Ovarian germ cell tumor pathophysiology: Difference between revisions
| (39 intermediate revisions by the same user not shown) | |||
| Line 3: | Line 3: | ||
{{CMG}}; {{AE}} {{Sahar}} {{MD}} | {{CMG}}; {{AE}} {{Sahar}} {{MD}} | ||
==Overveiw== | ==Overveiw== | ||
The pathophysiology of ovarian germ cell tumors depends on the histological subtype. However, their origin is the primordial germ cells that transformed pathologically in different stages of development. | The [[pathophysiology]] of [[ovarian]] [[germ cell]] [[tumors]] depends on the [[histological]] subtype. However, their origin is the [[primordial germ cells]] that [[Transformation|transformed]] [[Pathology|pathologically]] in different stages of development. | ||
==Pathophysiology== | ==Pathophysiology== | ||
=== | ===Pathogenesis=== | ||
*It is understood that [[ovarian]] [[germ cell]] [[tumors]] are the result of the [[Pathology|pathologic]] [[transformation]] of [[primordial germ cells]] during different stages of the development.<ref name="El-MaarriRijlaarsdam2015">{{cite journal|last1=El-Maarri|first1=Osman|last2=Rijlaarsdam|first2=Martin A.|last3=Tax|first3=David M. J.|last4=Gillis|first4=Ad J. M.|last5=Dorssers|first5=Lambert C. J.|last6=Koestler|first6=Devin C.|last7=de Ridder|first7=Jeroen|last8=Looijenga|first8=Leendert H. J.|title=Genome Wide DNA Methylation Profiles Provide Clues to the Origin and Pathogenesis of Germ Cell Tumors|journal=PLOS ONE|volume=10|issue=4|year=2015|pages=e0122146|issn=1932-6203|doi=10.1371/journal.pone.0122146}}</ref><ref>{{cite book | last = Carcangiu | first = M. L. | title = WHO Classification of Tumours of Female Reproductive Organs | publisher = International Agency for Research on Cancer | location = Lyon | year = 2014 | isbn = 978-92-832-4487-5 }}</ref> | |||
{{familytree/start |summary=Sample 1}} | |||
{{familytree | | | | | | | | A01 |A01=[[Germ cell]]}} | |||
{{familytree | | | | |,|-|-|-|^|-|-|-|-|.| | | }} | |||
{{familytree | | | B01 | | | | | | | | B02 | | |B01=[[Pathogenesis]]|B02=[[Malignant transformation]]}} | |||
{{familytree | | | |!| | | | | | | | | |!| }} | |||
{{familytree | | | C01 | | | | | | | | |!| |C01=[[Mature teratoma]]}} | |||
{{familytree | | | | | | | | | | | | | |!}} | |||
{{familytree | | | | | | | | | |,|-|-|-|+|-|-|-|.| }} | |||
{{familytree | | | | | | | | | E01 | | E02 | | E03 |E01=[[Tumors]] esxpressing [[transcription factors]] of [[pluripotency]]|E02=[[Tumors]] with primitive [[embryonic]] [[ectoderm]], [[mesoderm]], and/or [[endoderm]] differentiation|E03=[[Tumors]] with extraembroyonic differentiation}} | |||
{{familytree | | | | | | | | | |!| | | |!| | | |!| | }} | |||
{{familytree | | | | | | | | | F01 | | F02 | | F03 | |F01=[[Dysgerminoma]]/[[Embryonal carcinoma]]|F02=Immature [[teratoma]]|F03=[[Yolk sac tumor]]/[[Choriocarcinoma]]}} | |||
{{familytree/end}} | |||
===Mature teratoma=== | ===Mature teratoma=== | ||
*Mature teratomas are benign tumors originating from pathologic development of primordial germ cells.<ref name="VuralVural2015">{{cite journal|last1=Vural|first1=F.|last2=Vural|first2=B.|last3=Paksoy|first3=N.|title=Vaginal teratoma: A case report and review of the literature|journal=Journal of Obstetrics and Gynaecology|volume=35|issue=7|year=2015|pages=757–758|issn=0144-3615|doi=10.3109/01443615.2015.1004525}}</ref> | *[[Mature cystic teratoma|Mature teratomas]] are [[benign tumors]] originating from [[Pathology|pathologic]] development of [[primordial germ cells]].<ref name="VuralVural2015">{{cite journal|last1=Vural|first1=F.|last2=Vural|first2=B.|last3=Paksoy|first3=N.|title=Vaginal teratoma: A case report and review of the literature|journal=Journal of Obstetrics and Gynaecology|volume=35|issue=7|year=2015|pages=757–758|issn=0144-3615|doi=10.3109/01443615.2015.1004525}}</ref> | ||
*It originates from a single germ cell tumor after the first phase of meiosis.<ref name="LinderMcCaw1975">{{cite journal|last1=Linder|first1=David|last2=McCaw|first2=Barbara Kaiser|last3=Hecht|first3=Frederick|title=Parthenogenic Origin of Benign Ovarian Teratomas|journal=New England Journal of Medicine|volume=292|issue=2|year=1975|pages=63–66|issn=0028-4793|doi=10.1056/NEJM197501092920202}}</ref> | *It originates from a single [[germ cell]] [[tumor]] after the first phase of [[Meiosis I|meiosis]].<ref name="LinderMcCaw1975">{{cite journal|last1=Linder|first1=David|last2=McCaw|first2=Barbara Kaiser|last3=Hecht|first3=Frederick|title=Parthenogenic Origin of Benign Ovarian Teratomas|journal=New England Journal of Medicine|volume=292|issue=2|year=1975|pages=63–66|issn=0028-4793|doi=10.1056/NEJM197501092920202}}</ref> | ||
*These tumors contain the well-differentiated component of three germ layers.<ref name="VuralVural2015">{{cite journal|last1=Vural|first1=F.|last2=Vural|first2=B.|last3=Paksoy|first3=N.|title=Vaginal teratoma: A case report and review of the literature|journal=Journal of Obstetrics and Gynaecology|volume=35|issue=7|year=2015|pages=757–758|issn=0144-3615|doi=10.3109/01443615.2015.1004525}}</ref> | *These [[tumors]] contain the well-[[Differentiation|differentiated]] component of three [[germ layers]].<ref name="VuralVural2015">{{cite journal|last1=Vural|first1=F.|last2=Vural|first2=B.|last3=Paksoy|first3=N.|title=Vaginal teratoma: A case report and review of the literature|journal=Journal of Obstetrics and Gynaecology|volume=35|issue=7|year=2015|pages=757–758|issn=0144-3615|doi=10.3109/01443615.2015.1004525}}</ref> | ||
*Their usual location is the embryonic fusion line overhead and neck, mediastinum, a and presacral area and tend to present at a greater extent in the midline. | *Their usual location is the [[embryonic]] fusion line overhead and [[neck]], [[mediastinum]], a and presacral area and tend to present at a greater extent in the midline. | ||
===Dysgerminoma=== | ===Dysgerminoma=== | ||
*Dysgerminoma arises from primordial germ cells, which are gonadal cells that are normally involved in the gametogenesis.<ref name="El-MaarriRijlaarsdam2015">{{cite journal|last1=El-Maarri|first1=Osman|last2=Rijlaarsdam|first2=Martin A.|last3=Tax|first3=David M. J.|last4=Gillis|first4=Ad J. M.|last5=Dorssers|first5=Lambert C. J.|last6=Koestler|first6=Devin C.|last7=de Ridder|first7=Jeroen|last8=Looijenga|first8=Leendert H. J.|title=Genome Wide DNA Methylation Profiles Provide Clues to the Origin and Pathogenesis of Germ Cell Tumors|journal=PLOS ONE|volume=10|issue=4|year=2015|pages=e0122146|issn=1932-6203|doi=10.1371/journal.pone.0122146}}</ref> | *[[Dysgerminoma]] arises from [[primordial germ cells]], which are [[gonadal]] [[cells]] that are normally involved in the [[gametogenesis]].<ref name="El-MaarriRijlaarsdam2015">{{cite journal|last1=El-Maarri|first1=Osman|last2=Rijlaarsdam|first2=Martin A.|last3=Tax|first3=David M. J.|last4=Gillis|first4=Ad J. M.|last5=Dorssers|first5=Lambert C. J.|last6=Koestler|first6=Devin C.|last7=de Ridder|first7=Jeroen|last8=Looijenga|first8=Leendert H. J.|title=Genome Wide DNA Methylation Profiles Provide Clues to the Origin and Pathogenesis of Germ Cell Tumors|journal=PLOS ONE|volume=10|issue=4|year=2015|pages=e0122146|issn=1932-6203|doi=10.1371/journal.pone.0122146}}</ref> | ||
*The majority of dysgerminomas in women present in the stage 1A.<ref name=" | *The majority of [[Dysgerminoma|dysgerminomas]] in women present in the stage 1A.<ref name="AL HusainiSoudy2012">{{cite journal|last1=AL Husaini|first1=Hamed|last2=Soudy|first2=Hussein|last3=Darwish|first3=Alaa El Din|last4=Ahmed|first4=Mohamed|last5=Eltigani|first5=Amin|last6=AL Mubarak|first6=Mustafa|last7=Sabaa|first7=Amal Abu|last8=Edesa|first8=Wael|last9=AL-Tweigeri|first9=Taher|last10=Al-Badawi|first10=Ismail A.|title=Pure dysgerminoma of the ovary: a single institutional experience of 65 patients|journal=Medical Oncology|volume=29|issue=4|year=2012|pages=2944–2948|issn=1357-0560|doi=10.1007/s12032-012-0194-z}}</ref> | ||
*Bilateral invovlement occurs in 10% to 15% of the cases. | |||
*In < 15% of the affected cases, elements of other germ cell tumors can also be found.<ref name="pmid7279343">{{cite journal |vauthors=Gordon A, Lipton D, Woodruff JD |title=Dysgerminoma: a review of 158 cases from the Emil Novak Ovarian Tumor Registry |journal=Obstet Gynecol |volume=58 |issue=4 |pages=497–504 |date=October 1981 |pmid=7279343 |doi= |url=}}</ref> | *[[Bilateral]] invovlement occurs in 10% to 15% of the cases. | ||
*In < 15% of the affected cases, elements of other [[germ cell]] [[tumors]] can also be found.<ref name="pmid7279343">{{cite journal |vauthors=Gordon A, Lipton D, Woodruff JD |title=Dysgerminoma: a review of 158 cases from the Emil Novak Ovarian Tumor Registry |journal=Obstet Gynecol |volume=58 |issue=4 |pages=497–504 |date=October 1981 |pmid=7279343 |doi= |url=}}</ref> | |||
===Yolk sac tumor=== | ===Yolk sac tumor=== | ||
* | *These [[tumors]] develop from [[differentiation]] of [[Primordial germ cells|primitive germ cells]] in the direction of [[yolk sac]] or [[Vitelline arteries|vitelline structures]].<ref name="Young2014">{{cite journal|last1=Young|first1=Robert H.|title=The Yolk Sac Tumor|journal=International Journal of Surgical Pathology|volume=22|issue=8|year=2014|pages=677–687|issn=1066-8969|doi=10.1177/1066896914558265}}</ref> | ||
*They tend to grow very rapidly.<ref name="ShaabanRezvani2014">{{cite journal|last1=Shaaban|first1=Akram M.|last2=Rezvani|first2=Maryam|last3=Elsayes|first3=Khaled M.|last4=Baskin|first4=Henry|last5=Mourad|first5=Amr|last6=Foster|first6=Bryan R.|last7=Jarboe|first7=Elke A.|last8=Menias|first8=Christine O.|title=Ovarian Malignant Germ Cell Tumors: Cellular Classification and Clinical and Imaging Features|journal=RadioGraphics|volume=34|issue=3|year=2014|pages=777–801|issn=0271-5333|doi=10.1148/rg.343130067}}</ref> | *They tend to grow very rapidly.<ref name="ShaabanRezvani2014">{{cite journal|last1=Shaaban|first1=Akram M.|last2=Rezvani|first2=Maryam|last3=Elsayes|first3=Khaled M.|last4=Baskin|first4=Henry|last5=Mourad|first5=Amr|last6=Foster|first6=Bryan R.|last7=Jarboe|first7=Elke A.|last8=Menias|first8=Christine O.|title=Ovarian Malignant Germ Cell Tumors: Cellular Classification and Clinical and Imaging Features|journal=RadioGraphics|volume=34|issue=3|year=2014|pages=777–801|issn=0271-5333|doi=10.1148/rg.343130067}}</ref> | ||
*Bilateral involvement occurs in less than 5% of the cases. | *[[Bilateral]] involvement occurs in less than 5% of the cases. | ||
*In 10% of the cases, the contralateral ovary carries a dermoid cyst. | *In 10% of the cases, the [[contralateral]] ovary carries a [[dermoid cyst]]. | ||
*In 40% of cases, they are accompanied by other types of germ cell tumors.<ref name="KojimaharaNakahara2013">{{cite journal|last1=Kojimahara|first1=Takanobu|last2=Nakahara|first2=Kenji|last3=Takano|first3=Tadao|last4=Yaegashi|first4=Nobuo|last5=Nishiyama|first5=Hiroshi|last6=Fujimori|first6=Keiya|last7=Sato|first7=Naoki|last8=Terada|first8=Yukihiro|last9=Tase|first9=Toru|last10=Yokoyama|first10=Yoshihito|last11=Mizunuma|first11=Hideki|last12=Shoji|first12=Tadahiro|last13=Sugiyama|first13=Toru|last14=Kurachi|first14=Hirohisa|title=Yolk Sac Tumor of the Ovary: A Retrospective Multicenter Study of 33 Japanese Women by Tohoku Gynecologic Cancer Unit (TGCU)|journal=The Tohoku Journal of Experimental Medicine|volume=230|issue=4|year=2013|pages=211–217|issn=1349-3329|doi=10.1620/tjem.230.211}}</ref> | *In 40% of cases, they are accompanied by other types of [[germ cell]] [[tumors]].<ref name="KojimaharaNakahara2013">{{cite journal|last1=Kojimahara|first1=Takanobu|last2=Nakahara|first2=Kenji|last3=Takano|first3=Tadao|last4=Yaegashi|first4=Nobuo|last5=Nishiyama|first5=Hiroshi|last6=Fujimori|first6=Keiya|last7=Sato|first7=Naoki|last8=Terada|first8=Yukihiro|last9=Tase|first9=Toru|last10=Yokoyama|first10=Yoshihito|last11=Mizunuma|first11=Hideki|last12=Shoji|first12=Tadahiro|last13=Sugiyama|first13=Toru|last14=Kurachi|first14=Hirohisa|title=Yolk Sac Tumor of the Ovary: A Retrospective Multicenter Study of 33 Japanese Women by Tohoku Gynecologic Cancer Unit (TGCU)|journal=The Tohoku Journal of Experimental Medicine|volume=230|issue=4|year=2013|pages=211–217|issn=1349-3329|doi=10.1620/tjem.230.211}}</ref> | ||
==Genetics== | ==Genetics== | ||
*Dysgerminomas may be associated with gain or loss of complete or partial chromosomal materials such as:<ref name="pmid10850452">{{cite journal |vauthors=Kraggerud SM, Szymanska J, Abeler VM, Kaern J, Eknaes M, Heim S, Teixeira MR, Tropé CG, Peltomäki P, Lothe RA |title=DNA copy number changes in malignant ovarian germ cell tumors |journal=Cancer Res. |volume=60 |issue=11 |pages=3025–30 |date=June 2000 |pmid=10850452 |doi= |url=}}</ref> | *[[Ovarian]] [[germ cell]] [[tumors]] may be associated with [[cytogenetic]] abnormalities. | ||
*Immature teratomas may be associated with [[chromosomal]] changes such as:<ref name="pmid10850452">{{cite journal |vauthors=Kraggerud SM, Szymanska J, Abeler VM, Kaern J, Eknaes M, Heim S, Teixeira MR, Tropé CG, Peltomäki P, Lothe RA |title=DNA copy number changes in malignant ovarian germ cell tumors |journal=Cancer Res. |volume=60 |issue=11 |pages=3025–30 |date=June 2000 |pmid=10850452 |doi= |url=}}</ref> | |||
**[[Gain]] of all or parts of | |||
***1p | |||
***16p | |||
***19 | |||
***22q | |||
*[[Dysgerminoma|Dysgerminomas]] may be associated with gain or loss of complete or partial [[chromosomal]] materials such as:<ref name="pmid10850452">{{cite journal |vauthors=Kraggerud SM, Szymanska J, Abeler VM, Kaern J, Eknaes M, Heim S, Teixeira MR, Tropé CG, Peltomäki P, Lothe RA |title=DNA copy number changes in malignant ovarian germ cell tumors |journal=Cancer Res. |volume=60 |issue=11 |pages=3025–30 |date=June 2000 |pmid=10850452 |doi= |url=}}</ref> | |||
**Gain of: | **Gain of: | ||
***1p | ***1p | ||
| Line 42: | Line 61: | ||
***21q | ***21q | ||
***22q | ***22q | ||
***Whole of chromosome 7 | ***Whole of [[chromosome 7]] | ||
***Whole of chromosome 8 | ***Whole of [[chromosome 8]] | ||
***Whole of | ***Whole of [[chromosome 17]] | ||
***Whole of | ***Whole of [[chromosome 19]] | ||
**Losses from 13q | **Losses from 13q | ||
*Yolk sac tumor is associated with gaining of the 12p chromosome in 75% of the cases.<ref name="pmid10850452">{{cite journal |vauthors=Kraggerud SM, Szymanska J, Abeler VM, Kaern J, Eknaes M, Heim S, Teixeira MR, Tropé CG, Peltomäki P, Lothe RA |title=DNA copy number changes in malignant ovarian germ cell tumors |journal=Cancer Res. |volume=60 |issue=11 |pages=3025–30 |date=June 2000 |pmid=10850452 |doi= |url=}}</ref> | *Yolk sac [[tumor]] is associated with gaining of the 12p [[chromosome]] in 75% of the cases.<ref name="pmid10850452">{{cite journal |vauthors=Kraggerud SM, Szymanska J, Abeler VM, Kaern J, Eknaes M, Heim S, Teixeira MR, Tropé CG, Peltomäki P, Lothe RA |title=DNA copy number changes in malignant ovarian germ cell tumors |journal=Cancer Res. |volume=60 |issue=11 |pages=3025–30 |date=June 2000 |pmid=10850452 |doi= |url=}}</ref> | ||
* | **It may also be associated with [[chromosomal]] changes such as: | ||
***Gain of 1q | |||
* | |||
**Gain of | |||
==Associated Conditions== | ==Associated Conditions== | ||
Conditions associated with mature teratoma include: | [[Conditions]] associated with [[Mature cystic teratoma|mature teratoma]] include: | ||
*Anti-NMDA receptor encephalitis (although very rarely)<ref name="DalmauGleichman2008">{{cite journal|last1=Dalmau|first1=Josep|last2=Gleichman|first2=Amy J|last3=Hughes|first3=Ethan G|last4=Rossi|first4=Jeffrey E|last5=Peng|first5=Xiaoyu|last6=Lai|first6=Meizan|last7=Dessain|first7=Scott K|last8=Rosenfeld|first8=Myrna R|last9=Balice-Gordon|first9=Rita|last10=Lynch|first10=David R|title=Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies|journal=The Lancet Neurology|volume=7|issue=12|year=2008|pages=1091–1098|issn=14744422|doi=10.1016/S1474-4422(08)70224-2}}</ref> | *[[Anti-NMDA receptor encephalitis]] (although very rarely)<ref name="DalmauGleichman2008">{{cite journal|last1=Dalmau|first1=Josep|last2=Gleichman|first2=Amy J|last3=Hughes|first3=Ethan G|last4=Rossi|first4=Jeffrey E|last5=Peng|first5=Xiaoyu|last6=Lai|first6=Meizan|last7=Dessain|first7=Scott K|last8=Rosenfeld|first8=Myrna R|last9=Balice-Gordon|first9=Rita|last10=Lynch|first10=David R|title=Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies|journal=The Lancet Neurology|volume=7|issue=12|year=2008|pages=1091–1098|issn=14744422|doi=10.1016/S1474-4422(08)70224-2}}</ref> | ||
*Rarely, they | *Rarely, they contain [[pituitary]] [[cells]] capable of [[prolactin]] production and is associated with [[prolactinoma]].<ref name="KallenbergPesce1991">{{cite journal|last1=Kallenberg|first1=GA|last2=Pesce|first2=CM|last3=Norman|first3=B|last4=Ratner|first4=RE|last5=Silverberg|first5=SG|title=Ectopic hyperprolactinemia resulting from an ovarian teratoma|journal=International Journal of Gynecology & Obstetrics|volume=34|issue=2|year=1991|pages=194–195|issn=00207292|doi=10.1016/0020-7292(91)90266-8}}</ref> | ||
Polyembryoma may be associated with [[Klinefelter syndrome]].<ref name="pmid12679648">{{cite journal |vauthors=Beresford L, Fernandez CV, Cummings E, Sanderson S, Ming-Yu W, Giacomantonio M |title=Mediastinal polyembryoma associated with Klinefelter syndrome |journal=J. Pediatr. Hematol. Oncol. |volume=25 |issue=4 |pages=321–3 |date=April 2003 |pmid=12679648 |doi= |url=}}</ref> | |||
==Gross Pathology== | ==Gross Pathology== | ||
{| {{table}} | {| {{table}} cellpadding="4" cellspacing="0" style="border:#c9c9c9 1px solid; margin: 1em 1em 1em 0; border-collapse: collapse;" | ||
| align="center" style="background: #4479BA;" | {{fontcolor|#FFF|''' Ovarian germ cell tumor subtype'''}} | | align="center" style="background: #4479BA;" | {{fontcolor|#FFF|''' Ovarian germ cell tumor subtype'''}} | ||
| align="center" style="background: #4479BA;" | {{fontcolor|#FFF|'''Features on Gross Pathology'''}} | | align="center" style="background: #4479BA;" | {{fontcolor|#FFF|'''Features on Gross Pathology'''}} | ||
|- | |- | ||
| ''' | | '''Dysgerminonma'''|| | ||
* Unilateral (bilateral in 10% to 20% of the cases)<ref name=" | * Unilateral ([[bilateral]] in 10% to 20% of the cases)<ref name="pmid12733128">{{cite journal |vauthors=Chen VW, Ruiz B, Killeen JL, Coté TR, Wu XC, Correa CN |title=Pathology and classification of ovarian tumors |journal=Cancer |volume=97 |issue=10 Suppl |pages=2631–42 |date=May 2003 |pmid=12733128 |doi=10.1002/cncr.11345 |url=}}</ref> | ||
* more common on the right side | |||
* | * [[Solid]], white or grayish-withe [[Tumor|tumors]] | ||
* | |- | ||
| '''Embryonal Carcinoma'''|| | |||
* Unilateral, large [[mass]], averaging 17 cm <ref name="ShaabanRezvani2014">{{cite journal|last1=Shaaban|first1=Akram M.|last2=Rezvani|first2=Maryam|last3=Elsayes|first3=Khaled M.|last4=Baskin|first4=Henry|last5=Mourad|first5=Amr|last6=Foster|first6=Bryan R.|last7=Jarboe|first7=Elke A.|last8=Menias|first8=Christine O.|title=Ovarian Malignant Germ Cell Tumors: Cellular Classification and Clinical and Imaging Features|journal=RadioGraphics|volume=34|issue=3|year=2014|pages=777–801|issn=0271-5333|doi=10.1148/rg.343130067}}</ref> | |||
* Smooth outer [[Surface area|surface]] | |||
* Extensive area of [[necrosis]] and [[hemorrhage]] | |||
|- | |- | ||
|'''Endodermal sinus tumor or yolk sac tumors'''|| | |'''Endodermal sinus tumor or yolk sac tumors'''|| | ||
* Mixed solid and cystic component<ref name="ShaabanRezvani2014">{{cite journal|last1=Shaaban|first1=Akram M.|last2=Rezvani|first2=Maryam|last3=Elsayes|first3=Khaled M.|last4=Baskin|first4=Henry|last5=Mourad|first5=Amr|last6=Foster|first6=Bryan R.|last7=Jarboe|first7=Elke A.|last8=Menias|first8=Christine O.|title=Ovarian Malignant Germ Cell Tumors: Cellular Classification and Clinical and Imaging Features|journal=RadioGraphics|volume=34|issue=3|year=2014|pages=777–801|issn=0271-5333|doi=10.1148/rg.343130067}}</ref> | * Mixed [[solid]] and [[cystic]] component<ref name="ShaabanRezvani2014">{{cite journal|last1=Shaaban|first1=Akram M.|last2=Rezvani|first2=Maryam|last3=Elsayes|first3=Khaled M.|last4=Baskin|first4=Henry|last5=Mourad|first5=Amr|last6=Foster|first6=Bryan R.|last7=Jarboe|first7=Elke A.|last8=Menias|first8=Christine O.|title=Ovarian Malignant Germ Cell Tumors: Cellular Classification and Clinical and Imaging Features|journal=RadioGraphics|volume=34|issue=3|year=2014|pages=777–801|issn=0271-5333|doi=10.1148/rg.343130067}}</ref> | ||
* The solid portion is soft with grey to yellow color and areas of necrosis and/or hemorrhage | * The [[solid]] portion is soft with grey to yellow color and areas of [[necrosis]] and/or [[hemorrhage]] | ||
* The cystic portion is in between solid components and | * The [[cystic]] portion is in between [[solid]] components and results in a meshlike/honeycomb [[appearance]] | ||
* Unilateral and commonly affects the right ovary<ref name="KojimaharaNakahara2013">{{cite journal|last1=Kojimahara|first1=Takanobu|last2=Nakahara|first2=Kenji|last3=Takano|first3=Tadao|last4=Yaegashi|first4=Nobuo|last5=Nishiyama|first5=Hiroshi|last6=Fujimori|first6=Keiya|last7=Sato|first7=Naoki|last8=Terada|first8=Yukihiro|last9=Tase|first9=Toru|last10=Yokoyama|first10=Yoshihito|last11=Mizunuma|first11=Hideki|last12=Shoji|first12=Tadahiro|last13=Sugiyama|first13=Toru|last14=Kurachi|first14=Hirohisa|title=Yolk Sac Tumor of the Ovary: A Retrospective Multicenter Study of 33 Japanese Women by Tohoku Gynecologic Cancer Unit (TGCU)|journal=The Tohoku Journal of Experimental Medicine|volume=230|issue=4|year=2013|pages=211–217|issn=1349-3329|doi=10.1620/tjem.230.211}}</ref> | * Unilateral and commonly affects the right [[ovary]]<ref name="KojimaharaNakahara2013">{{cite journal|last1=Kojimahara|first1=Takanobu|last2=Nakahara|first2=Kenji|last3=Takano|first3=Tadao|last4=Yaegashi|first4=Nobuo|last5=Nishiyama|first5=Hiroshi|last6=Fujimori|first6=Keiya|last7=Sato|first7=Naoki|last8=Terada|first8=Yukihiro|last9=Tase|first9=Toru|last10=Yokoyama|first10=Yoshihito|last11=Mizunuma|first11=Hideki|last12=Shoji|first12=Tadahiro|last13=Sugiyama|first13=Toru|last14=Kurachi|first14=Hirohisa|title=Yolk Sac Tumor of the Ovary: A Retrospective Multicenter Study of 33 Japanese Women by Tohoku Gynecologic Cancer Unit (TGCU)|journal=The Tohoku Journal of Experimental Medicine|volume=230|issue=4|year=2013|pages=211–217|issn=1349-3329|doi=10.1620/tjem.230.211}}</ref> | ||
|- | |||
| '''Mixed germ cell tumors'''|| | |||
* Composed of more than one [[germ cell]] [[tumor]] element<ref name="ShaabanRezvani2014">{{cite journal|last1=Shaaban|first1=Akram M.|last2=Rezvani|first2=Maryam|last3=Elsayes|first3=Khaled M.|last4=Baskin|first4=Henry|last5=Mourad|first5=Amr|last6=Foster|first6=Bryan R.|last7=Jarboe|first7=Elke A.|last8=Menias|first8=Christine O.|title=Ovarian Malignant Germ Cell Tumors: Cellular Classification and Clinical and Imaging Features|journal=RadioGraphics|volume=34|issue=3|year=2014|pages=777–801|issn=0271-5333|doi=10.1148/rg.343130067}}</ref> | |||
* Main components are: | |||
** [[Dysgerminoma]] | |||
** [[Teratoma]] | |||
** [[Yolk sac tumor]] | |||
* Other [[germ cell]] [[tumors]] may be present | |||
|- | |- | ||
| ''' | | '''Polyembryoma'''|| | ||
* | * Large, unilateral [[tumor]] with microcystic surface<ref name="OlivaYoung2014">{{cite journal|last1=Oliva|first1=Esther|last2=Young|first2=Robert H.|title=Germ cell tumours of the ovary: selected topics|journal=Diagnostic Histopathology|volume=20|issue=9|year=2014|pages=364–375|issn=17562317|doi=10.1016/j.mpdhp.2014.07.003}}</ref> | ||
* | * Bulky [[appearance]] | ||
* | * Soft and reddish-brown color | ||
* [[hemorrhage]] in cut [[Surface area|surfaces]] | |||
|- | |- | ||
| '''Teratoma'''|| | | '''Teratoma'''|| | ||
'''Teratoma-mature''' | '''Teratoma-mature''' | ||
* The majority are 5 to 10 cm in diameter.<ref name="Yayla AbideBostancı Ergen2018">{{cite journal|last1=Yayla Abide|first1=Çiğdem|last2=Bostancı Ergen|first2=Evrim|title=Retrospective analysis of mature cystic teratomas in a single center and review of the literature|journal=Journal of Turkish Society of Obstetric and Gynecology|volume=15|issue=2|year=2018|pages=95–98|issn=1307699X|doi=10.4274/tjod.86244}}</ref> | * The majority are 5 to 10 cm in diameter.<ref name="Yayla AbideBostancı Ergen2018">{{cite journal|last1=Yayla Abide|first1=Çiğdem|last2=Bostancı Ergen|first2=Evrim|title=Retrospective analysis of mature cystic teratomas in a single center and review of the literature|journal=Journal of Turkish Society of Obstetric and Gynecology|volume=15|issue=2|year=2018|pages=95–98|issn=1307699X|doi=10.4274/tjod.86244}}</ref> | ||
* Unilocular in the | * Unilocular in the majority of cases (88%) | ||
* Predominantly cystic | * Predominantly [[cystic]] | ||
* Cystic content may contain | * [[Cystic]] content may contain [[sebaceous]] material that is semi-liquid in [[room temperature]] | ||
* Teeth may be found in Rokitansky’s protuberance - a well-defined, nipple-like structure covered with hair | * [[Teeth]] may be found in Rokitansky’s protuberance - a well-defined, [[nipple]]-like structure covered with [[hair]] | ||
'''Teratoma-immature''' | '''Teratoma-immature''' | ||
* Usually appear larger than mature teratomas<ref name="OutwaterSiegelman2001">{{cite journal|last1=Outwater|first1=Eric K.|last2=Siegelman|first2=Evan S.|last3=Hunt|first3=Jennifer L.|title=Ovarian Teratomas: Tumor Types and Imaging Characteristics|journal=RadioGraphics|volume=21|issue=2|year=2001|pages=475–490|issn=0271-5333|doi=10.1148/radiographics.21.2.g01mr09475}}</ref> | * Usually appear larger than mature [[Teratoma|teratomas]]<ref name="OutwaterSiegelman2001">{{cite journal|last1=Outwater|first1=Eric K.|last2=Siegelman|first2=Evan S.|last3=Hunt|first3=Jennifer L.|title=Ovarian Teratomas: Tumor Types and Imaging Characteristics|journal=RadioGraphics|volume=21|issue=2|year=2001|pages=475–490|issn=0271-5333|doi=10.1148/radiographics.21.2.g01mr09475}}</ref> | ||
* May be solid or with a prominent solid element | * May be [[solid]] or with a prominent [[solid]] element | ||
* Cystic cavities may be filled with serous or mucinous or fatty-sebaceous | * [[Cystic]] [[cavities]] may be filled with [[serous]] or [[mucinous]] or fatty-[[sebaceous]] fluid. | ||
* | * The [[Capsule|capsular]] component may not always be well-defined | ||
'''Teratoma-monodermal''' | '''Teratoma-monodermal''' | ||
* Struma ovarii: amber-colored thyroid tissue with areas of hemorrhage, necrosis, and fibrosis <ref name="OutwaterSiegelman2001">{{cite journal|last1=Outwater|first1=Eric K.|last2=Siegelman|first2=Evan S.|last3=Hunt|first3=Jennifer L.|title=Ovarian Teratomas: Tumor Types and Imaging Characteristics|journal=RadioGraphics|volume=21|issue=2|year=2001|pages=475–490|issn=0271-5333|doi=10.1148/radiographics.21.2.g01mr09475}}</ref> | * [[Struma ovarii]]: amber-colored [[thyroid]] [[tissue]] with areas of [[hemorrhage]], [[necrosis]], and [[fibrosis]] <ref name="OutwaterSiegelman2001">{{cite journal|last1=Outwater|first1=Eric K.|last2=Siegelman|first2=Evan S.|last3=Hunt|first3=Jennifer L.|title=Ovarian Teratomas: Tumor Types and Imaging Characteristics|journal=RadioGraphics|volume=21|issue=2|year=2001|pages=475–490|issn=0271-5333|doi=10.1148/radiographics.21.2.g01mr09475}}</ref> | ||
* Carcinoid tumor: a solid mass | * [[Carcinoid tumors|Carcinoid tumor]]: a [[solid]] [[mass]] | ||
|- | |- | ||
|} | |} | ||
==Microscopic Pathology== | ==Microscopic Pathology== | ||
{| {{table}} | {| {{table}} cellpadding="4" cellspacing="0" style="border:#c9c9c9 1px solid; margin: 1em 1em 1em 0; border-collapse: collapse;" | ||
| align="center" style="background: #4479BA;" | {{fontcolor|#FFF|''' Ovarian germ cell tumor subtype'''}} | | align="center" style="background: #4479BA;" | {{fontcolor|#FFF|''' Ovarian germ cell tumor subtype'''}} | ||
| align="center" style="background: #4479BA;" | {{fontcolor|#FFF|'''Features on Histopathological Microscopic Analysis'''}} | | align="center" style="background: #4479BA;" | {{fontcolor|#FFF|'''Features on Histopathological Microscopic Analysis'''}} | ||
| Line 126: | Line 137: | ||
|- | |- | ||
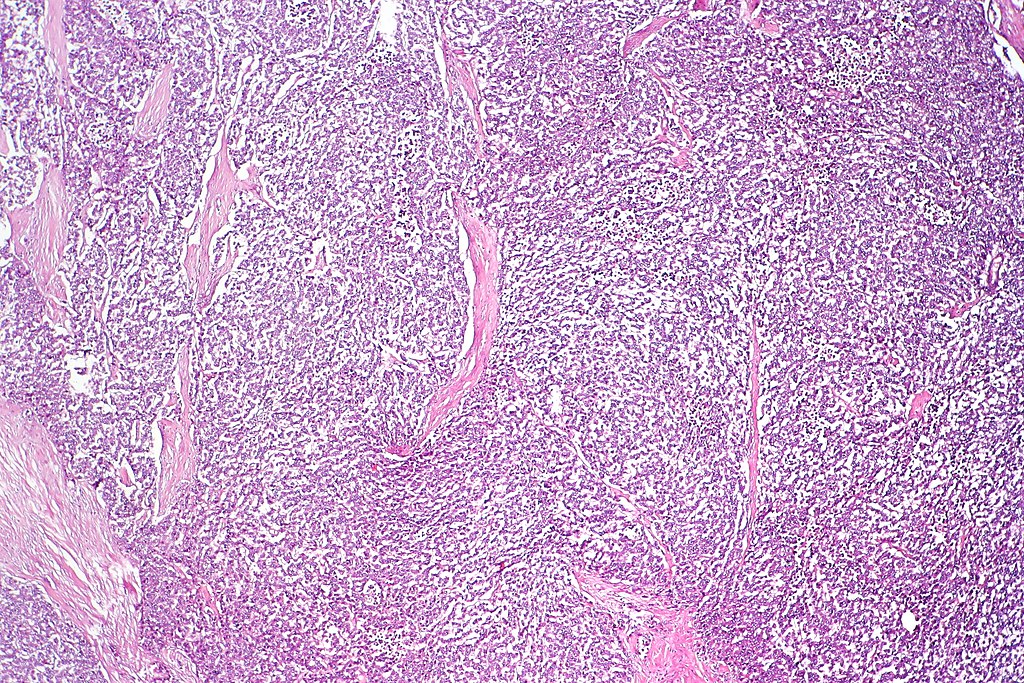
|''' Dysgerminomas'''|| | |''' Dysgerminomas'''|| | ||
* large, uniform, clear cells arranged in sheets <ref name="ShaabanRezvani2014">{{cite journal|last1=Shaaban|first1=Akram M.|last2=Rezvani|first2=Maryam|last3=Elsayes|first3=Khaled M.|last4=Baskin|first4=Henry|last5=Mourad|first5=Amr|last6=Foster|first6=Bryan R.|last7=Jarboe|first7=Elke A.|last8=Menias|first8=Christine O.|title=Ovarian Malignant Germ Cell Tumors: Cellular Classification and Clinical and Imaging Features|journal=RadioGraphics|volume=34|issue=3|year=2014|pages=777–801|issn=0271-5333|doi=10.1148/rg.343130067}}</ref> | * large, uniform, clear [[cells]] arranged in sheets <ref name="ShaabanRezvani2014">{{cite journal|last1=Shaaban|first1=Akram M.|last2=Rezvani|first2=Maryam|last3=Elsayes|first3=Khaled M.|last4=Baskin|first4=Henry|last5=Mourad|first5=Amr|last6=Foster|first6=Bryan R.|last7=Jarboe|first7=Elke A.|last8=Menias|first8=Christine O.|title=Ovarian Malignant Germ Cell Tumors: Cellular Classification and Clinical and Imaging Features|journal=RadioGraphics|volume=34|issue=3|year=2014|pages=777–801|issn=0271-5333|doi=10.1148/rg.343130067}}</ref> | ||
* Uniform cells has an "fried egg appearance"(large cytoplasm and small nucleus) that resemble primordial germ cells | * Uniform [[cells]] has an "fried egg [[appearance]]"(large [[cytoplasm]] and small [[nucleus]]) that resemble [[primordial germ cells]] | ||
* The stroma contains lymphocytes and septa like components. | * The [[stroma]] contains [[lymphocytes]] and [[septa]] like components. | ||
| [[File:Dysgerminoma. | | [[File:Dysgerminoma of the ovary.jpeg|thumb|none|400px|Contributed by CoRus13 in wikimedia.commons]] | ||
|- | |- | ||
|''' Embryonal carcinoma'''|| | |''' Embryonal carcinoma'''|| | ||
* Pseudoglandular pattern of | * Pseudoglandular pattern of [[Primitive (integral)|primitive]] [[cells]] <ref name="ShaabanRezvani2014">{{cite journal|last1=Shaaban|first1=Akram M.|last2=Rezvani|first2=Maryam|last3=Elsayes|first3=Khaled M.|last4=Baskin|first4=Henry|last5=Mourad|first5=Amr|last6=Foster|first6=Bryan R.|last7=Jarboe|first7=Elke A.|last8=Menias|first8=Christine O.|title=Ovarian Malignant Germ Cell Tumors: Cellular Classification and Clinical and Imaging Features|journal=RadioGraphics|volume=34|issue=3|year=2014|pages=777–801|issn=0271-5333|doi=10.1148/rg.343130067}}</ref> | ||
* Nuclei are: | * [[Nuclei]] are: | ||
** Large | ** Large | ||
** Croweded | ** Croweded | ||
** Pleomorphic | ** Pleomorphic | ||
** With prominent nucleoli | ** With prominent [[nucleoli]] | ||
| [[Image:800px-Embryonal_carcinoma_-_high_mag.jpg|300px|thumb|none| Embryonal carcinoma]] | | [[Image:800px-Embryonal_carcinoma_-_high_mag.jpg|300px|thumb|none| Contributed by Nephron in wikimedia.commons]] | ||
|- | |||
|'''Endodermal sinus tumor or yolk sac tumors'''|| | |||
* Schiller-Duval bodies (resemble renal [[glomeruli]]) - key feature <ref name="ShaabanRezvani2014">{{cite journal|last1=Shaaban|first1=Akram M.|last2=Rezvani|first2=Maryam|last3=Elsayes|first3=Khaled M.|last4=Baskin|first4=Henry|last5=Mourad|first5=Amr|last6=Foster|first6=Bryan R.|last7=Jarboe|first7=Elke A.|last8=Menias|first8=Christine O.|title=Ovarian Malignant Germ Cell Tumors: Cellular Classification and Clinical and Imaging Features|journal=RadioGraphics|volume=34|issue=3|year=2014|pages=777–801|issn=0271-5333|doi=10.1148/rg.343130067}}</ref> | |||
| [[Image:800px-Mixed_germ_cell_tumour_-_high_mag.jpg|thumb|none|300px|Micrograph showing the yolk sac component of a mixed germ cell tumor. Contributed by Nephrone in wikimedia.commons]] | |||
|- | |||
|'''Polyemryoma'''|| | |||
* Usually as a part of mixed [[germ cell]] [[tumor]]<ref name="ShaabanRezvani2014">{{cite journal|last1=Shaaban|first1=Akram M.|last2=Rezvani|first2=Maryam|last3=Elsayes|first3=Khaled M.|last4=Baskin|first4=Henry|last5=Mourad|first5=Amr|last6=Foster|first6=Bryan R.|last7=Jarboe|first7=Elke A.|last8=Menias|first8=Christine O.|title=Ovarian Malignant Germ Cell Tumors: Cellular Classification and Clinical and Imaging Features|journal=RadioGraphics|volume=34|issue=3|year=2014|pages=777–801|issn=0271-5333|doi=10.1148/rg.343130067}}</ref> | |||
* Contains small [[embryo]]-like bodies with central germ disks | |||
* Germ disk [[cavity]] has two part: | |||
** Embryonal carcinoma [[epithelia]] | |||
** Two cavities: | |||
*** [[Dorsal cavity]] that resembles the [[amniotic cavity]] | |||
*** [[Ventral cavity]] that resembles the [[yolk sac]] cavity | |||
| [[Image:TestispolyembryomaPerez37n.jpg|thumb|none|300px|Micrograph showing the embryoma component of a mixed germ cell tumor. Attributed by "courtesy of PathologyOutlines.com"]] | |||
|- | |- | ||
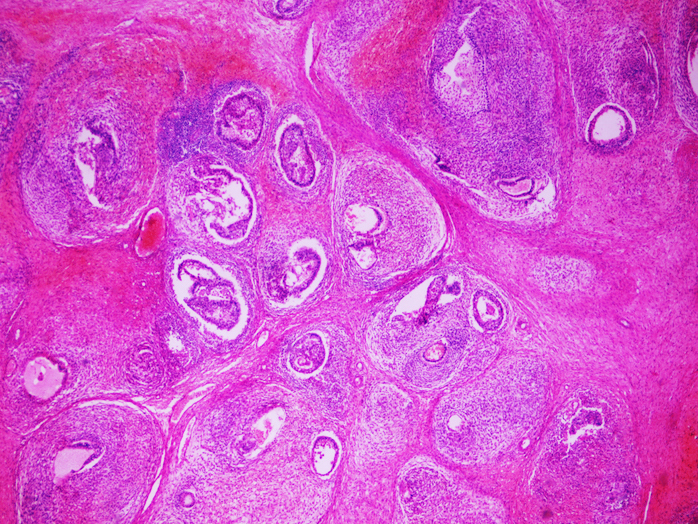
|'''Teratoma'''|| | |'''Teratoma'''|| | ||
'''Mature teratoma''' | '''Mature teratoma''' | ||
* The sections show ovarian parenchyma with a lesion consisting of benign dermal, gastrointestinal, and neural elements.<ref name= wpp>Mature teratoma. http://librepathology.org/wiki/index.php/Teratoma#Mature_teratoma. URL Accessed on November 12, 2015</ref> | * The sections show [[ovarian]] [[parenchyma]] with a [[lesion]] consisting of [[benign]] [[dermal]], [[gastrointestinal]], and [[neural]] elements.<ref name="wpp">Mature teratoma. http://librepathology.org/wiki/index.php/Teratoma#Mature_teratoma. URL Accessed on November 12, 2015</ref> | ||
* The neural elements show focal degenerative changes with macrophages and giant cells | * The [[neural]] elements show focal [[degenerative]] changes with [[macrophages]] and [[giant cells]] | ||
* Siderophages are present. | * Siderophages are present. | ||
* In general, mature teratoma usually appears as a well-established organization of tissues mimicking the relationship observed in normal organs such as:<ref name="pmid15761467">{{cite journal |vauthors=Ulbright TM |title=Germ cell tumors of the gonads: a selective review emphasizing problems in differential diagnosis, newly appreciated, and controversial issues |journal=Mod. Pathol. |volume=18 Suppl 2 |issue= |pages=S61–79 |date=February 2005 |pmid=15761467 |doi=10.1038/modpathol.3800310 |url=}}</ref> | * In general, mature [[teratoma]] usually appears as a well-established organization of [[tissues]] mimicking the relationship observed in normal organs such as:<ref name="pmid15761467">{{cite journal |vauthors=Ulbright TM |title=Germ cell tumors of the gonads: a selective review emphasizing problems in differential diagnosis, newly appreciated, and controversial issues |journal=Mod. Pathol. |volume=18 Suppl 2 |issue= |pages=S61–79 |date=February 2005 |pmid=15761467 |doi=10.1038/modpathol.3800310 |url=}}</ref> | ||
** respiratory epithelial layer surrounded by smooth muscle and cartilage | ** [[Respiratory epithelium|respiratory epithelial]] layer surrounded by [[smooth muscle]] and [[cartilage]] | ||
* Usually, there is scant mitosis in the tumor cells usually limited to the normal proliferative zone of the body part that they produce. | * Usually, there is scant [[mitosis]] in the [[Tumor cell|tumor cells]] usually limited to the normal proliferative zone of the body part that they produce. | ||
* No cytologic atypia is present. | * No [[Cytological|cytologic]] [[atypia]] is present. | ||
* Different type of tissues may be observed in the mature teratomas of the ovary such as: | * Different type of tissues may be observed in the mature [[Teratoma|teratomas]] of the ovary such as: | ||
**Choroid plexus | **[[Choroid plexus]] | ||
**Thyroid tissues | **[[Thyroid]] tissues | ||
**Pituitary tissues, although not commonly.<ref name="KallenbergPesce1991">{{cite journal|last1=Kallenberg|first1=GA|last2=Pesce|first2=CM|last3=Norman|first3=B|last4=Ratner|first4=RE|last5=Silverberg|first5=SG|title=Ectopic hyperprolactinemia resulting from an ovarian teratoma|journal=International Journal of Gynecology & Obstetrics|volume=34|issue=2|year=1991|pages=194–195|issn=00207292|doi=10.1016/0020-7292(91)90266-8}}</ref> | **[[Pituitary]] tissues, although not commonly.<ref name="KallenbergPesce1991">{{cite journal|last1=Kallenberg|first1=GA|last2=Pesce|first2=CM|last3=Norman|first3=B|last4=Ratner|first4=RE|last5=Silverberg|first5=SG|title=Ectopic hyperprolactinemia resulting from an ovarian teratoma|journal=International Journal of Gynecology & Obstetrics|volume=34|issue=2|year=1991|pages=194–195|issn=00207292|doi=10.1016/0020-7292(91)90266-8}}</ref> | ||
***Rarely, they produce prolactin and is associated with prolactinoma. | ***Rarely, they produce [[prolactin]] and is associated with [[prolactinoma]]. | ||
'''Immature teratoma''' | '''Immature teratoma''' | ||
* Tissues originating from the two or three | * [[Tissues]] originating from the two or three embryonal layers are present.<ref name="ShaabanRezvani2014">{{cite journal|last1=Shaaban|first1=Akram M.|last2=Rezvani|first2=Maryam|last3=Elsayes|first3=Khaled M.|last4=Baskin|first4=Henry|last5=Mourad|first5=Amr|last6=Foster|first6=Bryan R.|last7=Jarboe|first7=Elke A.|last8=Menias|first8=Christine O.|title=Ovarian Malignant Germ Cell Tumors: Cellular Classification and Clinical and Imaging Features|journal=RadioGraphics|volume=34|issue=3|year=2014|pages=777–801|issn=0271-5333|doi=10.1148/rg.343130067}}</ref> | ||
* There is a mixture of mature and immature tissue (primitive cells). | * There is a mixture of mature and immature [[tissue]] (primitive cells). | ||
* The presence of primitive elements is necessary to make the diagnosis. | * The presence of primitive elements is necessary to make the [[diagnosis]]. | ||
|[[File:Teratoma.jpg|thumb|none|300px| | |[[File:Mature Cystic Teratoma of the Ovary Bone Tissue (4047143950).jpg|thumb|none|300px|Mature cystic teratoma of the ovary: Bone Tissue | ||
Pathological and histological images courtesy of Ed Uthman at flickr. Contributed by wikimedia commons]] | |||
|- | |- | ||
|} | |} | ||
==Immunohistochemistry== | ==Immunohistochemistry== | ||
===Dysgerminoma=== | |||
* [[Dysgerminoma]] is positive for:<ref name="PectasidesPectasides2008">{{cite journal|last1=Pectasides|first1=D.|last2=Pectasides|first2=E.|last3=Kassanos|first3=D.|title=Germ cell tumors of the ovary|journal=Cancer Treatment Reviews|volume=34|issue=5|year=2008|pages=427–441|issn=03057372|doi=10.1016/j.ctrv.2008.02.002}}</ref> | |||
** OCT4 (this [[marker]] is a key [[diagnostic]] factor for the [[diagnosis]] of dysgerminoma) | |||
===Embryonal carcinoma=== | |||
*These [[Tumor|tumors]] are positive for:<ref name="ShaabanRezvani2014">{{cite journal|last1=Shaaban|first1=Akram M.|last2=Rezvani|first2=Maryam|last3=Elsayes|first3=Khaled M.|last4=Baskin|first4=Henry|last5=Mourad|first5=Amr|last6=Foster|first6=Bryan R.|last7=Jarboe|first7=Elke A.|last8=Menias|first8=Christine O.|title=Ovarian Malignant Germ Cell Tumors: Cellular Classification and Clinical and Imaging Features|journal=RadioGraphics|volume=34|issue=3|year=2014|pages=777–801|issn=0271-5333|doi=10.1148/rg.343130067}}</ref> | |||
** [[CD30]] | |||
** EMA | |||
** OCT3/4 | |||
===Endodermal sinus tumor=== | |||
* [[Yolk sac tumor|Yolk sac tumors]] are positive for:<ref name="PectasidesPectasides2008">{{cite journal|last1=Pectasides|first1=D.|last2=Pectasides|first2=E.|last3=Kassanos|first3=D.|title=Germ cell tumors of the ovary|journal=Cancer Treatment Reviews|volume=34|issue=5|year=2008|pages=427–441|issn=03057372|doi=10.1016/j.ctrv.2008.02.002}}</ref><ref name="CaoGuo2009">{{cite journal|last1=Cao|first1=Dengfeng|last2=Guo|first2=Shuangping|last3=Allan|first3=Robert W.|last4=Molberg|first4=Kyle H.|last5=Peng|first5=Yan|title=SALL4 Is a Novel Sensitive and Specific Marker of Ovarian Primitive Germ Cell Tumors and Is Particularly Useful in Distinguishing Yolk Sac Tumor From Clear Cell Carcinoma|journal=The American Journal of Surgical Pathology|volume=33|issue=6|year=2009|pages=894–904|issn=0147-5185|doi=10.1097/PAS.0b013e318198177d}}</ref> | |||
** [[AFP]] | |||
*** Absence of [[AFP]] does not exclude the [[diagnosis]]. | |||
** [[Cytokeratin]] (AE1/AE3) | |||
** Placental-like [[alkaline phosphatase]] in 50% of the individuals. | |||
** SALL4 ([[nuclear]]) in > 90% of the cases. | |||
** GPC3 | |||
===Non-gestational chriocarcinoma=== | |||
*These [[tumors]] [[stain]] for [[keratins]] strongly.<ref name="pmid12548163">{{cite journal |vauthors=Ordi J, Romagosa C, Tavassoli FA, Nogales F, Palacin A, Condom E, Torné A, Cardesa A |title=CD10 expression in epithelial tissues and tumors of the gynecologic tract: a useful marker in the diagnosis of mesonephric, trophoblastic, and clear cell tumors |journal=Am. J. Surg. Pathol. |volume=27 |issue=2 |pages=178–86 |date=February 2003 |pmid=12548163 |doi= |url=}}</ref> | |||
** AE1 | |||
** AE3 | |||
** CAM5 | |||
*[[Trophoblastic]] [[cells]] are positive for [[CD10]]. | |||
*[[Tumor]] may be positive for: | |||
** GATA3 ([[nuclear]]) in 80% of the cases<ref name="BanetGown2015">{{cite journal|last1=Banet|first1=Natalie|last2=Gown|first2=Allen M.|last3=Shih|first3=Ie-Ming|last4=Kay Li|first4=Qing|last5=Roden|first5=Richard B.S.|last6=Nucci|first6=Marisa R.|last7=Cheng|first7=Liang|last8=Przybycin|first8=Christopher G.|last9=Nasseri-Nik|first9=Niloofar|last10=Wu|first10=Lee-Shu-Fune|last11=Netto|first11=George J.|last12=Ronnett|first12=Brigitte M.|last13=Vang|first13=Russell|title=GATA-3 Expression in Trophoblastic Tissues|journal=The American Journal of Surgical Pathology|volume=39|issue=1|year=2015|pages=101–108|issn=0147-5185|doi=10.1097/PAS.0000000000000315}}</ref> | |||
** SALL4 ([[nuclear]]) in 70% of the cases<ref name="MiettinenWang2014">{{cite journal|last1=Miettinen|first1=Markku|last2=Wang|first2=Zengfeng|last3=McCue|first3=Peter A.|last4=Sarlomo-Rikala|first4=Maarit|last5=Rys|first5=Janusz|last6=Biernat|first6=Wojciech|last7=Lasota|first7=Jerzy|last8=Lee|first8=Yi-Shan|title=SALL4 Expression in Germ Cell and Non–Germ Cell Tumors|journal=The American Journal of Surgical Pathology|volume=38|issue=3|year=2014|pages=410–420|issn=0147-5185|doi=10.1097/PAS.0000000000000116}}</ref> | |||
** PLAP and EMA in 50% of the cases<ref name="pmid2457424">{{cite journal |vauthors=Niehans GA, Manivel JC, Copland GT, Scheithauer BW, Wick MR |title=Immunohistochemistry of germ cell and trophoblastic neoplasms |journal=Cancer |volume=62 |issue=6 |pages=1113–23 |date=September 1988 |pmid=2457424 |doi= |url=}}</ref> | |||
===Polyembryoma=== | |||
* [[Embryoid body]] of the [[tumor]] may be positive for Glypican3.<ref name="PredaNicolae2011">{{cite journal|last1=Preda|first1=Ovidiu|last2=Nicolae|first2=Alina|last3=Aneiros-Fernández|first3=José|last4=Borda|first4=Angela|last5=Nogales|first5=Francisco F|title=Glypican 3 is a sensitive, but not a specific, marker for the diagnosis of yolk sac tumours|journal=Histopathology|volume=58|issue=2|year=2011|pages=312–314|issn=03090167|doi=10.1111/j.1365-2559.2010.03735.x}}</ref> | |||
===Teratoma=== | ===Teratoma=== | ||
* Usually, teratomas are diagnosed histologically and routine use of immunohistochemistry is not needed. However it may be needed in the diagnosis of immature and monodermal types. | * Usually, [[Teratoma|teratomas]] are [[Diagnose|diagnosed]] [[histologically]] and routine use of [[immunohistochemistry]] is not needed. However it may be needed in the [[diagnosis]] of immature and monodermal types. | ||
* Neuronal elements of mature or immature teratomas are | * [[Neuronal]] elements of mature or immature [[Teratoma|teratomas]] are positive for:<ref name="TakayamaMatsumura2015">{{cite journal|last1=Takayama|first1=Yoshiyasu|last2=Matsumura|first2=Nozomi|last3=Nobusawa|first3=Sumihito|last4=Ikota|first4=Hayato|last5=Minegishi|first5=Takashi|last6=Yokoo|first6=Hideaki|title=Immunophenotypic features of immaturity of neural elements in ovarian teratoma|journal=Virchows Archiv|volume=468|issue=3|year=2015|pages=337–343|issn=0945-6317|doi=10.1007/s00428-015-1891-8}}</ref> | ||
** Glial fibrillary acidic protein (GFAP) | ** [[Glial fibrillary acidic protein]] (GFAP) | ||
** neuron specific enolase (NSE) | ** neuron specific enolase (NSE) | ||
** S-100 | ** [[S-100 protein|S-100]] | ||
* Monodermal teratoma<ref name="OutwaterSiegelman2001">{{cite journal|last1=Outwater|first1=Eric K.|last2=Siegelman|first2=Evan S.|last3=Hunt|first3=Jennifer L.|title=Ovarian Teratomas: Tumor Types and Imaging Characteristics|journal=RadioGraphics|volume=21|issue=2|year=2001|pages=475–490|issn=0271-5333|doi=10.1148/radiographics.21.2.g01mr09475}}</ref> | * Monodermal [[teratoma]]<ref name="OutwaterSiegelman2001">{{cite journal|last1=Outwater|first1=Eric K.|last2=Siegelman|first2=Evan S.|last3=Hunt|first3=Jennifer L.|title=Ovarian Teratomas: Tumor Types and Imaging Characteristics|journal=RadioGraphics|volume=21|issue=2|year=2001|pages=475–490|issn=0271-5333|doi=10.1148/radiographics.21.2.g01mr09475}}</ref> | ||
** | ** [[Carcinoid tumors|Carcinoid tumor]] may be positive for [[serotonin]] and [[hormonal]] [[peptides]]. | ||
==References== | ==References== | ||
Latest revision as of 17:20, 26 March 2019
|
Ovarian germ cell tumor Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Ovarian germ cell tumor pathophysiology On the Web |
|
American Roentgen Ray Society Images of Ovarian germ cell tumor pathophysiology |
|
Risk calculators and risk factors for Ovarian germ cell tumor pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sahar Memar Montazerin, M.D.[2] Monalisa Dmello, M.B,B.S., M.D. [3]
Overveiw
The pathophysiology of ovarian germ cell tumors depends on the histological subtype. However, their origin is the primordial germ cells that transformed pathologically in different stages of development.
Pathophysiology
Pathogenesis
- It is understood that ovarian germ cell tumors are the result of the pathologic transformation of primordial germ cells during different stages of the development.[1][2]
| Germ cell | |||||||||||||||||||||||||||||||||||||||
| Pathogenesis | Malignant transformation | ||||||||||||||||||||||||||||||||||||||
| Mature teratoma | |||||||||||||||||||||||||||||||||||||||
| Tumors esxpressing transcription factors of pluripotency | Tumors with primitive embryonic ectoderm, mesoderm, and/or endoderm differentiation | Tumors with extraembroyonic differentiation | |||||||||||||||||||||||||||||||||||||
| Dysgerminoma/Embryonal carcinoma | Immature teratoma | Yolk sac tumor/Choriocarcinoma | |||||||||||||||||||||||||||||||||||||
Mature teratoma
- Mature teratomas are benign tumors originating from pathologic development of primordial germ cells.[3]
- It originates from a single germ cell tumor after the first phase of meiosis.[4]
- These tumors contain the well-differentiated component of three germ layers.[3]
- Their usual location is the embryonic fusion line overhead and neck, mediastinum, a and presacral area and tend to present at a greater extent in the midline.
Dysgerminoma
- Dysgerminoma arises from primordial germ cells, which are gonadal cells that are normally involved in the gametogenesis.[1]
- The majority of dysgerminomas in women present in the stage 1A.[5]
- Bilateral invovlement occurs in 10% to 15% of the cases.
- In < 15% of the affected cases, elements of other germ cell tumors can also be found.[6]
Yolk sac tumor
- These tumors develop from differentiation of primitive germ cells in the direction of yolk sac or vitelline structures.[7]
- They tend to grow very rapidly.[8]
- Bilateral involvement occurs in less than 5% of the cases.
- In 10% of the cases, the contralateral ovary carries a dermoid cyst.
- In 40% of cases, they are accompanied by other types of germ cell tumors.[9]
Genetics
- Ovarian germ cell tumors may be associated with cytogenetic abnormalities.
- Immature teratomas may be associated with chromosomal changes such as:[10]
- Gain of all or parts of
- 1p
- 16p
- 19
- 22q
- Gain of all or parts of
- Dysgerminomas may be associated with gain or loss of complete or partial chromosomal materials such as:[10]
- Gain of:
- 1p
- 6p
- 12p
- 12q
- 15q
- 20q
- 21q
- 22q
- Whole of chromosome 7
- Whole of chromosome 8
- Whole of chromosome 17
- Whole of chromosome 19
- Losses from 13q
- Gain of:
- Yolk sac tumor is associated with gaining of the 12p chromosome in 75% of the cases.[10]
- It may also be associated with chromosomal changes such as:
- Gain of 1q
- It may also be associated with chromosomal changes such as:
Associated Conditions
Conditions associated with mature teratoma include:
- Anti-NMDA receptor encephalitis (although very rarely)[11]
- Rarely, they contain pituitary cells capable of prolactin production and is associated with prolactinoma.[12]
Polyembryoma may be associated with Klinefelter syndrome.[13]
Gross Pathology
| Ovarian germ cell tumor subtype | Features on Gross Pathology |
| Dysgerminonma | |
| Embryonal Carcinoma |
|
| Endodermal sinus tumor or yolk sac tumors | |
| Mixed germ cell tumors | |
| Polyembryoma |
|
| Teratoma |
Teratoma-mature
Teratoma-immature
Teratoma-monodermal
|
Microscopic Pathology
| Ovarian germ cell tumor subtype | Features on Histopathological Microscopic Analysis | Image |
| Dysgerminomas |
|
 |
| Embryonal carcinoma | 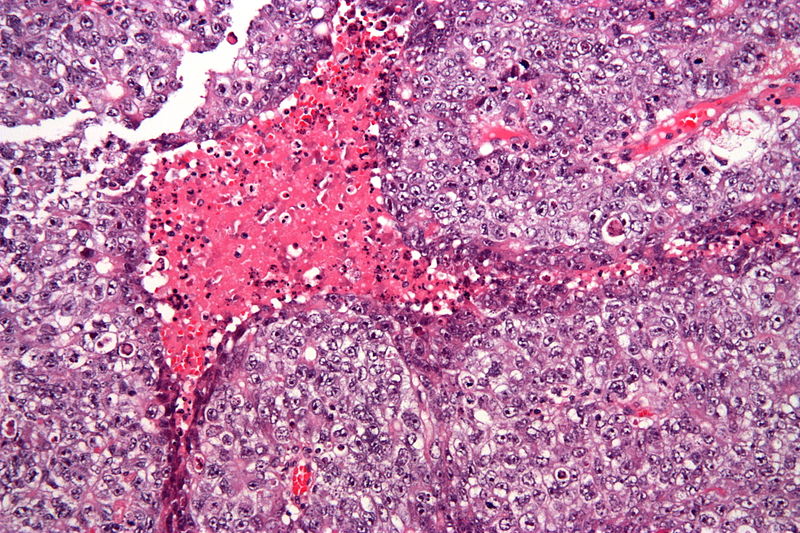 | |
| Endodermal sinus tumor or yolk sac tumors |  | |
| Polyemryoma |
|
 |
| Teratoma |
Mature teratoma
Immature teratoma |
 |
Immunohistochemistry
Dysgerminoma
- Dysgerminoma is positive for:[20]
- OCT4 (this marker is a key diagnostic factor for the diagnosis of dysgerminoma)
Embryonal carcinoma
Endodermal sinus tumor
- Yolk sac tumors are positive for:[20][21]
- AFP
- Cytokeratin (AE1/AE3)
- Placental-like alkaline phosphatase in 50% of the individuals.
- SALL4 (nuclear) in > 90% of the cases.
- GPC3
Non-gestational chriocarcinoma
- These tumors stain for keratins strongly.[22]
- AE1
- AE3
- CAM5
- Trophoblastic cells are positive for CD10.
- Tumor may be positive for:
Polyembryoma
- Embryoid body of the tumor may be positive for Glypican3.[26]
Teratoma
- Usually, teratomas are diagnosed histologically and routine use of immunohistochemistry is not needed. However it may be needed in the diagnosis of immature and monodermal types.
- Neuronal elements of mature or immature teratomas are positive for:[27]
- Glial fibrillary acidic protein (GFAP)
- neuron specific enolase (NSE)
- S-100
- Monodermal teratoma[17]
- Carcinoid tumor may be positive for serotonin and hormonal peptides.
References
- ↑ 1.0 1.1 El-Maarri, Osman; Rijlaarsdam, Martin A.; Tax, David M. J.; Gillis, Ad J. M.; Dorssers, Lambert C. J.; Koestler, Devin C.; de Ridder, Jeroen; Looijenga, Leendert H. J. (2015). "Genome Wide DNA Methylation Profiles Provide Clues to the Origin and Pathogenesis of Germ Cell Tumors". PLOS ONE. 10 (4): e0122146. doi:10.1371/journal.pone.0122146. ISSN 1932-6203.
- ↑ Carcangiu, M. L. (2014). WHO Classification of Tumours of Female Reproductive Organs. Lyon: International Agency for Research on Cancer. ISBN 978-92-832-4487-5.
- ↑ 3.0 3.1 Vural, F.; Vural, B.; Paksoy, N. (2015). "Vaginal teratoma: A case report and review of the literature". Journal of Obstetrics and Gynaecology. 35 (7): 757–758. doi:10.3109/01443615.2015.1004525. ISSN 0144-3615.
- ↑ Linder, David; McCaw, Barbara Kaiser; Hecht, Frederick (1975). "Parthenogenic Origin of Benign Ovarian Teratomas". New England Journal of Medicine. 292 (2): 63–66. doi:10.1056/NEJM197501092920202. ISSN 0028-4793.
- ↑ AL Husaini, Hamed; Soudy, Hussein; Darwish, Alaa El Din; Ahmed, Mohamed; Eltigani, Amin; AL Mubarak, Mustafa; Sabaa, Amal Abu; Edesa, Wael; AL-Tweigeri, Taher; Al-Badawi, Ismail A. (2012). "Pure dysgerminoma of the ovary: a single institutional experience of 65 patients". Medical Oncology. 29 (4): 2944–2948. doi:10.1007/s12032-012-0194-z. ISSN 1357-0560.
- ↑ Gordon A, Lipton D, Woodruff JD (October 1981). "Dysgerminoma: a review of 158 cases from the Emil Novak Ovarian Tumor Registry". Obstet Gynecol. 58 (4): 497–504. PMID 7279343.
- ↑ Young, Robert H. (2014). "The Yolk Sac Tumor". International Journal of Surgical Pathology. 22 (8): 677–687. doi:10.1177/1066896914558265. ISSN 1066-8969.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 8.7 8.8 8.9 Shaaban, Akram M.; Rezvani, Maryam; Elsayes, Khaled M.; Baskin, Henry; Mourad, Amr; Foster, Bryan R.; Jarboe, Elke A.; Menias, Christine O. (2014). "Ovarian Malignant Germ Cell Tumors: Cellular Classification and Clinical and Imaging Features". RadioGraphics. 34 (3): 777–801. doi:10.1148/rg.343130067. ISSN 0271-5333.
- ↑ 9.0 9.1 Kojimahara, Takanobu; Nakahara, Kenji; Takano, Tadao; Yaegashi, Nobuo; Nishiyama, Hiroshi; Fujimori, Keiya; Sato, Naoki; Terada, Yukihiro; Tase, Toru; Yokoyama, Yoshihito; Mizunuma, Hideki; Shoji, Tadahiro; Sugiyama, Toru; Kurachi, Hirohisa (2013). "Yolk Sac Tumor of the Ovary: A Retrospective Multicenter Study of 33 Japanese Women by Tohoku Gynecologic Cancer Unit (TGCU)". The Tohoku Journal of Experimental Medicine. 230 (4): 211–217. doi:10.1620/tjem.230.211. ISSN 1349-3329.
- ↑ 10.0 10.1 10.2 Kraggerud SM, Szymanska J, Abeler VM, Kaern J, Eknaes M, Heim S, Teixeira MR, Tropé CG, Peltomäki P, Lothe RA (June 2000). "DNA copy number changes in malignant ovarian germ cell tumors". Cancer Res. 60 (11): 3025–30. PMID 10850452.
- ↑ Dalmau, Josep; Gleichman, Amy J; Hughes, Ethan G; Rossi, Jeffrey E; Peng, Xiaoyu; Lai, Meizan; Dessain, Scott K; Rosenfeld, Myrna R; Balice-Gordon, Rita; Lynch, David R (2008). "Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies". The Lancet Neurology. 7 (12): 1091–1098. doi:10.1016/S1474-4422(08)70224-2. ISSN 1474-4422.
- ↑ 12.0 12.1 Kallenberg, GA; Pesce, CM; Norman, B; Ratner, RE; Silverberg, SG (1991). "Ectopic hyperprolactinemia resulting from an ovarian teratoma". International Journal of Gynecology & Obstetrics. 34 (2): 194–195. doi:10.1016/0020-7292(91)90266-8. ISSN 0020-7292.
- ↑ Beresford L, Fernandez CV, Cummings E, Sanderson S, Ming-Yu W, Giacomantonio M (April 2003). "Mediastinal polyembryoma associated with Klinefelter syndrome". J. Pediatr. Hematol. Oncol. 25 (4): 321–3. PMID 12679648.
- ↑ Chen VW, Ruiz B, Killeen JL, Coté TR, Wu XC, Correa CN (May 2003). "Pathology and classification of ovarian tumors". Cancer. 97 (10 Suppl): 2631–42. doi:10.1002/cncr.11345. PMID 12733128.
- ↑ Oliva, Esther; Young, Robert H. (2014). "Germ cell tumours of the ovary: selected topics". Diagnostic Histopathology. 20 (9): 364–375. doi:10.1016/j.mpdhp.2014.07.003. ISSN 1756-2317.
- ↑ Yayla Abide, Çiğdem; Bostancı Ergen, Evrim (2018). "Retrospective analysis of mature cystic teratomas in a single center and review of the literature". Journal of Turkish Society of Obstetric and Gynecology. 15 (2): 95–98. doi:10.4274/tjod.86244. ISSN 1307-699X.
- ↑ 17.0 17.1 17.2 Outwater, Eric K.; Siegelman, Evan S.; Hunt, Jennifer L. (2001). "Ovarian Teratomas: Tumor Types and Imaging Characteristics". RadioGraphics. 21 (2): 475–490. doi:10.1148/radiographics.21.2.g01mr09475. ISSN 0271-5333.
- ↑ Mature teratoma. http://librepathology.org/wiki/index.php/Teratoma#Mature_teratoma. URL Accessed on November 12, 2015
- ↑ Ulbright TM (February 2005). "Germ cell tumors of the gonads: a selective review emphasizing problems in differential diagnosis, newly appreciated, and controversial issues". Mod. Pathol. 18 Suppl 2: S61–79. doi:10.1038/modpathol.3800310. PMID 15761467.
- ↑ 20.0 20.1 Pectasides, D.; Pectasides, E.; Kassanos, D. (2008). "Germ cell tumors of the ovary". Cancer Treatment Reviews. 34 (5): 427–441. doi:10.1016/j.ctrv.2008.02.002. ISSN 0305-7372.
- ↑ Cao, Dengfeng; Guo, Shuangping; Allan, Robert W.; Molberg, Kyle H.; Peng, Yan (2009). "SALL4 Is a Novel Sensitive and Specific Marker of Ovarian Primitive Germ Cell Tumors and Is Particularly Useful in Distinguishing Yolk Sac Tumor From Clear Cell Carcinoma". The American Journal of Surgical Pathology. 33 (6): 894–904. doi:10.1097/PAS.0b013e318198177d. ISSN 0147-5185.
- ↑ Ordi J, Romagosa C, Tavassoli FA, Nogales F, Palacin A, Condom E, Torné A, Cardesa A (February 2003). "CD10 expression in epithelial tissues and tumors of the gynecologic tract: a useful marker in the diagnosis of mesonephric, trophoblastic, and clear cell tumors". Am. J. Surg. Pathol. 27 (2): 178–86. PMID 12548163.
- ↑ Banet, Natalie; Gown, Allen M.; Shih, Ie-Ming; Kay Li, Qing; Roden, Richard B.S.; Nucci, Marisa R.; Cheng, Liang; Przybycin, Christopher G.; Nasseri-Nik, Niloofar; Wu, Lee-Shu-Fune; Netto, George J.; Ronnett, Brigitte M.; Vang, Russell (2015). "GATA-3 Expression in Trophoblastic Tissues". The American Journal of Surgical Pathology. 39 (1): 101–108. doi:10.1097/PAS.0000000000000315. ISSN 0147-5185.
- ↑ Miettinen, Markku; Wang, Zengfeng; McCue, Peter A.; Sarlomo-Rikala, Maarit; Rys, Janusz; Biernat, Wojciech; Lasota, Jerzy; Lee, Yi-Shan (2014). "SALL4 Expression in Germ Cell and Non–Germ Cell Tumors". The American Journal of Surgical Pathology. 38 (3): 410–420. doi:10.1097/PAS.0000000000000116. ISSN 0147-5185.
- ↑ Niehans GA, Manivel JC, Copland GT, Scheithauer BW, Wick MR (September 1988). "Immunohistochemistry of germ cell and trophoblastic neoplasms". Cancer. 62 (6): 1113–23. PMID 2457424.
- ↑ Preda, Ovidiu; Nicolae, Alina; Aneiros-Fernández, José; Borda, Angela; Nogales, Francisco F (2011). "Glypican 3 is a sensitive, but not a specific, marker for the diagnosis of yolk sac tumours". Histopathology. 58 (2): 312–314. doi:10.1111/j.1365-2559.2010.03735.x. ISSN 0309-0167.
- ↑ Takayama, Yoshiyasu; Matsumura, Nozomi; Nobusawa, Sumihito; Ikota, Hayato; Minegishi, Takashi; Yokoo, Hideaki (2015). "Immunophenotypic features of immaturity of neural elements in ovarian teratoma". Virchows Archiv. 468 (3): 337–343. doi:10.1007/s00428-015-1891-8. ISSN 0945-6317.