancreatitis, not associated with sphincter of Oddi spasm, were reported in 2/807 (0.2%) of patients receiving 75 mg and 3/1032 (0.3%) of patients receiving 100 mg Eluxadoline twice daily in clinical trials. Of these 5 cases, 3 were associated with excessive alcohol intake, one was associated with biliary sludge, and in one case the patient discontinued Eluxadoline 2 weeks prior to the onset of symptoms. All pancreatic events resolved with lipase normalization upon discontinuation of Eluxadoline, with 80% (4/5) resolving within 1 week of treatment discontinuation. The case of sphincter of Oddi spasm-induced pancreatitis resolved within 24 hours of discontinuation.
Common Adverse Reactions
TABLE 1 provides the incidence of common adverse reactions reported in > 2% of IBS-D patients in either Eluxadoline treatment group and at an incidence greater than in the placebo group.
- Table 1: Common* Adverse Reactions in the Placebo-Controlled Studies in IBS-D Patients

VIBERZI: Eluxadoline's Brand name
Constipation was the most commonly reported adverse reaction in Eluxadoline-treated patients in these trials. Approximately 50% of constipation events occurred within the first 2 weeks of treatment while the majority occurred within the first 3 months of therapy. Rates of severe constipation were less than 1% in patients receiving 75 mg and 100 mg Eluxadoline. Similar rates of constipation occurred between the active and placebo arms beyond 3 months of treatment.
Adverse Reactions Leading to Discontinuation
Eight percent of patients treated with 75 mg, 8% of patients treated with 100 mg Eluxadoline and 4% of patients treated with placebo discontinued prematurely due to adverse reactions. In the Eluxadoline treatment groups, the most common reasons for discontinuation due to adverse reactions were constipation (1% for 75 mg and 2% for 100 mg) and abdominal pain (1% for both 75 mg and 100 mg). In comparison, less than 1% of patients in the placebo group withdrew due to constipation or abdominal pain.
Less Common Adverse Reactions
Adverse reactions that were reported in ≤ 2% of Eluxadoline-treated patients are listed below by body system.
- Gastrointestinal: gastroesophageal reflux disease
- General Disorders and administration site conditions: feeling drunk
- Investigations: increased AST
- Nervous system: sedation, somnolence
- Psychiatric disorders: euphoric mood
- Respiratory: asthma, bronchospasm, respiratory failure, wheezing
Postmarketing Experience
There is limited information regarding Eluxadoline Postmarketing Experience in the drug label.
Drug Interactions
The metabolism of Eluxadoline by CYP pathways has not been clearly established. In addition, the potential of Eluxadoline to inhibit CYP3A4 in the gut has not been established.
TABLES 2 and 3 include drugs which demonstrated a clinically important drug interaction with Eluxadoline or which potentially may result in clinically relevant interactions.
- Table 2: Established and Other Potentially Clinically Relevant Interactions Affecting Eluxadoline

VIBERZI: Eluxadoline's Brand name
- Table 3: Established and Other Potentially Clinically Relevant Interactions Affecting Drugs Co-Administered with Eluxadoline

VIBERZI: Eluxadoline's Brand name
Use in Specific Populations
Pregnancy
- Risk Summary
There are no studies with Eluxadoline in pregnant women that inform any drug-associated risks. The background risk of major birth defects and miscarriage for the indicated population is unknown. However, the background risk in the U.S. general population of major birth defects is 2 to 4% and of miscarriage is 15 to 20% of clinically recognized pregnancies. In animal reproduction studies, oral and subcutaneous administration of Eluxadoline to rats and rabbits during organogenesis at doses approximately 51 and 115 times the human exposure after a single oral dose of 100 mg, respectively, demonstrated no teratogenic effects. In a pre- and postnatal development study in rats, no adverse effects were observed in offspring with oral administration of Eluxadoline at doses approximately 10 times the human exposure.
- Data
- Animal Data
Eluxadoline administered as combined oral (1000 mg/kg/day) and subcutaneous (5 mg/kg/day) doses during the period of organogenesis to rats and rabbits (exposures about 51 and 115 times, respectively, the human AUC of 24 ng.h/mL after a single oral dose of 100 mg) did not cause any adverse effects on embryofetal development. A pre- and postnatal development study in rats showed no evidence of any adverse effect on pre- and postnatal development at oral doses of Eluxadoline up to 1000 mg/kg/day (with exposures about 10 times the human AUC of 24 ng.h/mL after a single oral dose of 100 mg). In the same study, Eluxadoline was detected in the milk of lactating rats administered oral doses of 100, 300 and 1000 mg/kg/day (with exposures about 1.8, 3 and 10 times, respectively, the human AUC of 24 ng.h/mL after a single oral dose of 100 mg). Milk samples were collected from six lactating females per group on lactation day 12. Mean concentrations of Eluxadoline in the milk of lactating rats on lactation day 12 were 2.78, 5.49 and 44.02 ng/mL at 100, 300 and 1000 mg/kg/day, respectively.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Eluxadoline in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Eluxadoline during labor and delivery.
Nursing Mothers
No data are available regarding the presence of Eluxadoline in human milk, the effects of Eluxadoline on the breastfed infant, or the effects of Eluxadoline on milk production. However, Eluxadoline is present in rat milk.
The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for Eluxadoline and any potential adverse effects on the breastfed infant from Eluxadoline or from the underlying maternal condition.
Pediatric Use
Safety and effectiveness in pediatric patients have not been established.
- Juvenile Toxicology Data
Eluxadoline was orally administered to juvenile rats at 500, 750, and 1500 mg/kg/day (about 16, 54 and 30 times, respectively, the human AUC of 24 ng.h/mL after a single oral dose of 100 mg) for 4 weeks. There were no adverse physiologic effects related to Eluxadoline. Based on these results, the NOAEL for male and female juvenile rats was 1500 mg/kg/day (about 30 times the human AUC of 24 ng.h/mL after a single oral dose of 100 mg).
Geriatic Use
Of 1795 IBS-D patients in clinical trials of Eluxadoline who received 75 mg or 100 mg twice daily, 139 (7.7%) were at least 65 years of age, while 15 (0.8%) were at least 75 years old. No overall differences in effectiveness were observed between these patients and younger patients. There were no overall differences in the types of adverse reactions observed between elderly and younger patients; however, a higher proportion of elderly patients than younger patients experienced adverse reactions (66% vs 59%), serious adverse reactions (9% vs 4%), and gastrointestinal adverse reactions (39% vs 28%).
Gender
There is no FDA guidance on the use of Eluxadoline with respect to specific gender populations.
Race
There is no FDA guidance on the use of Eluxadoline with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Eluxadoline in patients with renal impairment.
Hepatic Impairment
Plasma concentrations of Eluxadoline increase in patients with hepatic impairment.
Eluxadoline is contraindicated in patients with severe hepatic impairment (Child-Pugh Class C) as plasma concentrations of Eluxadoline increase significantly (16-fold) and there is no information to support the safety of Eluxadoline in these patients.
In patients with mild (Child-Pugh Class A) or moderate (Child-Pugh Class B) hepatic impairment, plasma concentrations of Eluxadoline increase to a lesser extent (6- and 4-fold, respectively). Administer Eluxadoline at a reduced dose of 75 mg twice daily to these patients. Monitor patients with any degree of hepatic impairment for impaired mental or physical abilities needed to perform potentially hazardous activities such as driving a car or operating machinery and for other Eluxadoline-related adverse reactions.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Eluxadoline in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Eluxadoline in patients who are immunocompromised.
Administration and Monitoring
Administration
The recommended dosage of Eluxadoline is 100 mg taken orally twice daily with food.
The recommended dosage of Eluxadoline is 75 mg taken orally twice daily with food in patients who:
- do not have a gallbladder.
- are unable to tolerate the 100 mg dose of Eluxadoline.
- are receiving concomitant OATP1B1 inhibitors.
- have mild (Child-Pugh Class A) or moderate (Child-Pugh Class B) hepatic impairment.
Discontinue Eluxadoline in patients who develop severe constipation for more than 4 days.
Instruct patients if they miss a dose, take the next dose at the regular time and not to take 2 doses at the same time to make up for a missed dose.
Monitoring
There is limited information regarding Eluxadoline Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Eluxadoline and IV administrations.
Overdosage
No reports of overdosage with Eluxadoline have been reported.
In the event of acute overdose, the stomach should be emptied and adequate hydration maintained. The patient should be carefully observed and given standard supportive treatment as required. Given Eluxadoline's action at opioid receptors, administration of a narcotic mu-opioid antagonist, such as naloxone, should be considered. Considering the short half-life of naloxone, repeated administration may be necessary. In the event of naloxone administration, subjects should be monitored closely for the return of overdose symptoms, which may indicate need for repeated naloxone injection.
DRUG ABUSE AND DEPENDENCE
- Controlled Substance
Eluxadoline is listed in Schedule IV of the Controlled Substances Act.
- Abuse
In a drug discrimination study in monkeys, intravenous administration of Eluxadoline hydrochloride produced full generalization to the morphine cue. In a self-administration study in monkeys, Eluxadoline hydrochloride was self-administered to a degree that was less than that of heroin but greater than that of saline.
Adverse reactions of euphoria and feeling drunk were reported in clinical trials of IBS-D evaluating 75 mg and 100 mg doses of Eluxadoline. The rate of euphoria was 0% for 75 mg and 0.2% (2/1032) for 100 mg and the rate of feeling drunk was 0.1% (1/807) for 75 mg and 0.1% (1/1032) for 100 mg.
In contrast, in two human abuse potential studies conducted in recreational opioid-experienced individuals, supratherapeutic oral doses of Eluxadoline (300 mg and/or 1000 mg) and intranasal doses of Eluxadoline (100 mg and/or 200 mg) produced the adverse reaction of euphoria (at a rate ranging from 14% to 28%) that was greater than that of placebo (0% to 5%) but less than that of oxycodone (44% to 76%). In the two human abuse potential studies, supratherapeutic oral and intranasal doses of Eluxadoline produced small but significant increases on positive subjective measures such as Drug Liking and High compared to placebo. Supratherapeutic oral and intranasal doses of Eluxadoline also produced small but significant increases on negative subjective measures such as Drug Disliking and Dysphoria compared to placebo. In the same studies, oxycodone (30 mg and 60 mg oral, and 15 and 30 mg intranasal) produced significantly greater responses on positive and negative subjective measures than those produced by Eluxadoline and placebo.
- Dependence
In studies with monkeys and rats in which Eluxadoline and Eluxadoline hydrochloride were chronically administered, discontinuation of the drug did not lead to behavioral signs of withdrawal, a measure of physical dependence. However, the ability of Eluxadoline hydrochloride in monkeys to induce self-administration suggests that the drug is sufficiently rewarding to produce reinforcement. In two human abuse potential studies with Eluxadoline conducted in recreational opioid-experienced individuals, euphoria was reported at a rate of 14% to 28%. These data suggest that Eluxadoline may produce psychological dependence.
Pharmacology
| |
| |
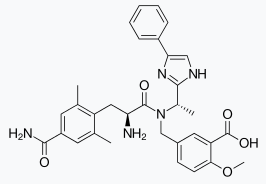
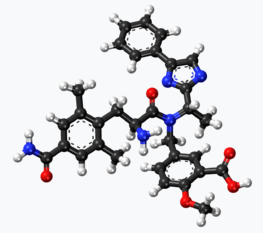
Eluxadoline
| |
| Systematic (IUPAC) name | |
| 5-({[(2S)-2-amino-3-(4-carbamoyl-2,6-dimethylphenyl)propanoyl][(1S)-1-(4-phenyl-1H-imidazol-2-yl)ethyl]amino}methyl)-2-methoxybenzoic acid | |
| Identifiers | |
| CAS number | |
| ATC code | A07 |
| PubChem | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 569.6508 g/mol |
| SMILES | & |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Protein binding | 81% |
| Metabolism | ? |
| Half life | 3.7–6 hours |
| Excretion | 82.2% (feces), <1% (urine)[1] |
| Therapeutic considerations | |
| Pregnancy cat. |
? |
| Legal status | |
| Routes | Oral |
Mechanism of Action
Eluxadoline is a mu-opioid receptor agonist; Eluxadoline is also a delta opioid receptor antagonist and a kappa opioid receptor agonist. The binding affinities (Ki) of Eluxadoline for the human mu and delta opioid receptors are 1.8 nM and 430 nM, respectively. The binding affinity (Ki) of Eluxadoline for the human kappa opioid receptor has not been determined; however, the Ki for guinea pig cerebellum kappa opioid receptor is 55 nM. In animals, Eluxadoline interacts with opioid receptors in the gut.
Eluxadoline is available as 75 mg and 100 mg tablets for oral administration. In addition to the active ingredient, Eluxadoline, each tablet contains the following inactive ingredients: silicified microcrystalline cellulose, colloidal silica, crospovidone, mannitol, magnesium stearate, and Opadry II (partially hydrolyzed polyvinyl alcohol, titanium dioxide, polyethylene glycol, talc, iron oxide yellow, and iron oxide red).
Structure

Eluxadoline is available as 75 mg and 100 mg tablets for oral administration. In addition to the active ingredient, Eluxadoline , each tablet contains the following inactive ingredients: silicified microcrystalline cellulose, colloidal silica, crospovidone, mannitol, magnesium stearate, and Opadry II (partially hydrolyzed polyvinyl alcohol, titanium dioxide, polyethylene glycol, talc, iron oxide yellow, and iron oxide red).
Pharmacodynamics
At a dose 10 times the maximum recommended dose (100 mg), Eluxadoline does not prolong the QT interval to any clinically relevant extent.
Pharmacokinetics
Following oral administration of 100 mg Eluxadoline in healthy subjects, the Cmax of Eluxadoline was approximately 2 to 4 ng/mL and AUC was 12 to 22 ng.h/mL. Eluxadoline has approximately linear pharmacokinetics with no accumulation upon repeated twice daily dosing. The variability of Eluxadoline pharmacokinetic parameters ranges from 51% to 98%.
Absolute bioavailability of Eluxadoline has not been determined. The median Tmax value was 1.5 hours (range: 1 to 8 hours) under fed conditions and 2 hours (range: 0.5 to 6 hours) under fasting conditions.
The administration of Eluxadoline with a high fat meal that contained approximately 800 to 1000 total calories, with 50% of calories being derived from fat content decreased the Cmax of Eluxadoline by 50% and AUC by 60%.
Plasma protein binding of Eluxadoline was 81%.
The mean plasma elimination half-life of Eluxadoline ranged from 3.7 hours to 6 hours.
Metabolism of Eluxadoline is not clearly established. There is evidence that glucuronidation can occur to form an acyl glucuronide metabolite.
Following a single oral dose of 300 mg [14C] Eluxadoline in healthy male subjects, 82.2% of the total radioactivity was recovered in feces within 336 hours and less than 1% was recovered in urine within 192 hours.
Specific Populations
Following a single oral 100–mg dose in subjects with varying degrees of liver impairment and healthy subjects, mean Eluxadoline plasma exposure was 6-fold, 4-fold, and 16-fold higher in mild, moderate, and severe hepatically impaired subjects (Child Pugh Class A, B, C), respectively, compared to the subjects with normal liver function.
Drug Interactions
- In Vitro Assessment of Drug Interactions
In vitro studies indicate that Eluxadoline is neither an inducer of CYP1A2, CYP2C9, CYP2C19, and CYP3A4, nor an inhibitor of CYP1A2, CYP2A6, CYP2B6, CYP2C9, CYP2C19, CYP3A4 and CYP2D6 at clinically relevant systemic concentrations. Although CYP2E1 was slightly inhibited by Eluxadoline (IC50 of approximately 20 micromolar [11 mcg/mL]), clinically meaningful interactions are unlikely. The in vitro studies were not adequate to establish the potential for Eluxadoline to inhibit CYP3A4 in the gut.
In vitro studies suggest that Eluxadoline is a substrate for OAT3, OATP1B1, BSEP and MRP2, but not for OCT1, OCT2, OAT1, OATP1B3, P-gp and BCRP. Based on the in vitro studies, clinically meaningful interaction via inhibition of OCT1, OCT2, OAT1, OAT3, OATP1B3, BSEP and MRP2 by Eluxadoline is unlikely. However, the in vitro studies were not adequate to establish the potential for eluxadoline to inhibit P-gp in the gut.
- In Vivo Assessment of Drug Interactions
The following drug interactions were studied in healthy subjects:
Coadministration of multiple doses of 100 mg Eluxadoline with multiple dose administration of an oral contraceptive (norethindrone 0.5 mg/ethinyl estradiol 0.035 mg) does not change the exposure of either drug.
Coadministration of a single dose of 100 mg Eluxadoline with a single dose of 600 mg cyclosporine resulted in 4.4-fold and 6.2-fold increase in AUC and Cmax of Eluxadoline, respectively, compared to administration of Eluxadoline alone.
Coadministration of a single dose of 100 mg Eluxadoline with a single dose of 500 mg probenecid resulted in a 35% and 31% increase in Eluxadoline AUC and Cmax, respectively, compared to administration of Eluxadoline alone. This change in Eluxadoline exposures is not expected to be clinically meaningful.
Coadministration of multiple doses of 100 mg Eluxadoline twice daily with a single dose 20 mg rosuvastatin resulted in an increase in the AUC (40%) and Cmax (18%) of rosuvastatin compared to administration of rosuvastatin alone. Similar results were observed with the active, major metabolite, n-desmethyl rosuvastatin.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
Two-year oral carcinogenicity studies have been conducted with Eluxadoline in CD-1 mice at doses up to 1500 mg/kg/day (about 14 times the human AUC of 24 ng.h/mL after a single oral dose of 100 mg) and in Sprague Dawley rats at oral doses up to 1500 mg/kg/day (about 36 times the human AUC of 24 ng.h/mL after a single oral dose of 100 mg). Oral administration of Eluxadoline for 104 weeks did not produce tumors in mice and rats.
Eluxadoline was negative in the Ames test, chromosome aberration test in human lymphocytes, in the mouse lymphoma cell (L5178Y/TK+/-) forward mutation test and in the in vivo rat bone marrow micronucleus test.
- Impairment of Fertility
Eluxadoline at oral doses up to 1000 mg/kg/day (about 10 times the human AUC of 24 ng.h/mL after a single oral dose of 100 mg) was found to have no adverse effect on fertility and reproductive performance of male and female rats.
Clinical Studies
The efficacy and safety of Eluxadoline in IBS-D patients was established in two randomized, multi-center, multi-national, double-blind, placebo-controlled trials (Studies 1 and 2). A total of 1281 patients in Study 1 and 1145 patients in Study 2 received treatment with Eluxadoline 75 mg, Eluxadoline 100 mg or placebo twice daily [overall, patients had a mean age of 45 years (range 18 to 80 years with 10% at least 65 years of age or older), 66% female, 86% white, 11% black, and 27% Hispanic].
All patients met Rome III criteria for IBS-D (loose [mushy] or watery stools ≥25% and hard or lumpy stools <25% of bowel movements) and were required to meet both of the following criteria:
- an average of worst abdominal pain scores in the past 24 hours of >3.0 on a 0 to 10 scale over the week prior to randomization.
- an average daily stool consistency score (Bristol Stool Scale or BSS) of ≥5.5 and at least 5 days with a BSS score ≥5 on a 1 to 7 scale over the week prior to randomization.
Pertinent exclusion criteria included: prior pancreatitis, alcohol abuse, cholecystitis prior 6 months, sphincter of Oddi dysfunction, inflammatory bowel disease, intestinal obstruction, gastrointestinal infection or diverticulitis within prior 3 months, lipase greater than 2 xULN, ALT or AST greater than 3 xULN.
Study 1 and Study 2 included identical 26-week double-blind, placebo-controlled treatment periods. Study 1 continued double-blinded for an additional 26 weeks for long-term safety (total of 52 weeks of treatment), followed by a 2-week follow-up. Study 2 included a 4-week single-blinded, placebo-withdrawal period upon completion of the 26-week treatment period. During the double-blind treatment phase and the single-blinded placebo withdrawal phase, patients were allowed to take loperamide rescue medication for the acute treatment of uncontrolled diarrhea, but were not allowed to take any other antidiarrheal, antispasmodic agent or rifaximin for their diarrhea. Additionally, patients were allowed to take aspirin-containing medications or nonsteroidal anti-inflammatory drugs, but no narcotic or opioid containing agents.
Efficacy of Eluxadoline was assessed in both trials using an overall composite responder primary endpoint. The primary endpoint was defined by the simultaneous improvement in the daily worst abdominal pain score by ≥30% as compared to the baseline weekly average AND a reduction in the BSS to <5 on at least 50% of the days within a 12-week time interval. Improvement in daily worst abdominal pain in the absence of a concurrent bowel movement was also considered a response day. Results for endpoints were based on electronic daily diary entries by patients.
The proportion of composite responders over 12 weeks is shown in TABLE 4. In both trials, the proportion of patients who were composite responders to Eluxadoline was statistically significantly higher than placebo for both doses. The proportion of patients who were composite responders to Eluxadoline was similar for male and female patients in both trials.
- Table 4: Efficacy Results in Randomized Clinical Trials

VIBERZI: Eluxadoline's Brand name
Additionally, the proportion of patients who were composite responders to Eluxadoline at each 4-week interval was numerically higher than placebo for both doses as early as month 1 through month 6 demonstrating that efficacy is maintained throughout the course of treatment.
During the 4 week single-blind withdrawal period in Study 2, no evidence of worsening of diarrhea or abdominal pain compared to baseline was demonstrated at either dose.
How Supplied
Eluxadoline is available as:
- 75 mg tablets: capsule-shaped tablets, coated in pale-yellow to light tan color, debossed with “FX75” on one side.
Bottle of 60: NDC 61874-075-60
- 100 mg tablets: capsule-shaped tablets, coated in pink-orange to peach color, debossed with “FX100” on one side.
Bottle of 60: NDC 61874-100-60
Storage
Store Eluxadoline tablets at 20°C to 25°C (68°F to 77°F) with excursions permitted to 15°C to 30°C (59°F to 86°F).
Images
Drug Images
{{#ask: Page Name::Eluxadoline |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel


{{#ask: Label Page::Eluxadoline |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling.
Instruct patients to:
- stop Eluxadoline and seek medical attention if unusual or severe abdominal pain develops, especially if they do not have a gallbladder.
- avoid chronic or acute excessive alcohol use while taking Eluxadoline.
- take one tablet twice daily with food.
- if they miss a dose, take the next dose at the regular time. Do not take 2 doses at the same time to make up for a missed dose.
- call their healthcare provider if they are unable to tolerate Eluxadoline.
- discontinue Eluxadoline and call their health care provider if they experience constipation lasting more than 4 days
- not take alosetron with Eluxadoline or not take loperamide on a chronic basis with Eluxadoline due to the potential for constipation. Loperamide may occasionally be used with Eluxadoline for acute management of severe diarrhea, but must be discontinued if constipation develops. Also, instruct patients to avoid taking Eluxadoline with other medications that may cause constipation (for example opioids, anticholinergics, etc.).
Precautions with Alcohol
- Eluxadoline is contraindicated in patients with alcoholism, alcohol abuse, alcohol addiction, or drink more than 3 alcoholic beverages/day.
- Avoid chronic or acute excessive alcohol use while taking Eluxadoline.
Brand Names
VIBERZI™
Look-Alike Drug Names
There is limited information regarding Eluxadoline Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ "Viberzi (eluxadoline) Tablets, for Oral Use, CIV. Full Prescribing Information". Actavis Pharma, Inc. Parsippany, NJ 07054 USA. Retrieved 26 December 2015.