Sinus bradycardia: Difference between revisions
Esther Lee (talk | contribs) |
|||
| Line 328: | Line 328: | ||
====EKG Examples==== | ====EKG Examples==== | ||
---- | |||
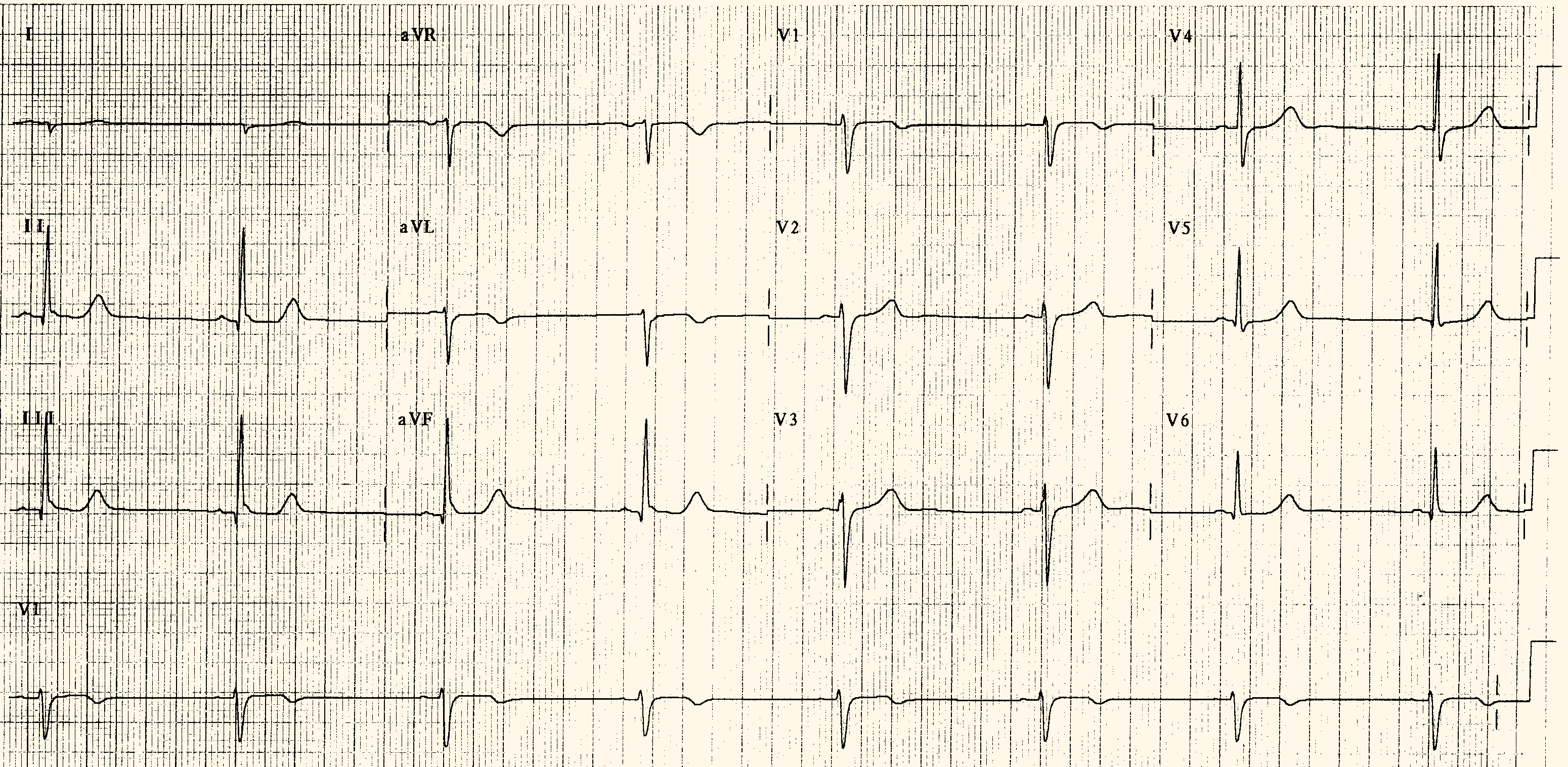
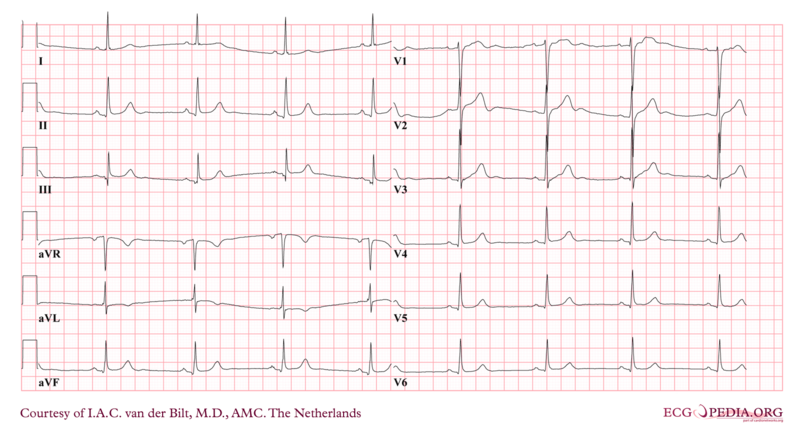
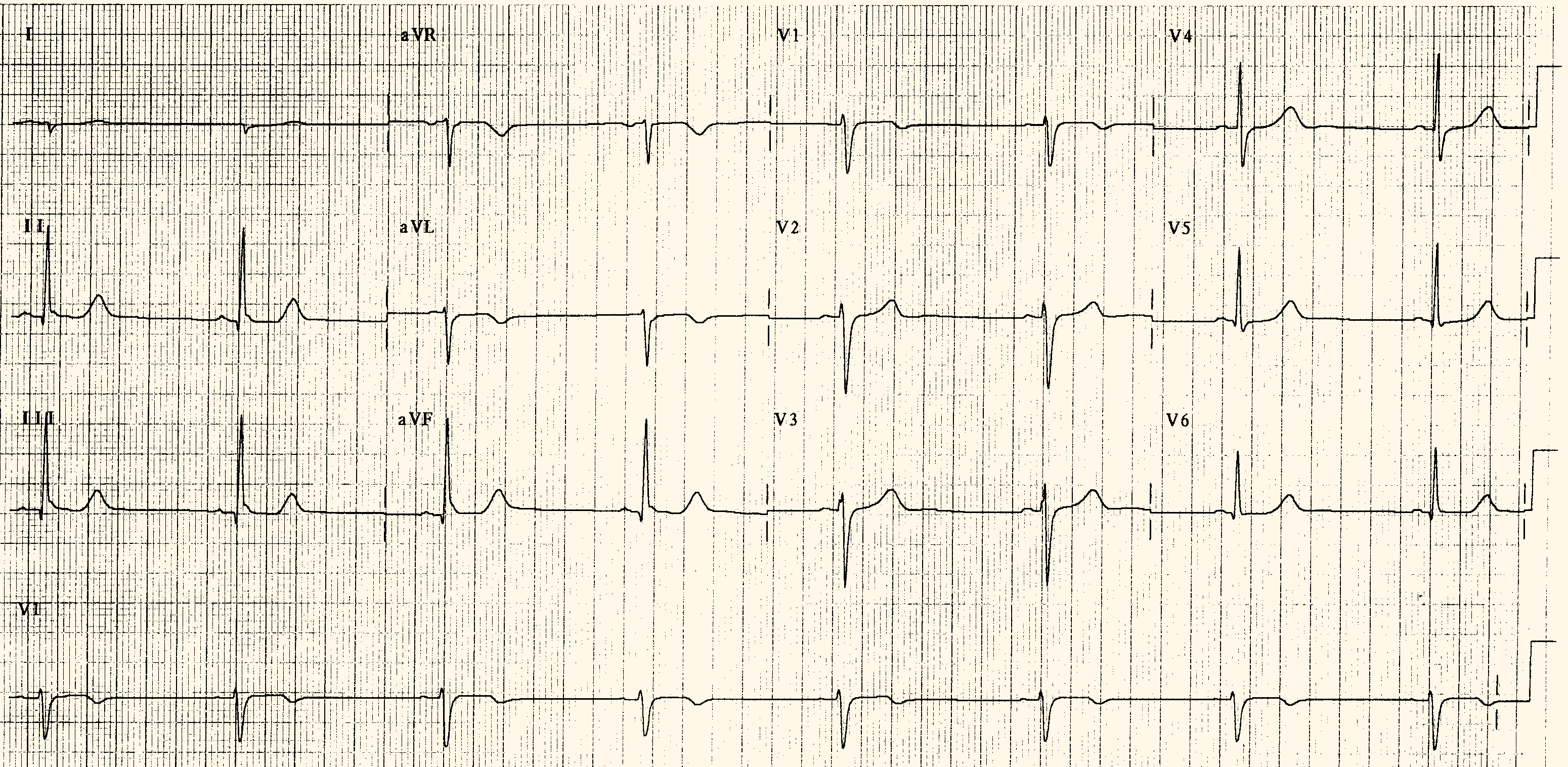
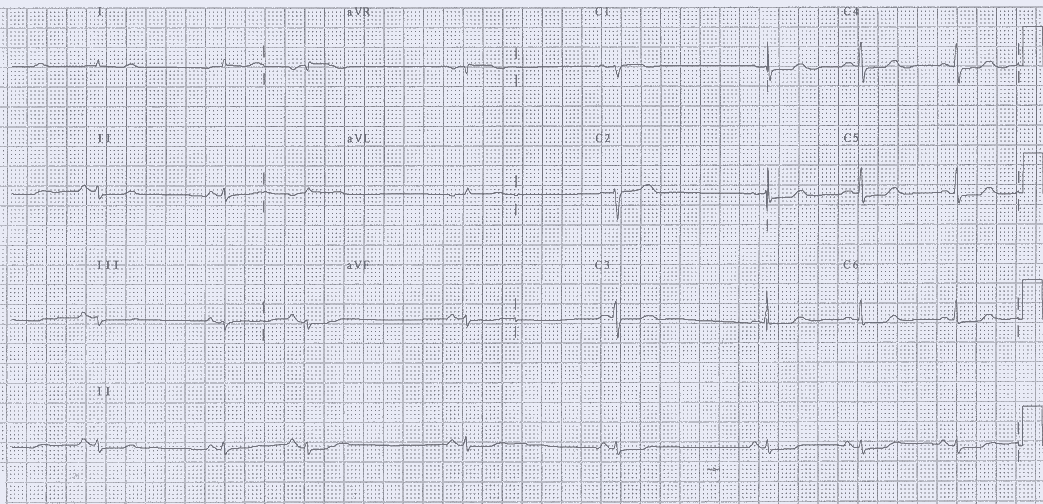
Below ECG images show sinus bradycardia. | Below ECG images show sinus bradycardia. | ||
[[Image:Sinusbradycardia2.png|center|800px]] | [[Image:Sinusbradycardia2.png|center|800px]] | ||
| Line 336: | Line 337: | ||
---- | ---- | ||
[[Image:Ecg_bradycardia 1.png|center|800px]] | [[Image:Ecg_bradycardia 1.png|center|800px]] | ||
==Treatment== | ==Treatment== | ||
Revision as of 15:06, 15 October 2012
| Sinus bradycardia | |
 | |
|---|---|
| Sinus bradycardia. | |
| ICD-9 | 427.81 |
| MeSH | D001146 |
|
WikiDoc Resources for Sinus bradycardia |
|
Articles |
|---|
|
Most recent articles on Sinus bradycardia Most cited articles on Sinus bradycardia |
|
Media |
|
Powerpoint slides on Sinus bradycardia |
|
Evidence Based Medicine |
|
Cochrane Collaboration on Sinus bradycardia |
|
Clinical Trials |
|
Ongoing Trials on Sinus bradycardia at Clinical Trials.gov Trial results on Sinus bradycardia Clinical Trials on Sinus bradycardia at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Sinus bradycardia NICE Guidance on Sinus bradycardia
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Sinus bradycardia Discussion groups on Sinus bradycardia Patient Handouts on Sinus bradycardia Directions to Hospitals Treating Sinus bradycardia Risk calculators and risk factors for Sinus bradycardia
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Sinus bradycardia |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
Sinus bradycardia is a heart rhythm that originates from the sinus node and has a rate of under 60 beats per minute. Common causes include sick sinus syndrome and pharmacotherapy such as beta-blockers. Sinus bradycardia is not unexpected in highly trained athletes. It only requires treatment if the patient is symptomatic.
Pathophysiology
This rhythm may be caused by one of the following:
- Increased vagal tone
- Intrinsic disease of the SA node
- An effect of drugs, such as the use of digitalis or beta-blockers
- Sleep
- Sinus bradycardia is a normal finding in a healthy, well-conditioned athlete
Genetics
The HCN4 genetic variant is associated with sinus bradycardia. Certain sodium channelopathies are associated with sinus bradycardia[1].
Causes
Common Causes
Causes by Organ System
Causes in Alphabetical Order
Epidemiology and Demographics
Among people under 25 years of age, approximately 30% have sinus bradycardia[2]. During sleep, heart rates may decline by 25 beats per minute in young patients, and 15 beats per minutes in the elderly. Heart rates of 30 beats/minute and pauses of up to 2 seconds are not uncommon in healthy people [3][4][5]
Diagnosis
Symptoms
The decreased heart rate can cause a decreased cardiac output resulting in symptoms such as:
Sinus bradycardia may be associated with no symptoms in a young athlete.
Physical Examination
Vitals
- There may be a wide pulse pressure
Skin
If cardiac output is reduced, there may be signs of end organ hypoperfusion such as cold clammy skin
Laboratory Studies
Based upon the patient's history and demographics, the following laboratory studies should be considered:
- Serum electrolytes including Ca, Mg
- TFTs should be checked
- Hypoglycemia should be excluded
- Consider a toxicologic screen
Electrocardiogram
- Rate: Less than 60
- Rhythm: Regular
- P waves: Upright, consistent, and normal in morphology and duration
- PR Interval: Between 0.12-0.21 seconds in duration
- QRS complex: Less than 0.12 seconds in width, and consistent in morphology
- Early repolarization is accentuated in the setting of sinus bradycardia
- Sinus arrhythmia often accompanies sinus brdycardia
EKG Examples
Below ECG images show sinus bradycardia.

Treatment
Acute Management
- If a patient is symptomatic, intravenous access should be established.
- Atropine can be administered down an endotracheal tube or can be administered intravenously. The dose is 0.5-1 mg IV or ET q 3-5 min up to 3 mg total (0.04 mg/kg). The pediatric dosing is 0.02 mg/kg/dose IV, minimum of 0.1 mg. Isoproteronol (Isoprel) has been used in the past, but carries risks.
- Transcutaneous pacing can be undertaken while a temporary wire is being placed.
- Offending or exacerbating agents such as beta-blockers, calcium channel blockers or digitalis should be discontinued and underlying causes treated.
- Sleep apnea is a common cause and should be treated with weight loss and BiPAP.
- Continuous monitoring in the hospital is recommended.
Chronic Management
Asymptomatic sinus bradycardia requires no treatment. Patients with Sick Sinus Syndrome generally require a pacemaker.
ACC/AHA/HRS Guideline Recommendations for Pacemaker Implantation (DO NOT EDIT)[6]
Recommendations for Permanent Pacing in Sinus Node Dysfunction (SND)
| “ |
Class I 1. Permanent pacemaker implantation is indicated for SND with documented symptomatic bradycardia, including frequent sinus pauses that produce symptoms.(Level of Evidence: C) 2. Permanent pacemaker implantation is indicated for symptomatic chronotropic incompetence. (Level of Evidence: C) 3. Permanent pacemaker implantation is indicated for symptomatic sinus bradycardia that results from required drug therapy for medical conditions. (Level of Evidence: C) Class IIa 1. Permanent pacemaker implantation is reasonable for SND with heart rate less than 40 bpm when a clear association between significant symptoms consistent with bradycardia and the actual presence of bradycardia has not been documented. (Level of Evidence:C) 2. Permanent pacemaker implantation is reasonable for syncope of unexplained origin when clinically significant abnormalities of sinus node function are discovered or provoked in electrophysiological studies. (Level of Evidence: C) Class IIb 1. Permanent pacemaker implantation may be considered in minimally symptomatic patients with chronic heart rate less than 40 bpm while awake. (Level of Evidence: C) Class III 1. Permanent pacemaker implantation is not indicated for SND in asymptomatic patients. (Level of Evidence:C) 2. Permanent pacemaker implantation is not indicated for SND in patients for whom the symptoms suggestive of bradycardia have been clearly documented to occur in the absence of bradycardia. (Level of Evidence:C) 3. Permanent pacemaker implantation is not indicated for SND with symptomatic bradycardia due to nonessential drug therapy. (Level of Evidence: C) |
” |
Sources
- Image courtesy of ECGpedia
References
- ↑ Milanesi R, Baruscotti M, Gnecchi-Ruscone T, DiFrancesco D (2006). "Familial sinus bradycardia associated with a mutation in the cardiac pacemaker channel". The New England Journal of Medicine. 354 (2): 151–7. doi:10.1056/NEJMoa052475. PMID 16407510. Retrieved 2011-02-23. Unknown parameter
|month=ignored (help) - ↑ HISS RG, LAMB LE, ALLEN MF (1960). "Electrocardiographic findings in 67,375 asymptomatic subjects. X. Normal values". The American Journal of Cardiology. 6: 200–31. PMID 13855921. Unknown parameter
|month=ignored (help);|access-date=requires|url=(help) - ↑ Hilgard J, Ezri MD, Denes P (1985). "Significance of ventricular pauses of three seconds or more detected on twenty-four-hour Holter recordings". The American Journal of Cardiology. 55 (8): 1005–8. PMID 3984858. Retrieved 2011-02-23. Unknown parameter
|month=ignored (help) - ↑ Brodsky M, Wu D, Denes P, Kanakis C, Rosen KM (1977). "Arrhythmias documented by 24 hour continuous electrocardiographic monitoring in 50 male medical students without apparent heart disease". The American Journal of Cardiology. 39 (3): 390–5. PMID 65912. Unknown parameter
|month=ignored (help);|access-date=requires|url=(help) - ↑ Bjerregaard P (1983). "Mean 24 hour heart rate, minimal heart rate and pauses in healthy subjects 40-79 years of age". European Heart Journal. 4 (1): 44–51. PMID 6339245. Retrieved 2011-02-23. Unknown parameter
|month=ignored (help) - ↑ Epstein AE, Dimarco JP, Ellenbogen KA, Estes NA, Freedman RA, Gettes LS, Gillinov AM, Gregoratos G, Hammill SC, Hayes DL, Hlatky MA, Newby LK, Page RL, Schoenfeld MH, Silka MJ, Stevenson LW, Sweeney MO (2008). "ACC/AHA/HRS 2008 Guidelines for device-based therapy of cardiac rhythm abnormalities". Heart Rhythm : the Official Journal of the Heart Rhythm Society. 5 (6): e1–62. doi:10.1016/j.hrthm.2008.04.014. PMID 18534360. Retrieved 2011-02-23. Unknown parameter
|month=ignored (help)