Tricuspid stenosis pathophysiology: Difference between revisions
No edit summary |
No edit summary |
||
| (42 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | |||
{{Tricuspid stenosis}} | {{Tricuspid stenosis}} | ||
{{CMG}} {{AE}} [[User:Mohammed Salih|Mohammed Salih, M.D.]] {{sali}} {{FB}} {{VKG}} | |||
==Overview== | |||
[[Tricuspid stenosis]] (TS) is characterized by structural changes in the [[tricuspid valve]]. The [[pathophysiology]] of [[tricuspid valve]] depends on the underlying [[etiology]]. In [[rheumatic heart disease]] which is the most common cause of [[tricuspid stenosis]], there is fibrous thickening of the [[valve]] leaflets and [[chordae tendinae|chordae tendineae]] with/without fusion of the [[commissures]] as a result of [[inflammation]]. The obstruction to right [[Ventricle (heart)|ventricular]] filling due to the [[Stenosis|stenotic]] [[tricuspid valve]] can result in [[systemic]] [[venous]] [[hypertension]] and [[congestion]]. | |||
==Pathophysiology== | ==Pathophysiology== | ||
The [[tricuspid | === Pathogenesis === | ||
*The [[Tricuspid Stenosis|tricuspid]] disease is characterized by diffuse [[fibrous]] thickening of the leaflets and fusion of 2 or 3. <ref name="pmid18222317">{{cite journal |vauthors=Shah PM, Raney AA |title=Tricuspid valve disease |journal=Curr Probl Cardiol |volume=33 |issue=2 |pages=47–84 |date=February 2008 |pmid=18222317 |doi=10.1016/j.cpcardiol.2007.10.004 |url=}}</ref><ref name="urlValvular Heart Disease - ScienceDirect">{{cite web |url=+https://www.sciencedirect.com/science/article/pii/B9780124202191000124?via%3Dihub |title=Valvular Heart Disease - ScienceDirect |format= |work= |accessdate=}}</ref><ref name="pmid28236633">{{cite journal |vauthors=Farag M, Arif R, Sabashnikov A, Zeriouh M, Popov AF, Ruhparwar A, Schmack B, Dohmen PM, Szabó G, Karck M, Weymann A |title=Repair or Replacement for Isolated Tricuspid Valve Pathology? Insights from a Surgical Analysis on Long-Term Survival |journal=Med. Sci. Monit. |volume=23 |issue= |pages=1017–1025 |date=February 2017 |pmid=28236633 |pmc=5338566 |doi=10.12659/msm.900841 |url=}}</ref><ref name="pmid30311884">{{cite journal |vauthors=Salem A, Abdelgawad AME, Elshemy A |title=Early and Midterm Outcomes of Rheumatic Mitral Valve Repair |journal=Heart Surg Forum |volume=21 |issue=5 |pages=E352–E358 |date=August 2018 |pmid=30311884 |doi=10.1532/hsf.1978 |url=}}</ref><ref name="pmid7720297">{{cite journal| author=Waller BF, Howard J, Fess S| title=Pathology of tricuspid valve stenosis and pure tricuspid regurgitation--Part I. | journal=Clin Cardiol | year= 1995 | volume= 18 | issue= 2 | pages= 97-102 | pmid=7720297 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=7720297 }} </ref> | |||
*Leaflet thickening usually occurs in the absence of calcific deposits, and the anteroseptal [[commissure]] is most commonly involved. | |||
*Incompletely developed leaflets, shortened or malformed chordae, a small annulus, or an abnormal number or size of [[papillary muscles]] may result in TS. | |||
*The [[valves]] consist of an outer layer of valve [[Endothelial cell|endothelial]] cells (VECs) surrounding three layers of the [[extracellular]] matrix each with specialized function and interspersed with [[interstitial]] [[valve]] cells (VICs). | |||
*[[Genetics|Genetic]] or acquired/environmental causes that disrupt the normal organization and composition of the [[Extracellular matrix|extracellular]] matrix and communication between VECs and VICs alter [[valve]] mechanics and interfere with the [[valve]] leaflet function, culminating in heart failure. | |||
*As a result of [[valvular stenosis]], there is a persistent [[diastolic pressure]] gradient between the [[right atrium]] and [[right ventricle]]. This gradient increases when blood flow across the [[tricuspid]] valve increases, as occurs with [[inspiration]] and [[exercise]], and decreases when blood flow decreases, such as with [[expiration]].<ref name="pmid22547754">{{cite journal |vauthors=Nishimura RA, Carabello BA |title=Hemodynamics in the cardiac catheterization laboratory of the 21st century |journal=Circulation |volume=125 |issue=17 |pages=2138–50 |date=May 2012 |pmid=22547754 |doi=10.1161/CIRCULATIONAHA.111.060319 |url=}}</ref> | |||
*The primary result of TS is [[Right atrium|right atrial]] pressure elevation and consequent right-sided [[congestion]].<ref name="pmid16645142">{{cite journal |vauthors=Hinton RB, Lincoln J, Deutsch GH, Osinska H, Manning PB, Benson DW, Yutzey KE |title=Extracellular matrix remodeling and organization in developing and diseased aortic valves |journal=Circ. Res. |volume=98 |issue=11 |pages=1431–8 |date=June 2006 |pmid=16645142 |doi=10.1161/01.RES.0000224114.65109.4e |url=}}</ref> | |||
*During [[sinus rhythm]], the right atrial "[[A wave|a]]" wave is increased and may approach the level of [[right ventricular]] [[systolic]] pressure. | |||
*The resting [[cardiac output]] may be reduced and fails to increase with exercise. | |||
*This may contribute to the only modestly elevated left atrial and pulmonary arterial pressures seen when mitral valve disease is also present. | |||
*As a result, most patients with significant [[tricuspid stenosis]] have [[systemic]] venous congestion with [[Jugular venous distention|jugular venous]] distension, [[ascites]], and [[peripheral edema]]. | |||
*The pathophysiology of [[tricuspid stenosis]] depends on the underlying etiology:<ref name="pmid7720297">{{cite journal| author=Waller BF, Howard J, Fess S| title=Pathology of tricuspid valve stenosis and pure tricuspid regurgitation--Part I. | journal=Clin Cardiol | year= 1995 | volume= 18 | issue= 2 | pages= 97-102 | pmid=7720297 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=7720297 }} </ref> | |||
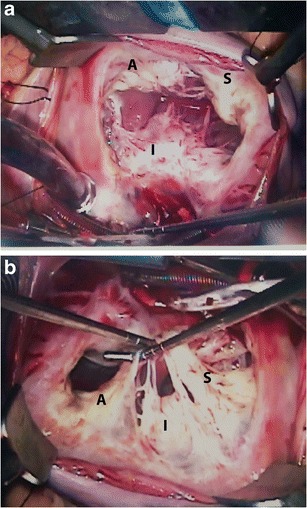
[[File:Normal anatomy of tricuspid valve.jpg|center|thumb|508x508px|Normal surgical [[anatomy]]. ('''a''') Superior view of the [[tricuspid valve]] shows the anterior leaflet (A), which is the largest; the [[septal]] leaflet (S), which is the smallest; and the posterior/inferior leaflet (P). ('''b''') Another view of the tricuspid valve showing the [[Papillary muscle|papillary muscles]], which are more numerous, smaller and more widely separated than those on the left side of the heart. Case courtesy by Soham Shah et al<ref>{{Cite web|url=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5028338/|title=Multimodal imaging of the tricuspid valve: normal appearance and pathological entities|last=|first=|date=|website=|archive-url=|archive-date=|dead-url=|access-date=}}</ref>]] | |||
<br /> | |||
== Associated Conditions == | |||
*[[Rheumatic]] [[tricuspid stenosis]]:<ref name="pmid30885854">{{cite journal |vauthors=Mathur A, Sharma N, Goyal P, Mittal P |title=Surgical Algorithm for Rheumatic Tricuspid Disease |journal=Ann. Thorac. Surg. |volume=108 |issue=2 |pages=e129–e132 |date=August 2019 |pmid=30885854 |doi=10.1016/j.athoracsur.2019.02.009 |url=}}</ref><ref name="pmid30617023">{{cite journal |vauthors=Itzhaki Ben Zadok O, Sagie A, Vaturi M, Shapira Y, Schwartzenberg S, Kuznitz I, Shochat T, Bental T, Yedidya I, Aravot D, Kornowski R, Sharony R |title=Long-Term Outcomes After Mitral Valve Replacement and Tricuspid Annuloplasty in Rheumatic Patients |journal=Ann. Thorac. Surg. |volume=107 |issue=2 |pages=539–545 |date=February 2019 |pmid=30617023 |doi=10.1016/j.athoracsur.2018.09.012 |url=}}</ref><ref name="pmid7720297">{{cite journal |vauthors=Waller BF, Howard J, Fess S |title=Pathology of tricuspid valve stenosis and pure tricuspid regurgitation--Part I |journal=Clin Cardiol |volume=18 |issue=2 |pages=97–102 |date=February 1995 |pmid=7720297 |doi=10.1002/clc.4960180212 |url=}}</ref><ref name="pmid7743689">{{cite journal |vauthors=Waller BF, Howard J, Fess S |title=Pathology of tricuspid valve stenosis and pure tricuspid regurgitation--Part II |journal=Clin Cardiol |volume=18 |issue=3 |pages=167–74 |date=March 1995 |pmid=7743689 |doi=10.1002/clc.4960180312 |url=}}</ref> | |||
** Diffuse scarring and fibrosis of the valve leaflets from [[inflammation]]. Fusion of the [[commissures]] may or may not occur. | |||
**[[Chordae tendineae]] may become thickened and shortened. | |||
** As a result of the dense [[collagen]] and elastic fibers that make up leaflet tissue, the normal leaflet layers become significantly distorted. | |||
*[[Carcinoid|Carcinoid heart disease]]: | |||
** Fibrous white [[plaques]] located on the [[valvular]] and mural [[endocardium]] are characteristic presentations of [[carcinoid]] valve lesions.<ref name="pmid30098723">{{cite journal |vauthors=Hayes AR, Davar J, Caplin ME |title=Carcinoid Heart Disease: A Review |journal=Endocrinol. Metab. Clin. North Am. |volume=47 |issue=3 |pages=671–682 |date=September 2018 |pmid=30098723 |doi=10.1016/j.ecl.2018.04.012 |url=}}</ref><ref name="pmid28596302">{{cite journal |vauthors=Hassan SA, Banchs J, Iliescu C, Dasari A, Lopez-Mattei J, Yusuf SW |title=Carcinoid heart disease |journal=Heart |volume=103 |issue=19 |pages=1488–1495 |date=October 2017 |pmid=28596302 |doi=10.1136/heartjnl-2017-311261 |url=}}</ref><ref name="pmid31587790">{{cite journal |vauthors=Perry D, Hayek SS |title=Carcinoid Heart Disease: A Guide for Clinicians |journal=Cardiol Clin |volume=37 |issue=4 |pages=497–503 |date=November 2019 |pmid=31587790 |doi=10.1016/j.ccl.2019.07.014 |url=}}</ref> | |||
** Valve leaflets become thick, rigid and smaller in area. | |||
**[[Atrial]] and [[ventricular]] surfaces of the valve structure contain fibrous tissue proliferation. | |||
* Congenital [[tricuspid stenosis]]: | |||
** More common in [[Infant|infants]] | |||
**[[Lesion|Lesions]] may present in a number of different ways, either singularly or in any combination of the following: | |||
*** Incompletely developed leaflets | |||
*** Shortened or malformed chordae | |||
*** Small annuli | |||
***[[Papillary muscle]]s of abnormal size and number | |||
*[[Infective endocarditis]]: | |||
**[[Stenosis]] may develop as a result of large infected [[Vegetation (pathology)|vegetations]] obstructing the opening of the [[tricuspid valve]].<ref name="pmid29050737">{{cite journal |vauthors=Aboukhoudir F, Boulet V, Rekik S, Pansieri M |title=[Lead-related infective endocarditis with massive vegetation causing severe functionnal tricuspid stenosis] |language=French |journal=Ann Cardiol Angeiol (Paris) |volume=66 |issue=5 |pages=326–329 |date=November 2017 |pmid=29050737 |doi=10.1016/j.ancard.2017.09.012 |url=}}</ref> | |||
* Other conditions may mimic [[tricuspid stenosis]] by the mechanical obstruction of flow through the [[tricuspid valve]]: | |||
** Supravalvular obstruction from congenital [[Diaphragm|diaphragms]] | |||
**[[Intracardiac]] or extracardiac [[Tumor|tumors]] | |||
**[[Thrombosis]] or [[emboli]] | |||
** Large [[endocarditis]] [[Vegetation (pathology)|vegetations]] | |||
** Other conditions that impair right-sided filling | |||
***[[Constrictive pericarditis]] | |||
***[[Restrictive cardiomyopathy]] | |||
==References== | ==References== | ||
Latest revision as of 04:46, 2 April 2020
|
Tricuspid stenosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Tricuspid stenosis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Tricuspid stenosis pathophysiology |
|
Risk calculators and risk factors for Tricuspid stenosis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Mohammed Salih, M.D. Syed Musadiq Ali M.B.B.S.[2] Fatimo Biobaku M.B.B.S [3] Vamsikrishna Gunnam M.B.B.S [4]
Overview
Tricuspid stenosis (TS) is characterized by structural changes in the tricuspid valve. The pathophysiology of tricuspid valve depends on the underlying etiology. In rheumatic heart disease which is the most common cause of tricuspid stenosis, there is fibrous thickening of the valve leaflets and chordae tendineae with/without fusion of the commissures as a result of inflammation. The obstruction to right ventricular filling due to the stenotic tricuspid valve can result in systemic venous hypertension and congestion.
Pathophysiology
Pathogenesis
- The tricuspid disease is characterized by diffuse fibrous thickening of the leaflets and fusion of 2 or 3. [1][2][3][4][5]
- Leaflet thickening usually occurs in the absence of calcific deposits, and the anteroseptal commissure is most commonly involved.
- Incompletely developed leaflets, shortened or malformed chordae, a small annulus, or an abnormal number or size of papillary muscles may result in TS.
- The valves consist of an outer layer of valve endothelial cells (VECs) surrounding three layers of the extracellular matrix each with specialized function and interspersed with interstitial valve cells (VICs).
- Genetic or acquired/environmental causes that disrupt the normal organization and composition of the extracellular matrix and communication between VECs and VICs alter valve mechanics and interfere with the valve leaflet function, culminating in heart failure.
- As a result of valvular stenosis, there is a persistent diastolic pressure gradient between the right atrium and right ventricle. This gradient increases when blood flow across the tricuspid valve increases, as occurs with inspiration and exercise, and decreases when blood flow decreases, such as with expiration.[6]
- The primary result of TS is right atrial pressure elevation and consequent right-sided congestion.[7]
- During sinus rhythm, the right atrial "a" wave is increased and may approach the level of right ventricular systolic pressure.
- The resting cardiac output may be reduced and fails to increase with exercise.
- This may contribute to the only modestly elevated left atrial and pulmonary arterial pressures seen when mitral valve disease is also present.
- As a result, most patients with significant tricuspid stenosis have systemic venous congestion with jugular venous distension, ascites, and peripheral edema.
- The pathophysiology of tricuspid stenosis depends on the underlying etiology:[5]
Associated Conditions
- Rheumatic tricuspid stenosis:[9][10][5][11]
- Diffuse scarring and fibrosis of the valve leaflets from inflammation. Fusion of the commissures may or may not occur.
- Chordae tendineae may become thickened and shortened.
- As a result of the dense collagen and elastic fibers that make up leaflet tissue, the normal leaflet layers become significantly distorted.
- Carcinoid heart disease:
- Fibrous white plaques located on the valvular and mural endocardium are characteristic presentations of carcinoid valve lesions.[12][13][14]
- Valve leaflets become thick, rigid and smaller in area.
- Atrial and ventricular surfaces of the valve structure contain fibrous tissue proliferation.
- Congenital tricuspid stenosis:
- More common in infants
- Lesions may present in a number of different ways, either singularly or in any combination of the following:
- Incompletely developed leaflets
- Shortened or malformed chordae
- Small annuli
- Papillary muscles of abnormal size and number
- Infective endocarditis:
- Stenosis may develop as a result of large infected vegetations obstructing the opening of the tricuspid valve.[15]
- Other conditions may mimic tricuspid stenosis by the mechanical obstruction of flow through the tricuspid valve:
- Supravalvular obstruction from congenital diaphragms
- Intracardiac or extracardiac tumors
- Thrombosis or emboli
- Large endocarditis vegetations
- Other conditions that impair right-sided filling
References
- ↑ Shah PM, Raney AA (February 2008). "Tricuspid valve disease". Curr Probl Cardiol. 33 (2): 47–84. doi:10.1016/j.cpcardiol.2007.10.004. PMID 18222317.
- ↑ [+https://www.sciencedirect.com/science/article/pii/B9780124202191000124?via%3Dihub "Valvular Heart Disease - ScienceDirect"] Check
|url=value (help). - ↑ Farag M, Arif R, Sabashnikov A, Zeriouh M, Popov AF, Ruhparwar A, Schmack B, Dohmen PM, Szabó G, Karck M, Weymann A (February 2017). "Repair or Replacement for Isolated Tricuspid Valve Pathology? Insights from a Surgical Analysis on Long-Term Survival". Med. Sci. Monit. 23: 1017–1025. doi:10.12659/msm.900841. PMC 5338566. PMID 28236633.
- ↑ Salem A, Abdelgawad A, Elshemy A (August 2018). "Early and Midterm Outcomes of Rheumatic Mitral Valve Repair". Heart Surg Forum. 21 (5): E352–E358. doi:10.1532/hsf.1978. PMID 30311884. Vancouver style error: initials (help)
- ↑ 5.0 5.1 5.2 Waller BF, Howard J, Fess S (1995). "Pathology of tricuspid valve stenosis and pure tricuspid regurgitation--Part I." Clin Cardiol. 18 (2): 97–102. PMID 7720297.
- ↑ Nishimura RA, Carabello BA (May 2012). "Hemodynamics in the cardiac catheterization laboratory of the 21st century". Circulation. 125 (17): 2138–50. doi:10.1161/CIRCULATIONAHA.111.060319. PMID 22547754.
- ↑ Hinton RB, Lincoln J, Deutsch GH, Osinska H, Manning PB, Benson DW, Yutzey KE (June 2006). "Extracellular matrix remodeling and organization in developing and diseased aortic valves". Circ. Res. 98 (11): 1431–8. doi:10.1161/01.RES.0000224114.65109.4e. PMID 16645142.
- ↑ "Multimodal imaging of the tricuspid valve: normal appearance and pathological entities".
- ↑ Mathur A, Sharma N, Goyal P, Mittal P (August 2019). "Surgical Algorithm for Rheumatic Tricuspid Disease". Ann. Thorac. Surg. 108 (2): e129–e132. doi:10.1016/j.athoracsur.2019.02.009. PMID 30885854.
- ↑ Itzhaki Ben Zadok O, Sagie A, Vaturi M, Shapira Y, Schwartzenberg S, Kuznitz I, Shochat T, Bental T, Yedidya I, Aravot D, Kornowski R, Sharony R (February 2019). "Long-Term Outcomes After Mitral Valve Replacement and Tricuspid Annuloplasty in Rheumatic Patients". Ann. Thorac. Surg. 107 (2): 539–545. doi:10.1016/j.athoracsur.2018.09.012. PMID 30617023.
- ↑ Waller BF, Howard J, Fess S (March 1995). "Pathology of tricuspid valve stenosis and pure tricuspid regurgitation--Part II". Clin Cardiol. 18 (3): 167–74. doi:10.1002/clc.4960180312. PMID 7743689.
- ↑ Hayes AR, Davar J, Caplin ME (September 2018). "Carcinoid Heart Disease: A Review". Endocrinol. Metab. Clin. North Am. 47 (3): 671–682. doi:10.1016/j.ecl.2018.04.012. PMID 30098723.
- ↑ Hassan SA, Banchs J, Iliescu C, Dasari A, Lopez-Mattei J, Yusuf SW (October 2017). "Carcinoid heart disease". Heart. 103 (19): 1488–1495. doi:10.1136/heartjnl-2017-311261. PMID 28596302.
- ↑ Perry D, Hayek SS (November 2019). "Carcinoid Heart Disease: A Guide for Clinicians". Cardiol Clin. 37 (4): 497–503. doi:10.1016/j.ccl.2019.07.014. PMID 31587790.
- ↑ Aboukhoudir F, Boulet V, Rekik S, Pansieri M (November 2017). "[Lead-related infective endocarditis with massive vegetation causing severe functionnal tricuspid stenosis]". Ann Cardiol Angeiol (Paris) (in French). 66 (5): 326–329. doi:10.1016/j.ancard.2017.09.012. PMID 29050737.