Shock (circulatory)
| Shock | ||
| ICD-10 | many incl. R57 | |
|---|---|---|
| ICD-9 | 785 | |
| DiseasesDB | 12013 | |
| MedlinePlus | 000039 | |
| eMedicine | emerg/531 med/285 emerg/533 | |
| MeSH | D012769 | |
Circulatory shock, commonly known as just shock, is a serious, life-threatening medical condition where insufficient blood flow reaches the body tissues. As the blood carries oxygen and nutrients around the body, reduced flow hinders the delivery of these components to the tissues, and can stop the tissues from functioning properly.[1] The process of blood entering the tissues is called perfusion, so when perfusion is not occurring properly this is called a hypoperfusional (hypo = below) state.
Circulatory shock should not be confused with the emotional state of shock, as the two are not related. Medical shock is a life-threatening medical emergency and one of the most common causes of death for critically-ill people. Shock can have a variety of effects, all with similar outcomes, but all relate to a problem with the body's circulatory system. For example, shock may lead to hypoxemia (a lack of oxygen in arterial blood) or cardiac arrest (the heart stopping).[2][3][4][5][6][7][8]
Stages of shock
There are four stages of shock. As it is a complex and continuous condition there is no sudden transition from one stage to the next.[9]
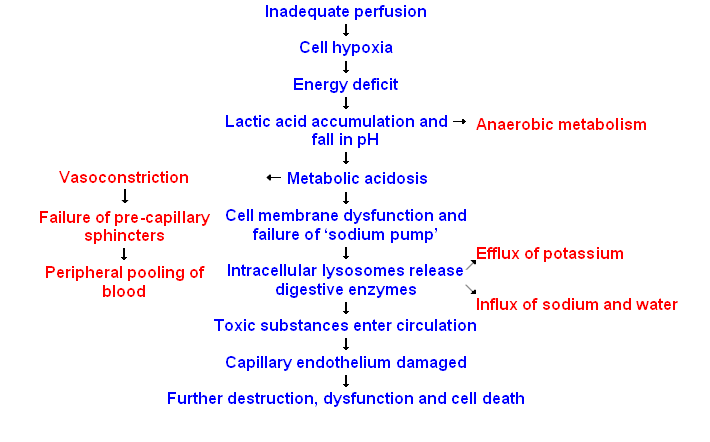
- Initial
- During this stage, the hypoperfusional state causes hypoxia, leading to the mitochondria being unable to produce adenosine triphosphate (ATP). Due to this lack of oxygen, the cell membranes become damaged, they become leaky to extra-cellular fluid, and the cells perform anaerobic respiration. This causes a build-up of lactic and pyruvic acid which results in systemic metabolic acidosis. The process of removing these compounds from the cells by the liver requires oxygen, which is absent.
- Compensatory (Compensating)
- This stage is characterised by the body employing physiological mechanisms, including neural, hormonal and bio-chemical mechanisms in an attempt to reverse the condition. As a result of the acidosis, the person will begin to hyperventilate in order to rid the body of carbon dioxide (CO2). CO2 indirectly acts to acidify the blood and by removing it the body is attempting to raise the pH of the blood. The baroreceptors in the arteries detect the resulting hypotension, and cause the release of adrenaline and noradrenaline. Noradrenaline causes predominately vasoconstriction with a mild increase in heart rate, whereas adrenaline predominately causes an increase in heart rate with a small effect on the vascular tone; the combined effect results in an increase in blood pressure. Renin-angiotensin axis is activated and arginine vasopressin is released to conserve fluid via the kidneys. Also, these hormones cause the vasoconstriction of the kidneys, gastrointestinal tract, and other organs to divert blood to the heart, lungs and brain. The lack of blood to the renal system causes the characteristic low urine production. However the effects of the Renin-angiotensin axis take time and are of little importance to the immediate homeostatic mediation of shock .
- Progressive (Decompensating)
- Should the cause of the crisis not be successfully treated, the shock will proceed to the progressive stage and the compensatory mechanisms begin to fail. Due to the decreased perfusion of the cells, sodium ions build up within while potassium ions leak out. As anaerobic metabolism continues, increasing the body's metabolic acidosis, the arteriolar smooth muscle and precapillary sphincters relax such that blood remains in the capillaries[1]. Due to this, the hydrostatic pressure will increase and, combined with histamine release, this will lead to leakage of fluid and protein into the surrounding tissues. As this fluid is lost, the blood concentration and viscosity increase, causing sludging of the micro-circulation. The prolonged vasoconstriction will also cause the vital organs to be compromised due to reduced perfusion[1]. If the bowel becomes sufficiently ischemic, bacteria may enter the blood stream, resulting the increased complication of endotoxic shock[1].
- Refractory (Irreversible)
- At this stage, the vital organs have failed and the shock can no longer be reversed. Brain damage and cell death have occurred. Death will occur imminently.
Types of shock
In 1972 Hinshaw and Cox suggested the following classification which is still used today.[2] It uses four types of shock: hypovolemic, cardiogenic, distributive and obstructive shock:[3][4][5][8][10]
- Hypovolemic shock - This is the most common type of shock and based on insufficient circulating volume. Its primary cause is loss of fluid from the circulation from either an internal or external source. An internal source may be haemorrhage. External causes may include extensive bleeding, high output fistulae or severe burns.
- Cardiogenic shock - This type of shock is caused by the failure of the heart to pump effectively. This can be due to damage to the heart muscle, most often from a large myocardial infarction. Other causes of cardiogenic shock include arrhythmias, cardiomyopathy, congestive heart failure (CHF), contusio cordis or cardiac valve problems.
- Distributive shock - As in hypovolaemic shock there is an insufficient intravascular volume of blood. This form of "relative" hypovolaemia is the result of dilation of blood vessels which diminishes systemic vascular resistance. Examples of this form of shock are:
- Septic shock - This is caused by an overwhelming infection leading to vasodilation, such as by Gram negative bacteria i.e. Escherichia coli, Proteus species, Klebsiella pneumoniae which release an endotoxin which produces adverse biochemical, immunological and occasionally neurological effects which are harmful to the body. Gram-positive cocci, such as pneumococci and streptococci, and certain fungi as well as Gram-positive bacterial toxins produce a similar syndrome.
- Anaphylactic shock - Caused by a severe anaphylactic reaction to an allergen, antigen, drug or foreign protein causing the release of histamine which causes widespread vasodilation, leading to hypotension and increased capillary permeability.
- Neurogenic shock - Neurogenic shock is the rarest form of shock. It is caused by trauma to the spinal cord resulting in the sudden loss of autonomic and motor reflexes below the injury level. Without stimulation by sympathetic nervous system the vessel walls relax uncontrolled, resulting in a sudden decrease in peripheral vascular resistance, leading to vasodilation and hypotension.
- Obstructive shock - In this situation the flow of blood is obstructed which impedes circulation and can result in circulatory arrest. Several conditions result in this form of shock.
- Cardiac tamponade in which fluid in the pericardium prevents inflow of blood into the heart (venous return). Constrictive pericarditis, in which the pericardium shrinks and hardens, is similar in presentation.
- Tension pneumothorax. Through increased intrathoracic pressure, bloodflow to the heart is prevented (venous return).
- Massive pulmonary embolism is the result of a thromboembolic incident in the bloodvessels of the lungs and hinders the return of blood to the heart.
- Aortic stenosis hinders circulation by obstructing the ventricular outflow tract
Recently a fifth form of shock has been introduced:[2]
- Endocrine shock based on endocrine disturbances.
- Hypothyroidism, in critically ill patients, reduces cardiac output and can lead to hypotension and respiratory insufficiency.
- Thyrotoxicosis may induce a reversible cardiomyopathy.
- Acute adrenal insufficiency is frequently the result of discontinuing corticosteroid treatment without tapering the dosage. However, surgery and intercurrent disease in patients on corticosteroid therapy without adjusting the dosage to accommodate for increased requirements may also result in this condition.
- Relative adrenal insufficiency in critically ill patients where present hormone levels are insufficient to meet the higher demands
Signs and symptoms
- Hypovolemic shock
- Anxiety, restlessness, altered mental state due to decreased cerebral perfusion and subsequent hypoxia.
- Hypotension due to decrease in circulatory volume.
- A rapid, weak, thready pulse due to decreased blood flow combined with tachycardia.
- Cool, clammy skin due to vasoconstriction and stimulation of vasoconstriction.
- Rapid and shallow respirations due to sympathetic nervous system stimulation and acidosis.
- Hypothermia due to decreased perfusion and evaporation of sweat.
- Thirst and dry mouth, due to fluid depletion.
- Fatigue due to inadequate oxygenation.
- Cold and mottled skin (cutis marmorata), especially extremities, due to insufficient perfusion of the skin.
- Distracted look in the eyes or staring into space, often with pupils dilated.
- Cardiogenic shock, similar to hypovolaemic shock but in addition:
- Distended jugular veins due to increased jugular venous pressure.
- Absent pulse due to tachyarrhythmia.
- Obstructive shock, similar to hypovolaemic shock but in addition:
- Distended jugular veins due to increased jugular venous pressure.
- Pulsus paradoxus in case of tamponade
- Septic shock, similar to hypovolaemic shock except in the first stages:
- Pyrexia (fever), due to increased level of cytokines[1].
- Systemic vasodilation resulting in hypotension (low blood pressure)[1].
- Systemic leukocyte adhesion to endothelial tissue[1].
- Reduced contractility of the heart[1].
- Diffuse capillary damage in the lung[1].
- Activation of the coagulation pathways, resulting in disseminated intravascular coagulation[1].
- Increased levels of neutrophils[1].
- Neurogenic shock, similar to hypovolemic shock except in the skin's characteristics. In neurogenic shock, the skin is warm and dry.
- Anaphylactic shock
- Skin eruptions and large welts.
- Localised edema, especially around the face.
- Weak and rapid pulse.
- Breathlessness and cough due to narrowing of airways and swelling of the throat.
Treatment

In the early stages, shock requires immediate intervention to preserve life. Therefore, the early recognition and treatment depends on the transfer to a hospital.
The management of shock requires immediate intervention, even before a diagnosis is made. Re-establishing perfusion to the organs is the primary goal through restoring and maintaining the blood circulating volume ensuring oxygenation and blood pressure are adequate, achieving and maintaining effective cardiac function, and preventing complications. Patients attending with the symptoms of shock will have, regardless of the type of shock, their airway managed and oxygen therapy initiated. In case of respiratory insufficiency (i.e. diminished levels of consciousness, hyperventilation due to acid-base disturbances or pneumonia) intubation and mechanical ventilation may be necessary. A paramedic may intubate in emergencies outside the hospital, whereas a patient with respiratory insufficiency in-hospital will be intubated usually by a respiratory therapist, paramedic, or physician.
The aim of these acts is to ensure survival during the transportation to the hospital; they do not cure the cause of the shock. Specific treatment depends on the cause.
A compromise must be found between:
- raising the blood pressure to be able to transport "safely" (when the blood pressure is too low, any motion can lower the heart and brain perfusion, and thus cause death);
- respecting the golden hour. If surgery is required, it should be performed within the first hour to maximise the patient's chance of survival.
Hypovolemic shock
In hypovolemic shock, caused by bleeding, it is necessary to immediately control the bleeding and restore the casualty's blood volume by giving infusions of isotonic crystalloid solutions. Blood transfusions, packed red blood cells (RBCs), Albumin (or other colloid solutions), or fresh-frozen plasma are necessary for loss of large amounts of blood (e.g. greater than 20% of blood volume), but can be avoided in smaller and slower losses. Hypovolemia due to burns, diarrhea, vomiting, etc. is treated with infusions of electrolyte solutions that balance the nature of the fluid lost. Sodium is essential to keep the fluid infused in the extracellular and intravascular space whilst preventing water intoxication and brain swelling. Metabolic acidosis (mainly due to lactic acid) accumulates as a result of poor delivery of oxygen to the tissues, and mirrors the severity of the shock. It is best treated by rapidly restoring intravascular volume and perfusion as above. Inotropic and vasoconstrictive drugs should be avoided, as they may interfere in knowing blood volume has returned to normal.[2][3][4][5]
Regardless of the cause, the restoration of the circulating volume is priority. As soon as the airway is maintained and oxygen administered the next step is to commence replacement of fluids via the intravenous route.
Opinion varies on the type of fluid used in shock. The most common are:
- Crystalloids - Such as sodium chloride (0.9%), or Lactated Ringer's. Dextrose solutions which contain free water are less effective at re-establishing circulating volume, and promote hyperglycaemia.
- Colloids - For example, polysaccharide (Dextran), polygeline (Haemaccel), succunylated gelatin (Gelofusine) and hetastarch (Hepsan). Colloids are, in general, much more expensive than crystalloid solutions and have not conclusively been shown to be of any benefit in the initial treatment of shock.
- Combination - Some clinicians argue that individually, colloids and crystalloids can further exacerbate the problem and suggest the combination of crystalloid and colloid solutions.
- Blood - Essential in severe hemorrhagic shock, often pre-warmed and rapidly infused.
It is to be noted that NO plain water should be given to the patient at any point, as the patient's low electrolyte levels would easily cause water intoxication, leading to premature death. An isotonic or solution high in electrolytes should be administered if intravenous delivery of recommended fluids is unavailable.
Vasoconstrictor agents have no role in the initial treatment of hemorrhagic shock, due to their relative inefficacy in the setting of acidosis, and because the body, in the setting of hemorrhagic shock, is in an endogenously catecholaminergic state. Definitive care and control of the hemorrhage is absolutely necessary, and should not be delayed.
Cardiogenic shock
In cardiogenic shock, depending on the type of myocardal infarction, one can infuse fluids or in shock refractory to infusing fluids,Template:Clarifyme inotropic agents. Inotropic agents, which enhance the heart's pumping capabilities, are used to improve the contractility and correct the hypotension. Should that not suffice, an intra-aortic balloon pump can be considered (which reduces the workload for the heart and improves perfusion of the coronary arteries) or a left ventricular assist device (which augments the pump-function of the heart.)[2][3][4][5]
The main goals of the treatment of cardiogenic shock are the re-establishment of circulation to the myocardium, minimising heart muscle damage and improving the heart's effectiveness as a pump. This is most often performed by percutaneous coronary intervention and insertion of a stent in the culprit coronary lesion or sometimes by cardiac bypass.
Although this is a protection reaction, the shock itself will induce problems; the circulatory system being less efficient, the body gets "exhausted" and finally, the blood circulation and the breathing slow down and finally stop (cardiac arrest). The main way to avoid this deadly consequence is to make the blood pressure rise again with
- fluid replacement with intravenous infusions;
- use of vasopressing drugs (e.g. to induce vasoconstriction);
- use of anti-shock trousers that compress the legs and concentrate the blood in the vital organs (lungs, heart, brain).
- use of blankets to keep the patient warm - metallic PET film emergency blankets are used to reflect the patient's body heat back to the patient.
Distributive shock
In distributive shock caused by sepsis the infection is treated with antibiotics and supportive care is given (i.e. inotropica, mechanical ventilation, renal function replacement). Anaphylaxis is treated with adrenaline to stimulate cardiac performance and corticosteroids to reduce the inflammatory response. In neurogenic shock because of vasodilation in the legs, one of the most suggested treatments is placing the patient in the Trendelenburg position, thereby elevating the legs and shunting blood back from the periphery to the body's core. However, since bloodvessels are highly compliant, and expand as result of the increased volume locally, this technique does not work. More suitable would be the use of vasopressors.[2][3][4][5]
Obstructive shock
In obstructive shock, the only therapy consists of removing the obstruction. Pneumothorax or haemothorax is treated by inserting a chest tube, pulmonary embolism requires thrombolysis (to reduce the size of the clot), or embolectomy (removal of the thrombus), tamponade is treated by draining fluid from the pericardial space through pericardiocentesis.[2][3][4][5]
Endocrine shock
In endocrine shock the hormone disturbances are corrected. Hypothyroidism requires supplementation by means of levothyroxine, in hyperthyroidism the production of hormone by the thyroid is inhibited through thyreostatica, i.e. methimazole (Tapazole) or PTU (propylthiouracil). Adrenal insufficiency is treated by supplementing corticosteroids. [2]
Prognosis
The prognosis of shock depends on the underlying cause and the nature and extent of concurrent problems. Hypovolemic, anaphylactic and neurogenic shock are readily treatable and respond well to medical therapy. Septic shock however, is a grave condition and with a mortality rate between 30% and 50%. The prognosis of cardiogenic shock is even worse. [2]
Shock is said to evolve from reversible to irreversible in experimental hemorrhagic shock involving certain animal species (dogs, rats, mice) that develop intense vasoconstriction of the gut. Death is due to hemorrhagic necrosis of the intestinal lining when shed blood in reinfused. In pigs and humans 1) this is not seen and cessation of bleeding and restoration of blood volume is usually very effective; however 2) prolonged hypovolemia and hypotension does carry a risk of respiratory and then cardiac arrest. Perfusion of the brain may be the greatest danger during shock. Therefore urgent treatment (cessation of bleeding, rapid restoration of circulating blood volume and ready respiratory support) is essential for a good prognosis in hypovolemic shock.
See also
- Acute respiratory distress syndrome (ARDS)
- Anaesthesia Trauma and Critical Care (ATACC)[1]
- Military Anti-Shock Trousers
- Physical trauma
- Sepsis
- Stress (medicine)
- Systemic inflammatory response syndrome (SIRS)
Notes
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; & Mitchell, Richard N. (2007). Robbins Basic Pathology (8th ed.). Saunders Elsevier. pp. 102-103 ISBN 978-1-4160-2973-1
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 Irwin, Richard S. (2003). Intensive Care Medicine. Lippincott Williams & Wilkins, Philadelphia & London. ISBN 0-7817-3548-3. Unknown parameter
|coauthors=ignored (help); Unknown parameter|month=ignored (help); External link in|title=(help) - ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Marino, Paul L. (2006). The ICU Book. Lippincott Williams & Wilkins, Philadelphia & London. ISBN 0-7817-4802-X. Unknown parameter
|month=ignored (help); External link in|title=(help) - ↑ 4.0 4.1 4.2 4.3 4.4 4.5 "Fundamental Critical Care Support, A standardized curriculum of Critical Care". Society of Critical Care Medicine, Des Plaines, Illinois.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 Harrison's Principles of Internal Medicine.
- ↑ "Cecil Textbook of Medicine".
- ↑ The Oxford Textbook of Medicine.
- ↑ 8.0 8.1 Shock: An Overview PDF by Michael L. Cheatham, MD, Ernest F.J. Block, MD, Howard G. Smith, MD, John T. Promes, MD, Surgical Critical Care Service, Department of Surgical Education, Orlando Regional Medical Center Orlando, Florida
- ↑ Armstrong, D.J. (2004). Shock. In: Alexander, M.F., Fawcett, J.N., Runciman, P.J. Nursing Practice. Hospital and Home. The Adult.(2nd edition): Edinburgh: Churchill Livingstone.
- ↑
Joynt, Gavin (April 2003). "Introduction to management of shock for junior ICU trainees and medical students". The Chinese University of Hong Kong. Unknown parameter
|accessyear=ignored (|access-date=suggested) (help); Unknown parameter|accessmonthday=ignored (help)
References
- Armstrong, D.J. (2004) "Shock". In: Alexander, M.F., Fawcett, J.N., Runciman, P.J. Nursing Practice. Hospital and Home. The Adult.(2nd edition). Edinburgh: Churchill Livingstone.
- Collins, T. (2000) "Understanding Shock". Nursing Standard. Vol. 14(49), pp. 35-41.
- Cuthbertson, B.H. and Webster, N.R. (1995) "Nitric oxide in critical care medicine". British Journal of Hospital Medicine. Vol. 54(11), pp. 579-582.
- Hand, H. (2001) "Shock". Nursing Standard. Vol. 15(48), pp. 45-55.
- Hobler, K, Napadono,R, "Tolerance of Swine to Acute Blood Volume Deficits", Journal of Trauma, 1974, August 14 (8):716-8.
- Irwin, R.S. and Rippe, J.M. (2003) Irwin and Rippe's Intensive Care Medicine (5th edition). Boston: Lippincott, Williams and Wilkins
- Irwin, R.S., Rippe, J.M., Curley, F.J., Heard, S.O. (1997) Procedures and Techniques in Intensive Care Medicine (3rd edition). Boston: Lippincott, Williams and Wilkins.
- Ledingham, I.M. and Ramsey, G. (1986) "Shock". British Journal of Anaesthesia Vol. 58, pp. 169-189.
- Marino, P. (1997) The ICU Book. (2nd edition). Philadelphia: Lippincott, Williams and Wilkins.
- Porth, C.M. (2005) Pathophysiology: Concepts of Altered Health States. (7th edition). Philadelphia: Lippincott, Williams and Wilkins
- Sheppard, M. (2005) Principles and practice of high dependency nursing. Edinburgh: Bailliere Tindall.
- Society of Critical Care Medicine. Fundamental Critical Care Support, A standardized curriculum of critical care. SSCM Illinois, 2001.
- Tortora, G.J. (2005) Principles of anatomy and physiology New Jersey: John Wiley, Inc
Template:General symptoms and signs
ar:صدمة (طب) bs:Šok (medicina) bg:Шок cs:Šok (lékařství) da:Shock de:Schock (Medizin) et:Šokk el:Καταπληξία gl:Shock id:Shock it:Shock he:הלם lt:Šokas mk:Шок nl:Shock no:Sjokk sah:Шок sq:Gjendja e shokut simple:Shock sr:Шок fi:Sokki sv:Cirkulationssvikt ta:அதிர்ச்சி