Amantadine (Gocovri)
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sonya Gelfand, Anmol Pitliya, M.B.B.S. M.D.[2]
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Amantadine (Gocovri) is a weak uncompetitive antagonist of the NMDA receptor that is FDA approved for the treatment of dyskinesia in patients with Parkinson’s disease receiving levodopa-based therapy, with or without concomitant dopaminergic medications. Common adverse reactions include hallucination, dizziness, dry mouth, peripheral edema, constipation, fall, and orthostatic hypotension.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indication
- Amantadine is indicated for the treatment of dyskinesia in patients with Parkinson’s disease receiving levodopa-based therapy, with or without concomitant dopaminergic medications.
Dosing Information
- The initial daily dosage of amantadine is 137 mg, administered orally once daily at bedtime. After one week, increase to the recommended dosage of 274 mg (two 137 mg capsules) once daily at bedtime.
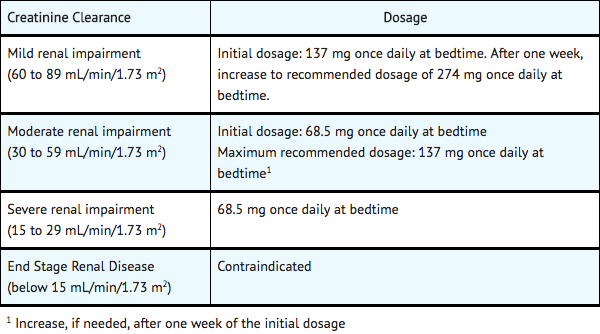
Dosing in Patients with Renal Impairment
- The initial and maximum recommended daily dosage of amantadine for patients with renal impairment (creatinine clearance estimated by Modification of Diet in Renal Disease (MDRD) method) is provided below.
Discontinuation and Missed Dose
- Rapid dose reduction or withdrawal of amantadine may cause adverse reactions. Therefore, to stop amantadine in patients who have been on the drug for more than 4 weeks, their dose should typically, if possible, be reduced by half for their final week of dosing.
- If a dose of amantadine is missed, the next dose should be taken as scheduled.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding amantadine Off-Label Guideline-Supported Use and Dosage (Adult) in the drug label.
Non–Guideline-Supported Use
There is limited information regarding amantadine Off-Label Non-Guideline-Supported Use and Dosage (Adult) in the drug label.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding Amantadine (Gocovri) FDA-Labeled Indications and Dosage (Pediatric) in the drug label.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding amantadine Off-Label Guideline-Supported Use and Dosage (Pediatric) in the drug label.
Non–Guideline-Supported Use
There is limited information regarding amantadine Off-Label Non-Guideline-Supported Use and Dosage (Pediatric) in the drug label.
Contraindications
- Amantadine is contraindicated in patients with end stage renal disease (ie., creatinine clearance below 15 mL/min/1.73 m2).
Warnings
Falling Asleep During Activities of Daily Living and Somnolence
- Patients treated for Parkinson’s disease have reported falling asleep while engaged in activities of daily living, including the operation of motor vehicles, which sometimes has resulted in accidents. Patients may not perceive warning signs, such as excessive drowsiness, or they may report feeling alert immediately prior to the event. In controlled clinical trials, somnolence and fatigue were reported as adverse reactions in 4% of patients treated with amantadine 274 mg and 1% for placebo.
- Before initiating treatment with amantadine, advise patients of the potential to develop drowsiness and specifically ask about factors that may increase the risk for somnolence with amantadine, such as concomitant sedating medications or the presence of a sleep disorder. If a patient develops daytime sleepiness or episodes of falling asleep during activities that require full attention (e.g., driving a motor vehicle, conversations, eating), amantadine should ordinarily be discontinued.
- If a decision is made to continue amantadine, patients should be advised not to drive and to avoid other potentially dangerous activities. There is insufficient information to establish that dose reduction will eliminate episodes of falling asleep while engaged in activities of daily living or daytime somnolence.
Suicidality and Depression
- In controlled clinical trials, suicidal ideation or suicide attempt was reported in 2% of amantadine-treated patients and 0% of placebo-treated patients. Depression or depressed mood was reported in 6% of amantadine-treated patients and 1% of placebo-treated patients. Confusional state was reported in 3% of amantadine-treated patients and 2% of placebo-treated patients. Apathy was reported in 2% of amantadine-treated patients and 0% of placebo-treated patients.
- Monitor patients for depression, including suicidal ideation or behavior. Prescribers should consider whether the benefits outweigh the risks of treatment with amantadine in patients with a history of suicidality or depression.
Hallucinations/Psychotic Behavior
- Patients with a major psychotic disorder should ordinarily not be treated with amantadine because of the risk of exacerbating psychosis. In controlled trials, the incidence of patients who experienced visual hallucination, auditory hallucination, delusions, illusions, or paranoia was 25% in patients treated with amantadine 274 mg and 3% in placebo-treated patients. Hallucinations caused discontinuation of treatment in 8% of amantadine-treated patients and 0% of placebo-treated patients.
- Observe patients for the occurrence of hallucinations throughout treatment, especially at initiation and after dose increases.
Dizziness and Orthostatic Hypotension
- In controlled clinical trials, 29% of amantadine-treated patients and 2% of placebo-treated patients experienced dizziness, syncope, orthostatic hypotension, presyncope, postural dizziness or hypotension. In amantadine-treated patients, 3% discontinued study treatment because of dizziness, postural dizziness, or syncope, compared to 0% of placebo-treated patients.
- Monitor patients for dizziness and orthostatic hypotension, especially after starting amantadine or increasing the dose. Concomitant use of alcohol when using amantadine is not recommended.
Withdrawal-Emergent Hyperpyrexia and Confusion
- A symptom complex resembling neuroleptic malignant syndrome (characterized by elevated temperature, muscular rigidity, altered consciousness, and autonomic instability), with no other obvious etiology, has been reported in association with rapid dose reduction, withdrawal of, or changes in drugs that increase central dopaminergic tone.
- Abrupt discontinuation of amantadine may cause an increase in the symptoms of Parkinson’s disease or cause delirium, agitation, delusions, hallucinations, paranoid reaction, stupor, anxiety, depression, or slurred speech. It is recommended to avoid sudden discontinuation of amantadine.
Impulse Control/Compulsive Behaviors
- Patients can experience intense urges to gamble, increased sexual urges, intense urges to spend money, binge eating, and/or other intense urges, and the inability to control these urges while taking one or more of the medications, including amantadine, that increase central dopaminergic tone. In some cases, these urges were reported to have stopped when the dose was reduced or the medication was discontinued. Because patients may not recognize these behaviors as abnormal, it is important for prescribers to specifically ask patients or their caregivers about the development of new or increased gambling urges, sexual urges, uncontrolled spending, or other urges while being treated with amantadine. Consider dose reduction or stopping the medication if a patient develops such urges while taking amantadine.
Adverse Reactions
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Placebo-Controlled Trials
- Amantadine was evaluated in two double-blind, placebo-controlled efficacy trials of similar design and population: Study 1 (123 patients) and Study 2 (75 patients). The study population was approximately 56% male and 94% white, with a mean age of 65 years (age range from 34 years to 82 years). The mean duration of levodopa-induced dyskinesia was 4 years (range 0.1 to 14 years). Active treatment started at 137 mg once daily for one week, followed by a dose increase to 274 mg once daily. The treatment duration was 25 weeks for Study 1 and 13 weeks for Study 2. Of the 100 patients in the safety population described below, 39 patients were treated with amantadine for 24 weeks. The safety data for these trials were pooled.
- The most common adverse reactions reported in >10% of amantadine-treated patients and more frequently than on placebo were: hallucination, dizziness, dry mouth, peripheral edema, constipation, falls, and orthostatic hypotension.
- The overall rate of discontinuation because of adverse reactions for amantadine-treated patients was 20%, compared to 8% for placebo-treated patients. Adverse reactions that led to treatment discontinuation in at least 2% of patients were hallucination (8% amantadine vs. 0% placebo), dry mouth (3% amantadine vs. 0% placebo), peripheral edema (3% amantadine vs. 0% placebo), blurred vision (amantadine 3% vs. 0% placebo), postural dizziness and syncope (amantadine 2% vs. 0% placebo), abnormal dreams (amantadine 2% vs. 1% placebo), dysphagia (amantadine 2% vs. 0% placebo), and gait disturbance (amantadine 2% vs. 0% placebo).
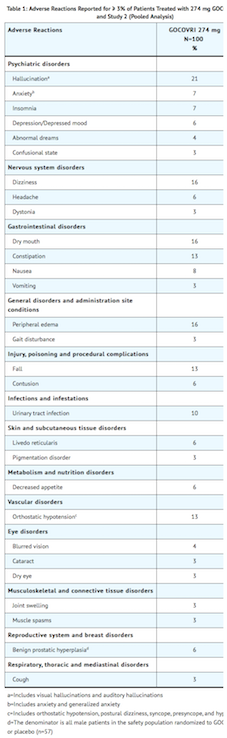
- Other clinically relevant adverse reactions observed at <3% included somnolence, fatigue, suicide ideation or attempt, apathy, delusions, illusions, and paranoia.
Difference in the Frequency of Adverse Reactions by Gender
- Adverse reactions reported more frequently in women treated with 274 mg of amantadine (n=46), compared to men (n=54), were: dry mouth (22% women, 11% men), nausea (13% women, 4% men), livedo reticularis (13% women, 0% men), abnormal dreams (9% women, 0% men) and cataracts (7% women, 0% men).
- Men treated with 274 mg of amantadine reported the following adverse reactions more frequently than women: dizziness (20% men, 11% women), peripheral edema (19% men, 11% women), anxiety (11% men, 2% women), orthostatic hypotension (7% men, 2% women) and gait disturbance (6% men, 0% women).
Difference in the Frequency of Adverse Reactions by Age
- Hallucinations (visual or auditory) were reported in 31% of amantadine-treated patients age 65 years and over (n=52), compared to 10% in patients below the age of 65 years (n=48). Falls were reported in 17% of amantadine-treated patients age 65 and over, compared to 8% of patients below age 65. Orthostatic hypotension was reported in 8% of patients age 65 and over, compared to 2% of patients below age 65.
Postmarketing Experience
There is limited information regarding Amantadine (Gocovri) Postmarketing Experience in the drug label.
Drug Interactions
- Other Anticholinergic Drugs
- Drugs Affecting Urinary pH
- Live Attenuated Influenza Vaccines
- Alcohol
Other Anticholinergic Drugs
- Products with anticholinergic properties may potentiate the anticholinergic-like side effects of amantadine. The dose of anticholinergic drugs or of amantadine should be reduced if atropine-like effects appear when these drugs are used concurrently.
Drugs Affecting Urinary pH
- The pH of the urine has been reported to influence the excretion rate of amantadine. Urine pH is altered by diet, drugs (e.g., carbonic anhydrase inhibitors, sodium bicarbonate), and clinical state of the patient (e.g., renal tubular acidosis or severe infections of the urinary tract).
- Since the excretion rate of amantadine increases rapidly when the urine is acidic, the administration of urine acidifying drugs may increase the elimination of the drug from the body. Alterations of urine pH towards the alkaline condition may lead to an accumulation of the drug with a possible increase in adverse reactions. Monitor for efficacy or adverse reactions under conditions that alter the urine pH to more acidic or alkaline, respectively.
Live Attenuated Influenza Vaccines
- Because of its antiviral properties, amantadine may interfere with the efficacy of live attenuated influenza vaccines. Therefore, live vaccines are not recommended during treatment with amantadine. Inactivated influenza vaccines may be used, as appropriate.
Alcohol
- Concomitant use with alcohol is not recommended, as it may increase the potential for CNS effects such as dizziness, confusion, lightheadedness, and orthostatic hypotension, and may result in dose-dumping.
Use in Specific Populations
Pregnancy
Risk Summary
- There are no adequate data on the developmental risk associated with use of amantadine in pregnant women. Animal studies suggest a potential risk for fetal harm with amantadine. In mice and rats, adverse developmental effects (embryolethality, increased incidence of malformations, and reduced fetal body weight) were observed when amantadine was administered to pregnant animals at clinically relevant doses.
- In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively. The background risk for major birth defects and miscarriage in patients with Parkinson’s disease is unknown.
Data (Animal)
- The effects of amantadine on development have not been tested in studies conducted in animals using currently recommended methodology; however, developmental toxicity studies of amantadine have been reported in the published literature.
- In mice, oral administration of amantadine (0, 10, or 40 mg/kg/day) to pregnant animals during organogenesis (gestation days 7-12) resulted in embryolethality and reduced fetal body weight at the highest dose tested, which was associated with maternal toxicity. The no-effect dose for developmental toxicity in mice (10 mg/kg/day) is less than the recommended human dose (RHD) of 274 mg/day, based on body surface area (mg/m2).
- In rats, oral administration of amantadine (0, 40 or 120 mg/kg/day) to pregnant animals during organogenesis (gestation days 7-12) resulted in embryolethality and reduced fetal body weight at the highest dose. The no-effect dose for developmental toxicity in this study (40 mg/kg/day) is approximately equal to the RHD on a mg/m2 basis.
- In another study in pregnant rats, oral administration of amantadine during organogenesis (gestation days 7-14) resulted in an increase in visceral and skeletal malformations at oral doses of 50 and 100 mg/kg/day. The no-effect dose for teratogenicity in this study (37 mg/kg/day) is approximately equal to the RHD on a mg/m2 basis.
- Evaluation of parturition, lactation, and post-natal development in a limited number of litters from the mouse and rat studies described above revealed reductions in live litter size and pup weights at birth at 40 mg/kg/day in mice and 120 mg/kg/day in rats.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Amantadine (Gocovri) in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Amantadine (Gocovri) during labor and delivery.
Nursing Mothers
Risk Summary
- Amantadine is excreted into human milk, but amounts have not been quantified. There is no information on the risk to a breastfed infant.
- Amantadine may alter breast milk production or excretion.
- The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for amantadine and any potential adverse effects on the breastfed infant from amantadine or from the underlying maternal condition.
Data
- In published studies, amantadine reduced serum prolactin levels and the symptoms of galactorrhea in patients taking neuroleptic drugs. The effect of amantadine on milk supply has not been evaluated in nursing mothers.
Pediatric Use
- The safety and effectiveness of amantadine in pediatric patients have not been established.
Geriatic Use
- The majority of people with Parkinson’s disease are 65 years and older. In Phase 3 clinical trials, the mean age of patients at study entry was 65 years. Of the total number of patients in clinical studies of amantadine, 46% were less than 65 years of age, 39% were 65-74 years of age, and 15% were 75 years of age or older.
- Hallucinations and falls occurred more frequently in patients 65 years of age or older, compared to those less than 65 years of age.
- No dose adjustment is recommended on the basis of age. Amantadine is known to be substantially excreted by the kidney, and the risk of adverse reactions may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
Gender
There is no FDA guidance on the use of Amantadine (Gocovri) with respect to specific gender populations.
Race
There is no FDA guidance on the use of Amantadine (Gocovri) with respect to specific racial populations.
Renal Impairment
- Amantadine is contraindicated for use in patients with end-stage renal disease (creatinine clearance lower than 15 mL/min/1.73 m2).
- For patients with moderate renal impairment (creatinine clearance between 30 and 59 mL/min/1.73 m2), a 50% dose reduction of amantadine dosage to a starting daily dose of 68.5 mg daily at bedtime for a week, to a maximum dosage of 137 mg daily at bedtime is recommended.
- For patients with severe renal impairment (creatinine clearance between 15 and 29 mL/min/1.73 m2), a daily dose of 68.5 mg at bedtime is the recommended initial and maximum dosage.
- Creatinine clearance values are estimated by the Modification of Diet in Renal Disease (MDRD) method.
Hepatic Impairment
There is no FDA guidance on the use of Amantadine (Gocovri) in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Amantadine (Gocovri) in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Amantadine (Gocovri) in patients who are immunocompromised.
Administration and Monitoring
Administration
- Amantadine should be swallowed whole. Do not crush, chew or divide capsules. If needed, amantadine may be administered by carefully opening and sprinkling the entire contents on a small amount (teaspoonful) of soft food, such as applesauce. The drug/food mixture should be swallowed immediately without chewing. Do not store mixture for future use.
- Amantadine can be taken with or without food.
- Concomitant use of amantadine with alcohol is not recommended.
- It is recommended to avoid sudden discontinuation of amantadine
Monitoring
- Influenza A virus infection: Reduction of signs and symptoms of influenza may be indicative of efficacy.
- Parkinson disease or drug induced extrapyramidal reactions: Reduction of extrapyramidal movements, rigidity, tremor, and gait disturbances may be indicative of efficacy.
- Changes in efficacy or adverse reactions: IN patients with conditions that change the urine pH (eg, renal tubular acidosis, severe infections of urinary tract, concomitant carbonic anhydrase inhibitors or sodium bicarbonate).
- Depression, including suicidal behavior or ideation.
- Hallucinations: Particularly during therapy initiation and dosage increase.
- History of congestive heart failure or peripheral edema.
- History of seizures and epileptic patients for possible increased seizure activity.
- New or increased gambling, sexual or other intense urges.
- Orthostatic hypotension and dizziness: Particularly after starting therapy or dosage increase.
- Signs or symptoms of neuroleptic malignant syndrome: During dosage reductions or discontinuation of therapy, especially if the patient is receiving neuroleptics.
- Skin examinations for the detection of melanoma: Frequently and on a regular basis during use.
IV Compatibility
There is limited information regarding the compatibility of Amantadine (Gocovri) and IV administrations.
Overdosage
- Deaths have been reported from overdose with amantadine. The lowest reported acute lethal dose was 1 gram of amantadine hydrochloride (equivalent to 0.8 g amantadine). Acute toxicity may be attributable to the anticholinergic effects of amantadine. Drug overdose has resulted in cardiac, respiratory, renal, or central nervous system toxicity. Pulmonary edema and respiratory distress (including adult respiratory distress syndrome, ARDS) have been reported with amantadine; renal dysfunction, including increased BUN and decreased creatinine clearance, can occur.
- Central nervous system effects that have been reported with overdose include agitation, aggressive behavior, hypertonia, hyperkinesia, ataxia, tremor, disorientation, depersonalization, fear, delirium, psychotic reactions, lethargy, and coma. Seizures may be exacerbated in patients with prior history of seizure disorders. Hyperthermia has occurred with amantadine overdose.
- For acute overdosing, general supportive measures should be employed along with immediate gastric decontamination if appropriate. Give intravenous fluids if necessary. The excretion rate of amantadine increases with acidification of urine, which may increase the elimination of the drug. Monitor patients for arrhythmias and hypotension. Electrocardiographic monitoring may be needed after ingestion because arrhythmias have been reported after overdose, including arrhythmias with fatal outcomes. Adrenergic agents, such as isoproterenol, in patients with an amantadine overdose has been reported to induce arrhythmias.
- Monitor blood electrolytes, urine pH, and urinary output. Although amantadine is not efficiently removed by hemodialysis, this procedure may be useful in the treatment of amantadine toxicity in patients with renal failure.
Pharmacology
| |
| Template:Px | |
Amantadine (Gocovri)
| |
| Systematic (IUPAC) name | |
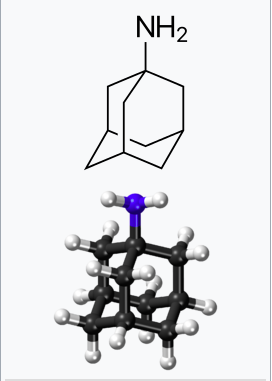
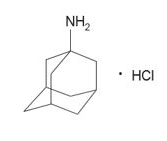
| Adamantan-1-amine | |
| Identifiers | |
| CAS number | |
| ATC code | N04 |
| PubChem | |
| DrugBank | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 151.249 g/mol |
| SMILES | & |
| Synonyms | 1-Adamantylamine |
| Pharmacokinetic data | |
| Bioavailability | 86–90% |
| Protein binding | 67% |
| Metabolism | Minimal (mostly to acetyl metabolites) |
| Half life | 10–31 hours |
| Excretion | Urine |
| Therapeutic considerations | |
| Pregnancy cat. | |
| Legal status |
Prescription Only (S4)(AU) ?(CA) POM(UK) [[Prescription drug|Template:Unicode-only]](US) |
| Routes | Oral |
Mechanism of Action
- The mechanism by which amantadine exerts efficacy in the treatment of dyskinesia in patients with Parkinson’s disease is unknown. Amantadine is a weak uncompetitive antagonist of the NMDA receptor. Amantadine has not been shown to possess direct anticholinergic activity in animal studies; however, it exhibits anticholinergic-like side effects such as dry mouth, urinary retention, and constipation in humans. Amantadine may have direct and indirect effects on dopamine neurons; it exerts dopaminergic-like side effects such as hallucinations and dizziness in humans.
Structure
Pharmacodynamics
- The effect of amantadine on QT prolongation was not studied in a dedicated thorough QT study.
- Alcohol consumption may increase the potential for CNS effects such as dizziness, confusion, lightheadedness, and orthostatic hypotension.
Pharmacokinetics
- Amantadine is an extended release formulation. The pharmacokinetics of amantadine from 68.5 mg, 137 mg, and 274 mg of amantadine are dose proportional in healthy subjects.
Absorption
- After a single dose bedtime administration of amantadine, the median Tmax for plasma amantadine was around 12 hours (range 6-20 hours). The steady-state concentrations of amantadine were achieved 4 days after the dose initiation. The steady-state total exposures (AUC0-tau) were 20-30% higher than after single dose, suggesting an accumulation ratio of 1.2-1.3.
Effect of Food
- A single dose crossover study of amantadine established the lack of effect of high-fat, high-calorie meal on plasma amantadine pharmacokinetics; additionally, administration of entire capsule contents sprinkled on applesauce also did not affect plasma amantadine pharmacokinetics.
Distribution
- The volume of distribution determined after the intravenous administration of amantadine to 15 healthy subjects was 3 to 8 L/kg, suggesting potential extravascular distribution. Amantadine is approximately 67% bound to plasma proteins over a concentration range of 0.1 to 2.0 µg/mL.
Elimination
- In a study with healthy volunteers after oral administration, the apparent plasma clearance of amantadine was estimated to be 0.27 ± 0.094 L/hr/kg (range 0.13 to 0.57 L/hr/kg). Amantadine is primarily excreted unchanged in the urine, and in a study of six healthy volunteers, the ratio of amantadine renal clearance to apparent plasma clearance was 0.79 ± 0.17 (mean ± SD). The mean plasma amantadine half-life at steady-state was approximately 16 hours.
Metabolism
- Eight metabolites of amantadine have been identified in human urine. One metabolite, an N-acetylated compound, was quantified in human urine and accounted for 0-15% of the administered dose in multiple studies. The contribution of this metabolite to efficacy or toxicity is not known.
Excretion
- Amantadine is primarily excreted unchanged in the urine by both glomerular filtration and tubular secretion.
Specific Population
Male/Female Patients
- In an integrated analysis of five studies in healthy volunteers (n=147), the mean total amantadine clearance following administration of amantadine, adjusted for body weight in kilograms, was 1.2 fold higher in males compared to females (95% CI: 1.1, 1.3, P=0.007). No dose adjustment by gender is warranted.
Renal Impairment
- The renal clearance of amantadine is significantly lower in adult patients with moderate or severe renal impairment, compared to healthy adults. Since the renal pathway is a major elimination pathway, impairment in renal function can result in significant accumulation in the plasma, warranting dose adjustment. The impact of renal impairment on dose adjustment was not investigated in a dedicated study.
- Based on PK simulations, the range of the total exposures (AUC0-tau) in subjects with normal renal function (creatinine clearance >90 mL/min/1.73 m2) or mild renal impairment (creatinine clearance between 60 and 89 mL/min/1.73 m2) were comparable for the same dosing regimen. However, patients with moderate renal impairment (creatinine clearance between 30 and 59 mL/min/1.73 m2) had higher exposures relative to patients with normal renal function or mild renal impairment. Severe renal impairment (creatinine clearance between 15 and 29 mL/min/1.73 m2) resulted in even higher total exposures. Dosage adjustment is recommended in patients with moderate and severe renal impairment. Amantadine is contraindicated in patients with end stage renal disease (creatinine clearance less than 15 mL/min/1.73 m2).
- Amantadine is inefficiently removed by hemodialysis.
Drug Interaction Studies
- The in-vitro dissolution-release profiles showed 52% drug release after 45 minutes, and up to 95% after 2 hours, at concentrations of 40% alcohol/0.1N HCl.
- In vitro studies indicate that amantadine has negligible or no inhibitory activity against cellular transporters (P-gp, BCRP, MATE2-K, OAT1, OAT3, OATP1B1, and OATP1B3) at plasma concentrations observed in patients with Parkinson’s disease on an amantadine 274 mg dose.
- In vitro studies in MDCK-II cells demonstrated that amantadine is not a substrate of the anionic transporters OAT1 or OAT3, or the cationic transporter MATE2-K. Amantadine was a poor substrate of the cationic transporters OCT2 and MATE1. Renal elimination of amantadine may be mediated in part by one or more organic cation transporters independent of OCT2. An in vivo study demonstrated that quinidine, a known organic cation transporter inhibitor, reduced amantadine clearance by approximately 33% in humans. The clinical significance is unknown. In vitro studies show that amantadine does not significantly inhibit the enzyme activity of drug metabolizing cytochrome P450 isoforms (CYP1A2, 2B6, 2C19, 2C8, 2C9, 2D6, 2E1, 3A4, and 3A5).
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
- Animal studies designed to evaluate the carcinogenic potential of amantadine have not been conducted.
Mutagenesis
- Amantadine was negative for genotoxicity in in vitro (Ames and mammalian cell [Chinese Hamster ovary and human peripheral blood lymphocytes]) assays in the presence or absence of metabolic activation and in an in vivo mouse bone marrow micronucleus assay.
Impairment of Fertility
- The effects of amantadine on fertility have not been adequately tested in a study in animals conducted according to current standards. In a reproduction study reported in the literature, oral administration of amantadine to male and female rats at a dose of 32 mg/kg/day resulted in impaired fertility. The no-effect dose for adverse effects on fertility (10 mg/kg/day) is less than the recommended human dose of 274 mg/day on a mg/m2 basis.
Clinical Studies
Overview of Studies
- Amantadine for the treatment of dyskinesia in patients with Parkinson’s disease was assessed in two randomized, double-blind, placebo-controlled efficacy trials: Study 1 and Study 2. Key inclusion criteria in both studies included at least 1 hour of troublesome dyskinesia time during the day and at least mild functional impact because of dyskinesia.
- Study 1 was conducted in 121 (modified Intention to Treat (mITT) population) Parkinson’s disease patients with dyskinesia in the United States (US) and Canada. The duration of treatment in Study 1 was up to 25 weeks. Study 2 was conducted in 75 (mITT population) patients with dyskinesia in the US, Germany, France, Spain, and Austria. The duration of treatment was 13 weeks.
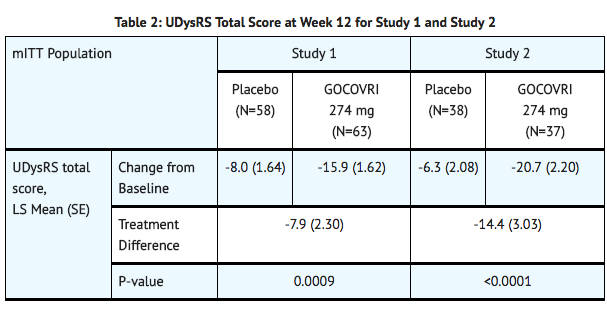
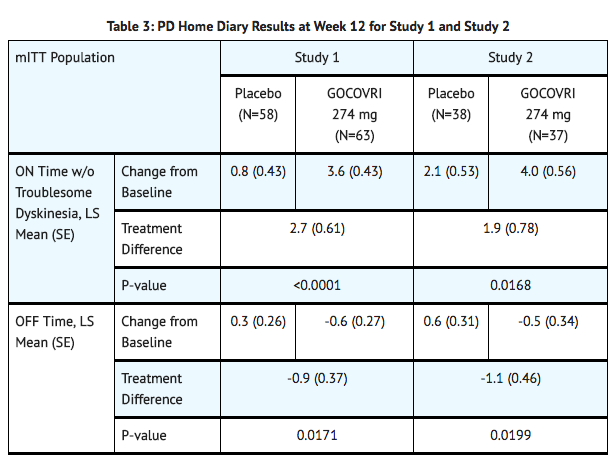
- In both studies, the primary efficacy endpoint was the change in total score of the Unified Dyskinesia Rating Scale (UDysRS) between baseline and Week 12. Key secondary endpoints derived from a Parkinson’s disease home diary included changes from baseline to Week 12 in ON time without troublesome dyskinesia and OFF time.
Study Population
- In Study 1 and Study 2, the mean age of patients at the time of Parkinson’s disease diagnosis was 55 years (range: 29-75 years).
- At baseline, patients had a mean UDysRS total score of 40.1 (range: 8-76), a mean duration of ON time without troublesome dyskinesia (Parkinson’s disease home diary) of 8.4 hours (range: 0-15.3), and a mean duration of OFF time of 2.8 hours (range: 0-9.5).
- Patients in Study 1 and Study 2 were treated with a stable dose of levodopa, with 32% of patients on levodopa monotherapy. Patients were also treated with concomitant dopamine agonists (54%) and/or MAO-B inhibitors (44%).
Study 1
- In Study 1, a significant decrease in mean UDysRS total score (reduction in dyskinesia) was observed at Week 12 in patients treated with amantadine, compared with placebo.
Study 2
- In Study 2, a significant decrease in mean UDysRS total score (reduction in dyskinesia) was observed at Week 12 in patients treated with amantadine, compared with placebo (TABLE 2).
- In Study 1 and Study 2, there was a significant increase in ON time without troublesome dyskinesia, and a significant decrease in OFF time between baseline and Week 12 in patients treated with amantadine, compared with placebo (TABLE 3).
How Supplied
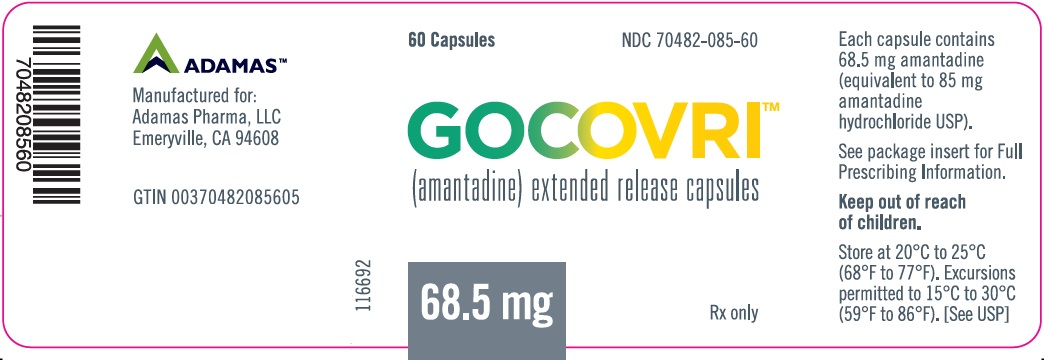
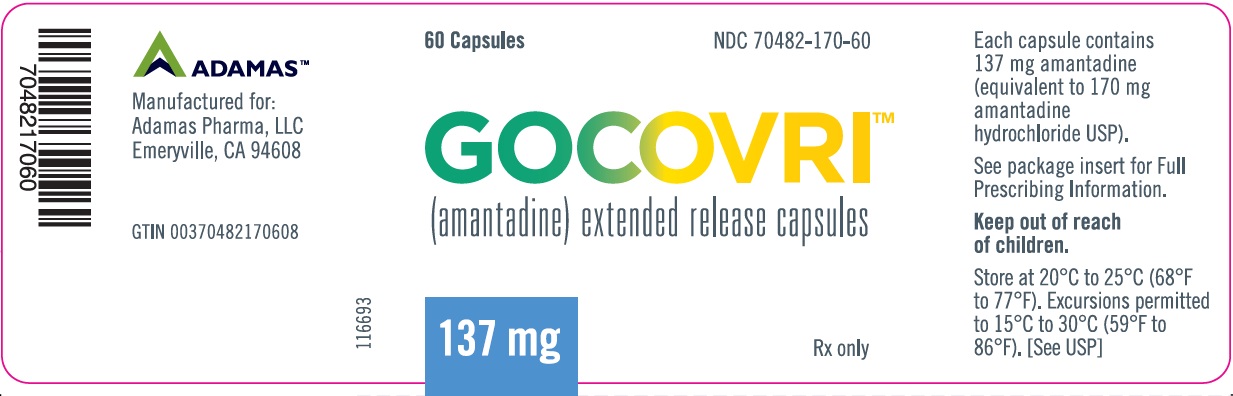
- Amantadine is supplied as extended release capsules in the following configurations:
- The 68.5 mg capsule is a white opaque size #2 capsule, with black printing of ‘ADAMAS’ on front and ‘85’ on back of the cap and three black bands printed on body of capsule.
- 60 count bottles NDC# 70482-085-60
- The 137 mg capsule is a light blue opaque size #0 capsule, with black printing of ‘ADAMAS’ on front and ‘170’ on back of the cap and three black bands printed on body of capsule.
- 60 count bottles NDC# 70482-170-60
Storage
- Store at 20°C to 25°C (68°F to 77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
Images
Drug Images
{{#ask: Page Name::Amantadine (Gocovri) |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
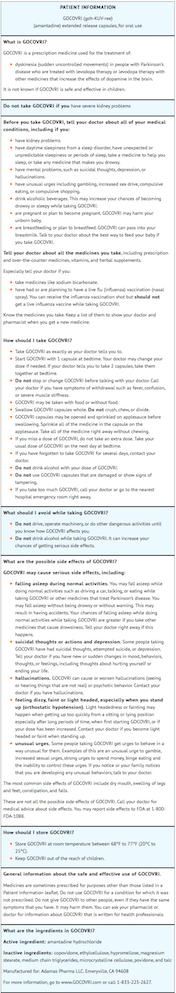
Package and Label Display Panel
{{#ask: Label Page::Amantadine (Gocovri) |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- Advise the patient to read the FDA-approved patient labeling (Patient Information).
Administration
- Instruct patients and caregivers that amantadine capsules should be swallowed whole and can be administered with or without food. Alternatively, amantadine capsules may be opened and the contents sprinkled on applesauce; the entire contents should be consumed immediately without chewing. Advise patients to speak to their healthcare provider before discontinuation of amantadine.
Falling Asleep During Activities of Daily Living
- Advise patients that sleepiness and fatigue that have been reported with amantadine and patients treated with Parkinson’s disease medications have reported falling asleep while engaged in activities of daily living. These adverse reactions may affect some patients’ ability to drive and operate machinery safely.
Suicidality and Depression
- Instruct patients, family members, and caregivers to notify their healthcare provider if depressed mood, depression, changes in behavior or thinking, and suicidal ideation or behavior develop during treatment.
Hallucinations/Psychotic Behavior
- Inform patients and caregivers that hallucinations and paranoia can occur while taking amantadine. Tell patients to report unreal visions, sounds, or sensations or other psychotic behavior to their healthcare provider promptly should they develop.
Dizziness and Orthostatic Hypotension
- An increased incidence of dizziness, orthostatic hypotension, and syncope was observed with administration of amantadine. Caution patients against standing rapidly after sitting or lying down, especially if they have been doing so for prolonged periods and especially at the initiation of treatment with amantadine.
Withdrawal-Emergent Hyperpyrexia and Confusion
- Advise patients to contact their healthcare provider before stopping amantadine. Tell patients to inform their healthcare provider if they develop withdrawal symptoms such as fever, confusion, or severe muscle stiffness.
Impulse Control/Compulsive Disorders
- Inform patients of the potential for experiencing intense urges to gamble, increased sexual urges, intense urges to spend money, binge eating, and other intense urges and the inability to control these urges while taking one or more of the medications that increase central dopaminergic tone, that are generally used for the treatment of Parkinson’s disease.
Drug Interactions
- Certain medications can cause an interaction with amantadine. Advise patients and/or caregivers to inform their healthcare provider of all the medicines the patient is taking, including over-the-counter medicines, dietary supplements, and herbal products. Inform patients that live influenza vaccines and consumption of alcohol are not recommended during treatment with amantadine.
Precautions with Alcohol
Alcohol-Amantadine (Gocovri) interaction has not been established. Talk to your doctor regarding the effects of taking alcohol with this medication.
Brand Names
- Gocovri
Look-Alike Drug Names
There is limited information regarding Amantadine (Gocovri) Look-Alike Drug Names in the drug label.
Drug Shortage
Price
References
The contents of this FDA label are provided by the National Library of Medicine.