|
|
| (26 intermediate revisions by 4 users not shown) |
| Line 1: |
Line 1: |
| __NOTOC__ | | __NOTOC__ |
| {{CMG}} | | |
| | {{CMG}}{{AE}}{{Mazia}} |
| {{Infobox_Disease | | | {{Infobox_Disease | |
| Name = {{PAGENAME}} | | | Name = {{PAGENAME}} | |
| Line 14: |
Line 15: |
| eMedicineTopic = 198 | | | eMedicineTopic = 198 | |
| }} | | }} |
| {{SI}} | | {{SK}}SIBO; small bowel bacterial overgrowth.{{SI}} |
| ==Overview== | | ==Overview== |
| | Small intestinal bacterial overgrowth (SIBO) was first discovered by Barber and Hummel in 1939. There is no established system for the [[classification]] of small intestinal bacterial overgrowth (SIBO).The [[pathogenesis]] of small intestinal bacterial overgrowth (SIBO) is characterized by an increased [[Microbial|microbial load]] in the [[Small intestine|small intestine.]] Disruption of protective [[homeostatic]] [[Mechanisms of action|mechanisms]] can increase the risk of SIBO. [[Bacterial|Bacterial colonization]] causes an [[inflammatory]] response in the [[intestinal mucosa]]. Damage to the [[intestinal mucosa]] leads to [[malabsorption]] of [[Bile acid|bile acids]], [[carbohydrates]], [[proteins]] and [[vitamins]] resulting in [[symptoms]] of [[diarrhea]] and [[weight loss]]. On [[gross pathology]], [[Mucosal|mucosal edema]], loss of normal vascular pattern, [[Erythema|patchy erythema]], friability and [[ulceration]] of the [[Small intestinal|small intestinal wall]] is associated with small intestinal bacterial overgrowth (SIBO). On [[microscopic]] [[histopathological]] [[analysis]] [[small intestine]] and [[colon]] are [[normal]] in most [[patients]] with SIBO. Findings include blunting of the [[intestinal villi]], thinning of the [[Mucosal|mucosa]] and [[Crypt (anatomy)|crypts]], increased [[Intraepithelial lymphocyte|intraepithelial lymphocytes]]. Small intestinal bacterial overgrowth (SIBO) must be differentiated from other diseases that cause [[chronic]] [[diarrhea]]. Small intestinal bacterial overgrowth is more commonly observed among [[elderly]] [[patients]]. Small intestinal bacterial overgrowth (SIBO) affects [[men]] and [[women]] equally.There is no [[racial]] predilection for small intestinal bacterial overgrowth (SIBO). Early [[clinical]] features include [[bloating]], [[flatulence]], [[abdominal pain]]. If left untreated, [[patients]] with small intestinal bacterial overgrowth (SIBO) may progress to develop [[diarrhea]], [[dyspepsia]] and [[weight loss]]. [[Prognosis]] is generally good and associated with frequent [[Relapse|relapses]] and [[symptom]]-free periods. The [[diagnosis]] of small intestinal bacterial overgrowth (SIBO) is made when at least one of the following [[diagnostic criteria]] are met: a [[positive]] [[carbohydrate]] [[breath]] [[test]] or [[bacterial]] [[concentration]] of >103 units/mL in a [[Jejunum|jejunal]] [[aspirate]] [[Culture medium|culture]]. [[Physical examination]] may be remarkable for [[distended abdomen]] with positive succussion splash as a result of distended [[bowel]] loops and [[peripheral edema]] due to [[malabsorption]]. Small intestinal bacterial obstruction(SIBO) may also be [[Diagnosis|diagnosed]] using [[breath]] [[Test|tests]]. The mainstay of [[therapy]] for small intestinal bacterial overgrowth (SIBO) is [[antibiotic therapy]]. Surgical approach can only be performed for [[patients]] with [[strictures]], [[fistulae]], and [[Diverticular|diverticula]] or any other structural abnormality resulting in [[obstruction]] and resultant bacterial overgrowth. Effective measures for the [[prevention]] of small bowel bacterial overgrowth syndrome include avoiding [[medications]] like [[narcotics]] and [[benzodiazepines]] that decrease [[Intestinal|intestinal motility]] and avoid [[achlorhydria]] in high-risk [[patients]]. Consider [[Antibiotic|antibiotic prophylaxis]] for [[patients]] with four or more episodes of recurrent [[small bowel]] bacterial overgrowth syndrome within one year. |
|
| |
|
| ==Historical Perspective== | | ==Historical Perspective== |
| *Small intestinal bacterial overgrowth (SIBO) was first discovered by Barber and Hummel in 1939. | | *Small intestinal bacterial overgrowth (SIBO) was first discovered by Barber and Hummel in 1939. |
| *In 2000, Pimentel et all at Cedars-Sinai Medical Center were first identified that SIBO was present in 78% of patients with irritable bowel syndrome (IBS), and that treatment with antibiotics improved symptoms. | | *In 2000, Pimentel et all at Cedars-Sinai Medical Center first identified that SIBO was present in 78% of patients with [[Irritable bowel syndrome|irritable bowel syndrome (IBS)]], and that [[Treatment IND|treatment]] with [[antibiotics]] improved [[symptoms]]<ref name="pmid11151884">{{cite journal| author=Pimentel M, Chow EJ, Lin HC| title=Eradication of small intestinal bacterial overgrowth reduces symptoms of irritable bowel syndrome. | journal=Am J Gastroenterol | year= 2000 | volume= 95 | issue= 12 | pages= 3503-6 | pmid=11151884 | doi=10.1111/j.1572-0241.2000.03368.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11151884 }} </ref>. |
| *In May 2015, U.S. Food and Drug Administration (FDA) approved rifaximin to treat SIBO. | | *In May 2015, U.S. [[Food and Drug Administration|Food and Drug Administration (FDA)]] approved [[rifaximin]] to treat SIBO. |
|
| |
|
| ==Classification== | | ==Classification== |
| *There is no established system for the classification of small intestinal bacterial overgrowth(SIBO). | | *There is no established system for the [[classification]] of small intestinal bacterial overgrowth (SIBO). |
|
| |
|
| ==Pathophysiology== | | ==Pathophysiology== |
| *The pathogenesis of small intestinal bacterial overgrowth (SIBO) is characterized by an increased microbial load in the small intestine. | | *The [[pathogenesis]] of small intestinal bacterial overgrowth (SIBO) is characterized by an increased [[microbial]] load in the [[small intestine]].<ref name="pmid3890541">{{cite journal |vauthors=Mathias JR, Clench MH |title=Review: pathophysiology of diarrhea caused by bacterial overgrowth of the small intestine |journal=Am. J. Med. Sci. |volume=289 |issue=6 |pages=243–8 |year=1985 |pmid=3890541 |doi= |url=}}</ref><ref name="pmid15156063">{{cite journal |vauthors=Hao WL, Lee YK |title=Microflora of the gastrointestinal tract: a review |journal=Methods Mol. Biol. |volume=268 |issue= |pages=491–502 |year=2004 |pmid=15156063 |doi=10.1385/1-59259-766-1:491 |url=}}</ref><ref name="pmid20572300">{{cite journal |vauthors=Bures J, Cyrany J, Kohoutova D, Förstl M, Rejchrt S, Kvetina J, Vorisek V, Kopacova M |title=Small intestinal bacterial overgrowth syndrome |journal=World J. Gastroenterol. |volume=16 |issue=24 |pages=2978–90 |year=2010 |pmid=20572300 |pmc=2890937 |doi= |url=}}</ref> |
| *A healthy individual has less than 103 organisms/mL in the upper small intestine, and the majority of these organisms are gram-positive bacteria. | | *A [[healthy]] individual has less than 103 organisms/mL in the upper [[small intestine]] and the majority of these [[organisms]] are [[gram-positive bacteria]]. |
| *Body's homeostatic mechanisms protect against excessive small intestinal colonization by bacteria include : | | *[[Human body|Human body's]] [[Homeostatic|homeostatic mechanisms]] that protect against excessive [[small intestinal]] colonization by [[Bacterial|bacteria]] include : |
| **Gastric acid and bile eradicate micro-organisms before they leave the stomach | | **[[Gastric acid]] and [[bile]] eradicate [[micro-organisms]] before they leave the [[stomach]]. |
| **Migrating motor complex clears the excess unwanted bacteria of upper intestine | | **[[Migrating motor complex]] clears the excess bacteria of upper intestine. |
| **Intestinal mucosa serves as a protective layer for the gut wall. | | **[[Intestinal]] [[mucosa]] serves as a [[Protecting group|protective layer]] for the [[Gut tract|gut wall]]. |
| **Normal intestinal flora (eg, Lactobacillus) maintains a low pH that prevents bacterial overgrowth. | | **Normal [[intestinal flora]] (eg, [[Lactobacillus]]) maintains a low [[pH]] that prevents bacterial overgrowth. |
| **Physical barrier of the ileocecal valve that prevents retrograde translocation of bacteria from colon to the small intestine. | | **Physical barrier of the [[ileocecal]] [[valve]] that prevents retrograde translocation of [[bacteria]] from [[colon]] to the [[small intestine]]. |
| *Disruption of these protective homeostatic mechanisms can increase the risk of SIBO. | | *Disruption of these protective [[Homeostatic|homeostatic mechanisms]] can increase the risk of SIBO. |
| *Bacterial colonization causes an inflammatory response in the intestinal mucosa. | | *[[Bacterial|Bacterial colonization]] causes an [[inflammatory]] response in the [[intestinal mucosa]]. |
| *Damage to the intestinal mucosa leads to malabsorption of bile acids, carbohydrates, proteins and vitamins resulting in symptoms of diarrhea and weightloss. | | *Damage to the [[intestinal mucosa]] leads to [[malabsorption]] of [[Bile acid|bile acids]], [[carbohydrates]], [[proteins]], and [[vitamins]] resulting in [[symptoms]] of [[diarrhea]] and [[weight loss]]. |
| *On gross pathology, mucosal edema, loss of normal vascular pattern, patchy erythema, friability and ulceration of the small intestinal wall is associated with small intestinal bacterial overgrowth (SIBO). | | *On [[gross pathology]], [[mucosal]] [[edema]], loss of normal [[vascular]] pattern, patchy [[erythema]], friability and [[ulceration]] of the [[Small intestinal|small intestinal wall]] is associated with small intestinal bacterial overgrowth (SIBO). |
| *On microscopic histopathological analysis small intestine and colon is normal in most patients with SIBO. Findings include: | | *On [[microscopic]] [[histopathological]] [[analysis]] [[small intestine]] and [[colon]] is normal in most [[patients]] with SIBO. However, in some patients, findings may include: |
| **Blunting of the intestinal villi | | **Blunting of the [[intestinal]] [[villi]] |
| **Thinning of the mucosa and crypts | | **Thinning of the [[mucosa]] and [[Crypt (anatomy)|crypts]] |
| **Increased intraepithelial lymphocytes | | **Increased [[Intraepithelial lymphocyte|intraepithelial lymphocytes]] |
| ==Causes== | | ==Causes== |
| *Small intestinal bacterial overgrowth (SIBO) may be caused by disruption of the protective homeostatic mechanisms that control enteric bacteria population. | | *Small intestinal bacterial overgrowth (SIBO) may be caused by disruption of the [[Protective group|protective]] [[homeostatic]] [[Mechanisms of action|mechanisms]] that control [[enteric]] [[Bacterial|bacteria]] [[population]].<ref name="pmid27123301">{{cite journal |vauthors=Deng L, Liu Y, Zhang D, Li Y, Xu L |title=Prevalence and treatment of small intestinal bacterial overgrowth in postoperative patients with colorectal cancer |journal=Mol Clin Oncol |volume=4 |issue=5 |pages=883–887 |year=2016 |pmid=27123301 |pmc=4840787 |doi=10.3892/mco.2016.807 |url=}}</ref><ref name="pmid20572300">{{cite journal |vauthors=Bures J, Cyrany J, Kohoutova D, Förstl M, Rejchrt S, Kvetina J, Vorisek V, Kopacova M |title=Small intestinal bacterial overgrowth syndrome |journal=World J. Gastroenterol. |volume=16 |issue=24 |pages=2978–90 |year=2010 |pmid=20572300 |pmc=2890937 |doi= |url=}}</ref><ref name="pmid6412829">{{cite journal |vauthors=McEvoy A, Dutton J, James OF |title=Bacterial contamination of the small intestine is an important cause of occult malabsorption in the elderly |journal=Br Med J (Clin Res Ed) |volume=287 |issue=6395 |pages=789–93 |year=1983 |pmid=6412829 |pmc=1549133 |doi= |url=}}</ref> |
| *Causes of small intestinal bacterial overgrowth (SIBO) include: | | *Causes of small intestinal bacterial overgrowth (SIBO) include: |
| **Irregular small intestinal motility | | **'''Irregular [[small intestinal]] [[motility]]:''' |
| ***Diabetic autonomic neuropathy | | ***[[Diabetic]] [[autonomic]] [[neuropathy]] |
| ***Scleroderma | | ***[[Scleroderma]] |
| ***Pseudo-obstruction | | ***[[Pseudo-obstruction-intestinal|Pseudo-obstruction]] |
| ***Amyloidosis | | ***[[Amyloidosis]] |
| ***Neurological diseases (eg, myotonic dystrophy, Parkinson disease) | | ***[[Neurological]] [[diseases]] (eg, [[myotonic]] [[dystrophy]], [[Parkinson]] [[disease]]) |
| ***Radiation enteritis | | ***[[Radiation]] [[enteritis]] |
| ***Crohn disease | | ***[[Crohn disease]] |
| ***Hypothyroidism | | ***[[Hypothyroidism]] |
| **Blind pouches in the gastrointestinal tract | | **'''Blind pouches in the gastrointestinal tract:''' |
| ***Side-to-side or end-to-side anastomoses | | ***Side-to-side or end-to-side [[anastomoses]] |
| ***Duodenal or jejunal diverticula | | ***[[Duodenal]] or [[Jejunum|jejunal]] [[Diverticular|diverticula]] |
| ***Segmental dilatation of the ileum | | ***Segmental dilatation of the [[ileum]] |
| ***Blind loop syndrome | | ***[[Blind loop syndrome]] |
| ***Biliopancreatic diversion | | ***Biliopancreatic diversion |
| ***Chagasic megacolon | | ***[[Megacolon|Chagasic megacolon]] |
| **Fistula | | **'''[[Fistula]]:''' |
| ***Gastrocolic fistulae | | ***[[Fistulae|Gastrocolic fistulae]] |
| ***Jejunal-colic fistulae | | ***[[Fistulae|Jejunal-colic fistulae]] |
| **Partial Obstruction | | **'''Partial [[Obstruction]]:''' |
| ***Strictures | | ***[[Strictures]] |
| ***Adhesions | | ***[[Adhesions]] |
| ***Abdominal masses | | ***[[Abdominal]] [[Mass|masses]] |
| ***Leiomyosarcoma | | ***[[Leiomyosarcoma]] |
| **Decreased gastric acid secretion | | **'''Decreased [[gastric acid]] [[Secretions|secretion]]:''' |
| ***Achlorhydria | | ***[[Achlorhydria]] |
| ***Vagotomy | | ***[[Vagotomy]] |
| ***Long-term proton pump inhibitor therapy | | ***Long-term [[proton pump inhibitor]] [[therapy]] |
| | |
| | ==Differentiating Small Intestinal Bacterial Overgrowth from other Diseases== |
| | *Small intestinal bacterial overgrowth (SIBO) must be differentiated from other diseases that cause chronic diarrhea. For differential diagnosis of chronic diarrhoea, click '''[[Chronic diarrhea differential diagnosis|here]].''' |
| | ==Epidemiology and Demographics== |
| | Epidemiology and demographics of small intestinal bacterial overgrowth is as follows: <ref name="pmid437407">{{cite journal |vauthors=King CE, Toskes PP |title=Small intestine bacterial overgrowth |journal=Gastroenterology |volume=76 |issue=5 Pt 1 |pages=1035–55 |year=1979 |pmid=437407 |doi= |url=}}</ref> |
| | ===Age=== |
| | *Small intestinal bacterial overgrowth is more commonly observed among [[elderly]] [[patients]]. |
| | ===Gender=== |
| | *Small intestinal bacterial overgrowth (SIBO) affects [[men]] and [[women]] equally. |
| | ===Race=== |
| | *There is no [[racial]] predilection for small intestinal bacterial overgrowth (SIBO). |
| | |
| | ==Risk Factors== |
| | *Common [[risk factors]] in the development of small intestinal bacterial overgrowth (SIBO) are :<ref name="pmid6412829">{{cite journal |vauthors=McEvoy A, Dutton J, James OF |title=Bacterial contamination of the small intestine is an important cause of occult malabsorption in the elderly |journal=Br Med J (Clin Res Ed) |volume=287 |issue=6395 |pages=789–93 |year=1983 |pmid=6412829 |pmc=1549133 |doi= |url=}}</ref><ref name="pmid20572300">{{cite journal |vauthors=Bures J, Cyrany J, Kohoutova D, Förstl M, Rejchrt S, Kvetina J, Vorisek V, Kopacova M |title=Small intestinal bacterial overgrowth syndrome |journal=World J. Gastroenterol. |volume=16 |issue=24 |pages=2978–90 |year=2010 |pmid=20572300 |pmc=2890937 |doi= |url=}}</ref> |
| | **[[Intestinal tract]] [[surgery]] |
| | **[[Irritable bowel syndrome]]<ref name="pmid31750966">{{cite journal| author=Ghoshal UC, Nehra A, Mathur A, Rai S| title=A meta-analysis on small intestinal bacterial overgrowth in patients with different subtypes of irritable bowel syndrome. | journal=J Gastroenterol Hepatol | year= 2020 | volume= 35 | issue= 6 | pages= 922-931 | pmid=31750966 | doi=10.1111/jgh.14938 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=31750966 }} </ref> |
| | **[[Liver cirrhosis]] |
| | **[[Celiac disease]] |
| | **[[Immune]] [[deficiency]] (eg, [[AIDS]], [[IgA deficiency]], [[Malnutrition|severe malnutrition]]) |
| | **[[Short bowel syndrome]] |
| | **[[End-stage renal disease]] |
| | **Gastrojejunal [[anastomosis]] |
| | **Antral [[resection]] |
| | **[[Pancreatic]] [[exocrine]] insufficiency |
| | |
| | == Natural History, Complications and Prognosis== |
| | *Early [[clinical]] [[Features (pattern recognition)|features]] include [[bloating]], [[flatulence]], [[abdominal pain]].<ref name="pmid437407">{{cite journal |vauthors=King CE, Toskes PP |title=Small intestine bacterial overgrowth |journal=Gastroenterology |volume=76 |issue=5 Pt 1 |pages=1035–55 |year=1979 |pmid=437407 |doi= |url=}}</ref><ref name="pmid15156063">{{cite journal |vauthors=Hao WL, Lee YK |title=Microflora of the gastrointestinal tract: a review |journal=Methods Mol. Biol. |volume=268 |issue= |pages=491–502 |year=2004 |pmid=15156063 |doi=10.1385/1-59259-766-1:491 |url=}}</ref> |
| | *If left untreated, [[patients]] with small intestinal bacterial overgrowth (SIBO) may progress to develop [[diarrhea]], [[dyspepsia]] and [[weight loss]]. |
| | *Common [[complications]] of small intestinal bacterial overgrowth (SIBO) include:<ref name="pmid7805370">{{cite journal |vauthors=Saltzman JR, Russell RM |title=Nutritional consequences of intestinal bacterial overgrowth |journal=Compr Ther |volume=20 |issue=9 |pages=523–30 |year=1994 |pmid=7805370 |doi= |url=}}</ref> |
| | **[[Iron]] [[deficiency]] resulting in [[microcytic]] [[anemia]] |
| | **[[Vitamin B-12]] or [[folate deficiency]] resulting in [[macrocytic anemia]] |
| | **[[Vitamin B-12|Vitamin B-12 deficiency]] associated [[polyneuropathy]] |
| | **[[Steatorrhea]] |
| | **[[Hypocalcemia]] |
| | **[[Vitamin A deficiency]] resulting in [[night blindness]] |
| | **[[Selenium deficiency]] causing [[dermatitis]] |
| | **[[Rosacea]] |
| | **[[Cachexia]] as a result of [[Protein energy malnutrition|protein-energy malnutrition]] |
| | *[[Prognosis]] is generally good and associated with frequent [[Relapse|relapses]] and [[symptom]]-free [[periods]]. |
| | |
| | == Diagnosis == |
| | ===Diagnostic Criteria=== |
| | |
| | [[Clinical practice guideline]]s by the American College of Gastroenterology guide diagnosis<ref name="pmid32023228">{{cite journal| author=Pimentel M, Saad RJ, Long MD, Rao SSC| title=ACG Clinical Guideline: Small Intestinal Bacterial Overgrowth. | journal=Am J Gastroenterol | year= 2020 | volume= 115 | issue= 2 | pages= 165-178 | pmid=32023228 | doi=10.14309/ajg.0000000000000501 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32023228 }} </ref>. |
| | *The [[diagnosis]] of small intestinal bacterial overgrowth (SIBO) is made when at least one of the following [[diagnostic]] [[criteria]] are met: |
| | **A [[positive]] [[carbohydrate]] [[breath]] [[test]] with an increase in hydrogen concentrations of 20 ppm from baseline within 90 - 120 minutes. |
| | **[[Bacterial]] [[Concentrations|concentration]] of >= 10<sup>3</sup> colony-forming units per milliliter (CFU/mL) in a duodenal/jejunal aspirate |
| | |
| | === Symptoms === |
| | *[[Symptoms]] of small intestinal bacterial overdose (SIBO) may include the following:<ref name="pmid7805370">{{cite journal |vauthors=Saltzman JR, Russell RM |title=Nutritional consequences of intestinal bacterial overgrowth |journal=Compr Ther |volume=20 |issue=9 |pages=523–30 |year=1994 |pmid=7805370 |doi= |url=}}</ref> |
| | :*[[Bloating]] |
| | :*[[Flatulence]] |
| | :*[[Abdominal discomfort]] |
| | :*[[Chronic]] [[watery diarrhea]] |
| | :*[[Weight loss]] |
| | |
| | === Physical Examination === |
| | *[[Patients]] with small intestinal bacterial overgrowth (SIBO) usually appear normal.<ref name="pmid15156063">{{cite journal |vauthors=Hao WL, Lee YK |title=Microflora of the gastrointestinal tract: a review |journal=Methods Mol. Biol. |volume=268 |issue= |pages=491–502 |year=2004 |pmid=15156063 |doi=10.1385/1-59259-766-1:491 |url=}}</ref> |
| | *[[Physical examination]] may be remarkable for: |
| | :*[[Distended abdomen]] with [[positive]] succussion splash as a result of distended [[bowel]] loops |
| | :*[[Peripheral edema]] due to [[malabsorption]] |
| | |
| | === Laboratory Findings === |
| | *A [[positive]] [[carbohydrate]] [[breath]] [[test]] has a sensitivity of 55% and specificity of 82% of small intestinal bacterial overgrowth (SIBO).<ref name="pmid31743632">{{cite journal| author=Losurdo G, Leandro G, Ierardi E, Perri F, Barone M, Principi M | display-authors=etal| title=Breath Tests for the Non-invasive Diagnosis of Small Intestinal Bacterial Overgrowth: A Systematic Review With Meta-analysis. | journal=J Neurogastroenterol Motil | year= 2020 | volume= 26 | issue= 1 | pages= 16-28 | pmid=31743632 | doi=10.5056/jnm19113 | pmc=6955189 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=31743632 }} </ref> |
| | *An elevated concentration of [[bacterial]] [[Colony Forming Units (CFU)|colony forming units]] >103/mL in [[Jejunum|jejunal]] [[aspirate]] culture is [[diagnostic]] of small intestinal bacterial overgrowth (SIBO). |
| | *Other [[laboratory]] findings consistent with the [[diagnosis]] of small intestinal bacterial overgrowth (SIBO) include: |
| | **[[Macrocytic anemia]] |
| | **[[B12 deficiency]] |
| | **Presence of [[fecal fat]] on [[stool examination]]. |
| | **Low levels of [[thiamine]] and [[niacin]] |
| | **Elevated serum [[folate]] and [[vitamin K]] levels |
| | |
| | ===Imaging Findings=== |
| | *The [[CT-scans|CT]] [[abdomen]] or [[MRI]] may demonstrate associated [[strictures]], [[Malrotation of gut|malrotation]], [[fistulae]].<ref name="pmid15156063">{{cite journal |vauthors=Hao WL, Lee YK |title=Microflora of the gastrointestinal tract: a review |journal=Methods Mol. Biol. |volume=268 |issue= |pages=491–502 |year=2004 |pmid=15156063 |doi=10.1385/1-59259-766-1:491 |url=}}</ref> |
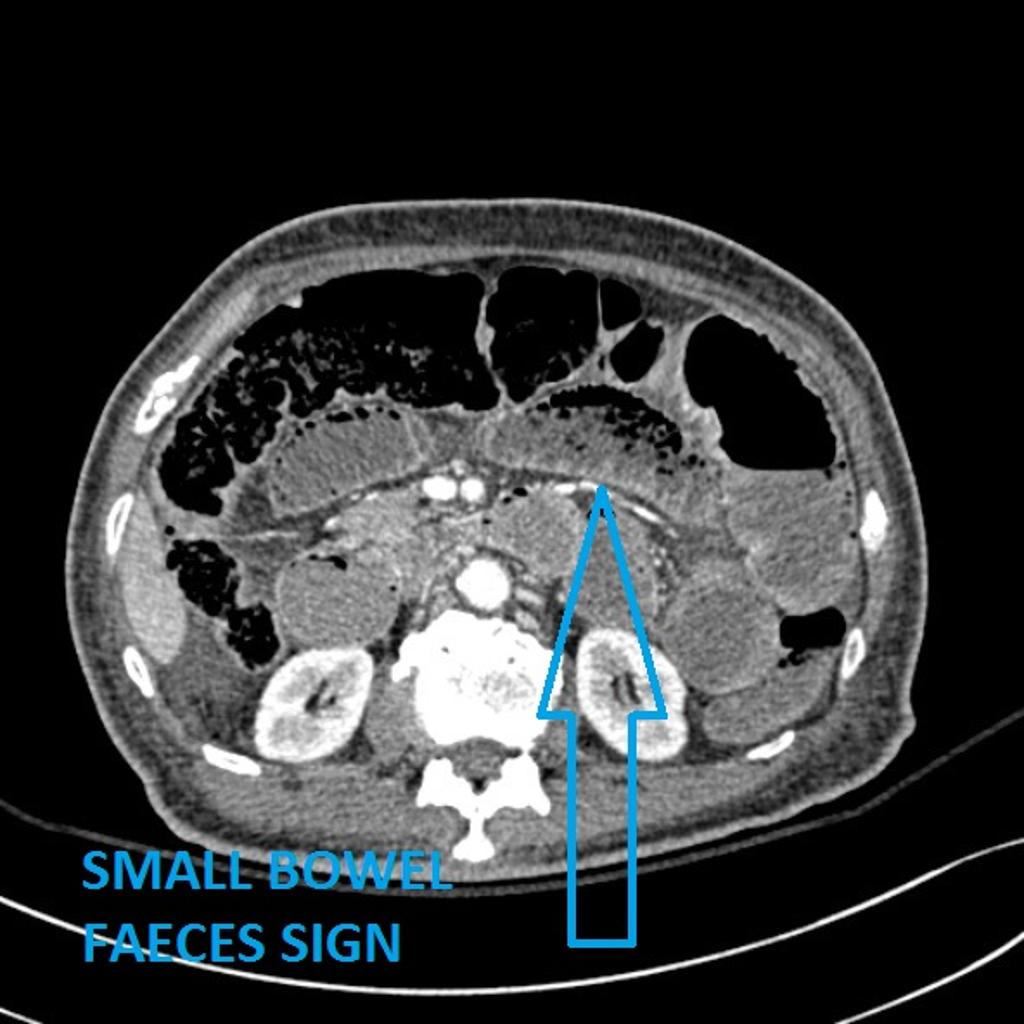
| | *Small intestinal bacterial overgrowth can result in [[small bowel obstruction]] that presents as [[small bowel]] feces sign on abdominal CT. |
| | *Small bowel feces sign is the presence of particulate feculent material mingled with gas bubbles in the lumen of the small intestine, it is believed to be the result of delayed intestinal transit. |
| | [[File:Ischaemic-bowel-5.jpg||center|400px|thumb|Small bowel faeces sign<small>Case courtesy of Dr Ian Bickle, <a href="https://radiopaedia.org/">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/29769">rID: 29769</a></small>]] |
|
| |
|
| ==Differentiating [disease name] from other Diseases== | | ===Other Diagnostic Studies=== |
| *Small intestinal bacterial overgrowth (SIBO) must be differentiated from other diseases that cause chronic diarrhea.
| | ====Breath Tests==== |
| '''The following table outlines the major differential diagnoses of chronic diarrhea.'''<ref name="Casburn-JonesFarthing2004">{{cite journal|last1=Casburn-Jones|first1=Anna C|last2=Farthing|first2=Michael Jg|title=Traveler's diarrhea|journal=Journal of Gastroenterology and Hepatology|volume=19|issue=6|year=2004|pages=610–618|issn=0815-9319|doi=10.1111/j.1440-1746.2003.03287.x}}</ref><ref name="KamatMathur2006">{{cite journal|last1=Kamat|first1=Deepak|last2=Mathur|first2=Ambika|title=Prevention and Management of Travelers’ Diarrhea|journal=Disease-a-Month|volume=52|issue=7|year=2006|pages=289–302|issn=00115029|doi=10.1016/j.disamonth.2006.08.003}}</ref><ref name="PfeifferDuPont2012">{{cite journal|last1=Pfeiffer|first1=Margaret L.|last2=DuPont|first2=Herbert L.|last3=Ochoa|first3=Theresa J.|title=The patient presenting with acute dysentery – A systematic review|journal=Journal of Infection|volume=64|issue=4|year=2012|pages=374–386|issn=01634453|doi=10.1016/j.jinf.2012.01.006}}</ref><ref name="pmid24506120">{{cite journal |vauthors=Barr W, Smith A |title=Acute diarrhea |journal=Am Fam Physician |volume=89 |issue=3 |pages=180–9 |year=2014 |pmid=24506120 |doi= |url=}}</ref><ref name="pmid29255768">{{cite journal |vauthors=Amil Dias J |title=Celiac Disease: What Do We Know in 2017? |journal=GE Port J Gastroenterol |volume=24 |issue=6 |pages=275–278 |year=2017 |pmid=29255768 |doi=10.1159/000479881 |url=}}</ref><ref name="pmid29254859">{{cite journal |vauthors=Kotloff KL, Riddle MS, Platts-Mills JA, Pavlinac P, Zaidi AKM |title=Shigellosis |journal=Lancet |volume= |issue= |pages= |year=2017 |pmid=29254859 |doi=10.1016/S0140-6736(17)33296-8 |url=}}</ref><ref name="Yamamoto-FurushoBosques-Padilla2017">{{cite journal|last1=Yamamoto-Furusho|first1=J.K.|last2=Bosques-Padilla|first2=F.|last3=de-Paula|first3=J.|last4=Galiano|first4=M.T.|last5=Ibañez|first5=P.|last6=Juliao|first6=F.|last7=Kotze|first7=P.G.|last8=Rocha|first8=J.L.|last9=Steinwurz|first9=F.|last10=Veitia|first10=G.|last11=Zaltman|first11=C.|title=Diagnóstico y tratamiento de la enfermedad inflamatoria intestinal: Primer Consenso Latinoamericano de la Pan American Crohn's and Colitis Organisation|journal=Revista de Gastroenterología de México|volume=82|issue=1|year=2017|pages=46–84|issn=03750906|doi=10.1016/j.rgmx.2016.07.003}}</ref><ref name="BorbélyOsterwalder2017">{{cite journal|last1=Borbély|first1=Yves M|last2=Osterwalder|first2=Alice|last3=Kröll|first3=Dino|last4=Nett|first4=Philipp C|last5=Inglin|first5=Roman A|title=Diarrhea after bariatric procedures: Diagnosis and therapy|journal=World Journal of Gastroenterology|volume=23|issue=26|year=2017|pages=4689|issn=1007-9327|doi=10.3748/wjg.v23.i26.4689}}</ref><ref name="CrawfordRamani2017">{{cite journal|last1=Crawford|first1=Sue E.|last2=Ramani|first2=Sasirekha|last3=Tate|first3=Jacqueline E.|last4=Parashar|first4=Umesh D.|last5=Svensson|first5=Lennart|last6=Hagbom|first6=Marie|last7=Franco|first7=Manuel A.|last8=Greenberg|first8=Harry B.|last9=O'Ryan|first9=Miguel|last10=Kang|first10=Gagandeep|last11=Desselberger|first11=Ulrich|last12=Estes|first12=Mary K.|title=Rotavirus infection|journal=Nature Reviews Disease Primers|volume=3|year=2017|pages=17083|issn=2056-676X|doi=10.1038/nrdp.2017.83}}</ref><ref name="pmid11068510">{{cite journal |vauthors=Kist M |title=[Chronic diarrhea: value of microbiology in diagnosis] |language=German |journal=Praxis (Bern 1994) |volume=89 |issue=39 |pages=1559–65 |year=2000 |pmid=11068510 |doi= |url=}}</ref><ref name="pmid4014291">{{cite journal |vauthors=Guerrant RL, Shields DS, Thorson SM, Schorling JB, Gröschel DH |title=Evaluation and diagnosis of acute infectious diarrhea |journal=Am. J. Med. |volume=78 |issue=6B |pages=91–8 |year=1985 |pmid=4014291 |doi= |url=}}</ref><ref name="pmid10575169">{{cite journal |vauthors=López-Vélez R, Turrientes MC, Garrón C, Montilla P, Navajas R, Fenoy S, del Aguila C |title=Microsporidiosis in travelers with diarrhea from the tropics |journal=J Travel Med |volume=6 |issue=4 |pages=223–7 |year=1999 |pmid=10575169 |doi= |url=}}</ref><ref name="WahnschaffeIgnatius2009">{{cite journal|last1=Wahnschaffe|first1=Ulrich|last2=Ignatius|first2=Ralf|last3=Loddenkemper|first3=Christoph|last4=Liesenfeld|first4=Oliver|last5=Muehlen|first5=Marion|last6=Jelinek|first6=Thomas|last7=Burchard|first7=Gerd Dieter|last8=Weinke|first8=Thomas|last9=Harms|first9=Gundel|last10=Stein|first10=Harald|last11=Zeitz|first11=Martin|last12=Ullrich|first12=Reiner|last13=Schneider|first13=Thomas|title=Diagnostic value of endoscopy for the diagnosis of giardiasis and other intestinal diseases in patients with persistent diarrhea from tropical or subtropical areas|journal=Scandinavian Journal of Gastroenterology|volume=42|issue=3|year=2009|pages=391–396|issn=0036-5521|doi=10.1080/00365520600881193}}</ref><ref name="pmid27765536">{{cite journal |vauthors=Mena Bares LM, Carmona Asenjo E, García Sánchez MV, Moreno Ortega E, Maza Muret FR, Guiote Moreno MV, Santos Bueno AM, Iglesias Flores E, Benítez Cantero JM, Vallejo Casas JA |title=75SeHCAT scan in bile acid malabsorption in chronic diarrhoea |journal=Rev Esp Med Nucl Imagen Mol |volume=36 |issue=1 |pages=37–47 |year=2017 |pmid=27765536 |doi=10.1016/j.remn.2016.08.005 |url=}}</ref><ref name="pmid19365159">{{cite journal |vauthors=Gibson RJ, Stringer AM |title=Chemotherapy-induced diarrhoea |journal=Curr Opin Support Palliat Care |volume=3 |issue=1 |pages=31–5 |year=2009 |pmid=19365159 |doi=10.1097/SPC.0b013e32832531bb |url=}}</ref><ref name="pmid23384808">{{cite journal |vauthors=Abraham BP, Sellin JH |title=Drug-induced, factitious, & idiopathic diarrhoea |journal=Best Pract Res Clin Gastroenterol |volume=26 |issue=5 |pages=633–48 |year=2012 |pmid=23384808 |doi=10.1016/j.bpg.2012.11.007 |url=}}</ref><ref name="pmid25692805">{{cite journal |vauthors=Reintam Blaser A, Deane AM, Fruhwald S |title=Diarrhoea in the critically ill |journal=Curr Opin Crit Care |volume=21 |issue=2 |pages=142–53 |year=2015 |pmid=25692805 |doi=10.1097/MCC.0000000000000188 |url=}}</ref><ref name="pmid17373914">{{cite journal |vauthors=McMahan ZH, DuPont HL |title=Review article: the history of acute infectious diarrhoea management--from poorly focused empiricism to fluid therapy and modern pharmacotherapy |journal=Aliment. Pharmacol. Ther. |volume=25 |issue=7 |pages=759–69 |year=2007 |pmid=17373914 |doi=10.1111/j.1365-2036.2007.03261.x |url=}}</ref><ref name="pmid23384801">{{cite journal |vauthors=Schiller LR |title=Definitions, pathophysiology, and evaluation of chronic diarrhoea |journal=Best Pract Res Clin Gastroenterol |volume=26 |issue=5 |pages=551–62 |year=2012 |pmid=23384801 |doi=10.1016/j.bpg.2012.11.011 |url=}}</ref><ref name="pmid3523719">{{cite journal |vauthors=Giannella RA |title=Chronic diarrhea in travelers: diagnostic and therapeutic considerations |journal=Rev. Infect. Dis. |volume=8 Suppl 2 |issue= |pages=S223–6 |year=1986 |pmid=3523719 |doi= |url=}}</ref><ref name="pmid16151544">{{cite journal| author=Silverberg MS, Satsangi J, Ahmad T, Arnott ID, Bernstein CN, Brant SR et al.| title=Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a Working Party of the 2005 Montreal World Congress of Gastroenterology. | journal=Can J Gastroenterol | year= 2005 | volume= 19 Suppl A | issue= | pages= 5A-36A | pmid=16151544 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16151544 }}</ref><ref name="pmid12135027">{{cite journal| author=Sauter GH, Moussavian AC, Meyer G, Steitz HO, Parhofer KG, Jüngst D| title=Bowel habits and bile acid malabsorption in the months after cholecystectomy. | journal=Am J Gastroenterol | year= 2002 | volume= 97 | issue= 7 | pages= 1732-5 | pmid=12135027 | doi=10.1111/j.1572-0241.2002.05779.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12135027 }}</ref><ref name="pmid1702075">{{cite journal| author=Maiuri L, Raia V, Potter J, Swallow D, Ho MW, Fiocca R et al.| title=Mosaic pattern of lactase expression by villous enterocytes in human adult-type hypolactasia. | journal=Gastroenterology | year= 1991 | volume= 100 | issue= 2 | pages= 359-69 | pmid=1702075 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1702075 }}</ref><ref name="pmid14439871">{{cite journal| author=RUBIN CE, BRANDBORG LL, PHELPS PC, TAYLOR HC| title=Studies of celiac disease. I. The apparent identical and specific nature of the duodenal and proximal jejunal lesion in celiac disease and idiopathic sprue. | journal=Gastroenterology | year= 1960 | volume= 38 | issue= | pages= 28-49 | pmid=14439871 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14439871 }}</ref><ref name="pmid8209928">{{cite journal| author=Konvolinka CW| title=Acute diverticulitis under age forty. | journal=Am J Surg | year= 1994 | volume= 167 | issue= 6 | pages= 562-5 | pmid=8209928 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8209928 }} </ref><ref name="pmid16698746">{{cite journal| author=Satsangi J, Silverberg MS, Vermeire S, Colombel JF| title=The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. | journal=Gut | year= 2006 | volume= 55 | issue= 6 | pages= 749-53 | pmid=16698746 | doi=10.1136/gut.2005.082909 | pmc=1856208 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16698746 }} </ref><ref name="pmid12700377">{{cite journal| author=Haque R, Huston CD, Hughes M, Houpt E, Petri WA| title=Amebiasis. | journal=N Engl J Med | year= 2003 | volume= 348 | issue= 16 | pages= 1565-73 | pmid=12700377 | doi=10.1056/NEJMra022710 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12700377 }} </ref><ref name="pmid8694025">{{cite journal| author=Hertzler SR, Savaiano DA| title=Colonic adaptation to daily lactose feeding in lactose maldigesters reduces lactose intolerance. | journal=Am J Clin Nutr | year= 1996 | volume= 64 | issue= 2 | pages= 232-6 | pmid=8694025 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8694025 }} </ref><ref name="pmid9414969">{{cite journal| author=Briet F, Pochart P, Marteau P, Flourie B, Arrigoni E, Rambaud JC| title=Improved clinical tolerance to chronic lactose ingestion in subjects with lactose intolerance: a placebo effect? | journal=Gut | year= 1997 | volume= 41 | issue= 5 | pages= 632-5 | pmid=9414969 | doi= | pmc=1891556 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9414969 }} </ref><ref name="pmid15391722">{{cite journal| author=BLACK-SCHAFFER B| title=The tinctoral demonstration of a glycoprotein in Whipple's disease. | journal=Proc Soc Exp Biol Med | year= 1949 | volume= 72 | issue= 1 | pages= 225-7 | pmid=15391722 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15391722 }} </ref>
| | *Small intestinal bacterial obstruction (SIBO) may also be [[Diagnose|diagnosed]] using [[breath]] [[Test|tests]].<ref name="pmid10773721">{{cite journal |vauthors=Stotzer PO, Kilander AF |title=Comparison of the 1-gram (14)C-D-xylose breath test and the 50-gram hydrogen glucose breath test for diagnosis of small intestinal bacterial overgrowth |journal=Digestion |volume=61 |issue=3 |pages=165–71 |year=2000 |pmid=10773721 |doi=10.1159/000007753 |url=}}</ref><ref name="pmid24095975">{{cite journal |vauthors=Saad RJ, Chey WD |title=Breath testing for small intestinal bacterial overgrowth: maximizing test accuracy |journal=Clin. Gastroenterol. Hepatol. |volume=12 |issue=12 |pages=1964–72; quiz e119–20 |year=2014 |pmid=24095975 |doi=10.1016/j.cgh.2013.09.055 |url=}}</ref><ref name="pmid437407">{{cite journal |vauthors=King CE, Toskes PP |title=Small intestine bacterial overgrowth |journal=Gastroenterology |volume=76 |issue=5 Pt 1 |pages=1035–55 |year=1979 |pmid=437407 |doi= |url=}}</ref> |
| | *[[Breath]] [[Test|tests]] have the advantage of being easy to perform, noninvasive, and inexpensive. [[Breath]] [[Test|tests]] are based on the principle that [[carbohydrates]] are [[metabolized]] by [[bacteria]] in the [[gut]] to produce [[hydrogen]] or [[methane]] that is [[Absorbed dose|absorbed]] and [[excreted]] in [[breath]]. |
| | *The findings on [[carbohydrate]] [[breath]] [[test]] [[diagnostic]] of small intestinal bacterial obstruction (SIBO) include: |
| | **An increase in [[hydrogen]] by ≥20 ppm above [[Baseline (medicine)|baseline]] within 90 minutes. |
| | **A [[methane]] level ≥10 ppm regardless of the time during the [[breath]] [[test]]. |
| | '''Preparation for breath testing''' |
|
| |
|
| <span style="font-size:85%">'''Abbreviations:''' '''GI:''' [[Gastrointestinal tract|Gastrointestinal]], '''CBC''': [[Complete blood count]], '''WBC:''' [[White blood cells|White blood cell]], '''RBC''': [[Red blood cell]], '''Plt:''' [[Platelet]], '''Hgb:''' [[Hemoglobin]], '''ESR''': [[Erythrocyte sedimentation rate]], '''CRP''': [[C-reactive protein|C–reactive protein]], '''IgE:''' [[Immunoglobulin E]], '''IgA:''' [[Immunoglobulin A]], '''ETEC:''' [[Escherichia coli enteritis]], '''EPEC''': [[Escherichia coli|Enteropathogenic Escherichia coli]], '''EIEC''': [[Escherichia coli enteritis|Enteroinvasive Escherichia coli]], '''EHEC''': [[Escherichia coli|Enterohemorrhagic Escherichia coli]], '''EAEC''': [[Escherichia coli enteritis|Enteroaggregative Escherichia coli]], '''Nl''': Normal, '''ASCA''': [[Anti saccharomyces cerevisiae antibodies]], '''ANCA''': [[Anti-neutrophil cytoplasmic antibody|Anti–neutrophil cytoplasmic antibody]], '''DNA''': [[DNA|Deoxyribonucleic acid]], '''CFTR''': [[Cystic fibrosis transmembrane conductance regulator]], '''SLC10A2''': [[SLC10A2|Solute carrier family 10 member 2]], '''SeHCAT''': [[SeHCAT|Selenium homocholic acid taurine or tauroselcholic acid]], '''IEL''': Intraepithelial [[Lymphocyte|lymphocytes]], '''MRCP''': [[Magnetic resonance cholangiopancreatography]], '''ANA''': [[Antinuclear antibodies]], '''AMA''': [[Anti-mitochondrial antibody]], '''LDH''': [[Lactate dehydrogenase]], '''CPK''': [[Creatine phosphokinase]], '''PCR''': [[Polymerase chain reaction]], '''ELISA''': [[Enzyme linked immunosorbent assay (ELISA)|Enzyme–linked immunosorbent assay]], '''LT''': Heat–labile [[enterotoxin]], ST: Heat–stable [[enterotoxin]], '''RT-PCR''': Reverse–transcriptase [[polymerase chain reaction]], '''CD4:''' [[CD4|Cluster of differentiation 4]], '''HIV''': [[Human Immunodeficiency Virus (HIV)|Human immunodeficiency virus]], '''RUQ''': [[RUQ|Right-upper quadrant]], '''VIP''': [[Vasoactive intestinal peptide]], '''GI:''' [[Gastrointestinal tract|Gastrointestinal]], '''FAP''': [[Familial adenomatous polyposis]], '''HNPCC''': [[Hereditary nonpolyposis colorectal cancer]], '''MTP''': [[Microsomal triglyceride transfer protein]], '''Scl‑70''': Anti–[[Type I topoisomerase|topoisomerase I]], '''TSH''': [[Thyroid-stimulating hormone]], '''T4''': [[Thyroxine]], '''T3''': [[Triiodothyronine]], '''DTR''': [[Deep tendon reflex]], '''RNA''': [[RNA|Ribonucleic acid]]</span>
| | ''Indications for the patient'' |
| | * Fasting period prior to test should be 8-12 h |
| | * Antibiotics should be avoided 4 weeks prior to test |
| | * Prokinetic agents (e.g. cisapride, domperidone, erythromycin) and laxatives should be stopped 1 week prior to test–''if tolerated by the patient'' |
| | * Complex carbohydrates (e.g. bread, pasta, rice, legumes, etc.) should be avoided 24 hours prior to test |
| | * Physical activity should be avoided during the test |
| | * Smoking should be avoided on the day of the test |
| | * It is not necessary to stop proton pump inhibitors for the test |
| | ''Indications for the physician'' |
| | * Lactulose dose: 10 g followed by one cup of water |
| | * Glucose dose: 75 g mixed with or followed by one cup of water |
| | * Lactose: 25 g mixed with one cup of water |
| | * Fructose: 25 g mixed with or followed by one cup of water |
|
| |
|
| {| class="wikitable" style="border: 0px; font-size: 100%; margin: 3px;" align="center"
| | == Treatment == |
| ! colspan="2" rowspan="5" style="background:#4479BA; color: #FFFFFF;" align="center" |Cause
| | Treatment options available for small intestinal bacterial overgrowth syndrome are as follows: <ref name="pmid19243285">{{cite journal |vauthors=Pimentel M |title=Review of rifaximin as treatment for SIBO and IBS |journal=Expert Opin Investig Drugs |volume=18 |issue=3 |pages=349–58 |year=2009 |pmid=19243285 |doi=10.1517/13543780902780175 |url=}}</ref><ref name="pmid437407">{{cite journal |vauthors=King CE, Toskes PP |title=Small intestine bacterial overgrowth |journal=Gastroenterology |volume=76 |issue=5 Pt 1 |pages=1035–55 |year=1979 |pmid=437407 |doi= |url=}}</ref> |
| | colspan="9" style="background:#4479BA; color: #FFFFFF;" align="center" |'''Clinical manifestation''' | | ===Medical Therapy=== |
| ! colspan="9" rowspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |'''Lab findings'''
| | *The mainstay of [[therapy]] for small intestinal bacterial overgrowth (SIBO) is [[antibiotic therapy]].<ref name="pmid28078798">Gatta L, Scarpignato C. Systematic review with meta-analysis: rifaximin is effective and safe for the treatment of small intestine bacterial overgrowth. Aliment Pharmacol Ther. 2017 Mar;45(5):604-616. doi: 10.1111/apt.13928. Epub 2017 Jan 12. PMID: [http://pubmed.gov/28078798 28078798]; PMCID: PMC5299503.</ref> |
| ! rowspan="5" style="background:#4479BA; color: #FFFFFF;" align="center" |Extra intestinal findings
| | *[[Antibiotics]] acts by eliminating the [[bacterial]] [[Overgrowth syndrome|overgrowth]]. |
| ! rowspan="5" style="background:#4479BA; color: #FFFFFF;" align="center" |Cause/Pathogenesis
| | * [[Rifaximin]] is the [[antibiotic]] of choice for the [[Treatments|treatment]] of small intestinal bacterial overgrowth (SIBO). |
| ! rowspan="5" style="background:#4479BA; color: #FFFFFF;" align="center" |Gold standard diagnosis
| | ** Rifaximin may only work in patients who have [[irritable bowel syndrome]]<ref name="pmid25319626">{{cite journal| author=Boltin D, Perets TT, Shporn E, Aizic S, Levy S, Niv Y | display-authors=etal| title=Rifaximin for small intestinal bacterial overgrowth in patients without irritable bowel syndrome. | journal=Ann Clin Microbiol Antimicrob | year= 2014 | volume= 13 | issue= | pages= 49 | pmid=25319626 | doi=10.1186/s12941-014-0049-x | pmc=4201689 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25319626 }} </ref> |
| |-
| | **Preferred regimen: [[Rifaximin]] 550 mg PO q8h for 14 days. |
| ! colspan="8" style="background:#4479BA; color: #FFFFFF;" align="center" |Symptoms
| | *Response to [[antibiotics]] can be assessed by the [[symptomatic]] improvement. In case of recurrent [[symptoms]], the [[antibiotic]] [[dose]] is repeated. |
| ! rowspan="4" style="background:#4479BA; color: #FFFFFF;" align="center" |GI signs
| |
| |-
| |
| ! colspan="2" rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Duration
| |
| ! colspan="3" rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Diarrhea
| |
| ! rowspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |Fever
| |
| ! rowspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |Abdominal pain
| |
| ! rowspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |Weight loss
| |
| |- | |
| ! colspan="5" style="background:#4479BA; color: #FFFFFF;" align="center" |Stool exam
| |
| | colspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |'''CBC''' | |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Other lab findings
| |
| |-
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Acute
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Chronic
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Watery
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Bloody
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Fatty
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |WBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |RBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Ova/Parasite
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Osmotic gap
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Other
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |WBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Hgb
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Plt
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Crohns disease|Crohn's disease]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ±
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Abdominal tenderness]]
| |
| * Oral [[mucosal]] lesions
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↑
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↓
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↑
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Anti saccharomyces cerevisiae antibodies]] (ASCA)
| |
| * [[Vitamin B12]] deficiency
| |
| * Elevated [[erythrocyte sedimentation rate|ESR]]
| |
| * Elevated [[C-reactive protein|CRP]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Uveitis]]
| |
| * [[Arthritis]]
| |
| * [[Erythema nodosum]]
| |
| * [[Pyoderma gangrenosum]]
| |
| * [[Amyloidosis]]
| |
| * Venous and arterial [[thromboembolism]]
| |
| * [[Kidney stone|Renal stones]]
| |
| * [[Bronchiectasis]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * Abnormal immune response to self [[antigens]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Colonoscopy]] with [[biopsy]]
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Ulcerative colitis]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ±
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Abdominal tenderness]]
| |
| * [[Blood]] on [[rectal examination]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↑
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↓
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↑
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Anti-neutrophil cytoplasmic antibody|Anti–neutrophil cytoplasmic antibody]] ([[P-ANCA|P–ANCA]])
| |
| * [[Hypoalbuminemia]]
| |
| * [[Hypokalemia]]
| |
| * [[Hypomagnesemia]]
| |
| * Elevated [[Erythrocyte sedimentation rate|ESR]]
| |
| * Elevated [[C-reactive protein|CRP]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Skin rash]]
| |
| * [[Iritis]]
| |
| * [[Uveitis]]
| |
| * Seronegative [[arthritis]]
| |
| * [[Clubbing]]
| |
| * [[Erythema nodosum]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * Abnormal immune response to self [[antigens]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Colonoscopy]] with [[biopsy]]
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Celiac disease]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ±
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ±
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Abdominal distention]]
| |
| * Increased [[bowel]] sounds
| |
| * Oral [[Mucous membrane|mucosal]] lesions
| |
| * [[Hepatosplenomegaly]]
| |
| * [[Ascites]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * Fat droplets on [[sudan stain]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ↓
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[IgA]] endomysial [[antibody]]
| |
| * Anti–tissue [[transglutaminase]] [[antibody]]
| |
| * [[Anti-gliadin antibodies|Anti–gliadin antibody]]
| |
| * [[Fat soluble vitamins]] deficiency
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Malabsorption]]
| |
| * [[Dementia]]
| |
| * [[Dermatitis herpetiformis]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[HLA-DQ2|HLA–DQ2]]
| |
| * [[HLA-DQ8|HLA–DQ8]]
| |
| * Innate responses to wheat [[Protein|proteins]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[IgA]] endomysial [[antibody]]
| |
| * Anti–tissue [[transglutaminase]] [[antibody]]
| |
| |-
| |
| ! colspan="2" rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Cause
| |
| ! colspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Duration
| |
| ! colspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |Diarrhea
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Fever
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Abdominal pain
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Weight loss
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |GI signs
| |
| ! colspan="5" style="background:#4479BA; color: #FFFFFF;" align="center" |Stool exam
| |
| ! colspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |CBC
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Other lab findings
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Extra intestinal findings
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Cause/Pathogenesis
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Gold standard diagnosis
| |
| |-
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Acute
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Chronic
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Watery
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Bloody
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Fatty
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |WBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |RBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Ova/Parasite
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Osmotic gap
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Other
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |WBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Hgb
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Plt
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Cystic fibrosis]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |±
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Abdominal distension|Abdominal distention]]
| |
| *[[Hepatosplenomegaly]]
| |
| *[[Rectal prolapse]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * Fat droplets on [[sudan stain]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↓
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * Positive [[DNA]] analysis for [[CFTR|cystic fibrosis transmembrane conductance regulator]] [[CFTR|(CFTR)]]
| |
| * Nasal transepithelial potential difference
| |
| * [[Fat soluble vitamins]] deficiency
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Malabsorption]]
| |
| * Recurrent [[respiratory tract infection]]
| |
| * [[Bronchiectasis]]
| |
| * [[Diabetes mellitus]]
| |
| * [[Scoliosis]]
| |
| * [[Infertility]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * Mutations in the [[cystic fibrosis transmembrane conductance regulator]] ([[CFTR]]) protein
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * Positive [[genetic testing]]
| |
| * Elevated [[Sweat chloride test|sweat chloride]] ≥60 mmol/L
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Chronic pancreatitis]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Tenderness (medicine)|Abdominal tenderness]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * Fat droplets on [[sudan stain]]
| |
| * Positive [[fecal elastase]] measurement
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * Slightly elevated [[amylase]] and [[lipase]]
| |
| * Abnormal pancreatic function test
| |
| * [[Secretin]] stimulation test
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Malabsorption]]
| |
| * [[Diabetes mellitus]]
| |
| * [[Pancreatic pseudocyst]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Toxin|Toxins]]
| |
| * Recurrent [[acute pancreatitis]]
| |
| * [[Genetics|Genetic]] predesposition
| |
| * [[Autoimmunity|Autoimmune]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Magnetic resonance cholangiopancreatography]] ([[Magnetic resonance cholangiopancreatography|MRCP]])
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Bile acid malabsorption]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="Left" |
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Fat droplets on [[sudan stain]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Reduced [[cholesterol]] level
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Malabsorption]]
| |
| *[[Hypotension]]
| |
| *[[Tachycardia]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Genetic defects in ''[[SLC10A2]]''
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[SeHCAT]] test
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Microscopic colitis]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Abdominal tenderness]]
| |
| * Fecal [[incontinence]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↓
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Hypokalemia]]
| |
| * Elevated [[C-reactive protein|CRP]]
| |
| * Positive [[autoantibodies]] include:
| |
| **RF
| |
| **[[ANA]]
| |
| **[[Anti-mitochondrial antibody|AMA]]
| |
| **[[ANCA]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Arthritis]]
| |
| * [[Uveitis]]
| |
| * [[Idiopathic thrombocytopenic purpura]]
| |
| * Pleuro [[pericarditis]]
| |
| * [[Hypothyroidism]]
| |
| * [[Psoriasis]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Mucosal]] [[immune responses]] to luminal factors in a genetically predisposed individual
| |
| * Drug–induced
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Colonoscopy]] with [[mucosal]] [[biopsy]] with [[mononuclear]] infiltrates:
| |
| ** [[Collagenous colitis]] is characterized by a colonic subepithelial [[collagen]] band >10 micrometers in diameter
| |
| ** [[Lymphocytic]] [[colitis]] is characterized by ≥20 intraepithelial [[lymphocytes]] (IEL) per 100 surface epithelial cells
| |
| |-
| |
| ! colspan="2" rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Cause
| |
| ! colspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Duration
| |
| ! colspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |Diarrhea
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Fever
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Abdominal pain
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Weight loss
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |GI signs
| |
| ! colspan="5" style="background:#4479BA; color: #FFFFFF;" align="center" |Stool exam
| |
| ! colspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |CBC
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Other lab findings
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Extra intestinal findings
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Cause/Pathogenesis
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Gold standard diagnosis
| |
| |-
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Acute
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Chronic
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Watery
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Bloody
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Fatty
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |WBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |RBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Ova/Parasite
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Osmotic gap
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Other
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |WBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Hgb
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Plt
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Infective colitis]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="Left" |
| |
| *Rebound [[Tenderness (medicine)|abdominal tenderness]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Positive [[stool culture]]
| |
| *Positive fecal calprotectin
| |
| *Positive fecal [[lactoferrin]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↑
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↓
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↑
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Elevated [[C-reactive protein|CRP]]
| |
| *Elevated [[Erythrocyte sedimentation rate|ESR]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Arthritis]]
| |
| * [[Uveitis]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Salmonella|''Salmonella'']]
| |
| *[[Shigella|''Shigella'']]
| |
| *[[Campylobacter|''Campylobacter'']]
| |
| *''[[Escherichia coli|E. coli 0157:H7]]''
| |
| *[[Clostridium difficile|''Clostridium difficile'']]
| |
| *[[Entamoeba histolytica|''Entamoeba histolytica'']]
| |
| *[[Adenoviridae|''Adenovirus'']]
| |
| *[[Cytomegalovirus|''Cytomegalovirus'']]
| |
| *[[Herpes simplex virus|''Herpes simplex virus'']]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Stool culture]]
| |
| *[[Blood culture]]
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Ischemic colitis]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="Left" |
| |
| *Hyperactive then absent [[Stomach rumble|bowel sounds]]
| |
| *[[Tenderness (medicine)|Abdominal tenderness]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↑
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↓
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↑
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Elevated [[C-reactive protein|CRP]]
| |
| *Elevated [[Erythrocyte sedimentation rate|ESR]]
| |
| *Elevated serum [[Lactic acid|lactate]]
| |
| *Elevated [[lactate dehydrogenase]] ([[Lactate dehydrogenase|LDH]])
| |
| *Elevated [[Creatine kinase|creatine phosphokinase]] ([[Creatine kinase|CPK]])
| |
| *Elevated [[amylase]]
| |
| *[[Hypoalbuminemia]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Henoch-Schönlein purpura|IgA vasculitis]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Thrombophilia|Hypercoagulability]]
| |
| *Nonocclusive [[Ischemic colitis|colonic ischemia]]
| |
| *[[Embolism|Embolic]] and [[Thrombosis|thrombotic]] arterial occlusion
| |
| *[[Mesenteric vein thrombosis]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Abdominal [[Computed tomography|CT scan]]
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Lactose intolerance]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Abdominal tenderness ]]
| |
| * [[Abdominal distention]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↑
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * Lactose tolerance test
| |
| * Genetic testing
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Headache]]
| |
| * [[Vertigo]]
| |
| * [[Memory impairment]]
| |
| * [[Lethargy]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * Reduction of lactase enzyme activity or inability to produce persistent [[lactase]]
| |
| * Congenital [[lactase deficiency]]
| |
| * Secondary lactose malabsorption
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Small bowel]] [[biopsy]]
| |
| * Lactose breath hydrogen test
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Irritable bowel syndrome]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |±
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |±
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |±
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Abdominal tenderness]]
| |
| * [[Abdominal distention]]
| |
| * Normal [[Stomach rumble|bowel sounds]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Anxiety]]
| |
| *[[Palpitation]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Unknown
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * Diagnosis of exclusion
| |
| |-
| |
| ! colspan="2" rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Cause
| |
| ! colspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Duration
| |
| ! colspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |Diarrhea
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Fever
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Abdominal pain
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Weight loss
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |GI signs
| |
| ! colspan="5" style="background:#4479BA; color: #FFFFFF;" align="center" |Stool exam
| |
| ! colspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |CBC
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Other lab findings
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Extra intestinal findings
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Cause/Pathogenesis
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Gold standard diagnosis
| |
| |-
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Acute
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Chronic
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Watery
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Bloody
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Fatty
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |WBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |RBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Ova/Parasite
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Osmotic gap
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Other
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |WBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Hgb
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Plt
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Whipple's disease]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ±
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Hepatosplenomegaly]]
| |
| * [[Ascites]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * Positive [[fecal fat]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↓
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↓
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↓/↑
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Hypoalbuminemia]]
| |
| *[[Fat soluble vitamins]] deficiency
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Malabsorption]]
| |
| * [[Ocular motility disorders|Abnormal extraocular movement]]
| |
| * [[Lymphadenopathy]]
| |
| * [[Hyperpigmentation]]
| |
| * [[Uveitis]]
| |
| * [[Endocarditis]]
| |
| * [[Encephalitis]]
| |
| * [[Dementia]]
| |
| * [[Pleural effusion]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Tropheryma whipplei|''Tropheryma whipplei'']]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Small intestine]] [[biopsy]] for [[Tropheryma whipplei]] testing
| |
| * [[PCR]] testing
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Tropical sprue]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * Angular [[stomatitis]]
| |
| * Oral mucosal lesion
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Positive [[stool culture]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ↓
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Fat soluble vitamins]] deficiency
| |
| * [[Vitamin B12 deficiency]]
| |
| * [[Folate deficiency]]
| |
| * [[Hypokalemia]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Myalgia]]
| |
| *[[Neuropathy]]
| |
| *[[Edema]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * ''[[Escherichia coli]]''
| |
| * ''[[Klebsiella pneumoniae]]''
| |
| * ''[[Enterobacter cloacae]]''
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * Diagnosis of exclusion
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Small bowel bacterial overgrowth syndrome|Small bowel bacterial overgrowth]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Abdominal distension|Abdominal distention]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Positive [[stool culture]]
| |
| *Positive [[fecal fat]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↓
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Hypoalbuminemia]]
| |
| * Abnormal [[Hydrogen Breath Test|hydrogen breath test]]
| |
| * [[Lactic acidosis]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Malabsorption]]
| |
| * [[Rosacea]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * Excess bacteria in the [[small intestine]]
| |
| * Alterations in [[Intestine|intestinal]] [[anatomy]] or GI motility
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * Diagnosis of exclusion
| |
| |-
| |
| ! colspan="2" rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Cause
| |
| ! colspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Duration
| |
| ! colspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |Diarrhea
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Fever
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Abdominal pain
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Weight loss
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |GI signs
| |
| ! colspan="5" style="background:#4479BA; color: #FFFFFF;" align="center" |Stool exam
| |
| ! colspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |CBC
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Other lab findings
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Extra intestinal findings
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Cause/Pathogenesis
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Gold standard diagnosis
| |
| |-
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Acute
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Chronic
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Watery
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Bloody
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Fatty
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |WBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |RBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Ova/Parasite
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Osmotic gap
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Other
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |WBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Hgb
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Plt
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Salmonellosis]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="Left" |
| |
| *[[Abdominal distention]]
| |
| *Diffuse [[abdominal tenderness]]
| |
| *[[Hepatosplenomegaly]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Positive [[stool culture]]
| |
| *Positive serologic testing
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↑
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↑
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Hypokalemia]]
| |
| *[[Hypernatremia]]
| |
| *[[Hyponatremia]]
| |
| * [[Hypercalciuria]]
| |
| * [[Hypocitraturia]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Post-infectious arthritis|Post–infectious arthritis]]
| |
| * [[Obtundation]]
| |
| * [[Bacteremia]]
| |
| * [[Pericarditis]]
| |
| * [[Pyelonephritis]]
| |
| *[[Brain abscess]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Salmonella|''Salmonella'']]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Stool culture]]
| |
| |-
| |
| ! rowspan="2" style="background:#DCDCDC;" align="center" |[[Escherichia coli enteritis]]
| |
| | style="background:#DCDCDC;" align="center" |[[EPEC|'''EPEC''']]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="Left" |
| |
| *Diffuse [[abdominal tenderness]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Positive [[stool culture]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↑
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *''[[Enteropathogenic E. coli]]''
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Hybridization probe|DNA probe]] or [[polymerase chain reaction]] ([[Polymerase chain reaction|PCR]]) of the ''EPEC'' adherence factor
| |
| *[[Stool culture]]
| |
| |-
| |
| | style="background:#DCDCDC;" align="center" |[[EAEC|'''EAEC''']]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="Left" |
| |
| *Diffuse [[abdominal tenderness]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Positive [[stool culture]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↑
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↓
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↓
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Chronic infection in [[Immunodeficiency|immunocompromised]] patients
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Escherichia coli enteritis|''Enteroaggregative E. coli'']]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Stool culture]]
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Aeromonas]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="Left" |
| |
| * [[Abdominal distention]]
| |
| * Hyperactive [[Stomach rumble|bowel sounds]]
| |
| * Diffuse [[abdominal tenderness]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Positive [[stool culture]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↑
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Wound [[infection]]
| |
| *[[Bacteremia]]
| |
| *[[Hemolytic-uremic syndrome|Hemolytic uremic syndrome]]
| |
| *[[Meningitis]]
| |
| *[[Ocular]] infection
| |
| *[[Pneumonia]]
| |
| *[[Urinary tract infection]]
| |
| *[[Osteomyelitis]]
| |
| *[[Peritonitis]]
| |
| *[[Acute cholecystitis]]
| |
| *[[Opportunistic infection|Opportunistic infections]] in [[Immunodeficiency|immunocompromised]] patients
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *''[[Aeromonas]]'' virulence factors including [[Endotoxin|endotoxins]], [[Hemolysin|hemolysins]], [[Enterotoxin|enterotoxins]], and adherence factors
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Blood culture]]
| |
| *Wound [[Culture collection|culture]]
| |
| |-
| |
| ! colspan="2" rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Cause
| |
| ! colspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Duration
| |
| ! colspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |Diarrhea
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Fever
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Abdominal pain
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Weight loss
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |GI signs
| |
| ! colspan="5" style="background:#4479BA; color: #FFFFFF;" align="center" |Stool exam
| |
| ! colspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |CBC
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Other lab findings
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Extra intestinal findings
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Cause/Pathogenesis
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Gold standard diagnosis
| |
| |-
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Acute
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Chronic
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Watery
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Bloody
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Fatty
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |WBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |RBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Ova/Parasite
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Osmotic gap
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Other
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |WBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Hgb
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Plt
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Mycobacterium avium complex]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Abdominal distension|Abdominal distention]]
| |
| *[[Hepatosplenomegaly]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↓
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↓
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Elevated [[Liver function tests|liver enzymes]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Opportunistic infection]] in [[Immunodeficiency|immunocompromised]] patients
| |
| *[[Pulmonary]] [[infection]]
| |
| *[[Lymphadenopathy|Adenopathy]]
| |
| *[[Sleep hyperhidrosis|Night sweats]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Mycobacterium avium complex|''Mycobacterium avium complex'']]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Blood culture]]
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[CMV colitis]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |±
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Diffuse [[Tenderness (medicine)|abdominal tenderness]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Viral antigen assay
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↓
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Decreased [[CD4]] level
| |
| *Abnormal [[Liver function tests|liver function test]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Encephalitis]]
| |
| *[[Guillain-Barré syndrome|Guillain–Barré syndrome]]
| |
| *[[Pneumonia]]
| |
| *[[Retinitis]]
| |
| *[[Pericarditis]] and [[myocarditis]]
| |
| *[[Atherosclerosis]]
| |
| *[[Venous thromboembolism|Venous thrombosis]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Cytomegalovirus|''Cytomegalovirus'']]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Quantitative polymerase chain reaction|Quantitative PCR]] tests
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Human Immunodeficiency Virus (HIV)|HIV]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="Left" |
| |
| *[[Abdominal distension|Abdominal distention]]
| |
| *Diffuse [[Tenderness (medicine)|abdominal tenderness]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↓
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↓
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Decreased [[CD4]] level
| |
| *[[Electrolyte disturbance|Electrolyte imbalance]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Lymphadenopathy]]
| |
| *Disseminated [[infection]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Human Immunodeficiency Virus (HIV)|''HIV'']]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *HIV virologic (viral load) test
| |
| *Immunoassay
| |
| |-
| |
| ! colspan="2" rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Cause
| |
| ! colspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Duration
| |
| ! colspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |Diarrhea
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Fever
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Abdominal pain
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Weight loss
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |GI signs
| |
| ! colspan="5" style="background:#4479BA; color: #FFFFFF;" align="center" |Stool exam
| |
| ! colspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |CBC
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Other lab findings
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Extra intestinal findings
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Cause/Pathogenesis
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Gold standard diagnosis
| |
| |-
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Acute
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Chronic
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Watery
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Bloody
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Fatty
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |WBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |RBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Ova/Parasite
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Osmotic gap
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Other
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |WBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Hgb
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Plt
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Entamoeba histolytica]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="Left" |
| |
| *[[Abdominal distension|Abdominal distention]]
| |
| *Diffuse [[Tenderness (medicine)|abdominal tenderness]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↑
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Liver abscess]]
| |
| *Pleuropulmonary infection
| |
| *[[Cardiac]] [[infection]]
| |
| *[[Brain abscess]]
| |
| *[[Skin and soft-tissue infections|Cutaneous infection]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Entamoeba histolytica|''Entamoeba histolytica'']]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Antigen testing
| |
| *Serology
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Giardia lamblia|Giardia]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="Left" |
| |
| *[[Abdominal distension|Abdominal distention]]
| |
| *Diffuse [[Tenderness (medicine)|abdominal tenderness]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Malabsorption]]
| |
| *[[Urticaria]]
| |
| *[[Depression]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *''[[Giardia lamblia]]''
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Antigen detection assays
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Cryptosporidium]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="Left" |
| |
| *[[Abdominal distension|Abdominal distention]]
| |
| *Diffuse [[Tenderness (medicine)|abdominal tenderness]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Positive stool microscopy
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Elevated [[alkaline phosphatase]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Chronic, life–threatening illness in [[Immunodeficiency|immunocompromised]] patients
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Cryptosporidium|''Cryptosporidium'']]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Polymerase chain reaction
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Microsporidia]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="Left" |
| |
| *[[Abdominal distension|Abdominal distention]]
| |
| *Diffuse [[Tenderness (medicine)|abdominal tenderness]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Positive stool microscopy
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Decreased [[CD4]] count
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Malabsorption]]
| |
| *[[Keratitis]]
| |
| *[[Seizure]]
| |
| *[[Myositis]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Microsporidia]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Antigen detection assays
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Isospora]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Abdominal distension|Abdominal distention]]
| |
| *Diffuse [[Tenderness (medicine)|abdominal tenderness]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Positive stool microscopy
| |
| *Positive [[fecal fat]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↑
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Elevated [[Eosinophil granulocyte|eosinophils]]
| |
| *[[Hypokalemia]]
| |
| *Increased [[creatinine]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Chronic illness in [[Immunodeficiency|immunocompromised]] patients
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Isospora|''Isospora'']]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Detecting oocysts in the feces
| |
| |-
| |
| ! colspan="2" rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Cause
| |
| ! colspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Duration
| |
| ! colspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |Diarrhea
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Fever
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Abdominal pain
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Weight loss
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |GI signs
| |
| ! colspan="5" style="background:#4479BA; color: #FFFFFF;" align="center" |Stool exam
| |
| ! colspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |CBC
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Other lab findings
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Extra intestinal findings
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Cause/Pathogenesis
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Gold standard diagnosis
| |
| |-
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Acute
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Chronic
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Watery
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Bloody
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Fatty
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |WBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |RBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Ova/Parasite
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Osmotic gap
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Other
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |WBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Hgb
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Plt
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Carcinoid syndrome|Carcinoid tumor]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="Left" |
| |
| * [[Abdominal distention]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↓
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Elevated urinary [[5-Hydroxyindoleacetic acid|5–hydroxyindoleacetic acid]] ([[5-Hydroxyindoleacetic acid|5–HIAA]]) level
| |
| *High [[chromogranin A]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Flushing|Facial flushing]]
| |
| *[[Jaundice]]
| |
| *[[Edema]]
| |
| *[[Valvular heart disease]]
| |
| *[[Congestive heart failure|Right–sided heart failure]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Well–differentiated [[Neuroendocrine tumors|neuroendocrine tumor]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Blood [[chromogranin A]] level
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[VIPoma]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="Left" |
| |
| * [[Abdominal distention]]
| |
| * Abdominal [[RUQ]] [[tenderness]]
| |
| * [[Nausea]]
| |
| * [[Vomiting]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↓
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Elevated [[VIP]] level
| |
| *[[Hypokalemia]]
| |
| *[[Hypochlorhydria]] or [[achlorhydria]]
| |
| *Low osmotic gap (<50 mOsm/kg)
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Rash]]
| |
| * [[Facial flushing]]
| |
| * [[Dehydration]]
| |
| * [[Lethargy]]
| |
| * [[Muscle weakness]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * Primary secretory tumor
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * Blood [[VIP]] levels
| |
| * Followed by imaging
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Zollinger-Ellison syndrome|Zollinger–Ellison syndrome]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="Left" |
| |
| ** [[Tenderness|Epigastric tenderness]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↓
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↓
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * Positive [[secretin]] stimulation test
| |
| * Elevated serum [[chromogranin A]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| ** [[Jaundice]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Gastrin]] producing [[tumor]] mainly in [[duodenum]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Secretin]] stimulation test
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Neuroendocrine tumors|Somatostatinoma]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="Left" |
| |
| ** [[Tenderness|Epigastric tenderness]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↓
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Elevated fasting plasma [[somatostatin]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| ** [[Diabetes mellitus]]
| |
| ** [[Gallstone disease|Cholelithiasis]]
| |
| ** [[Jaundice]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Neuroendocrine tumors]] of D–cell origin
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Plasma [[somatostatin]] level
| |
| *Followed by imaging
| |
| |-
| |
| ! colspan="2" rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Cause
| |
| ! colspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Duration
| |
| ! colspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |Diarrhea
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Fever
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Abdominal pain
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Weight loss
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |GI signs
| |
| ! colspan="5" style="background:#4479BA; color: #FFFFFF;" align="center" |Stool exam
| |
| ! colspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |CBC
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Other lab findings
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Extra intestinal findings
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Cause/Pathogenesis
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Gold standard diagnosis
| |
| |-
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Acute
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Chronic
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Watery
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Bloody
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Fatty
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |WBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |RBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Ova/Parasite
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Osmotic gap
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Other
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |WBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Hgb
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Plt
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Lymphoma]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="Left" |
| |
| *Diffuse [[Tenderness (medicine)|abdominal tenderness]]
| |
| *[[Hepatosplenomegaly]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↓
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Paraproteinemia]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Malabsorption]]
| |
| * [[Lactose intolerance]]
| |
| * [[Ascites]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Primary [[tumor]] of GI tract
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Colonoscopy]] with [[biopsy]]
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Colorectal cancer]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Diffuse [[Tenderness (medicine)|abdominal tenderness]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↓
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * Positive [[carcinoembryonic antigen]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Metastasis]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[FAP|FAP gene]]
| |
| *[[Hereditary nonpolyposis colorectal cancer|HNPCC gene]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| ** [[Colonoscopy]] and [[biopsy]]
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |Medications
| |
| * [[ACE inhibitor|ACE inhibitors]]
| |
| * [[Digoxin]]
| |
| * [[Cephalosporin|Cephalosporins]]
| |
| * [[Statins]]
| |
| * [[Thiazide|Thiazide diuretics]]
| |
| * [[Triptans]]
| |
| * [[Lactulose]]
| |
| * [[HIV AIDS medical therapy|Anti retroviral agents]]
| |
| * [[Chemotherapy|Chemotherapeutic agents]]
| |
| * [[Antifungal drug|Antifungals]]
| |
| * [[Magnesium]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |±
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |±
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="Left" |
| |
| *[[Abdominal distention]]
| |
| *[[Dehydration]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↑/↓
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↑
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Elevated plasma level of drug
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Inflammation]]
| |
| *[[Pseudomembranous enterocolitis|Pseudomembranous colitis]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Clinical evaluation after discontinuation of the drugs
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |Factitious diarrhea
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="Left" |
| |
| *[[Abdominal distention]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↑/↓
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Hypokalemia]]
| |
| *[[Metabolic alkalosis]]
| |
| *[[Hypermagnesemia]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Malabsorption]]
| |
| *[[Lethargy]]
| |
| *[[Generalized weakness]]
| |
| *[[Acute kidney injury|Acute renal failure]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Medication|Medications]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Clinical evaluation after discontinuation of the drugs
| |
| |-
| |
| ! colspan="2" rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Cause
| |
| ! colspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Duration
| |
| ! colspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |Diarrhea
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Fever
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Abdominal pain
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Weight loss
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |GI signs
| |
| ! colspan="5" style="background:#4479BA; color: #FFFFFF;" align="center" |Stool exam
| |
| ! colspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |CBC
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Other lab findings
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Extra intestinal findings
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Cause/Pathogenesis
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Gold standard diagnosis
| |
| |-
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Acute
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Chronic
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Watery
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Bloody
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Fatty
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |WBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |RBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Ova/Parasite
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Osmotic gap
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Other
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |WBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Hgb
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Plt
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Heavy metal ingestion]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="Left" |
| |
| *[[Abdominal distention]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Elevated plasma heavy metal level
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Headache]]
| |
| *[[Paresthesia|Numbness]]
| |
| *[[Alopecia]]
| |
| *[[Vertigo]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Heavy metal ingestion]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Plasma level of heavy metal
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Organophosphate poisoning]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="Left" |
| |
| *[[Saliva|Salivation]]
| |
| *[[Nausea and vomiting|Vomiting]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Reduced RBC acetylcholinesterase
| |
| *Plasma [[cholinesterase]] activity
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Dysautonomia|Autonomic dysfunction]]
| |
| *Motor deficit
| |
| *Sensory deficit
| |
| *[[Bronchospasm]]
| |
| *[[Urination]]
| |
| *[[Miosis]]
| |
| *[[Bradycardia]]
| |
| *[[Lacrimation]]
| |
| *[[Sweating]]
| |
| *[[Cardiac arrhythmia|Cardiac arrhythmias]]
| |
| *[[Acute kidney injury|Acute renal injury]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Neurotoxin|Neurotoxins]] bind to [[ACHE|acetylcholinesterase]] (AChE)
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Clinical diagnosis
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Opium withdrawal]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="Left" |
| |
| *Hyperactive [[Stomach rumble|bowel sounds]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Azotemia]]
| |
| *[[Hypokalemia]]
| |
| *[[Metabolic alkalosis]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Dysphoria]]
| |
| *[[Agitation (emotion)|Restlessness]]
| |
| *[[Perspiration|Sweating]]
| |
| *[[Rhinorrhea]]
| |
| *[[Tears|Lacrimation]]
| |
| *[[Myalgia]]
| |
| *[[Arthralgia]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Opium|Opium withdrawal]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Clinical diagnosis following [[opium withdrawal]]
| |
| |-
| |
| ! colspan="2" rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Cause
| |
| ! colspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Duration
| |
| ! colspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |Diarrhea
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Fever
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Abdominal pain
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Weight loss
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |GI signs
| |
| ! colspan="5" style="background:#4479BA; color: #FFFFFF;" align="center" |Stool exam
| |
| ! colspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |CBC
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Other lab findings
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Extra intestinal findings
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Cause/Pathogenesis
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Gold standard diagnosis
| |
| |-
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Acute
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Chronic
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Watery
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Bloody
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Fatty
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |WBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |RBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Ova/Parasite
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Osmotic gap
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Other
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |WBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Hgb
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Plt
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Short bowel syndrome]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Abdominal distension|Abdominal distention]]
| |
| * [[Tenderness (medicine)|Abdominal tenderness]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Positive [[fecal fat]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↓
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ↑
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Hypoalbuminemia]]
| |
| * High level of [[Acute phase protein|acute phase reactant]]
| |
| * Abnormal [[liver function tests]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * Prior [[Intestine|intestinal]] surgery
| |
| * [[Malabsorption]]
| |
| * [[Crohn's disease]]
| |
| * [[Cancer|Malignancy]]
| |
| * Peripheral [[edema]]
| |
| * [[Muscle atrophy]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * Surgical [[bowel resection]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Clinical diagnosis following [[bowel resection]]
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Radiation enteropathy|Radiation enteritis]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="Left" |
| |
| * [[Tenderness (medicine)|Abdominal tenderness]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Positive [[fecal fat]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↓
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Vitamin B12 deficiency
| |
| *[[Hypoalbuminemia]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Prior history of [[Cancer|malignancy]] and [[radiation therapy]]
| |
| *[[Malabsorption]]
| |
| *[[Telangiectasia|Telangiectasias]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Radiation therapy|Radiation]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Segmental bowel [[inflammation]] on [[endoscopy]] or [[colonoscopy]]
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Gastric dumping syndrome|Dumping syndrome]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="Left" |
| |
| *Hyperactive [[bowel sound]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Hypoglycemia]]
| |
| * [[Hydrogen Breath Test|Hydrogen breath test]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Malnutrition]]
| |
| *[[Fat soluble vitamins|Fat soluble vitamin]] deficiency
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Post operative complications|Postgastrectomy]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Clinical diagnosis following [[gastrectomy]]
| |
| |-
| |
| ! colspan="2" rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Cause
| |
| ! colspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Duration
| |
| ! colspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |Diarrhea
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Fever
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Abdominal pain
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Weight loss
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |GI signs
| |
| ! colspan="5" style="background:#4479BA; color: #FFFFFF;" align="center" |Stool exam
| |
| ! colspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |CBC
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Other lab findings
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Extra intestinal findings
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Cause/Pathogenesis
| |
| ! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Gold standard diagnosis
| |
| |-
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Acute
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Chronic
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Watery
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Bloody
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Fatty
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |WBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |RBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Ova/Parasite
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Osmotic gap
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Other
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |WBC
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Hgb
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" |Plt
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Abetalipoproteinemia]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Abdominal distension]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * Low [[triglyceride]]
| |
| * Low total [[cholesterol]] levels
| |
| * [[Acanthocytes]]
| |
| * Low [[vitamin E]] levels
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Ataxia]]
| |
| * [[Visual field defect]]
| |
| * [[Dysarthria]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Autosomal recessive]] disorder caused by mutations encoding the [[microsomal triglyceride transfer protein]] (MTP)
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * Clinical findings and low [[triglyceride]] and [[cholesterol]] level
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Hyperthyroidism]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |±
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |–
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Positive [[fecal fat]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * Elevated [[T4]]
| |
| * Elevated [[T3]]
| |
| * Decreased [[TSH]]
| |
| * High serum [[alkaline phosphatase]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * Lump in the neck
| |
| * Lid lag
| |
| * [[Malabsorption]]
| |
| * [[Sweating]]
| |
| * [[Hyperpigmentation]]
| |
| * [[Proptosis]]
| |
| * [[Tremor]]
| |
| * Increased [[Deep tendon reflex|DTR]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[Graves' disease]]
| |
| * [[Hashimoto's thyroiditis]]
| |
| * [[Toxic adenoma]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * [[TSH]]
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Diabetic neuropathy]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="Left" |
| |
| *[[Fecal incontinence]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Positive [[fecal fat]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↓
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Hyperglycemia]]
| |
| *[[Azotemia]]
| |
| *[[Hypokalemia]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Malabsorption]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Unclear
| |
| *Disordered [[motility]]
| |
| *Increased [[Intestine|intestinal]] secretion
| |
| *[[Small intestinal bacterial overgrowth]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Clinical diagnosis in a patient with long lasting [[diabetes mellitus]]
| |
| |-
| |
| ! colspan="2" style="background:#DCDCDC;" align="center" |[[Scleroderma|Systemic sclerosis]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |±
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="Left" |
| |
| *[[Abdominal pain|Epigastric tenderness]]
| |
| *[[Fecal incontinence]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | +
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | –
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Positive [[fecal fat]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" |↓
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Nl
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| * Anti–[[Type I topoisomerase|topoisomerase I]] (Scl‑70) antibodies
| |
| * [[Antinuclear antibodies]] ([[Antinuclear antibodies|ANA]])
| |
| * [[Anti-centromere antibodies|Anti–centromere antibodies]] | |
| * Anti–[[RNA polymerase III]] antibody | |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Malabsorption]]
| |
| *[[Skin changes]]
| |
| *[[Raynaud's phenomenon|Raynaud phenomenon]] | |
| *[[Pulmonary hypertension]]
| |
| *[[Arthritis]]
| |
| *[[Telangiectasia]]
| |
| *[[Chronic renal failure]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *[[Autoimmunity|Autoimmune reaction]]
| |
| | style="padding: 5px 5px; background: #F5F5F5;" align="left" |
| |
| *Clinical diagnosis
| |
| *Followed by serologic tests
| |
| |- }
| |
| |}
| |
|
| |
|
| | === Surgery === |
| | *[[Surgery|Surgical approach]] can only be performed for [[patients]] with [[strictures]], [[fistulae]], and [[Diverticular|diverticula]] or any other structural abnormality resulting in [[obstruction]] and resultant bacterial overgrowth.<ref name="pmid15156063">{{cite journal |vauthors=Hao WL, Lee YK |title=Microflora of the gastrointestinal tract: a review |journal=Methods Mol. Biol. |volume=268 |issue= |pages=491–502 |year=2004 |pmid=15156063 |doi=10.1385/1-59259-766-1:491 |url=}}</ref> |
|
| |
|
| | === Prevention === |
| | *Effective measures for the [[prevention]] of small bowel bacterial overgrowth syndrome include:<ref name="pmid437407">{{cite journal |vauthors=King CE, Toskes PP |title=Small intestine bacterial overgrowth |journal=Gastroenterology |volume=76 |issue=5 Pt 1 |pages=1035–55 |year=1979 |pmid=437407 |doi= |url=}}</ref> |
| | **Avoiding [[medications]] like [[narcotics]] and [[benzodiazepines]] that decrease [[intestinal]] [[motility]]. |
| | **Avoid [[achlorhydria]] in high-risk [[patients]]. |
| | **Consider [[antibiotic]] [[prophylaxis]] for [[patients]] with four or more episodes of recurrent small bowel bacterial overgrowth syndrome within one year. |
|
| |
|
| ==References== | | ==References== |
| <div class="references-small"><references/></div> | | <div class="references-small"><references /></div> |
|
| |
|
| ==External links== | | ==External links== |
| * [http://www.medicinenet.com/irritable_bowel_syndrome/page6.htm IBS and small intestinal bacterial overgrowth (SIBO)] | | * [http://www.medicinenet.com/irritable_bowel_syndrome/page6.htm IBS and small intestinal bacterial overgrowth (SIBO)] |
|
| |
|
| |
|
| |
|
| [[Category:Bacteria]] | | [[Category:Bacteria]] |