Squamous cell carcinoma of the skin: Difference between revisions
No edit summary |
|||
| Line 144: | Line 144: | ||
*'''[[Squamous cell carcinoma medical treatment|Medical treatment]]''' | *'''[[Squamous cell carcinoma medical treatment|Medical treatment]]''' | ||
*'''[[Squamous cell carcinoma surgical treatment|Surgical treatment]]''' | *'''[[Squamous cell carcinoma surgical treatment|Surgical treatment]]''' | ||
*'''[[Primary Prevention]]''' | |||
==Future and Investigational treatment strategies== | ==Future and Investigational treatment strategies== | ||
Revision as of 15:19, 14 June 2012
For patient information click here
Template:DiseaseDisorder infobox
|
Squamous cell carcinoma of the skin Microchapters |
|
Differentiating Squamous cell carcinoma of the skin from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Squamous cell carcinoma of the skin On the Web |
|
American Roentgen Ray Society Images of Squamous cell carcinoma of the skin |
|
Directions to Hospitals Treating Squamous cell carcinoma of the skin |
|
Risk calculators and risk factors for Squamous cell carcinoma of the skin |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Aditya Govindavarjhulla, M.B.B.S. [2], Raviteja Guddeti, M.B.B.S. [3]
Overview
Historical Aspects
Pathophysiology
Epidemiology and Demographics
Risk Factors
Screening
Causes of Squamous cell carcinoma
Differential Diagnosis
Natural History Complications and Prognosis
Clinical Features
Diagnosis
Diagnosis is via a biopsy. For the skin, look under skin biopsy.
The pathological appearance of a squamous cell cancer varies with the depth of the biopsy. For that reason, a biopsy including the subcutanous tissue and basalar epithelium, to the surface is necessary for correct diagnosis. The performance of a shave biopsy (see skin biopsy) might not acquire enough information for a diagnosis. An excision biopsy is ideal, but not practical in most cases. An incisional or punch biopsy is preferred. A shave biopsy is least ideal, especially if only the superficial portion is acquired.
Physical Examination
Skin
Squamous cell carcinoma of the skin is often caused by long term exposure to the sun. To be diagnosed, a biopsy is done where a sample is taken and examined under a microscope by a Pathologist. If it is found to be cancerous, a surgery is done to remove it.
Squamous cell carcinomas account for about 20% of non-melanoma skin cancers, (with basal cell carcinomas accounting for about 80%), and are clinically more significant because of their ability to metastasize. Squamous cell carcinoma is usually developed in the epithelial layer of the skin and sometimes in various mucous membranes of the body.
Squamous cell carcinoma is the second most common cancer of the skin (after basal cell carcinoma but more common than melanoma). It usually occurs in areas exposed to the sun, and can generally be treated by excision or mohs surgery only.
Sunlight exposure and immunosuppression are risk factors for SCC of the skin with chronic sun exposure being the strongest environmental risk factor.[1] The risk of metastasis is low, but is much higher than basal cell carcinoma.
Squamous cell cancers of the lip and ears have high metastatic and recurrence rate (20 to 50%)[2]. Squamous cell cancers of the skin in individuals on immunotherapy or having lymphoproliferative disorders (leukemias) are much more aggressive, regardless of their location.[3]
Australian scientist Ian Frazer who developed the cervical cancer vaccine, says that animal tests have been effective in preventing squamous cell carcinoma in animals, and there may be a human vaccine against this kind of skin cancer within the decade.[4]
Ear Nose and Throat
-
Squamous cell carcinoma in oral cavity.
Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology -
Squamous cell carcinoma in oral cavity.
Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology -
Squamous cell carcinoma in oral cavity.
Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology
-
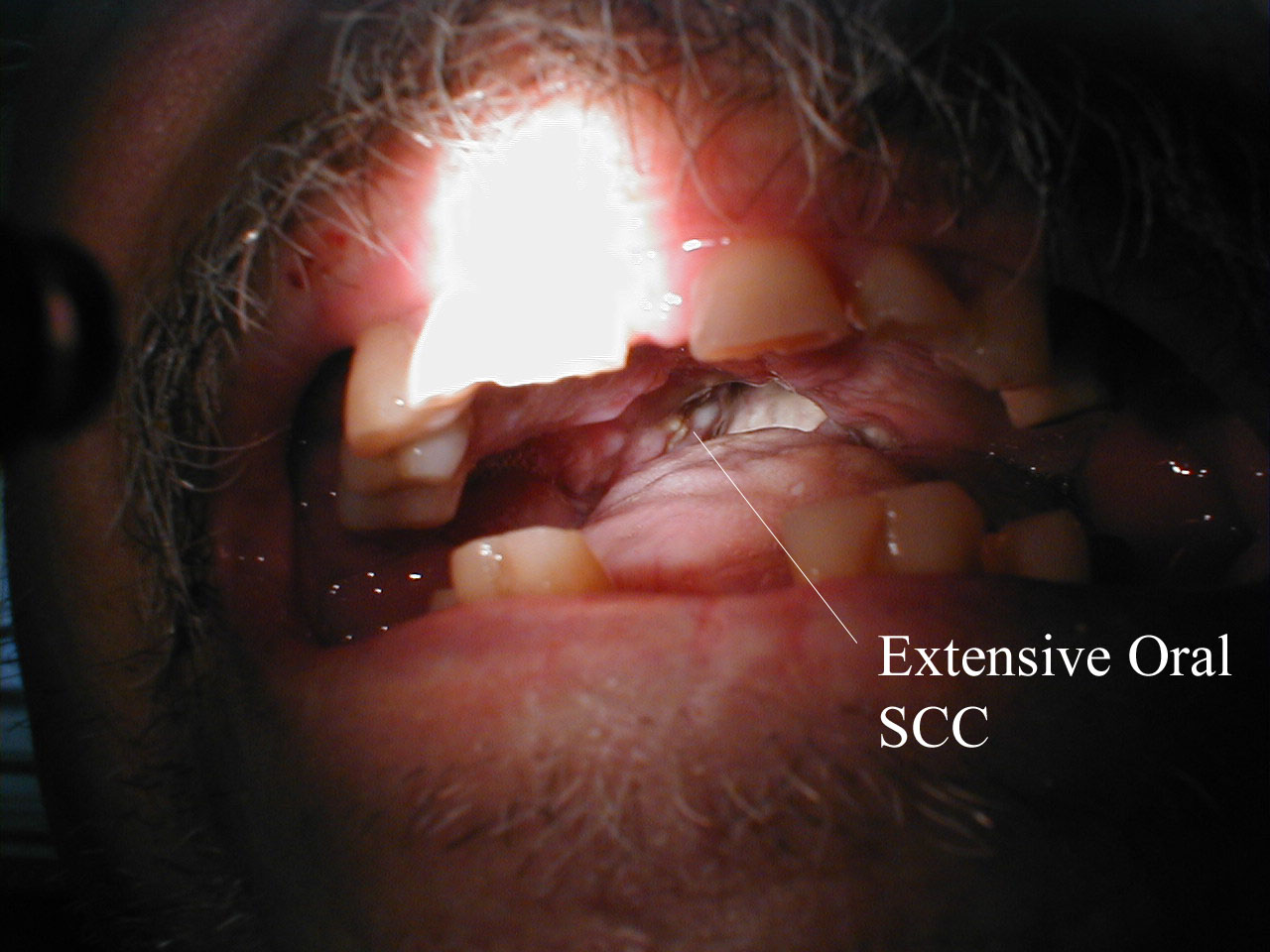
Squamous Cell Cancer of the Mouth: Irregular, necrotic appearing tissue on the inside of the mouth due to extensive squamous cell cancer. Patient has limited ability to open his mouth (aka trismus) as a result of the infiltrating cancer.
-
Squamous Cell Cancer, Base of Tongue: Note white area with swelling, right base of tongue.
-
Squamous Cell Cancer of the Mouth: Cancer that began along the lower gum line has spread to left submandibular lymph nodes.
-
Squamous Cell Cancer of the Mouth: Cancer that began along the lower gum line has spread to left submandibular lymph nodes.
Esophagus
Esophageal cancer may be due to either squamous cell carcinoma (ESCC) or adenocarcinoma (EAC). SCCs tend to occur closer to the mouth, while adenocarcinomas occur closer to the stomach. Dysphagia (difficulty swallowing, solids worse than liquids) and odynophagia are common initial symptoms. If the disease is localized, esophagectomy may offer the possibility of a cure. If the disease has spread, chemotherapy and radiotherapy are commonly used.
Penis
When squamous cell carcinoma in situ (Bowen's disease) is found on the penis, it is called erythroplasia of Queyrat[10]. This type of cancer respond very well to an experimental agent called Aldara.
Prostate
When associated with the prostate, squamous cell carcinoma is very aggressive in nature. It is difficult to detect as there is no increase in prostate specific antigen levels seen; meaning that the cancer is often diagnosed at an advanced stage.
Lung
When associated with the lung, it often causes ectopic production of parathyroid hormone-related protein (PTHrP), resulting in hypercalcemia.
-
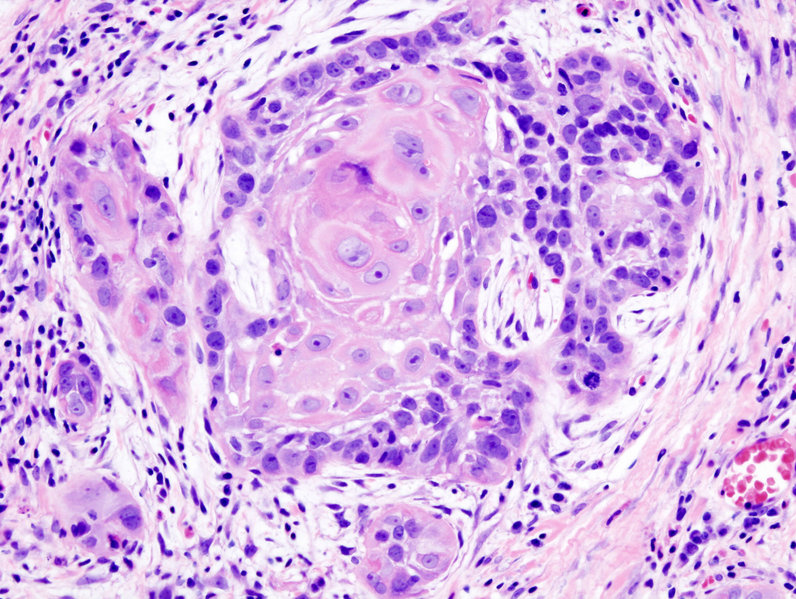
Biopsy of a highly differentiated squamous cell carcinoma of the mouth. Haematoxylin & eosin stain.
-
Photograph of a squamous cell carcinoma. Tumour is on the left, obstructing the bronchus (lung). Beyond the tumour the bronchus is inflammed and contains mucus
Vagina and cervix
Vaginal squamous cell carcinoma spreads slowly and usually stays near the vagina, but may spread to the lungs and liver. This is the most common type of vaginal cancer.
Cervix: Squamous cell carcinoma
<youtube v=zB47nE-i8dQ/>
<youtube v=J3kULzKGzws/>
Treatment
Future and Investigational treatment strategies
In 2007, Australian biopharmaceutical company Clinuvel Pharmaceuticals Limited began clinical trials with a melanocyte-stimulating hormone called melanotan (known by the International Nonproprietary Name afamelanotide, formerly CUV1647)[11] to provide photoprotection for organ transplant patients against squamous cell carcinoma of the skin and actinic keratosis.[12][13]
Cetuximab a monoclonal antibody that targets the epidermal growth factor receptor (EGFR), has antitumor activity in patients with advanced squamous cell carcinoma of the skin, as initially suggested by case reports.
References
- ↑ name="mdconsult"
- ↑ http://www.aad.org/public/publications/pamphlets/sun_squamous.html
- ↑ http://www.skincarephysicians.com/skincancernet/squamous_cell_carcinoma.html
- ↑ Cosmos Online - Skin cancer vaccine within reach (http://www.cosmosmagazine.com/news/2327/skin-cancer-vaccine-within-reach)
- ↑ http://picasaweb.google.com/mcmumbi/USMLEIIImages
- ↑ http://picasaweb.google.com/mcmumbi/USMLEIIImages
- ↑ http://www.ghorayeb.com
- ↑ http://www.ghorayeb.com
- ↑ http://www.ghorayeb.com
- ↑ http://www.emedicine.com/derm/TOPIC144.HTM
- ↑ "World Health Organisation assigns CUV1647 generic name" (PDF). Clinuvel. 2008. Retrieved 2008-06-17.
- ↑ Clinuvel » Investors » FAQs
- ↑ PharmaAsia - Clinuvel’s Drug Begins Global Phase II Skin Cancer Trials
External links
- Information on Squamous Cell Carcinoma from The Skin Cancer Foundation
- Article by Stephen D Hess, MD, PhD
- DermNet NZ: Squamous cell carcinoma
- Squamous cell carcinoma in transplant recipients
Template:Tumors of bone, cartilage, skin, connective, and soft tissue Template:Respiratory and intrathoracic neoplasia Template:Genital neoplasia Template:Epithelial neoplasms
de:Plattenepithelkarzinom he:קרצינומת תאי קשקש nl:Plaveiselcelcarcinoom



![Squamous cell skin cancer.[5]](/images/1/17/Squamous_cell_skin_cancer.jpg)
![A large squamous cell carcinoma of the tongue[6]](/images/e/e9/Squamous_cell_carcinoma.jpg)
![This patient had two adjacent cancers. The flat black lesion below the antitragus is a malignant melanoma. The white elevated keratotic lesion is a squamous cell carcinoma [7].](/images/f/f4/AuricleMelanoma_SqCC.jpg)



![Recurrent squamous cell carcinoma of the auricle (far left) excised with a stellate incision across the antihelix[8].](/images/c/c8/Auriclesqccastellateexcision.jpg)
![The final result of the excision[9].](/images/c/cc/Auricle003.jpg)