Perianal abscess: Difference between revisions
m (Changes made per Mahshid's request) |
m (Bot: Removing from Primary care) |
||
| Line 379: | Line 379: | ||
==References== | ==References== | ||
{{Reflist|2}}[[Category:Disease | {{Reflist|2}} | ||
[[Category:Disease]] | |||
[[Category:Up-To-Date]] | [[Category:Up-To-Date]] | ||
[[Category:Surgery]] | [[Category:Surgery]] | ||
[[Category:Gastroenterology]] | [[Category:Gastroenterology]] | ||
Latest revision as of 23:38, 29 July 2020
|
WikiDoc Resources for Perianal abscess |
|
Articles |
|---|
|
Most recent articles on Perianal abscess Most cited articles on Perianal abscess |
|
Media |
|
Powerpoint slides on Perianal abscess |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Perianal abscess at Clinical Trials.gov Trial results on Perianal abscess Clinical Trials on Perianal abscess at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Perianal abscess NICE Guidance on Perianal abscess
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Perianal abscess Discussion groups on Perianal abscess Patient Handouts on Perianal abscess Directions to Hospitals Treating Perianal abscess Risk calculators and risk factors for Perianal abscess
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Perianal abscess |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Aravind Kuchkuntla, M.B.B.S[2]
Synonyms and keywords: Anorectal abscess, Ischiorectal abscess, Supralevator abscess, Horse shoe abscess
To return to abscess main page, click here.
Overview
Anorectal abscess is secondary to blockade of the anal gland ducts, resulting in a infection of the gland. The anatomical position of the anal glands in relation to the anal canal is responsible for the variation in the location of the abscess. Initial infection occurs in the anal gland duct and it takes the path of least resistance. The anorectal abscess are classified into low abscess and high based on the location of the abscess. Patients with low abscess present with anal pain associated with bowel movement, and patients with high abscess present systemic manifestations such as fever and malaise in addition to anal pain. On examination tenderness and flactulance suggest anorectal abscess. It is an emergency condition and must be treated promptly within 24 hours of presentation as spread of infection can result in perineal cellulitis and sepsis. Incision and drainage is the definitive treatment and should be performed under local or general anesthesia based on the location of the abscess. With treatment prognosis is good but a risk of recurrence and formation of a fistula is high in patients with improper drainage and failure to identify existing fistula. Antibiotic therapy does not help with treatment of the infection and wound healing.
Historical Perspective
- In 1880, Herman and Desfosses described the anal glands within the internal sphincter, sub-mucosa and their opening into the anal crypts and demonstrated that the infection of these glands and the spread of the infection through the intersphincteric space can result in the formation of a anorectal abscess.[1]
- Tucker and Hellwig, provided evidence that the initial infection occurs in the anal ducts allowing the infection to spread from the anal lumen into the anal canal wall.[1]
- In 1950, Goligher described the treatment for anorectal abscess with incision and curettage with antibiotic bath and primary closure.[1]
Classification
Based on the location of the abscess in relation to the anal canal and the spread of infection to the surrounding structures, anorectal abscess can be classified into [2][3]
- Perianal abscess: When the infection reaches the anal verge passing between the internal sphincter and external sphincter, it results in the formation of a perianal abscess.
- Ischiorectal abscess: If the infection ruptures through the external sphincter it results in a formation of a ischiorectal abscess.
- Supralevator abscess: If the infection extends superiorly, it can form a supralevator abscess.
- Horseshoe abscess: Extension of the abscess to both the ischiorectal fossa results in the formation of a horseshoe abscess.
Based on the location the abscesses can also be classified into:[4]
- High anorectal abscess: These include intersphincteric, perianal, and ischiorectal abscesses.
- Low anorectal abscess: These incude submucosal, supralevator abscesses.
Pathophysiology
Pathogenesis
- Anal canal is a 2 to 4cm in length, starts at the anorectal junction to the end of anal verge.[5]
- It is divided into a upper and a lower part by transition zone that is seen at the dentate line or pectinate line which is surrounded by longitudinal mucosal folds, called columns of morgagni.[5]
- Each of this fold contains anal crypts, each of which contains 3 to 12 anal glands, the distribution of these glands is not uniform with most of the glands present anterior to the position of the anal canal and fewer in the posterior position.[5]
- The initial infection occurs in the ducts of the anal glands and the spread of infection results in the formation of the abscess, various theories were put forward to describe the pathogenesis and the most accepted one is the cryptoglandular theory.[6]
- The crytoglandular theory states that obstruction of anal gland duct results in a infection and due to the presence of these glands deep in relation to the anal canal and sphincter, the infection follows the path of least resistance resulting in abscess formation at the termination of the gland.[7][8]
Causes
Source of Infection
- Supralevator abscess can be caused by the spread of infection from abdominal infections such as appendicitis, diverticulitis, or gynecologic sepsis.
- Spread of infection of ano-rectal Crohn's disease.
- Trauma to the anal canal
- Cancer of the anal canal or the anal glands
Microbial Causes
Organisms commonly causing anorectal abscess include:
Epidemiology and Demographics
Incidence
- The incidence of anorectal abscess is estimated to be around 68,000 to 96,000 cases per year in the United States.[1]
Gender
- Anorectal abscesses are two times more frequently seen in men than women.[10]
Age
- Patients with anorectal abscess present between ages of 20 to 60 years with a mean age of 40 in both sexes.[1]
Race
- There are limited epidemiological studies which studied the frequency of anorectal abscess with race differences, however a study in Chicago reported a 92% of the patients presented with anorectal abscess were of African-American origin.[11]
Risk Factors
Risk factors for the development of recurrent of anal abscesses include[12]:
- Crohn's disease
- Diabetes mellitus
- History of abscess in the ischiorectal location
- HIV infection[13]
- Receptive anal sex
Differential Diagnosis
Anorectal abscess must be differentiated from other causes of anal pain including anal fissure, thrombosed hemorrhoids, levator spasm, sexually transmitted disease, proctitis, hidradenitis suppurativa, infected skin furuncles, herpes simplex virus, tuberculosis, syphilis, actinomycosis and cancer.[14]
| Disease | Definition | Causes | Clinical Features | Diagnosis |
|---|---|---|---|---|
| Fistula in ano |
|
|
| |
| Anal Fissure |
|
|
|
|
| Thrombosed External Hemorrhoids |
|
|
|
|
| Levator spasm |
|
|
|
|
| Proctatitis |
|
|
||
| Hidradenitis suppurativa |
|
|
||
| Infected skin furuncle |
|
| ||
| Bartholin's abscess |
|
|
|
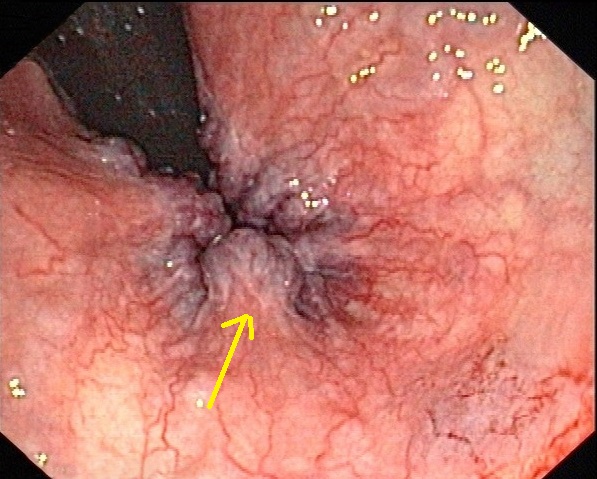
Perianal absscess must be differentiated from other diseases that cause anal discomfort and pain with defecation such as hemorrhoids, anal fissure and anal cancer.
| Disease | History | Physical exam findings | Sample image |
|---|---|---|---|
| Hemorrhoids |
External hemorrhoids
Internal hemorrhoids
|
Skin examination
Digital rectal examination
|
 |
| Anal fissure |
|
|
 |
| Rectal prolapse |
|
|
 |
| Perianal abscess |
|
|
|
| Anal cancer |
|
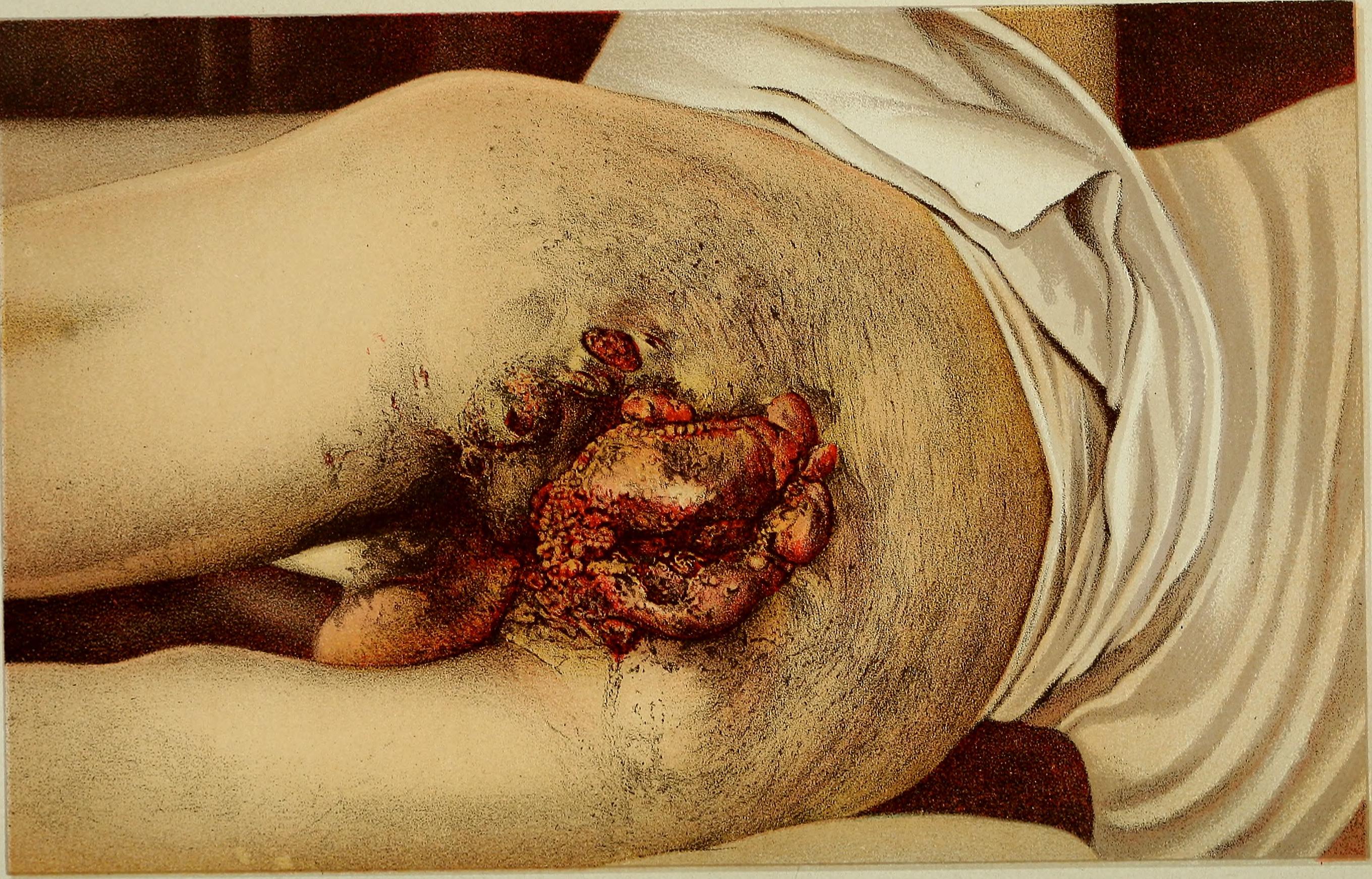 | |
| Condylomata acuminata |
|
|
Natural History, Prognosis, Complications
Natural History
If left untreated, anorectal abscess can spread to the surrounding tissue and can cause perineal cellulitis and sepsis. Perianal abscess is the most common type followed by ischiorectal abscess.[11]
Prognosis
Prognosis of patients is good with incision and drainage and most patients do not require any antibiotic therapy after the procedure, except for patients with HIV infection, Crohn's disease. Majority of patients have relief of pain after abscess drainage and healing takes time as it heals by secondary intention.[24]
Complications
Diagnosis
History and Symptoms
- Patients with low abscess typically present with anal pain. Other findings include:[25]
- Anal pain
- Pain associated with bowel movement: It is worse when the person sits down and right before a bowel movement. After the individual has a bowel movement, the pain usually lessens.[26]
- Swelling
- Chills
- Constipation
- Discharge of pus from the rectum
- Fever
- Patients with high abscess present with :
Physical Examination
General Appearance
- Patients with high abscess present with fever, elevated body temperature can be noticed.[3]
Digital Rectal Examination
- It is difficult to perform digital rectal examination due to the severe pain, therefore patient should be examined under local anesthesia to identify the location of the abscess and also if suspicion of a high abscess (Supralevator abscess) is present.
- Anoscopy should not be performed.[27]
- Anorectal abscess is a clinical diagnosis and presence of induration, tenderness and fluctulance are diagnostic of perianal and ishciorectal abscess. In patients with intersphincteric or supralevator abscesses external findings are minimal only pelvic or rectal tenderness or fluctulance on digital rectal examination can be demonstrated.
Physical examination findings demonstrated in anorectal abscess include: [3]
- Erythema
- Warmth
- Tenderness
- Induration
- Fluctulance
(Images courtesy of Charlie Goldberg, M.D., UCSD School of Medicine and VA Medical Center, San Diego, CA)
Laboratory Findings
- Anorectal abscess is a clinical diagnosis and physical examination is sufficient to make the diagnosis, therefore complete laboratory testing is not done in most of the patients.[3]
- Complete blood count will demonstrate a neutrophilia and elevated ESR.
- Bleeding time and clotting time and routine pre-operative evaluation must be performed.
- Culture and gram staining of the necrotic tissue is done to establish cause of infection.
Imaging
Ultrasound
- Endoanal ultrasound is useful in detecting horse-shoe abscesses extension and presence of fistula tracts with high sensitivity.[28]
- Three dimensional ultrasound is useful in patients to identify the anatomical locations of complex perianal abscesses and fistula tracts.[29]
CT Scan
- CT scan is useful in patients with complex suppurative anorectal conditions such as supralevator abscess and to identify other etiologies causing anorectal abscess such as pelvic infections, appendicitis, Crohn's disease and diverticulitis.
Treatment
Medical Therapy
- Medical therapy is not recommended in patients with anal abscess as the antibiotics have poor penetration in to the abscess cavity and are not helpful to in treatment of the infection or wound healing.[30][3]
- Antibiotics may be considered in patients with extensive cellulitis, HIV infection and diabetes mellitus.[3]
- Patients with low neutrophil count (500-1000/mm³) and also in patients with no fluctulance medical therapy can be helpful in resolution of the abscess, however in patients with neutrophil count of >1000/mm³ and with fluctulance surgical drainage is a better option for treatment.[31][3]
- Prophylactic antibiotics prior to incision and drainage is recommended by American Heart Association, in patients with prosthetic valves, previous bacterial endocarditis, congenital heart disease, and heart transplant recipients with valve pathology.[32][3]
Surgical Therapy
- Management of anal abscess should be prompt as the risk of involving the surrounding tissue resulting in perineal cellulitis and sepsis is high.[33]
- Primary treatment for anorectal abscess is incision and drainage and it should be performed within 24 hours of presentation.
- Patients with perianal abscess and ischiorectal abscess can be treated in a outpatient setting under local anesthesia using 1% lidocaine or bupivacaine with epinephrine is injected subcutaneously into the area affected by the abscess to provide adequate infilteration into the skin. [3]
- Patients with loculations or large ischiorectal, intersphincteric, supralevator, or horseshoe abscesses should be admitted to the hospital and the procedure should be performed under anesthesia.[3]
Procedure
- Under aseptic precautions a scalpel is used to make a cruciate or elliptical incision over the area of flactulance. The incision should be close to the anal verge to minimize the length of a potential fistula.[3]
- After incision is made the necrotic tissue is removed and loculations are broken using a hemostat or a finger.[3]
- After the procedure the wound is packed with a gauze sponge which is removed after 24 hours.[34]
- Regular sitz bath is recommended after the surgery, it will help in local cleansing and wound healing.
- A variation in the incision and drainage is using a small latex catheter (Pezzer catheter). After a small incision is made the catheter is inserted into the cavity and is left in place for a duration of 3 to 10 days till the abscess cavity is drained and the cavity closes around the catheter.[35]
Complications
- Recurrence of the abscess: The recurrence rate depends on the location of the abscess and the duration of follow-up, the rate ranges from 3% to 44%. Other factors influencing the recurrence rate include incomplete initial drainage, failure to break up loculations within the abscess, missed abscess undiagnosed fistula. Recurrence rates are high in horseshoe abscess with a range from 18% to 50% which require multiple surgeries.[36][37][38][3]
- Urinary retention
- Postoperative bleeding
Prevention
Primary Prevention
- Abstain from anal intercourse
- Adequate treatment of Crohn's disease and HIV infection
- Maintaining proper hygiene
Secondary Prevention
- Early incision and drainage, with regular sitz bath is adviced in all patients.
- Identification of pre-existing fistula tract and fistulotomy during incision and drainage decreases the risk of recurrence and fistula formation.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Abcarian H (2011). "Anorectal infection: abscess-fistula". Clin Colon Rectal Surg. 24 (1): 14–21. doi:10.1055/s-0031-1272819. PMC 3140329. PMID 22379401.
- ↑ Janicke DM, Pundt MR (1996). "Anorectal disorders". Emerg. Med. Clin. North Am. 14 (4): 757–88. doi:10.1016/S0733-8627(05)70278-9. PMID 8921768. Unknown parameter
|month=ignored (help) - ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 Steele, Scott R.; Kumar, Ravin; Feingold, Daniel L.; Rafferty, Janice L.; Buie, W. Donald (2011). "Practice Parameters for the Management of Perianal Abscess and Fistula-in-Ano". Diseases of the Colon & Rectum. 54 (12): 1465–1474. doi:10.1097/DCR.0b013e31823122b3. ISSN 0012-3706.
- ↑ Rizzo JA, Naig AL, Johnson EK (2010). "Anorectal abscess and fistula-in-ano: evidence-based management". Surg Clin North Am. 90 (1): 45–68, Table of Contents. doi:10.1016/j.suc.2009.10.001. PMID 20109632.
- ↑ 5.0 5.1 5.2 "Anatomy and Embryology - Springer".
- ↑ Rickard MJ (2005). "Anal abscesses and fistulas". ANZ J Surg. 75 (1–2): 64–72. doi:10.1111/j.1445-2197.2005.03280.x. PMID 15740520.
- ↑ PARKS AG (1961). "Pathogenesis and treatment of fistuila-in-ano". Br Med J. 1 (5224): 463–9. PMC 1953161. PMID 13732880.
- ↑ Coremans G, Dockx S, Wyndaele J, Hendrickx A (2003). "Do anal fistulas in Crohn's disease behave differently and defy Goodsall's rule more frequently than fistulas that are cryptoglandular in origin?". Am J Gastroenterol. 98 (12): 2732–5. doi:10.1111/j.1572-0241.2003.08716.x. PMID 14687825.
- ↑ Albright JB, Pidala MJ, Cali JR, Snyder MJ, Voloyiannis T, Bailey HR (2007). "MRSA-related perianal abscesses: an underrecognized disease entity". Dis Colon Rectum. 50 (7): 996–1003. doi:10.1007/s10350-007-0221-x. PMID 17525863.
- ↑ Ommer A, Herold A, Berg E, Fürst A, Sailer M, Schiedeck T (2012). "German S3 guideline: anal abscess". Int J Colorectal Dis. 27 (6): 831–7. doi:10.1007/s00384-012-1430-x. PMID 22362468.
- ↑ 11.0 11.1 Read DR, Abcarian H (1979). "A prospective survey of 474 patients with anorectal abscess". Dis Colon Rectum. 22 (8): 566–8. PMID 527452.
- ↑ Adamo K, Sandblom G, Brännström F, Strigård K (2016). "Prevalence and recurrence rate of perianal abscess--a population-based study, Sweden 1997-2009". Int J Colorectal Dis. 31 (3): 669–73. doi:10.1007/s00384-015-2500-7. PMID 26768004.
- ↑ Goldberg, Gary S.; Orkin, Bruce A.; Smith, Lee E. (1994). "Microbiology of human immunodeficiency virus anorectal disease". Diseases of the Colon & Rectum. 37 (5): 439–443. doi:10.1007/BF02076188. ISSN 0012-3706.
- ↑ Adikrisna R, Udagawa M, Sugita Y, Ishii T, Okamoto H, Yabata E (2015). "[A Case of Squamous Cell Carcinoma of the Anal Canal with a Perianal Abscess]". Gan To Kagaku Ryoho. 42 (12): 2322–4. PMID 26805351.
- ↑ Schlichtemeier S, Engel A (2016). "Anal fissure". Aust Prescr. 39 (1): 14–7. doi:10.18773/austprescr.2016.007. PMC 4816871. PMID 27041801.
- ↑ Beaty JS, Shashidharan M (2016). "Anal Fissure". Clin Colon Rectal Surg. 29 (1): 30–7. doi:10.1055/s-0035-1570390. PMC 4755763. PMID 26929749.
- ↑ Cannon JA (2017). "Evaluation, Diagnosis, and Medical Management of Rectal Prolapse". Clin Colon Rectal Surg. 30 (1): 16–21. doi:10.1055/s-0036-1593431. PMID 28144208.
- ↑ Blaker K, Anandam JL (2017). "Functional Disorders: Rectoanal Intussusception". Clin Colon Rectal Surg. 30 (1): 5–11. doi:10.1055/s-0036-1593433. PMID 28144206.
- ↑ Sahnan K, Adegbola SO, Tozer PJ, Watfah J, Phillips RK (2017). "Perianal abscess". BMJ. 356: j475. PMID 28223268.
- ↑ Moureau-Zabotto L, Vendrely V, Abramowitz L, Borg C, Francois E, Goere D, Huguet F, Peiffert D, Siproudhis L, Ducreux M, Bouché O (2017). "Anal cancer: French Intergroup Clinical Practice Guidelines for diagnosis, treatment and follow-up". Dig Liver Dis. doi:10.1016/j.dld.2017.05.011. PMID 28610905.
- ↑ Prigge ES, von Knebel Doeberitz M, Reuschenbach M (2017). "Clinical relevance and implications of HPV-induced neoplasia in different anatomical locations". Mutat. Res. 772: 51–66. doi:10.1016/j.mrrev.2016.06.005. PMID 28528690.
- ↑ Wieland U, Kreuter A (2017). "[Genital warts in HIV-infected individuals]". Hautarzt (in German). 68 (3): 192–198. doi:10.1007/s00105-017-3938-z. PMID 28160045.
- ↑ Köhn FM, Schultheiss D, Krämer-Schultheiss K (2016). "[Dermatological diseases of the external male genitalia : Part 2: Infectious and malignant dermatological]". Urologe A (in German). 55 (7): 981–96. doi:10.1007/s00120-016-0163-9. PMID 27364818.
- ↑ Ramanujam PS, Prasad ML, Abcarian H, Tan AB (1984). "Perianal abscesses and fistulas. A study of 1023 patients". Dis Colon Rectum. 27 (9): 593–7. PMID 6468199.
- ↑ Whiteford MH, Kilkenny J, Hyman N, Buie WD, Cohen J, Orsay C; et al. (2005). "Practice parameters for the treatment of perianal abscess and fistula-in-ano (revised)". Dis Colon Rectum. 48 (7): 1337–42. doi:10.1007/s10350-005-0055-3. PMID 15933794.
- ↑ Ferri, Fred (2015). Ferri's clinical advisor 2015 : 5 books in 1. Philadelphia, PA: Elsevier/Mosby. ISBN 978-0323083751.
- ↑ Chang J, Mclemore E, Tejirian T (2016). "Anal Health Care Basics". Perm J. 20 (4): 74–80. doi:10.7812/TPP/15-222. PMC 5101094. PMID 27723447.
- ↑ Sheikh P (2012). "Controversies in fistula in ano". Indian J Surg. 74 (3): 217–20. doi:10.1007/s12262-012-0594-5. PMC 3397182. PMID 23730047.
- ↑ Santoro GA, Fortling B (2007). "The advantages of volume rendering in three-dimensional endosonography of the anorectum". Dis Colon Rectum. 50 (3): 359–68. doi:10.1007/s10350-006-0767-z. PMID 17237912.
- ↑ Stewart MP, Laing MR, Krukowski ZH (1985). "Treatment of acute abscesses by incision, curettage and primary suture without antibiotics: a controlled clinical trial". Br J Surg. 72 (1): 66–7. PMID 3881155.
- ↑ Macfie J, Harvey J (1977). "The treatment of acute superficial abscesses: a prospective clinical trial". Br J Surg. 64 (4): 264–6. PMID 322789.
- ↑ Wilson W, Taubert KA, Gewitz M, Lockhart PB, Baddour LM, Levison M; et al. (2007). "Prevention of infective endocarditis: guidelines from the American Heart Association: a guideline from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group". Circulation. 116 (15): 1736–54. doi:10.1161/CIRCULATIONAHA.106.183095. PMID 17446442.
- ↑ Slauf P, Antoš F, Marx J (2014). "[Acute periproctal abscesses]". Rozhl Chir. 93 (4): 226–31. PMID 24881481.
- ↑ Smith SR, Newton K, Smith JA, Dumville JC, Iheozor-Ejiofor Z, Pearce LE; et al. (2016). "Internal dressings for healing perianal abscess cavities". Cochrane Database Syst Rev (8): CD011193. doi:10.1002/14651858.CD011193.pub2. PMID 27562822.
- ↑ Hasan RM (2016). "A study assessing postoperative Corrugate Rubber drain of perianal abscess". Ann Med Surg (Lond). 11: 42–46. doi:10.1016/j.amsu.2016.09.003. PMC 5037211. PMID 27699001.
- ↑ Cox SW, Senagore AJ, Luchtefeld MA, Mazier WP (1997). "Outcome after incision and drainage with fistulotomy for ischiorectal abscess". Am Surg. 63 (8): 686–9. PMID 9247434.
- ↑ Onaca N, Hirshberg A, Adar R (2001). "Early reoperation for perirectal abscess: a preventable complication". Dis Colon Rectum. 44 (10): 1469–73. PMID 11598476.
- ↑ Held D, Khubchandani I, Sheets J, Stasik J, Rosen L, Riether R (1986). "Management of anorectal horseshoe abscess and fistula". Dis Colon Rectum. 29 (12): 793–7. PMID 3792160.

