Template:Hypercholesterolemia
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Jair Basantes de la Calle, M.D.
2018 AHA ACC Guideline on the Management of Blood Cholesterol. Primary Prevention
Primary Prevention Adults 40 to 75 Years of Age With LDL-C Levels 70 to 189 mg/dL (1.7 to 4.8 mmol/L)
| Class I
|
| "1. In adults at intermediate-risk, statin therapy reduces risk of ASCVD, and in the context of a risk discussion, if a decision is made for statin therapy, a moderate-intensity statin should be recommended (Level of Evidence: A) "
|
| "2. In intermediate-risk patients, LDL-C levels should be reduced by 30% or more, and for optimal ASCVD risk reduction, especially in high-risk patients, levels should be reduced by 50% or more. (Level of Evidence: A) "
|
| "3. For the primary prevention of clinical ASCVD* in adults 40 to 75 years of age without diabetes mellitus and with an LDL-C level of 70 to 189 mg/dL (1.7 to 4.8 mmol/L), the 10-year ASCVD risk of a first “hard” ASCVD event (fatal and nonfatal MI or stroke) should be estimated by using the race- and sex-specific PCE, and adults should be categorized as being at low risk (<5%), borderline risk (5% to <7.5%), intermediate-risk (≥7.5% to <20%), and high-risk (≥20%)(Level of Evidence: B-NR) "
|
| "4. Clinicians and patients should engage in a risk discussion that considers risk factors, adherence to healthy lifestyle, the potential for ASCVD risk-reduction benefits, and the potential for adverse effects and drug–drug interactions, as well as patient preferences, for an individualized treatment decision(Level of Evidence: B-NR) "
|
[1]
| Class IIa
|
| " 5. In intermediate-risk adults, risk-enhancing factors favor initiation or intensification of statin therapy (Level of Evidence B-R)".
|
| '' 6. In intermediate-risk or selected borderline-risk adults, if the decision about statin use remains uncertain, it is reasonable to use a CAC score in the decision to withhold, postpone or initiate statin therapy (Level of Evidence B-NR)''
|
| ''7. In intermediate-risk adults or selected borderline-risk adults in whom a CAC score is measured for the purpose of making a treatment decision, AND
▪If the coronary calcium score is zero, it is reasonable to withhold statin therapy and reassess in 5 to 10 years, as long as higher risk conditions are absent (diabetes mellitus, family history of premature CHD, cigarette smoking)
▪If CAC score is 1 to 99, it is reasonable to initiate statin therapy for patients ≥55 years of age
▪If CAC score is 100 or higher or in the 75th percentile or higher, it is reasonable to initiate statin therapy (Level of Evidence B- NR)''
|
[1]
| Class IIa
|
| " 8. In intermediate-risk adults who would benefit from more aggressive LDL-C lowering and in whom high-intensity statins are advisable but not acceptable or tolerated, it may be reasonable to add a nonstatin drug (ezetimibe or bile acid sequestrant) to a moderate-intensity statin (Level of Evidence B-R)".
|
| '' 9. In patients at borderline risk, in risk discussion, the presence of risk-enhancing factors may justify initiation of moderate-intensity statin therapy (Level of Evidence B-NR)''
|
[1]
Monitoring in Response to LDL-C–Lowering Therapy
| Class I
|
| "1. Adherence to changes in lifestyle and effects of LDL-C–lowering medication should be assessed by measurement of fasting lipids and appropriate safety indicators 4 to 12 weeks after statin initiation or dose adjustment and every 3 to 12 months thereafter based on need to assess adherence or safety.(Level of Evidence: A)"
|
[1]
Primary Prevention in older adults
| Class IIb
|
| " 1. In adults 75 years of age or older with an LDL-C level of 70 to 189 mg/dL (1.7 to 4.8 mmol/L), initiating a moderate-intensity statin may be reasonable (Level of Evidence B-R)".
|
| '' 2. In adults 75 years of age or older, it may be reasonable to stop statin therapy when functional decline (physical or cognitive), multimorbidity, frailty, or reduced life-expectancy limits the potential benefits of statin therapy (Level of Evidence B-R)''
|
| ''3. In adults 76 to 80 years of age with an LDL-C level of 70 to 189 mg/dL (1.7 to 4.8 mmol/L), it may be reasonable to measure CAC to reclassify those with a CAC score of zero to avoid statin therapy (Level of Evidence B- NR)''
|
[1]
Primary Prevention in Children and Adolescents
| Class I
|
| "1. In adults at intermediate-risk, statin therapy reduces risk of ASCVD, and in the context of a risk discussion, if a decision is made for statin therapy, a moderate-intensity statin should be recommended (Level of Evidence: A) "
|
| "2. In children and adolescents with lipid abnormalities, lifestyle counseling is beneficial for lowering LDL-C. (Level of Evidence: B-NR) "
|
[1]
| Class IIa
|
| " 3. In children and adolescents 10 years of age or older with an LDL-C level persistently 190 mg/dL or higher (≥4.9 mmol/L) or 160 mg/dL or higher (4.1 mmol/L) with a clinical presentation consistent with FH and who do not respond adequately with 3 to 6 months of lifestyle therapy, it is reasonable to initiate statin therapy (Level of Evidence B-R)".
|
| '' 4. In children and adolescents with a family history of either early CVD or significant hypercholesterolemia, it is reasonable to measure a fasting or nonfasting lipoprotein profile as early as age 2 years to detect FH or rare forms of hypercholesterolemia.(Level of Evidence B-NR)''
|
| ''5. In children and adolescents found to have moderate or severe hypercholesterolemia, it is reasonable to carry out reverse-cascade screening of family members, which includes cholesterol testing for first-, second-, and when possible, third-degree biological relatives, for detection of familial forms of hypercholesterolemia (Level of Evidence B-NR)''
|
| ''6. In children and adolescents with obesity or other metabolic risk factors, it is reasonable to measure a fasting lipid profile to detect lipid disorders as components of the metabolic syndrome (Level of Evidence C-LD)''
|
[1]
| Class IIb
|
| " 7. In children and adolescents without cardiovascular risk factors or a family history of early CVD, it may be reasonable to measure a fasting lipid profile or nonfasting non-HDL-C once between the ages of 9 and 11 years, and again between the ages of 17 and 21 years, to detect moderate to severe lipid abnormalities (Level of Evidence B-NR)".
|
[1]
Other Population at risk:
Ethnicity
| Class IIa
|
| " 1. For clinical decision-making in adults of different races/ethnicities, it is reasonable for clinicians to review race/ethnic features that can influence ASCVD risk.S4.5.1-1 so as to adjust the choice of statin or intensity of treatment (Level of Evidence B-NR)".
|
[1]
Issues and Recommendations Concerning Women
| Class I
|
| "1. Clinicians should consider conditions specific to women, such as premature menopause (age <40 years) and history of pregnancy-associated disorders (hypertension, preeclampsia, gestational diabetes mellitus, small-for-gestational-age infants, preterm deliveries), when discussing lifestyle intervention and the potential for benefit of statin therapy (Level of Evidence: B-NR) "
|
| "2. Women of childbearing age who are treated with statin therapy and are sexually active should be counseled to use a reliable form of contraception (Level of Evidence: C-LD) "
|
| "3. Women of childbearing age with hypercholesterolemia who plan to become pregnant should stop the statin 1 to 2 months before pregnancy is attempted, or if they become pregnant while on a statin, should have the statin stopped as soon as the pregnancy is discovered (≥20%)(Level of Evidence: B-NR) "
|
[1]
Adults with CKD
| Class IIa
|
| " 1. In adults, 40 to 75 years of age with LDL-C 70 to 189 mg/dL (1.7 to 4.8 mmol/L) who are at 10-year ASCVD risk of 7.5% or higher, CKD not treated with dialysis or kidney transplantation is a risk-enhancing factor and initiation of a moderate-intensity statin or moderate-intensity statins combined with ezetimibe can be useful (Level of Evidence B-NR)".
|
[1]
| Class IIb
|
| " 2. In adults with advanced kidney disease that requires dialysis treatment who are currently on LDL-lowering therapy with a statin, it may be reasonable to continue the statin (Level of Evidence C-LD)".
|
[1]
| Class III (No Benefit)
|
| "3. In adults with advanced kidney disease who require dialysis treatment, initiation of a statin is not recommended. (Level of Evidence:B-R) "
|
[1]
Adults With Chronic Inflammatory Disorders and HIV
| Class IIa
|
| " 1. In adults 40 to 75 years of age with LDL-C 70 to 189 mg/dL (1.7 to 4.8 mmol/L) who have a 10-year ASCVD risk of 7.5% or higher, chronic inflammatory disorders and HIV are risk-enhancing factors and in risk discussion favor moderate-intensity statin therapy or high-intensity statin therapy (Level of Evidence B-NR)".
|
| '' 2. In patients with chronic inflammatory disorders or HIV, a fasting lipid profile and assessment of ASCVD risk factors can be useful as a) a guide to benefit of statin therapy and b) for monitoring or adjusting lipid-lowering drug therapy before and 4 to 12 weeks after starting inflammatory disease–modifying therapy or antiretroviral therapy.(Level of Evidence B-NR)''
|
| ''3. In adults with rheumathoid arthritis who undergo ASCVD risk assessment with measurement of a lipid profile, it can be useful to recheck lipid values and other major ASCVD risk factors 2 to 4 months after the patient’s inflammatory disease has been controlled (Level of Evidence C B-NR)''
|
2013 ACC AHA guideline on the treatment of blood cholesterol primary prevention
Primary Prevention in Adult ≥21 Years With LDL–C ≥190 mg/dL
| Class I
|
| "1. Individuals with LDL–C ≥190 mg/dL or triglycerides ≥500 mg/dL should be evaluated for secondary causes of hyperlipidemia.(Level of Evidence: B)"
|
"2. Adults ≥21 years of age with primary LDL–C ≥190 mg/dL should be treated with statin therapy (10-year ASCVD risk estimation is not required):
- Use high-intensity statin therapy unless contraindicated.
- For individuals unable to tolerate high-intensity statin therapy, use the maximum tolerated statin intensity.(Level of Evidence: B)"
|
| Class IIa
|
| "1. For individuals ≥21 years of age with an untreated primary LDL–C ≥190 mg/dL, it is reasonable to intensify statin therapy to achieve at least a 50% LDL–C reduction.(Level of Evidence: B)"
|
| Class IIb
|
| "1. For individuals ≥21 years of age with an untreated primary LDL–C ≥190 mg/dL, after the maximum intensity of statin therapy has been achieved, addition of a nonstatin drug may be considered to further lower LDL–C. Evaluate the potential for ASCVD risk reduction benefits, adverse effects, drug-drug interactions, and consider patient preferences.(Level of Evidence: C)"
|
| Secondary Cause |
Elevated LDL–C |
Elevated Triglycerides
|
| Diet |
Saturated or trans fats, weight gain, anorexia |
Weight gain, very low-fat diets, high intake of refined carbohydrates, excessive alcohol intake
|
| Drugs |
Diuretics, cyclosporine, Glucocorticoid, amiodarone |
Oral estrogens, glucocorticoids, bile acid sequestrants, protease inhibitors, retinoic acid, anabolic steroids, sirolimus, raloxifene, tamoxifen, beta blockers (not carvedilol), thiazides
|
| Diseases |
Biliary obstruction, nephrotic syndrome |
Nephrotic syndrome, chronic renal failure, lipodystrophies
|
| Disorders and altered states of metabolism |
Hypothyroidism, obesity, pregnancy* |
Diabetes (poorly controlled), hypothyroidism, obesity; pregnancy*
|
* Cholesterol and triglycerides rise progressively throughout pregnancy (81); treatment with statins, niacin, and ezetimibe are contraindicated during pregnancy and lactation.
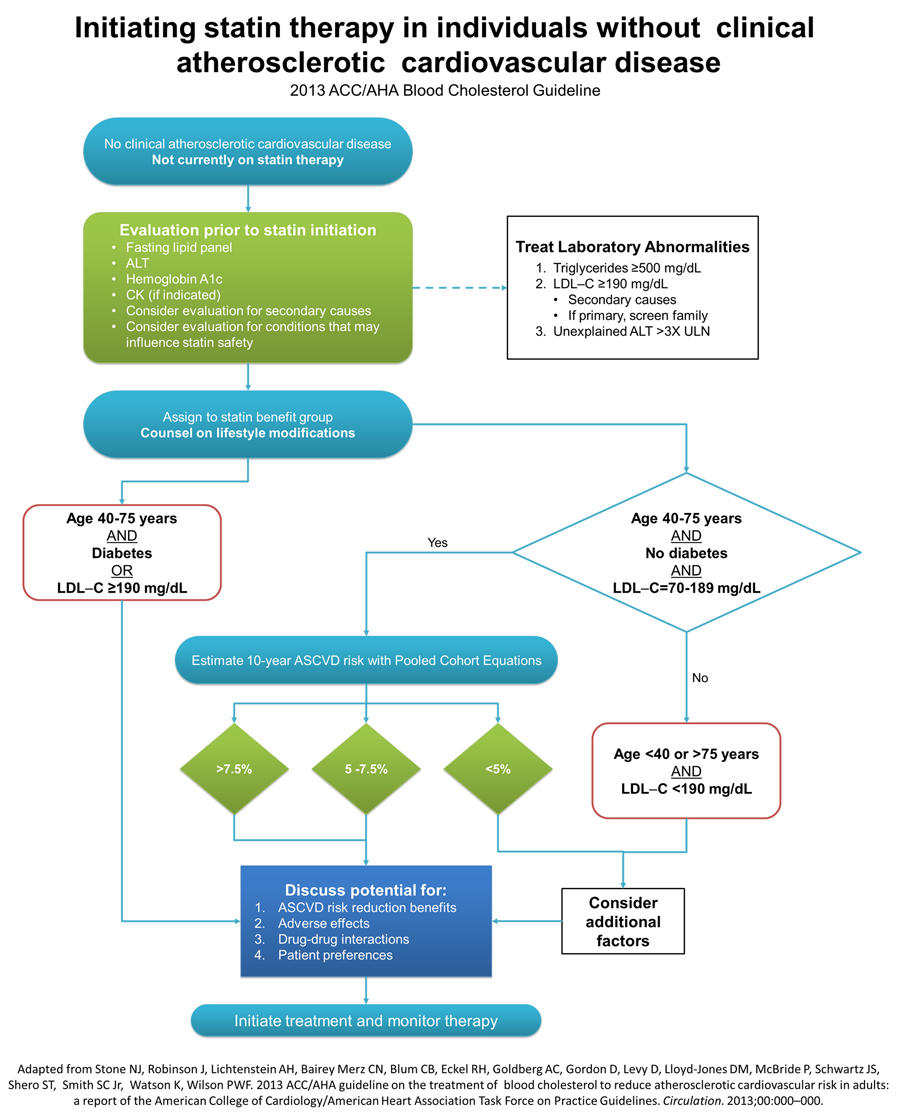
Primary Prevention in Individuals With Diabetes
| Class I
|
| "1. Moderate-intensity statin therapy should be initiated or continued for adults 40 to 75 years of age with diabetes mellitus.(Level of Evidence: A)"
|
| Class IIa
|
| "1. High-intensity statin therapy is reasonable for adults 40 to 75 years of age with diabetes mellitus with a ≥7.5% estimated 10-year ASCVD risk unless contraindicated.(Level of Evidence: B)"
|
| "2. In adults with diabetes mellitus, who are <40 or >75 years of age, it is reasonable to evaluate the potential for ASCVD benefits and for adverse effects, for drug-drug interactions, and to consider patient preferences when deciding to initiate, continue, or intensify statin therapy.(Level of Evidence: C)"
|
Primary Prevention in Individuals Without Diabetes and With LDL–C 70 to 189 mg/dL
| Class I
|
| "1. The Pooled Cohort Equations should be used to estimate 10-year ASCVD risk for individuals with LDL–C 70 to 189 mg/dL without clinical ASCVD* to guide initiation of statin therapy for the primary prevention of ASCVD.(Level of Evidence: B)"
|
| "2. Adults 40 to 75 years of age with LDL–C 70 to 189 mg/dL, without clinical ASCVD or diabetes and an estimated 10-year ASCV risk ≥7.5% should be treated with moderate- to high-intensity statin therapy.(Level of Evidence: A)"
|
| Class IIa
|
| "1. It is reasonable to offer treatment with a moderate-intensity statin to adults 40 to 75 years of age, with LDL–C 70 to 189 mg/dL, without clinical ASCVD* or diabetes and an estimated 10-year ASCVD risk of 5% to <7.5%.(Level of Evidence: B)"
|
| "2. Before initiating statin therapy for the primary prevention of ASCVD in adults with LDL–C 70 to 189 mg/dL without clinical ASCVD or diabetes it is reasonable for clinicians and patients to engage in a discussion which considers the potential for ASCVD risk reduction benefits and for adverse effects, for drug-drug interactions, and patient preferences for treatment.(Level of Evidence: C)"
|
| Class IIb
|
| "1. In adults with LDL–C <190 mg/dL who are not otherwise identified in a statin benefit group, or for whom after quantitative risk assessment a risk based treatment decision is uncertain, additional factors may be considered to inform treatment decision making. In these individuals, statin therapy for primary prevention may be considered after evaluating the potential for ASCVD risk reduction benefits, adverse effects, drug-drug interactions, and discussion of patient preferences.(Level of Evidence: C)"
|
Initiating and Management of Statin Therapy in Individuals Without Clinical ASCVD
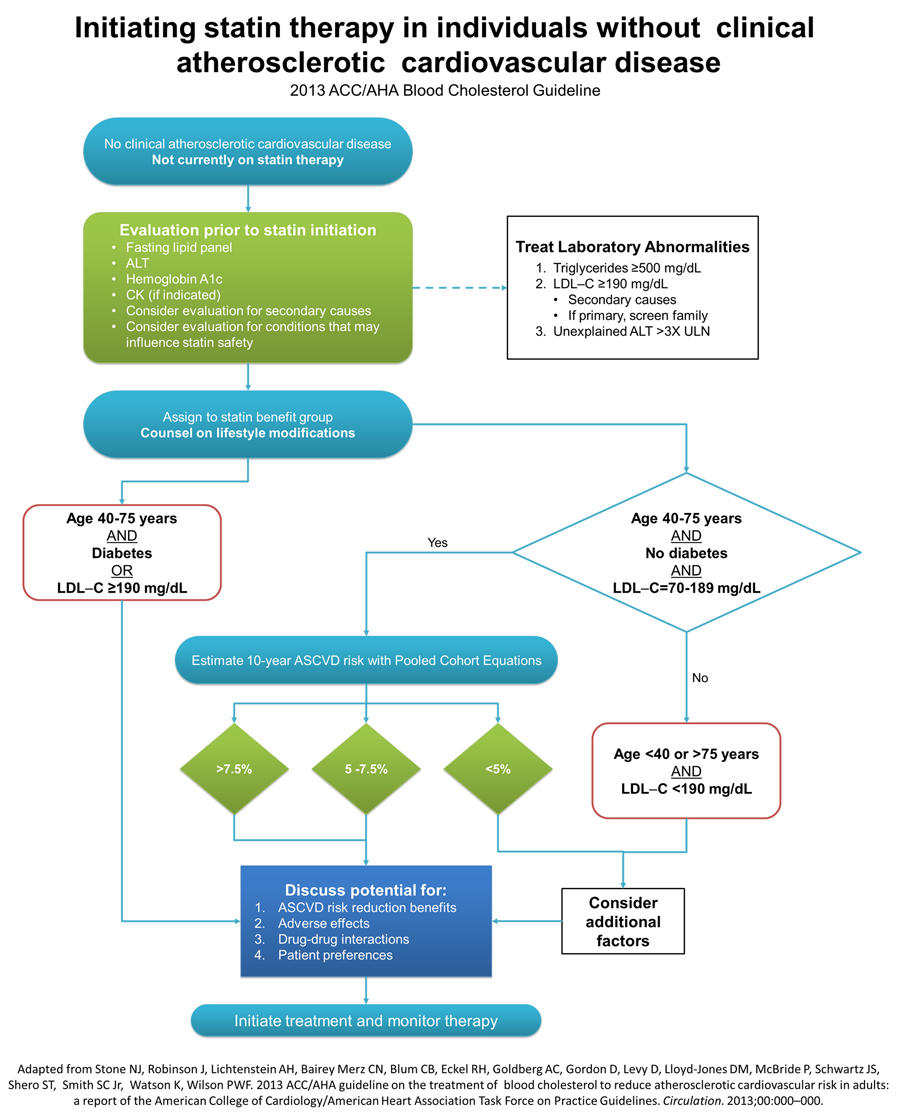
Clinical ASCVD is defined as acute coronary syndromes or history of MI, stable or unstable angina, coronary revascularization, stroke, or TIA presumed to be of atherosclerotic origin, and peripheral arterial disease or revascularization.
Risk Assessment in Primary Prevention
| Rationale for the Expert Panel Approach to Primary Prevention Guidelines[2]
|
| 1. Cholesterol-lowering medications, particularly statins, are efficacious and effective for reducing risk for initial cardiovascular events.
|
| 2. Statins are associated with similar relative-risk reductions for cardiovascular events across the majority of primary-prevention patient groups studied.*
|
| 3. The extent of relative-risk reductions for ASCVD is proportional to the degree of LDL–C lowering observed on statin therapy. Therefore, more intensive statin therapy could reduce risk more than moderate- or lower-intensity statin therapy.
|
| 4. According to consistent findings, the absolute benefit in ASCVD risk reduction is proportional to the baseline risk of the patient group or individual, and to the intensity of statin therapy.
|
| 5. Patients or groups at higher baseline absolute risk, therefore, will derive greater absolute benefit from initiation of statin therapy over a period of 5 to 10 years.
|
| 6. The absolute risk for adverse outcomes, including a small excess in cases of newly diagnosed diabetes, also appears to be proportional to the intensity of statin therapy. However, the adverse outcome of incident (or earlier diagnosis of) diabetes must be weighed in the context of the potentially fatal or debilitating occurrence of MI or stroke that could be prevented by statin therapy.
|
| 7. The Expert Panel emphasizes that the occurrence of a major CVD event (MI or stroke) represents a much greater harm to health status than does an increase in blood glucose leading to a diagnosis of diabetes. The net absolute benefit of statin therapy may be considered as a comparison of the absolute risk reduction for CVD compared with the absolute excess risks including that for diabetes. Benefit also could be understood as a comparison of the number of statin-treated patients that would result in the prevention of 1 case of major ASCVD (NNT) with the number of statin-treated patients that would result in 1 excess case of diabetes (NNH).
|
| 8. Because the absolute benefit in terms of CVD risk reduction depends on the baseline absolute risk for CVD, the absolute benefit from initiation of statin therapy is lower and would approach the risk for adverse effects in patients with lower baseline levels of predicted CVD risk.
|
| 9. Available RCT evidence indicates a clear net absolute benefit of initiation of moderate-to-intensive statin therapy at a baseline estimated 10-year ASCVD risk of ≥7.5%.
|
| 10. Available RCT evidence indicates that when baseline ASCVD risk is 5.0% to <7.5%, there is still net absolute benefit with moderate-intensity statin therapy. However, the tradeoffs between the ASCVD risk reduction benefit and adverse effects are less clear. Thus, a risk-benefit discussion is even more important for individuals with this range of ASCVD risk. The net benefit of high-intensity statin therapy appears to be marginal in such individuals.
|
Conclusion
On the basis of the above tenets and its review of the evidence, this guideline recommends initiation of moderate or intensive statin therapy for patients who are eligible for primary CVD prevention and have a predicted 10-year “hard” ASCVD risk of ≥7.5%. This guideline recommends that initiation of moderate-intensity statin therapy be considered for patients with predicted 10-year “hard” ASCVD risk of 5.0% to <7.5% or intensive statin therapy for patients who are eligible for primary CVD prevention and have a predicted 10-year “hard” ASCVD risk of ≥7.5%. This guideline recommends that initiation of moderate-intensity statin therapy be considered for patients with predicted 10-year “hard” ASCVD risk of 5.0% to <7.5%.
|
References
[1]
Template:WikiDoc Sources
CME Category::Cardiology