Dysphagia endoscopy
Jump to navigation
Jump to search
|
Dysphagia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Dysphagia endoscopy On the Web |
|
American Roentgen Ray Society Images of Dysphagia endoscopy |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Hamid Qazi, MD, BSc [2], Feham Tariq, MD [3]
Overview
FEES and VFSS may be helpful in the diagnosis of dysphagia. The FEES uses a transnasal laryngoscope, and swallowing is directly evaluated by using measured quantities of food colored with blue liquid dye and compared before and after swallowing.
Endoscopy
Flexible fiberoptic endoscopic examination of swallowing (FEES)
Indications
FEES is indicated in
- In critically ill patients.
- Patients who cannot be transferred to the fluoroscopy room.
- Patients who require prompt evaluation.
Procedure
- A scope is passed through the nasal cavity to evaluate nasopharynx, laryngopharynx, and hypopharynx.
- If no structural abnormalities are seen, pharyngeal response is tested before and after swallowing.
- A normal endoscopy is followed by manometry.
Interpretation of FEES
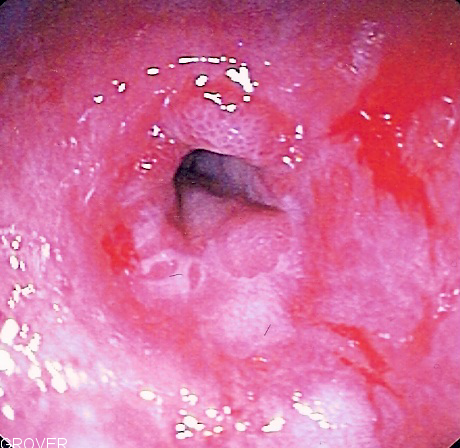
The endoscopy findings for dysphagia are as follows:[1][2]
- Middle and lower biopsies of the esophagus should be taken with the intention of excluding eosinophilic esophagitis.
- Majority will be normal or demonstrates only mild erosive disease.
- Structural abnormalities
- Strictures
- GERD
- Webs/Rings
References
- ↑ Philpott, Hamish; Garg, Mayur; Tomic, Dunya; Balasubramanian, Smrithya; Sweis, Rami (2017). "Dysphagia: Thinking outside the box". World Journal of Gastroenterology. 23 (38): 6942–6951. doi:10.3748/wjg.v23.i38.6942. ISSN 1007-9327.
- ↑ Scheurer U (1991). "[Dysphagia]". Ther Umsch. 48 (3): 150–61. PMID 2042117.