Syphilis pathophysiology: Difference between revisions
Aysha Aslam (talk | contribs) |
Aysha Aslam (talk | contribs) |
||
| Line 30: | Line 30: | ||
*It is speculated that there is a shift from Th1 to Th2 response during secondary syphilis. | *It is speculated that there is a shift from Th1 to Th2 response during secondary syphilis. | ||
*Cyototxic T cells and incomplete humoral response is mainly responsible for persistence of infection and tissue damage in tertiary syphilis. | *Cyototxic T cells and incomplete humoral response is mainly responsible for persistence of infection and tissue damage in tertiary syphilis. | ||
*Ineffective type 4 delayed hypersensitivity reaction containing [[macrophages]] and sensitized [[T cells]] | *Ineffective type 4 delayed hypersensitivity reaction containing [[macrophages]] and sensitized [[T cells]] is mainly responsible for [[gumma]] formation in various organs. | ||
===Pathogenesis of chronic infection in syphilis=== | ===Pathogenesis of chronic infection in syphilis=== | ||
Revision as of 16:48, 23 September 2016
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
|
Syphilis Microchapters | |
|
Diagnosis | |
|
Treatment | |
|
Case Studies | |
|
Syphilis pathophysiology On the Web | |
|
American Roentgen Ray Society Images of Syphilis pathophysiology | |
|
Risk calculators and risk factors for Syphilis pathophysiology | |
Overview
Syphilis is caused by a spirochete, treponema pallidum. It has an incubation period of 3 - 12 weeks. Spirochete penetrates intact mucous membrane or microscopic dermal abrasions and rapidly enters systemic circulation with the central nervous system being invaded during the early phase of infection. The meninges and blood vessels are initially involved with the brain parenchyma and spinal cord being involved in the later stages of the disease. The histopathological hallmark findings are endarteritis and plasma cell-rich infiltrates reflecting a delayed-type of hypersensitivity to the spirochete
Pathogenesis
Pathogenesis of syphilis may be described in the following steps:
Transmission
Treponema pallidum is usually transmitted via direct contact with the infected lesion (sexual contact) or blood transfusion (rare).
Incubation
Incubation period varies with the size of innoculum (9-90 days)
Dissemination
- Following transmission, the Trepenoma Pallidum uses the intact or abraded mucous membrane to enter the body.
- After entering the body, it may disseminate to lymphatics and blood stream to gain access to any organ of the body.
- It uses fibronectin molecules to attach to endothelial surface of vessels in organs resulting in inflammation and obliteration of small blood vessels causing vasculitis (end arteritis obliterans).
- Organism has slow replication rate (30-33 hrs) and evades initial host immune response resulting in local infection.
- Initial infection called primary syphilis resolves in few weeks due to cellular host immune response.
Seeding
- Few weeks to months after initial infection, it disseminates to other parts of body resulting in constitutional sytmptoms and characteristic rash called secondary syphilis.
- It may seed to different organs of the body esp cardiovascular system and central nervous system resulting in tertiary syphilis.
Immune response
- Different stages of syphilis results from interaction between antigen and host immune response.
- Initial infection in primary syphilis is limited due to Th1 response and lack of antibody response.
- It is speculated that there is a shift from Th1 to Th2 response during secondary syphilis.
- Cyototxic T cells and incomplete humoral response is mainly responsible for persistence of infection and tissue damage in tertiary syphilis.
- Ineffective type 4 delayed hypersensitivity reaction containing macrophages and sensitized T cells is mainly responsible for gumma formation in various organs.
Pathogenesis of chronic infection in syphilis
- Lack of immunogenic molecules in outer sheath of Treponema Pallidum
- Insufficient humoral immune response.
- Downregulation of Th1 response and shift to Th2 immune response in secondary and tertiary syphilis.
- Decreased strength of delayed hypersensitivity reaction(HIV)
Genetics
There is no known genetic association of syphilis.
Associated conditions
Syphilis is associated with increased transmission of HIV. The underlying mechanism may be related to accumulation of dendritic cells containing CCR5 co receptors at the site of infection, the same receptor entity binding HIV.
Gross pathology
On gross pathology, following features are characteristic findings of syphilis.
Microscopic pathology
On microscopic histopathological analysis, characteristic findings of syphilis depends on the stage of the disease:
Primary syphilis
- Mononuclear leukocytic infiltration, macrophages, and lymphocytes
- Swelling and proliferation of small blood vessels
Secondary syphilis
- Swelling and dilatation of blood vessels in the dermis
- Epidermal hyperplasia and neutrophilic infiltration
- Inflammatory cell infiltrate predominantly plasma cell
Tertiary syphilis
- Small vessel inflammation (end arteritis obliterans)
- Gummas

- The lesion may persist for 4 to 6 weeks and usually heals spontaneously.
- Local lymph node swelling can occur.
- During the initial incubation period, individuals are otherwise asymptomatic. As a result, many patients do not seek medical care immediately.
- Syphilis can not be contracted through toilet seats, daily activities, hot tubs, or sharing eating utensils or clothing.[1]
Secondary Syphilis
- Secondary syphilis occurs approximately 1-6 months (commonly 6 to 8 weeks) after the primary infection.
- There are many different manifestations of secondary disease.
- There may be a symmetrical reddish-pink non-itchy rash on the trunk and extremities.[2]
- The rash can involve the palms of the hands and the soles of the feet.
- In moist areas of the body, the rash becomes flat broad whitish lesions known as condylomata lata.
- Mucous patches may also appear on the genitals or in the mouth.
- All of these lesions are infectious and harbor active treponeme organisms.
- A patient with syphilis is most contagious when he or she has secondary syphilis.
- Other symptoms common at this stage include:
- Enlarged lymph nodes.
- Fever,
- Headache,
- Malaise,
- Meningismus, and
- Sore throat,
- Weight loss,
- Rare manifestations include:
- An acute meningitis that occurs in about 2% of patients,
- Arthritis,
- Hepatitis,
- Hypertrophic gastritis,
- Intersitial keratitis,
- Iritis, and
- Optic neuritis,
- Patchy proctitis,
- Periostitis,
- Rectosigmoid mass,
- Renal disease,
- Ulcerative colitis,
- Uveitis.
-
Typical presentation of secondary syphilis rash on the palms of the hands and usually also seen on soles of feet
-
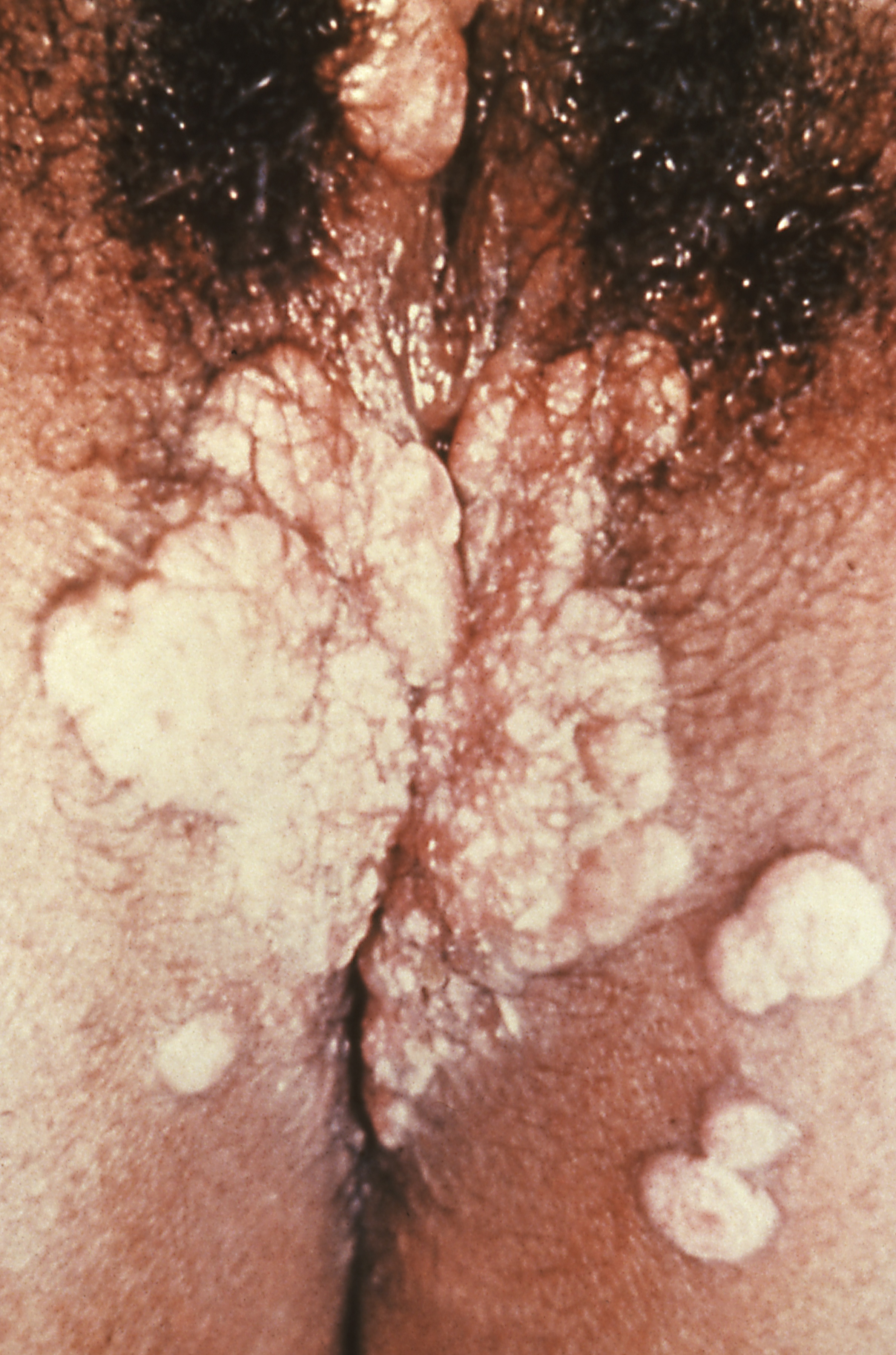
Condyoma lata (syphilis secondary)
-
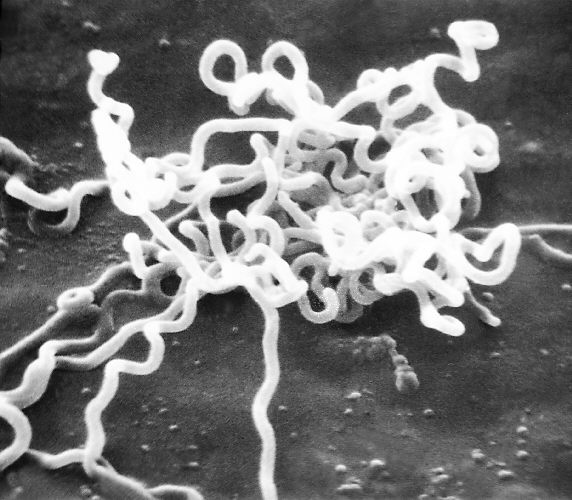
Electron micrograph of Treponema pallidum
-
Syphilis lesions on a patient's back
-
Syphilis lesions on a patient's chest
-
Chancres on the penile shaft due to a primary syphilitic infection
-
Secondary syphilis manifested perineal condylomata lata lesions, which presented as gray, raised papules that sometimes appear on the vulva or near the anus, or in any other warm intertriginous region.
-
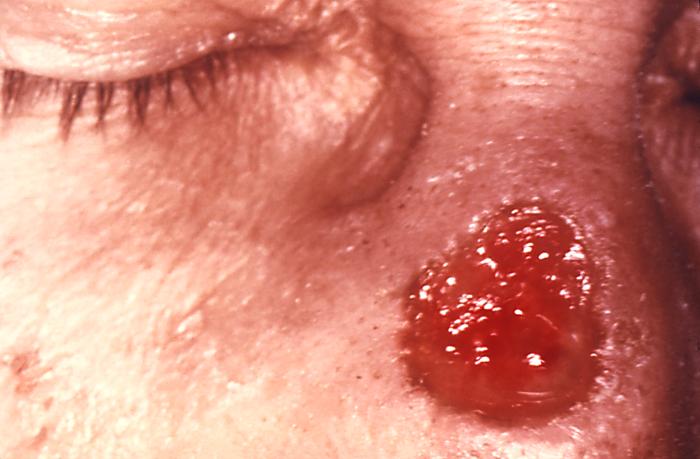
Gumma of the nose due to long standing tertiary syphilis
Latent Syphilis
- Latent syphilis is defined as having serologic proof of infection without signs or symptoms of disease.[3]
- Latent syphilis is further described as either early or late.
- Early latent syphilis is defined as having syphilis for two years or less from the time of initial infection without signs or symptoms of disease.
- Late latent syphilis is infection for greater than two years but without clinical evidence of disease. The distinction is important for both therapy and risk for transmission.
- In the real-world, the timing of infection is often not known and should be presumed to be late for the purpose of therapy. Early latent syphilis may be treated with a single intramuscular injection of a long-acting penicillin. Late latent syphilis, however, requires three weekly injections.
- For infectiousness, however, late latent syphilis is not considered as contagious as early latent syphilis.
Tertiary Syphilis
- Tertiary syphilis usually occurs 1-10 years after the initial infection, though in some cases it can take up to 50 years.
- This stage is characterized by the formation of gummas which are soft, tumor-like balls of inflammation known as granulomas.
- The granulomas are chronic and represent an inability of the immune system to completely clear the organism.
- Gummas were once readily seen in the skin and mucous membranes although they tend to occur internally in recent history. They may appear almost anywhere in the body including in the skeleton.
- The gummas produce a chronic inflammatory state in the body with mass-effects upon the local anatomy.
- Other characteristics of untreated tertiary syphilis include neuropathic joint disease, which are a degeneration of joint surfaces resulting from loss of sensation and fine position sense (proprioception).
- The more severe manifestations include neurosyphilis and cardiovascular syphilis. In a study of untreated syphilis, 10% of patients developed cardiovascular syphilis, 16% had gumma formation, and 7% had neurosyphilis.[4]
Neurosyphilis
- Neurosyphilis refers to a site of infection involving the central nervous system (CNS).
- Neurosyphilis may occur at any stage of syphilis.
- Before the advent of antibiotics, it was typically seen in 25-35% of patients with syphilis.
- Neurosyphilis is now most common in patients with HIV infection. Reports of neurosyphilis in HIV-infected persons are similar to cases reported before the HIV pandemic. The precise extent and significance of neurologic involvement in HIV-infected patients with syphilis, reflected by either laboratory or clinical criteria, have not been well characterized. Furthermore, the alteration of host immunosuppression by antiretroviral therapy in recent years has further complicated such characterization.
- Approximately 35% to 40% of persons with secondary syphilis have asymptomatic central nervous system (CNS) involvement, as demonstrated by any of these on cerebrospinal fluid (CSF) examination:
- An abnormal leukocyte cell count, protein level, or glucose level
- Demonstrated reactivity to Venereal Disease Research Laboratory (VDRL) antibody test
- There are four clinical types of neurosyphilis:
- The late forms of neurosyphilis (tabes dorsalis and general paresis) are seen much less frequently since the advent of antibiotics.
- The most common manifestations today are asymptomatic or symptomatic meningitis.
1. Asymptomatic Meningitis
- Asymptomatic neurosyphilis usually has no signs or symptoms and is diagnosed exclusively with the presence or absence of CSF abnormalities notably pleocytosis, elevated protein, decreased glucose.
2. Symptomatic Meningitis
- Acute syphilitic meningitis usually occurs within the first year of infection; 10% of cases are diagnosed at the time of the secondary rash.
- Develops within 6-months to several years of primary infection
- Patients present with headache, meningeal irritation, and cranial nerve abnormalities, especially the optic nerve, facial nerve, and the vestibulocochlear nerve.
- Rarely, it affects the spine instead of the brain, causing focal muscle weakness or sensory loss.
- Typical meningitis symptoms: headache, nausea, vomiting, photophobia
3. Meningovascular Syphilis
- Meningovascular syphilis occurs a few months to 10 years (average, 7 years) after the primary syphilis infection.
- Meningovascular syphilis can be associated with prodromal symptoms lasting weeks to months before focal deficits are identifiable.
- Prodromal symptoms include:
- Headache,
- Insomnia, and
- Paresthesias,
- Psychiatric abnormalities such as personality changes.
- Unilateral numbness,
- Upper or lower extremity weakness,
- Vertigo,
- The focal deficits initially are intermittent or progress slowly over a few days.
- Angiography may be able to demonstrate areas of narrowing in the blood vessels or total occlusion.
4. Parenchymatous Neurosyphilis
- Argyll robertson pupil: small irregular pupil
- Clinical presents as general paresis or tabes dorsalis with resultant ataxia
- Develops 15-20 years after primary infection
- General paresis[5], otherwise known as general paresis of the insane, is a severe manifestation of neurosyphilis.
- It is a chronic dementia which ultimately results in death in as little as 2-3 years.
- Patients generally have progressive personality changes, memory loss, and poor judgment.
- More rarely, they can have psychosis, depression, or mania.
- Imaging of the brain usually shows atrophy.
Microscopic Pathology
Brain: Gumma of Syphilis
{{#ev:youtube|Cd60sjchsN8}}
Brain: Paresis (syphilis)
{{#ev:youtube|1Ibu71qHznA}}
References
- ↑ Centers for Disease Control (CDC) (05-2004). "STD Facts - Syphilis". Centers for Disease Control. Check date values in:
|date=(help) - ↑ Dylewski J, Duong M (2007 Jan 2). "The rash of secondary syphilis". CMAJ. 176 (1): 33–5. doi:10.1503/cmaj.060665. Check date values in:
|date=(help) - ↑
- ↑ Clark EG, Danbolt N (1964). "The Oslo study of the natural course of untreated syphilis: An epidemiologic investigation based on a re-study of the Boeck-Bruusgaard material". Med Clin North Am. 48: 613.
- ↑ Richard B. Jamess, MD, PhD (2002). "Syphilis- Sexually Transmitted Infections, 2006". Sexually transmitted diseases treatment guidelines. External link in
|title=(help)