Osteopontin: Difference between revisions
m (Robot: Automated text replacement (-{{WikiDoc Cardiology Network Infobox}} +, -<references /> +{{reflist|2}}, -{{reflist}} +{{reflist|2}})) |
imported>JCW-CleanerBot m (→Role in allergy and asthma: task, replaced: Cytokine. → Cytokine) |
||
| (3 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
{{Infobox_gene}} | |||
{{ | {{Infobox protein family | ||
| | | Symbol = Osteopontin | ||
| | | Name = Osteopontin | ||
| | | image = | ||
| | | width = | ||
| | | caption = crystal structure of anti-osteopontin antibody 23c3 in complex with w43a mutated epitope peptide | ||
| Pfam = PF00865 | |||
| Pfam_clan = | |||
| InterPro = IPR002038 | |||
| SMART = | |||
| PROSITE = PDOC00689 | |||
| MEROPS = | |||
| SCOP = | |||
| TCDB = | |||
| OPM family = | |||
| OPM protein = | |||
| CAZy = | |||
| CDD = | |||
}} | }} | ||
:''Not to be confused with [[Osteocalcin]], [[Osteonectin]] or [[Osteoprotegerin|Osteoprotegerin (OPG)]].'' | |||
'''Osteopontin (OPN)''', also known as bone sialoprotein I (BSP-1 or BNSP), early T-lymphocyte activation (ETA-1), secreted phosphoprotein 1 (SPP1), 2ar and Rickettsia resistance (Ric),<ref>{{cite web | title = Entrez Gene: SPP1 secreted phosphoprotein 1 | url = https://www.ncbi.nlm.nih.gov/sites/entrez?db=gene&cmd=retrieve&dopt=default&list_uids=6696&rn=1| accessdate = }}</ref> is a [[protein]] that in humans is encoded by the ''SPP1'' gene (secreted phosphoprotein 1). The murine ortholog is ''Spp1''. Osteopontin is a [[SIBLING proteins|SIBLING]] ([[glycoprotein]]) that was first identified in 1986 in [[osteoblasts]]. | |||
< | The prefix ''[[wikt:osteo-|osteo-]]'' indicates that the protein is expressed in [[bone]], although it is also expressed in other tissues. The suffix ''-pontin'' is derived from "pons," the Latin word for bridge, and signifies osteopontin's role as a linking protein. Osteopontin is an [[Extracellular matrix|extracellular structural protein]] and therefore an [[organic compound|organic]] component of [[bone]]. Synonyms for this [[protein]] include sialoprotein I and 44K BPP (bone phosphoprotein). | ||
{{ | |||
| | The gene has 7 [[exons]], spans 5 [[kilobase]]s in length and in humans it is located on the [[locus (genetics)|long arm]] of [[chromosome 4]] region 22 (4q1322.1). The protein is composed of ~300 [[amino acids]] residues and has ~30 [[carbohydrate]] residues attached including 10 [[sialic acid]] residues, which are attached to the protein during [[Posttranslational modification|post-translational modification]] in the [[Golgi apparatus]]. The protein is rich in acidic residues: 30-36% are either aspartic or glutamic acid. | ||
| | |||
| | ==Structure== | ||
| | |||
| | === General structure === | ||
| | |||
OPN is a highly negatively charged, extracellular matrix protein that lacks an extensive secondary structure.<ref name="WangKX"/> It is composed of about 300 amino acids (297 in mouse; 314 in human) and is expressed as a 33-kDa nascent protein; there are also functionally important cleavage sites. OPN can go through [[posttranslational modifications]], which increase its apparent molecular weight to about 44 kDa.<ref name="pmid16406521">{{cite journal | vauthors = Rangaswami H, Bulbule A, Kundu GC | title = Osteopontin: role in cell signaling and cancer progression | journal = Trends Cell Biol. | volume = 16 | issue = 2 | pages = 79–87 | date = February 2006 | pmid = 16406521 | doi = 10.1016/j.tcb.2005.12.005 }}</ref> The OPN gene is composed of 7 exons, 6 of which containing coding sequence.<ref name="pmid1974876">{{cite journal | vauthors = Young MF, Kerr JM, Termine JD, Wewer UM, Wang MG, McBride OW, Fisher LW | title = cDNA cloning, mRNA distribution and heterogeneity, chromosomal location, and RFLP analysis of human osteopontin (OPN) | journal = Genomics | volume = 7 | issue = 1 | pages = 491–502 | date = August 1990 | pmid = 1974876 | doi = 10.1016/0888-7543(90)90191-V | url = https://zenodo.org/record/1258571 | format = Submitted manuscript }}</ref><ref name="pmid 2726470">{{cite journal | vauthors = Kiefer MC, Bauer DM, Barr PJ | title = The cDNA and derived amino acid sequence for human osteopontin | journal = Nucleic Acids Res. | volume = 17 | issue = 1 | pages = 3306 | date = April 1989 | pmid = 2726470 | pmc = 317745 | doi = 10.1093/nar/17.8.3306 }}</ref> The first two exons contain the 5' untranslated region (5' UTR).<ref name="pmid7665163">{{cite journal | vauthors = Crosby AH, Edwards SJ, Murray JC, Dixon MJ | title = Genomic organization of the human osteopontin gene: exclusion of the locus from a causative role in the pathogenesis of dentinogenesis imperfecta type II | journal = Genomics | volume = 27 | issue = 1 | pages = 155–160 | date = May 1995 | pmid = 7665163 | doi = 10.1006/geno.1995.1018 }}</ref> Exons 2, 3, 4, 5, 6, and 7 code for 17, 13, 27, 14, 108 and 134 amino acids, respectively.<ref name="pmid7665163"/> All intron-exon boundaries are of the phase 0 type, thus alternative exon splicing maintains the reading frame of the OPN gene. | |||
| | |||
| | [[Image:OPN2.jpg|thumb|250px|right|'''Figure 1. Proteolytic cleavage sites for full length osteopontin (OPN-FL).''' Thrombin exposes the cleaved epitope SVVYGLR (OPN-R), and then CPB removes the c-terminal arginine from OPN-R. The cleaved epitope has a non-RGD domain, which binds to integrin receptors (α4β1, α9β1, and α9β4). Next to the cleaved epitope, there is a RGD domain that interacts with other integrin receptors (αvβ1,3,5, and α5β1).]] | ||
| | === Isoforms === | ||
| | |||
| | Full-length OPN (OPN-FL) can be modified by [[thrombin]] cleavage, which exposes a cryptic sequence, SVVYGLR on the cleaved form of the protein known as OPN-R (Fig. 1). This thrombin-cleaved OPN (OPN-R) exposes an [[epitope]] for integrin receptors of α4β1, α9β1, and α9β4.<ref name="Laffon">{{cite journal | vauthors = Laffón A, García-Vicuña R, Humbría A, Postigo AA, Corbí AL, de Landázuri MO, Sánchez-Madrid F | title = Upregulated expression and function of VLA-4 fibronectin receptors on human activated T cells in rheumatoid arthritis | journal = J. Clin. Invest. | volume = 88 | issue = 2 | pages = 546–52 | date = August 1991 | pmid = 1830891 | pmc = 295383 | doi = 10.1172/JCI115338 }}</ref><ref name="Seiffge">{{cite journal | vauthors = Seiffge D | title = Protective effects of monoclonal antibody to VLA-4 on leukocyte adhesion and course of disease in adjuvant arthritis in rats | journal = J. Rheumatol. | volume = 23 | issue = 12 | pages = 2086–91 | date = December 1996 | pmid = 8970045 | doi = }}</ref> These integrin receptors are present on a number of immune cells such as [[mast cells]],<ref name="Reinholt">{{cite journal | vauthors = Reinholt FP, Hultenby K, Oldberg A, Heinegård D | title = Osteopontin--a possible anchor of osteoclasts to bone | journal = Proc. Natl. Acad. Sci. U.S.A. | volume = 87 | issue = 12 | pages = 4473–5 | date = June 1990 | pmid = 1693772 | pmc = 54137 | doi = 10.1073/pnas.87.12.4473 }}</ref> neutrophils,<ref name="pmid16440289">{{cite journal | vauthors = Banerjee A, Apte UM, Smith R, Ramaiah SK | title = Higher neutrophil infiltration mediated by osteopontin is a likely contributing factor to the increased susceptibility of females to alcoholic liver disease | journal = J. Pathol. | volume = 208 | issue = 4 | pages = 473–85 | date = March 2006 | pmid = 16440289 | doi = 10.1002/path.1917 }}</ref> and T cells. It is also expressed by monocytes and macrophages.<ref name="pmid16632752">{{cite journal | vauthors = Sodek J, Batista Da Silva AP, Zohar R | title = Osteopontin and mucosal protection | journal = J. Dent. Res. | volume = 85 | issue = 5 | pages = 404–15 | date = May 2006 | pmid = 16632752 | doi = 10.1177/154405910608500503 | url = http://jdr.iadrjournals.org/cgi/pmidlookup?view=long&pmid=16632752 }}</ref> Upon binding these receptors, cells use several [[signal transduction]] pathways to elicit immune responses in these cells. OPN-R can be further cleaved by Carboxypeptidase B (CPB) by removal of C-terminal arginine and become OPN-L. The function of OPN-L is largely unknown. | ||
| | |||
| | It appears an intracellular variant of OPN (iOPN) is involved in a number of cellular processes including migration, fusion and motility.<ref name="Zohar">{{cite journal | vauthors = Zohar R, Suzuki N, Suzuki K, Arora P, Glogauer M, McCulloch CA, Sodek J | title = Intracellular osteopontin is an integral component of the CD44-ERM complex involved in cell migration | journal = J Cell Physiol | volume = 184 | issue = 1 | pages = 118–130 | date = July 2000 | pmid = 10825241 | pmc = | doi = 10.1002/(SICI)1097-4652(200007)184:1<118::AID-JCP13>3.0.CO;2-Y }}</ref><ref name="Suzuki">{{cite journal | vauthors = Suzuki K, Zhu B, Rittling SR, Denhardt DT, Goldberg HA, McCulloch CA, Sodek J | title = Colocalization of intracellular osteopontin with CD44 is associated with migration, cell fusion, and resorption in osteoclasts | journal = J Bone Miner Res | volume = 17 | issue = 1 | pages = 1486–1497 | date = August 2002 | pmid = 12162503 | pmc = | doi = 10.1359/jbmr.2002.17.8.1486 }}</ref><ref name="Zhu">{{cite journal | vauthors = Zhu B, Suzuki K, Goldberg HA, Rittling SR, Denhardt DT, McCulloch CA, Sodek J | title = Osteopontin modulates CD44-dependent chemotaxis of peritoneal macrophages through G-protein-coupled receptors: evidence of a role for an intracellular form of osteopontin | journal = Journal of Cellular Physiology | volume = 198 | issue = 1 | pages = 155–167 | date = January 2004 | pmid = 14584055 | pmc = | doi = 10.1002/jcp.10394 }}</ref><ref name="Junaid">{{cite journal | vauthors = Junaid A, Moon MC, Harding GE, Zahradka P | title = Osteopontin localizes to the nucleus of 293 cells and associates with polo-like kinase-1 | journal = Am J Physiol Cell Physiol | volume = 292 | issue = 1 | pages = 919–926 | date = February 2007 | pmid = 17005603 | pmc = | doi = 10.1152/ajpcell.00477.2006 }}</ref> Intracellular OPN is generated using an alternative translation start site on the same mRNA species used to generate the extracellular isoform.<ref name="Shinohara">{{cite journal | vauthors = Shinohara ML, Kim HJ, Kim JH, Garcia VA, Cantor H | title = Alternative translation of osteopontin generates intracellular and secreted isoforms that mediate distinct biological activities in dendritic cells | journal = Proc Natl Acad Sci USA | volume = 105 | issue = 1 | pages = 7235–7239 | date = May 2008 | pmid = 18480255 | pmc = 2438233 | doi = 10.1073/pnas.0802301105 }}</ref> This alternative translation start site is downstream of the N-terminal endoplasmic reticulum-targeting signal sequence, thus allowing cytoplasmic translation of OPN. | ||
| | |||
Various human cancers, including breast cancer, have been observed to express splice variants of OPN.<ref name="He">{{cite journal | vauthors = He B, Mirza M, Weber GF | title = An osteopontin splice variant induces anchorage independence in human breast cancer cells | journal = Oncogene | volume = 25 | issue = 1 | pages = 2192–2202 | date = April 2006 | pmid = 16288209 | pmc = | doi = 10.1038/sj.onc.1209248 }}</ref><ref name="Mirza">{{cite journal | vauthors = Mirza M, Shaughnessy E, Hurley JK, Vanpatten KA, Pestano GA, He B, Weber GF | title = Osteopontin-c is a selective marker of breast cancer | journal = Int J Cancer | volume = 122 | issue = 1 | pages = 889–897 | date = February 2008 | pmid = 17960616 | pmc = | doi = 10.1002/ijc.23204 }}</ref> The cancer-specific splice variants are osteopontin-a, osteopontin-b, and osteopontin-c. Exon 5 is lacking from osteopontin-b, whereas osteopontin-c lacks exon 4.<ref name="He"/> Osteopontin-c has been suggested to facilitate the anchorage-independent phenotype of some human breast cancer cells due to its inability to associate with the extracellular matrix.<ref name="He"/> | |||
== Biosynthesis == | |||
[[File:Journal.pmed.0020314.g001 Osteopontin.png|left|thumb|Osteopontin seen in a lung tissue sample from a patient with ideopathic pulmonary fibrosis.]] | |||
Osteopontin is biosynthesized by a variety of tissue types including cardiac [[fibroblasts]],<ref name ="Ashizawa">{{cite journal | vauthors = Ashizawa N, Graf K, Do YS, Nunohiro T, Giachelli CM, Meehan WP, Tuan TL, Hsueh WA | title = Osteopontin is produced by rat cardiac fibroblasts and mediates A(II)-induced DNA synthesis and collagen gel contraction | journal = J. Clin. Invest. | volume = 98 | issue = 10 | pages = 2218–27 | date = November 1996 | pmid = 8941637 | pmc = 507670 | doi = 10.1172/JCI119031 }}</ref> [[preosteoblasts]], osteoblasts, [[osteocytes]], [[odontoblasts]], some [[bone marrow]] [[Cell (biology)|cells]], hypertrophic [[chondrocytes]], [[dendritic cells]], [[macrophages]],<ref name ="Murry">{{cite journal | vauthors = Murry CE, Giachelli CM, Schwartz SM, Vracko R | title = Macrophages express osteopontin during repair of myocardial necrosis | journal = Am. J. Pathol. | volume = 145 | issue = 6 | pages = 1450–62 | date = December 1994 | pmid = 7992848 | pmc = 1887495 | doi = }}</ref> [[smooth muscle]],<ref name="Ikeda">{{cite journal | vauthors = Ikeda T, Shirasawa T, Esaki Y, Yoshiki S, Hirokawa K | title = Osteopontin mRNA is expressed by smooth muscle-derived foam cells in human atherosclerotic lesions of the aorta | journal = J. Clin. Invest. | volume = 92 | issue = 6 | pages = 2814–20 | date = December 1993 | pmid = 8254036 | pmc = 288482 | doi = 10.1172/JCI116901 }}</ref> skeletal muscle [[myoblasts]],<ref name="Uaesoontrachoon">{{cite journal | vauthors = Uaesoontrachoon K, Yoo HJ, Tudor EM, Pike RN, Mackie EJ, Pagel CN | title = Osteopontin and skeletal muscle myoblasts: Association with muscle regeneration and regulation of myoblast function in vitro | journal = Int. J. Biochem. Cell Biol. | volume = 40 | issue = 10 | pages = 2303–14 | date = April 2008 | pmid = 18490187 | doi = 10.1016/j.biocel.2008.03.020 }}</ref> [[endothelial cells]], and extraosseous (non-bone) cells in the inner [[ear]], [[brain]], [[kidney]], [[deciduum]], and [[placenta]]. Synthesis of osteopontin is stimulated by [[calcitriol]] (1,25-dihydroxy-vitamin D<sub>3</sub>). | |||
=== Regulation === | |||
Regulation of the osteopontin gene is incompletely understood. Different cell types may differ in their regulatory mechanisms of the OPN gene. OPN expression in bone predominantly occurs by osteoblasts and osteocyctes (bone-forming cells) as well as osteoclasts (bone-resorbing cells).<ref name="pmid8314886">{{cite journal | vauthors = Merry K, Dodds R, Littlewood A, Gowen M | title = Expression of Osteopontin mRNA by osteoclasts and osteoblasts in modelling adult human bone | journal = J Cell Sci | volume = 104 | issue = 4 | pages = 1013–1020 | date = April 1993 | pmid = 8314886 | doi = }}</ref> Runx2 (aka Cbfa1) and osterix (Osx) transcription factors are required for the expression of OPN <ref name="pmid11792318">{{cite journal | vauthors = Nakashima K, Zhou X, Kunkel G, Zhang Z, Deng JM, Behringer RR, de Crombrugghe B | title = The novel zinc finger-containing transcription factor osterix is required for osteoblast differentiation and bone formation | journal = Cell | volume = 108 | issue = 1 | pages = 17–29 | date = January 2002 | pmid = 11792318 | doi = 10.1016/S0092-8674(01)00622-5 }}</ref> Runx2 and Osx bind promoters of osteoblast-specific genes such as ''Col1α1'', ''Bsp'', and ''Opn'' and upregulate transcription.<ref name="pmid9182762">{{cite journal | vauthors = Ducy P, Zhang R, Geoffroy V, Ridall AL, Karsenty G | title = Osf2/Cbfa1: a transcriptional activator of osteoblast differentiation | journal = Cell | volume = 89 | issue = 1 | pages = 747–754 | date = May 1997 | pmid = 9182762 | doi = 10.1016/S0092-8674(00)80257-3 }}</ref> | |||
Hypocalcemia and hypophosphatemia (instances that stimulate kidney proximal tubule cells to produce calcitriol (1α,25-dihydroxyvitamin D3)) lead to increases in OPN transcription, translation and secretion.<ref name="pmid14730782">{{cite journal | vauthors = Yucha C, Guthrie D | title = Renal homeostasis of calcium | journal = Nephrol Nurs J | volume = 30 | issue = 1 | pages = 755–764 | date = December 2003 | pmid = 14730782 | doi = }}</ref> This is due to the presence of a high-specificity vitamin D response element ([[VDRE]]) in the OPN gene promoter.<ref name="pmid3478171">{{cite journal | vauthors = Prince CW, Butler WT | title = 1,25-Dihydroxyvitamin D3 regulates the biosyntheis of osteopontin, a bone-derived cell attachment protein, in clonal osteoblast-like osteosarcoma cells | journal = Coll Relat Res | volume = 7 | issue = 1 | pages = 305–313 | date = September 1987 | pmid = 3478171 | doi = 10.1016/s0174-173x(87)80036-5 }}</ref><ref name="pmid2592421">{{cite journal | vauthors = Oldberg A, Jirskog-Hed B, Axelsson S, Heinegård D | title = Regulation of bone sialoprotein mRNA by steroid hormones | journal = J Cell Biol | volume = 109 | issue = 1 | pages = 3183–3186 | date = December 1989 | pmid = 2592421 | pmc = 2115918 | doi = 10.1083/jcb.109.6.3183 }}</ref><ref name="pmid2009532">{{cite journal | vauthors = Chang PL, Prince CW | title = 1 alpha,25-Dihydroxyvitamin D3 enhances 12-O-tetradecanoylphorbol-13-acetate- induced tumorigenic transformation and osteopontin expression in mouse JB6 epidermal cells | journal = Cancer Res | volume = 51 | issue = 8 | pages = 2144–2150 | date = May 1991 | pmid = 2009532 | doi = }}</ref> | |||
Extracellular inorganic phosphate (ePi) has also been identified as a modulator of OPN expression.<ref name="pmid19131315">{{cite journal | vauthors = Fatherazi S, Matsa-Dunn D, Foster BL, Rutherford RB, Somerman MJ, Presland RB | title = Phosphate regulates osteopontin gene transcription | journal = J Dent Res | volume = 88 | issue = 1 | pages = 39–44 | date = January 2009 | pmid = 19131315 | pmc = 3128439 | doi = 10.1177/0022034508328072 }}</ref> | |||
Stimulation of OPN expression also occurs upon exposure of cells to pro-inflammatory cytokines,<ref name="pmid11145688">{{cite journal | vauthors = Guo H, Cai CQ, Schroeder RA, Kuo PC | title = Osteopontin is a negative feedback regulator of nitric oxide synthesis in murine macrophages | journal = J Immunol | volume = 166 | issue = 1 | pages = 1079–1086 | date = January 2001 | pmid = 11145688 | doi = 10.4049/jimmunol.166.2.1079 }}</ref> classical mediators of acute inflammation (e.g. tumour necrosis factor α [TNFα], infterleukin-1β [IL-1β]), angiotensin II, transforming growth factor β (TGFβ) and parathyroid hormone (PTH),<ref name="pmid10807582">{{cite journal | vauthors = Ricardo SD, Franzoni DF, Roesener CD, Crisman JM, Diamond JR | title = Angiotensinogen and AT(1) antisense inhibition of osteopontin translation in rat proximal tubular cells | journal = Am J Physiol Renal Physiol | volume = 278 | issue = 1 | pages = 708–716 | date = May 2000 | pmid = 10807582 | doi = 10.1152/ajprenal.2000.278.5.F708}}</ref><ref name="pmid2465299">{{cite journal | vauthors = Noda M, Rodan GA | title = Transcriptional regulation of osteopontin production in rat osteoblast-like cells by parathyroid hormone | journal = J Cell Biol | volume = 108 | issue = 1 | pages = 713–718 | date = February 1989 | pmid = 2465299 | pmc = 2115413 | doi = 10.1083/jcb.108.2.713 }}</ref> although a detailed mechanistic understanding of these regulatory pathways are not yet known. Hyperglycemia and hypoxia are also known to increase OPN expression.<ref name="pmid10807582"/><ref name="pmid11120606">{{cite journal | vauthors = Hullinger TG, Pan Q, Viswanathan HL, Somerman MJ | title = TGFbeta and BMP-2 activation of the OPN promoter: roles of smad- and hox-binding elements | journal = Exp Cell Res | volume = 262 | issue = 1 | pages = 69–74 | date = January 2001 | pmid = 11120606 | doi = 10.1006/excr.2000.5074 }}</ref><ref name="pmid11249858">{{cite journal | vauthors = Sodhi CP, Phadke SA, Batlle D, Sahai A | title = Hypoxia and high glucose cause exaggerated mesangial cell growth and collagen synthesis: role of osteopontin | journal = Am J Physiol Renal Physiol | volume = 280 | issue = 1 | pages = 667–674 | date = April 2001 | pmid = 11249858 | doi = 10.1152/ajprenal.2001.280.4.F667}}</ref> | |||
== Biological function == | |||
}} | === Role in biomineralization === | ||
OPN belongs to a family of secreted acidic proteins whose members have an abundance of negatively charged amino acids such as [[aspartic acid|Asp]] and [[glutamic acid|Glu]].<ref name="pmid12952171">{{cite journal | vauthors = Fisher LW, Fedarko NS | title = Six genes expressed in bones and teeth encode the current members of the SIBLING family of proteins | journal = Connect. Tissue Res. | volume = 44 Suppl 1 | issue = | pages = 33–40 | year = 2003 | pmid = 12952171 | doi = 10.1080/03008200390152061 }}</ref> OPN also has a large number of consensus sequence sites for post-translational [[phosphorylation]] of Ser residues to form [[phosphoserine]], providing additional negative charge.<ref name="pmid15869464">{{cite journal | vauthors = Christensen B, Nielsen MS, Haselmann KF, Petersen TE, Sørensen ES | title = Post-translationally modified residues of native human osteopontin are located in clusters: identification of 36 phosphorylation and five O-glycosylation sites and their biological implications | journal = Biochem. J. | volume = 390 | issue = Pt 1 | pages = 285–92 | date = August 2005 | pmid = 15869464 | pmc = 1184582 | doi = 10.1042/BJ20050341 }}</ref> Contiguous stretches of high negative charge in OPN have been identified and named the polyAsp motif (poly-aspartic acid) and the ASARM motif (acidic serine- and aspartate-rich motif), with the latter sequence having multiple phosphorylation sites.<ref name="pmid21177780">{{cite journal | vauthors = David V, Martin A, Hedge AM, Drezner MK, Rowe PS | title = ASARM peptides: PHEX-dependent and -independent regulation of serum phosphate | journal = Am. J. Physiol. Renal Physiol. | volume = 300 | issue = 3 | pages = F783–91 | date = March 2011 | pmid = 21177780 | pmc = 3064126 | doi = 10.1152/ajprenal.00304.2010 }}</ref><ref name="pmid18162525">{{cite journal | vauthors = Martin A, David V, Laurence JS, Schwarz PM, Lafer EM, Hedge AM, Rowe PS | title = Degradation of MEPE, DMP1, and release of SIBLING ASARM-peptides (minhibins): ASARM-peptide(s) are directly responsible for defective mineralization in HYP | journal = Endocrinology | volume = 149 | issue = 4 | pages = 1757–72 | date = April 2008 | pmid = 18162525 | pmc = 2276704 | doi = 10.1210/en.2007-1205 }}</ref><ref name="pmid18597632">{{cite journal | vauthors = Addison WN, Nakano Y, Loisel T, Crine P, McKee MD | title = MEPE-ASARM peptides control extracellular matrix mineralization by binding to hydroxyapatite: an inhibition regulated by PHEX cleavage of ASARM | journal = J. Bone Miner. Res. | volume = 23 | issue = 10 | pages = 1638–49 | date = October 2008 | pmid = 18597632 | doi = 10.1359/jbmr.080601 }}</ref><ref name="pmid19775205">{{cite journal | vauthors = Addison WN, Masica DL, Gray JJ, McKee MD | title = Phosphorylation-dependent inhibition of mineralization by osteopontin ASARM peptides is regulated by PHEX cleavage | journal = J. Bone Miner. Res. | volume = 25 | issue = 4 | pages = 695–705 | date = April 2010 | pmid = 19775205 | doi = 10.1359/jbmr.090832 }}</ref> This overall negative charge of OPN, along with its specific acidic motifs and the fact that OPN is an intrinsically disordered protein<ref name="pmid23848319">{{cite journal | vauthors = Kurzbach D, Platzer G, Schwarz TC, Henen MA, Konrat R, Hinderberger D | title = Cooperative Unfolding of Compact Conformations of the Intrinsically Disordered Protein Osteopontin | journal = Biochemistry | volume = 52 | issue = 31 | pages = 5167–75 | date = July 2013 | pmid = 23848319 | pmc = 3737600 | doi = 10.1021/bi400502c }}</ref><ref name="pmid22634174">{{cite journal | vauthors = Kalmar L, Homola D, Varga G, Tompa P | title = Structural disorder in proteins brings order to crystal growth in biomineralization | journal = Bone | volume = 51 | issue = 3 | pages = 528–34 | date = September 2012 | pmid = 22634174 | doi = 10.1016/j.bone.2012.05.009 }}</ref> allowing for open and flexible structures, permit OPN to bind strongly to calcium atoms available at crystal surfaces in various biominerals.<ref name="pmid19775205"/><ref name="pmid20174473">{{cite journal | vauthors = Azzopardi PV, O'Young J, Lajoie G, Karttunen M, Goldberg HA, Hunter GK | title = Roles of electrostatics and conformation in protein-crystal interactions | journal = PLoS ONE | volume = 5 | issue = 2 | pages = e9330 | year = 2010 | pmid = 20174473 | pmc = 2824833 | doi = 10.1371/journal.pone.0009330 }}</ref><ref name="pmid20527831">{{cite journal | vauthors = Hunter GK, O'Young J, Grohe B, Karttunen M, Goldberg HA | title = The flexible polyelectrolyte hypothesis of protein-biomineral interaction | journal = Langmuir | volume = 26 | issue = 24 | pages = 18639–46 | date = December 2010 | pmid = 20527831 | doi = 10.1021/la100401r }}</ref> Such binding of OPN to various types of calcium-based biominerals ‒ such as calcium-phosphate mineral in bones and teeth,<ref name="pmid7626799">{{cite journal | vauthors = McKee MD, Nanci A | title = Postembedding colloidal-gold immunocytochemistry of noncollagenous extracellular matrix proteins in mineralized tissues | journal = Microsc. Res. Tech. | volume = 31 | issue = 1 | pages = 44–62 | date = May 1995 | pmid = 7626799 | doi = 10.1002/jemt.1070310105 }}</ref> calcium-carbonate mineral in inner ear otoconia<ref name="pmid7806488">{{cite journal | vauthors = Takemura T, Sakagami M, Nakase T, Kubo T, Kitamura Y, Nomura S | title = Localization of osteopontin in the otoconial organs of adult rats | journal = Hear. Res. | volume = 79 | issue = 1–2 | pages = 99–104 | date = September 1994 | pmid = 7806488 | doi = 10.1016/0378-5955(94)90131-7 }}</ref> and avian eggshells,<ref name="pmid22201802">{{cite journal | vauthors = Hincke MT, Nys Y, Gautron J, Mann K, Rodriguez-Navarro AB, McKee MD | title = The eggshell: structure, composition and mineralization | journal = Front. Biosci. | volume = 17 | issue = | pages = 1266–80 | year = 2012 | pmid = 22201802 | doi = 10.2741/3985 }}</ref> and calcium-[[oxalate]] mineral in kidney stones<ref name="pmid8619372">{{cite journal | vauthors = McKee MD, Nanci A, Khan SR | title = Ultrastructural immunodetection of osteopontin and osteocalcin as major matrix components of renal calculi | journal = J. Bone Miner. Res. | volume = 10 | issue = 12 | pages = 1913–29 | date = December 1995 | pmid = 8619372 | doi = 10.1002/jbmr.5650101211 }}</ref><ref name="pmid18728346">{{cite journal | vauthors = O'Young J, Chirico S, Al Tarhuni N, Grohe B, Karttunen M, Goldberg HA, Hunter GK | title = Phosphorylation of osteopontin peptides mediates adsorption to and incorporation into calcium oxalate crystals | journal = Cells Tissues Organs (Print) | volume = 189 | issue = 1–4 | pages = 51–5 | year = 2009 | pmid = 18728346 | doi = 10.1159/000151724 }}</ref><ref name="pmid19581305">{{cite journal | vauthors = Chien YC, Masica DL, Gray JJ, Nguyen S, Vali H, McKee MD | title = Modulation of calcium oxalate dihydrate growth by selective crystal-face binding of phosphorylated osteopontin and polyaspartate peptide showing occlusion by sectoral (compositional) zoning | journal = J. Biol. Chem. | volume = 284 | issue = 35 | pages = 23491–501 | date = August 2009 | pmid = 19581305 | pmc = 2749123 | doi = 10.1074/jbc.M109.021899 }}</ref> – acts as a mineralization inhibitor to regulate crystal growth.<ref name="pmid11021631">{{cite journal | vauthors = Sodek J, Ganss B, McKee MD | title = Osteopontin | journal = Crit. Rev. Oral Biol. Med. | volume = 11 | issue = 3 | pages = 279–303 | year = 2000 | pmid = 11021631 | doi = 10.1177/10454411000110030101 }}</ref> | |||
OPN is a substrate protein for a number of enzymes whose actions may modulate the mineralization-inhibiting function of OPN. [[PHEX]] (phosphate-regulating gene with homologies to endopeptidases on the X chromosome) is one such enzyme, which extensively degrades OPN, and whose inactivating gene mutations (in X-linked hypophosphatemia, XLH) lead to altered processing of OPN such that inhibitory OPN cannot be degraded and accumulates in the bone (and tooth) extracellular matrix, likely contributing locally to the osteomalacia (soft hypomineralized bones) characteristic of XLH.<ref>{{cite journal | vauthors = McKee MD, Hoac B, Addison WN, Barros NM, Millán JL, Chaussain C | title = Extracellular matrix mineralization in periodontal tissues: Noncollagenous matrix proteins, enzymes, and relationship to hypophosphatasia and X-linked hypophosphatemia | journal = Periodontology 2000 | volume = 63 | issue = 1 | pages = 102–22 | date = October 2013 | pmid = 23931057 | pmc = 3766584 | doi = 10.1111/prd.12029 }}</ref><ref>{{cite journal | vauthors = Boukpessi T, Hoac B, Coyac BR, Leger T, Garcia C, Wicart P, Whyte MP, Glorieux FH, Linglart A, Chaussain C, McKee MD | title = Osteopontin and the dento-osseous pathobiology of X-linked hypophosphatemia | journal = Bone | volume = 95 | pages = 151–161 | date = February 2017 | pmid = 27884786 | doi = 10.1016/j.bone.2016.11.019 }}</ref><ref>{{cite journal | vauthors = Barros NM, Hoac B, Neves RL, Addison WN, Assis DM, Murshed M, Carmona AK, McKee MD | title = Proteolytic processing of osteopontin by PHEX and accumulation of osteopontin fragments in Hyp mouse bone, the murine model of X-linked hypophosphatemia | journal = Journal of Bone and Mineral Research | volume = 28 | issue = 3 | pages = 688–99 | date = March 2013 | pmid = 22991293 | doi = 10.1002/jbmr.1766 }}</ref> | |||
Along with its role in the regulation of normal mineralization within the extracellular matrices of bones and teeth,<ref name="pmid16612083">{{cite journal | vauthors = McKee MD, Addison WN, Kaartinen MT | title = Hierarchies of extracellular matrix and mineral organization in bone of the craniofacial complex and skeleton | journal = Cells Tissues Organs (Print) | volume = 181 | issue = 3–4 | pages = 176–88 | year = 2005 | pmid = 16612083 | doi = 10.1159/000091379 }}</ref> OPN is also upregulated at sites of pathologic, [[ectopic calcification]]<ref name="pmid12466120">{{cite journal | vauthors = Steitz SA, Speer MY, McKee MD, Liaw L, Almeida M, Yang H, Giachelli CM | title = Osteopontin inhibits mineral deposition and promotes regression of ectopic calcification | journal = Am. J. Pathol. | volume = 161 | issue = 6 | pages = 2035–46 | date = December 2002 | pmid = 12466120 | pmc = 1850905 | doi = 10.1016/S0002-9440(10)64482-3 }}</ref><ref name="pmid10079244">{{cite journal | vauthors = Giachelli CM | title = Ectopic calcification: gathering hard facts about soft tissue mineralization | journal = Am. J. Pathol. | volume = 154 | issue = 3 | pages = 671–5 | date = March 1999 | pmid = 10079244 | pmc = 1866412 | doi = 10.1016/S0002-9440(10)65313-8 }}</ref> – such as for example, in [[urolithiasis]] and [[calciphylaxis|vascular calcification]] ‒ presumably at least in part to inhibit debilitating mineralization in these soft tissues. | |||
=== Role in bone remodeling === | |||
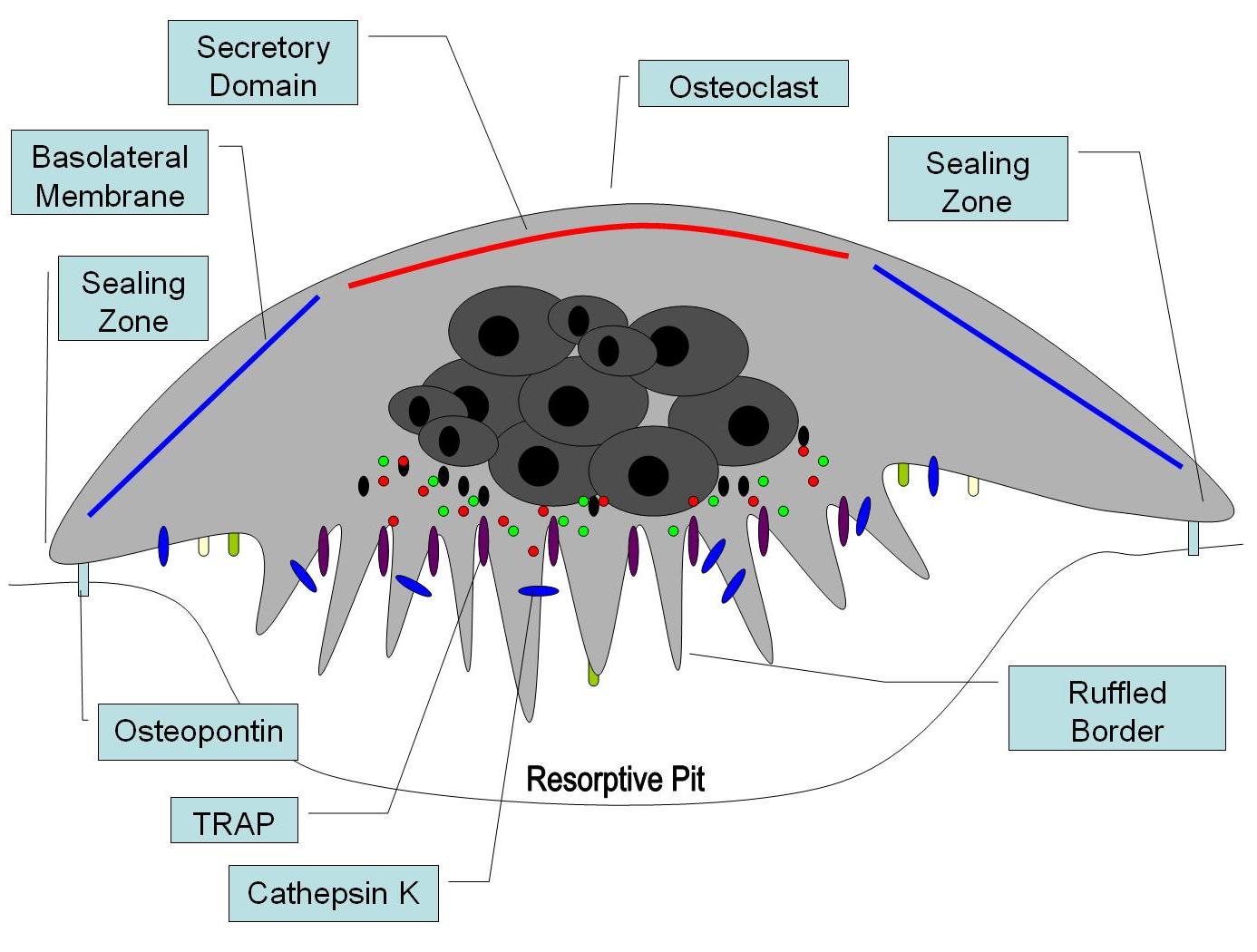
Osteopontin has been implicated as an important factor in [[bone remodeling]].<ref name="pmid18854347">{{cite journal | vauthors = Choi ST, Kim JH, Kang EJ, Lee SW, Park MC, Park YB, Lee SK | title = Osteopontin might be involved in bone remodelling rather than in inflammation in ankylosing spondylitis | journal = Rheumatology (Oxford) | volume = 47 | issue = 12 | pages = 1775–9 | date = December 2008 | pmid = 18854347 | doi = 10.1093/rheumatology/ken385 }}</ref> Specifically, research suggests it plays a role in anchoring [[osteoclasts]] to the mineral matrix of bones.<ref name="Reinholt"/> The organic part of bone is about 20% of the dry weight, and counts in, other than osteopontin, [[collagen type I]], [[osteocalcin]], [[osteonectin]], [[bone sialo protein]], and [[alkaline phosphatase]]. Collagen type I counts for 90% of the protein mass. The inorganic part of bone is the mineral [[hydroxyapatite]], Ca<sub>10</sub>(PO<sub>4</sub>)<sub>6</sub>(OH)<sub>2</sub>. Loss of this mineral may lead to [[osteoporosis]], as the bone is depleted for calcium if this is not supplied in the diet. | |||
OPN serves to initiate the process by which [[osteoclast]]s develop their [[Osteoclast#Function|ruffled border]]s to begin bone resorption. It is also found in [[urine]], where it inhibits [[kidney stone]] formation. | |||
=== Role in immune functions === | |||
As discussed, OPN binds to several integrin receptors including α4β1, α9β1, and α9β4 expressed by [[leukocytes]]. These receptors have been well-established to function in cell adhesion, migration, and survival in these cells. Therefore, recent research efforts have focused on the role of OPN in mediating such responses. | |||
Osteopontin (OPN) is expressed in a range of immune cells, including macrophages, [[neutrophils]], dendritic cells, and [[T cells|T]] and [[B cells]], with varying kinetics. OPN is reported to act as an immune modulator in a variety of manners.<ref name="WangKX">{{cite journal | vauthors = Wang KX, Denhardt DT | title = Osteopontin: role in immune regulation and stress responses | journal = Cytokine Growth Factor Rev. | volume = 19 | issue = 5–6 | pages = 333–45 | year = 2008 | pmid = 18952487 | doi = 10.1016/j.cytogfr.2008.08.001 | url = http://hdl.rutgers.edu/1782.2/rucore10001600001.ETD.17059 }}</ref> Firstly, it has [[chemotaxis|chemotactic properties]], which promote cell recruitment to inflammatory sites. It also functions as an [[Cell adhesion protein|adhesion protein]], involved in [[Cell adhesion|cell attachment]] and [[wound healing]]. In addition, OPN mediates cell activation and [[cytokine]] production, as well as promoting cell survival by regulating [[apoptosis]].<ref name=WangKX /> The following examples are found.<ref name=WangKX /> | |||
==== Role in Heart ==== | |||
OPN expression increases under a variety of conditions of the heart, and is associated with increased myocyte apoptosis and myocardial dysfunction.<ref>{{cite journal | vauthors = Singh M, Dalal S, Singh K | title = Osteopontin: At the cross-roads of myocyte survival and myocardial function | journal = Life Sci | date = 2014 | pmid = 25265596 | doi = 10.1016/j.lfs.2014.09.014 | volume=118 | issue = 1 | pages=1–6 | pmc=4254317}}</ref> | |||
==== Chemotaxis ==== | |||
OPN plays an important role in neutrophil recruitment in alcoholic liver disease.<ref name="pmid16440289"/><ref name="pmid15885730">{{cite journal | vauthors = Apte UM, Banerjee A, McRee R, Wellberg E, Ramaiah SK | title = Role of osteopontin in hepatic neutrophil infiltration during alcoholic steatohepatitis | journal = Toxicol. Appl. Pharmacol. | volume = 207 | issue = 1 | pages = 25–38 | date = August 2005 | pmid = 15885730 | doi = 10.1016/j.taap.2004.12.018 }}</ref> OPN is important for the migration of neutrophil [[in vitro]].<ref name="pmid17680800">{{cite journal | vauthors = Koh A, da Silva AP, Bansal AK, Bansal M, Sun C, Lee H, Glogauer M, Sodek J, Zohar R | title = Role of osteopontin in neutrophil function | journal = Immunology | volume = 122 | issue = 4 | pages = 466–75 | date = December 2007 | pmid = 17680800 | pmc = 2266047 | doi = 10.1111/j.1365-2567.2007.02682.x }}</ref> In addition, OPN recruits inflammatory cells to arthritis joints in the collagen-induced arthritis model of rheumatoid arthritis.<ref name="pmid11953989">{{cite journal | vauthors = Ohshima S, Kobayashi H, Yamaguchi N, Nishioka K, Umeshita-Sasai M, Mima T, Nomura S, Kon S, Inobe M, Uede T, Saeki Y | title = Expression of osteopontin at sites of bone erosion in a murine experimental arthritis model of collagen-induced arthritis: possible involvement of osteopontin in bone destruction in arthritis | journal = Arthritis Rheum. | volume = 46 | issue = 4 | pages = 1094–101 | date = April 2002 | pmid = 11953989 | doi = 10.1002/art.10143 }}</ref><ref name="pmid11469452">{{cite journal | vauthors = Sakata M, Tsuruha JI, Masuko-Hongo K, Nakamura H, Matsui T, Sudo A, Nishioka K, Kato T | title = Autoantibodies to osteopontin in patients with osteoarthritis and rheumatoid arthritis | journal = J. Rheumatol. | volume = 28 | issue = 7 | pages = 1492–5 | date = July 2001 | pmid = 11469452 | doi = }}</ref> A recent in vitro study in 2008 has found that OPN plays a role in mast cell migration.<ref name="Nagasaka">{{cite journal | vauthors = Nagasaka A, Matsue H, Matsushima H, Aoki R, Nakamura Y, Kambe N, Kon S, Uede T, Shimada S | title = Osteopontin is produced by mast cells and affects IgE-mediated degranulation and migration of mast cells | journal = Eur. J. Immunol. | volume = 38 | issue = 2 | pages = 489–99 | date = February 2008 | pmid = 18200503 | doi = 10.1002/eji.200737057 | title-link = degranulation }}</ref> Here OPN knock-out mast cells were cultured and they observed a decreased level of chemotaxis in these cells compared to wildtype mast cells. OPN was also found to act as a macrophage [[chemotactic]] factor.<ref name="Burdo">{{cite journal | vauthors = Burdo TH, Wood MR, Fox HS | title = Osteopontin prevents monocyte recirculation and apoptosis | journal = J. Leukoc. Biol. | volume = 81 | issue = 6 | pages = 1504–11 | date = June 2007 | pmid = 17369493 | pmc = 2490714 | doi = 10.1189/jlb.1106711 }}</ref> In this study, researchers looked at the accumulation of macrophages in the brain of rhesus monkeys and found that OPN prevented macrophages from leaving the accumulation site, indicating an increased level of chemotaxis. | |||
==== Cell activation ==== | |||
Activated T cells are promoted by [[Interleukin 12|IL-12]] to differentiate towards the Th1 type, producing cytokines including IL-12 and [[IFNγ]]. OPN inhibits production of the Th2 cytokine IL-10, which leads to enhanced Th1 response. OPN influences cell-mediated immunity and has Th1 cytokine functions. It enhances B cell immunoglobulin production and proliferation.<ref name="WangKX"/> Recent studies in 2008 suggest that OPN also induces mast cell degranulation.<ref name="Nagasaka"/> The researchers here observed that [[IgE-mediated anaphylaxis]] was significantly reduced in OPN knock-out mice compared to wild-type mice. The role of OPN in activation of macrophages has also been implicated in a cancer study, when researchers discovered that OPN-producing tumors were able to induce macrophage activation compared to OPN-deficient tumors.<ref name="Crawford">{{cite journal | vauthors = Crawford HC, Matrisian LM, Liaw L | title = Distinct roles of osteopontin in host defense activity and tumor survival during squamous cell carcinoma progression in vivo | journal = Cancer Res. | volume = 58 | issue = 22 | pages = 5206–15 | date = November 1998 | pmid = 9823334 | doi = }}</ref> | |||
[[Image:Biological functions of OPN.jpg|thumb|500px|right|'''Fig 2. Known immunologic functions of OPN.''' OPN binds to several integrin receptors including α4β1, α9β1, and α9β4 expressed by leukocytes and are known to induce cell adhesion, migration, and survival in immune cells including neutrophils, macrophages, T cells, mast cells, and osteoclasts.]] | |||
==== Apoptosis ==== | |||
OPN is an important anti-[[apoptotic]] factor in many circumstances. OPN blocks the activation-induced cell death of macrophages and T cells as well as fibroblasts and endothelial cells exposed to harmful stimuli.<ref name="Denhardt">{{cite journal | vauthors = Denhardt DT, Noda M, O'Regan AW, Pavlin D, Berman JS | title = Osteopontin as a means to cope with environmental insults: regulation of inflammation, tissue remodeling, and cell survival | journal = J. Clin. Invest. | volume = 107 | issue = 9 | pages = 1055–61 | date = May 2001 | pmid = 11342566 | pmc = 209291 | doi = 10.1172/JCI12980 }}</ref><ref name="PMID15494684">{{cite journal | vauthors = Standal T, Borset M, Sundan A | title = Role of osteopontin in adhesion, migration, cell survival and bone remodeling | journal = Exp. Oncol. | volume = 26 | issue = 3 | pages = 179–84 | date = September 2004 | pmid = 15494684 | doi = }}</ref> OPN prevents non-programmed cell death in inflammatory colitis.<ref name="PMID16741956">{{cite journal | vauthors = Da Silva AP, Pollett A, Rittling SR, Denhardt DT, Sodek J, Zohar R | title = Exacerbated tissue destruction in DSS-induced acute colitis of OPN-null mice is associated with downregulation of TNF-alpha expression and non-programmed cell death | journal = J. Cell. Physiol. | volume = 208 | issue = 3 | pages = 629–39 | date = September 2006 | pmid = 16741956 | doi = 10.1002/jcp.20701 }}</ref> | |||
== Potential clinical application == | |||
The fact that OPN interacts with multiple cell surface receptors that are ubiquitously expressed makes it an active player in many physiological and pathological processes including wound healing, bone turnover, tumorigenesis, inflammation, ischemia, and immune responses1. Therefore, manipulation of plasma (or local) OPN levels may be useful in the treatment of autoimmune diseases, cancer metastasis, bone (and tooth) mineralization diseases, [[osteoporosis]], and some forms of stress.<ref name="WangKX"/> | |||
===Role in autoimmune diseases === | |||
OPN has been implicated in pathogenesis of [[rheumatoid arthritis]]. For instance, researchers found that OPN-R, the thrombin-cleaved form of OPN, was elevated in the rheumatoid arthritis joint. However, the role of OPN in rheumatoid arthritis is still unclear. One group found that OPN knock-out mice were protected against arthritis.<ref name="Yumoto">{{cite journal | vauthors = Yumoto K, Ishijima M, Rittling SR, Tsuji K, Tsuchiya Y, Kon S, Nifuji A, Uede T, Denhardt DT, Noda M | title = Osteopontin deficiency protects joints against destruction in anti-type II collagen antibody-induced arthritis in mice | journal = Proc. Natl. Acad. Sci. U.S.A. | volume = 99 | issue = 7 | pages = 4556–61 | date = April 2002 | pmid = 11930008 | pmc = 123686 | doi = 10.1073/pnas.052523599 }}</ref> while others were not able to reproduce this observation.<ref name="Jacobs">{{cite journal | vauthors = Jacobs JP, Pettit AR, Shinohara ML, Jansson M, Cantor H, Gravallese EM, Mathis D, Benoist C | title = Lack of requirement of osteopontin for inflammation, bone erosion, and cartilage damage in the K/BxN model of autoantibody-mediated arthritis | journal = Arthritis Rheum. | volume = 50 | issue = 8 | pages = 2685–94 | date = August 2004 | pmid = 15334485 | doi = 10.1002/art.20381 }}</ref> OPN has been found to play a role in other autoimmune diseases including [[autoimmune hepatitis]], allergic airway disease, and [[multiple sclerosis]].<ref name="Chabas">{{cite journal | vauthors = Chabas D, Baranzini SE, Mitchell D, Bernard CC, Rittling SR, Denhardt DT, Sobel RA, Lock C, Karpuj M, Pedotti R, Heller R, Oksenberg JR, Steinman L | title = The influence of the proinflammatory cytokine, osteopontin, on autoimmune demyelinating disease | journal = Science | volume = 294 | issue = 5547 | pages = 1731–5 | date = November 2001 | pmid = 11721059 | doi = 10.1126/science.1062960 }}</ref> | |||
===Role in cancers and inflammatory diseases === | |||
It has been shown that OPN drives [[Interleukin 17|IL-17]] production;<ref name="pmid17290272">{{cite journal | vauthors = Steinman L | title = A brief history of T(H)17, the first major revision in the T(H)1/T(H)2 hypothesis of T cell-mediated tissue damage | journal = Nat. Med. | volume = 13 | issue = 2 | pages = 139–45 | date = February 2007 | pmid = 17290272 | doi = 10.1038/nm1551 }}</ref> OPN is [[gene expression|overexpressed]] in a variety of [[cancer]]s, including [[lung cancer]], [[breast cancer]], [[colorectal cancer]], [[stomach cancer]], [[ovarian cancer]], papillary thyroid carcinoma, [[melanoma]] and [[pleural]] mesothelioma; OPN contributes both [[glomerulonephritis]] and [[tubulointerstitial nephritis]]; and OPN is found in [[atheromatous plaques]] within [[arteries]]. Thus, manipulation of plasma OPN levels may be useful in the treatment of autoimmune diseases, cancer metastasis, osteoporosis and some forms of stress.<ref name="WangKX" /> | |||
Research has implicated osteopontin in excessive scar-forming and a gel has been developed to inhibit its effect.<ref name="urlBBC NEWS | Health | Gel to speed up wound healing">{{cite web | url = http://news.bbc.co.uk/2/hi/health/7199897.stm | title = Gel 'to speed up wound healing' | author = | authorlink = | date = 2008-01-22 | format = | website = Health | publisher = BBC NEWS | pages = | archiveurl = | archivedate = | quote = | accessdate = 2009-01-26}}</ref> | |||
===Role in colitis === | |||
Opn is up-regulated in [[inflammatory bowel disease]] (IBD).<ref name="Gassler">{{cite journal | vauthors = Gassler N, Autschbach F, Gauer S, Bohn J, Sido B, Otto HF, Geiger H, Obermüller N | title = Expression of osteopontin (Eta-1) in Crohn disease of the terminal ileum | journal = Scand J Gastroenterol | volume = 37 | issue = 11| pages = 1286–95 | date = November 2002 | pmid = 12465727 | doi = 10.1080/003655202761020560}}</ref> Opn expression is highly up-regulated in intestinal immune and non-immune cells and in the plasma of patients with [[Crohn's disease|Crohn’s disease]] (CD) and [[ulcerative colitis]] (UC), as well as in the colon and plasma of mice with experimental colitis.<ref name="Gassler"/><ref name="Sato">{{cite journal | vauthors = Sato T, Nakai T, Tamura N, Okamoto S, Matsuoka K, Sakuraba A, Fukushima T, Uede T, Hibi T | title = Osteopontin/Eta-1 upregulated in Crohn's disease regulates the Th1 immune response | journal = Gut | volume = 54 | issue = 9| pages = 1254–62 | date = September 2005 | pmid = 16099792 | |||
| doi = 10.1136/gut.2004.048298 | pmc=1774642}}</ref><ref name="Mishima">{{cite journal | vauthors = Mishima R, Takeshima F, Sawai T, Ohba K, Ohnita K, Isomoto H, Omagari K, Mizuta Y, Ozono Y, Kohno S | title = High plasma osteopontin levels in patients with inflammatory bowel disease | journal = J Clin Gastroenterol| volume = 41 | issue = 2| pages = 167–72 | date = February 2007 | pmid = 17245215| doi = 10.1097/MCG.0b013e31802d6268}}</ref> Increased plasma Opn levels are related to the severity of CD inflammation, and certain Opn gene (Spp1) haplotypes are modifiers of CD susceptibility. Opn has also a proinflammatory role in TNBS- and dextran sulfate sodium (DSS)-induced colitis, which are mouse models for IBD. Opn was found highly expressed by a specific dendritic cell (DC) subset derived from murine mesenteric lymph nodes (MLNs)and is highly proinflammatory for colitis.<ref name="Kourepini">{{cite journal | vauthors = Kourepini E, Aggelakopoulou M, Alissafi T, Paschalidis N, Simoes DC, Panoutsakopoulou V | title = Osteopontin expression by CD103- dendritic cells drives intestinal inflammation | journal = Proc Natl Acad Sci U S A | volume = 111 | issue = 9| pages = E856–E865 | date = March 2014 | pmid = 24550510 | doi = 10.1073/pnas.1316447111 | pmc=3948306}}</ref> Dendritic cells are important for the development of intestinal inflammation in humans with IBD and in mice with experimental colitis. Opn expression by this inflammatory MLN DC subset is crucial for their pathogenic action during colitis.<ref name="Kourepini"/> | |||
===Role in allergy and asthma === | |||
Osteopontin has recently been associated with [[allergic inflammation]] and [[asthma]]. Expression of Opn is significantly increased in lung epithelial and subepithelial cells of asthmatic patients in comparison to healthy subjects.<ref name="Xanthou">{{cite journal | vauthors = Xanthou G, Alissafi T, Semitekolou M, Simoes DC, Economidou E, Gaga M, Lambrecht BN, Lloyd CM, Panoutsakopoulou V | title = Osteopontin has a crucial role in allergic airway disease through regulation of dendritic cell subsets | journal = Nat. Med. | volume = 13 | issue = 5 | pages = 570–9 | date = May 2007 | pmid = 17435770 | doi = 10.1038/nm1580 | pmc = 3384679 }}</ref> Opn expression is also upregulated in lungs of mice with allergic airway inflammation.<ref name="Xanthou"/> The secreted form of Opn (Opn-s) plays a proinflammatory role during allergen sensitization (OVA/Alum), as neutralization of Opn-s during that phase results in significantly milder allergic airway inflammation.<ref name="Xanthou"/> In contrast, neutralization of Opn-s during antigenic challenge exacerbates allergic airway disease.<ref name="Xanthou"/> These effects of Opn-s are mainly mediated by the regulation of Th2-suppressing plasmacytoid dendritic cells (DCs) during primary sensitization and Th2-promoting conventional DCs during secondary antigenic challenge.<ref name="Xanthou"/> OPN deficiency was also reported to protect against remodeling and [[bronchial hyperresponsiveness]] (BHR), again using a chronic allergen-challenge model of airway remodeling.<ref name="Simoes">{{cite journal | vauthors = Simoes DC, Xanthou G, Petrochilou K, Panoutsakopoulou V, Roussos C, Gratziou C | title = Osteopontin deficiency protects against airway remodeling and hyperresponsiveness in chronic asthma | journal = Am J Respir Crit Care Med | volume = 179 | issue = 10 | pages = 894–902 | date = May 2009 | pmid = 19234104 | doi = 10.1164/rccm.200807-1081OC }}</ref> Furthermore, it was recently demonstrated that OPN expression is upregulated in human asthma, is associated with remodeling changes and its subepithelial expression correlates to disease severity.<ref name="Samitas">{{cite journal | vauthors = Samitas K, Zervas E, Vittorakis S, Semitekolou M, Alissafi T, Bossios A, Gogos H, Economidou E, Lötvall J, Xanthou G, Panoutsakopoulou V, Gaga M | title = Osteopontin expression and relation to disease severity in human asthma | journal = Eur. Respir. J. | volume = 37 | issue = 2 | pages = 331–41 | year = 2010 | pmid = 20562127 | doi = 10.1183/09031936.00017810 }}</ref> OPN has also been reported to be increased in the [[sputum]] supernatant of smoking asthmatics,<ref name="Hillas">{{cite journal | vauthors = Hillas G, Loukides S, Kostikas K, Simoes D, Petta V, Konstantellou E, Emmanouil P, Papiris S, Koulouris N, Bakakos P | title = Increased levels of osteopontin in sputum supernatant of smoking asthmatics | journal = Cytokine | volume = 61 | issue = 1 | pages = 251–5 | date = Jan 2013 | pmid = 23098767 | doi = 10.1016/j.cyto.2012.10.002 }}</ref> as well as the [[BALF]] and bronchial tissue of smoking controls and asthmatics.<ref name="Samitas2">{{cite journal | vauthors = Samitas K, Zervas E, Xanthou G, Panoutsakopoulou V, Gaga M | title = Osteopontin is increased in the bronchoalveolar lavage fluid and bronchial tissue of smoking asthmatics | journal = Cytokine | volume = 61 | issue = 3 | pages = 713–5 | date = Feb 2013 | pmid = 23384656 | doi = 10.1016/j.cyto.2012.12.028 }}</ref> | |||
===Role in muscle disease and injury === | |||
Evidence is accumulating that suggests that osteopontin plays a number of roles in diseases of [[skeletal muscle]], such as [[Duchenne muscular dystrophy]]. Osteopontin has been described as a component of the inflammatory environment of dystrophic and injured muscles,<ref name="Uaesoontrachoon" /><ref name="Porter">{{cite journal | vauthors = Porter JD, Khanna S, Kaminski HJ, Rao JS, Merriam AP, Richmonds CR, Leahy P, Li J, Guo W, Andrade FH | title = A chronic inflammatory response dominates the skeletal muscle molecular signature in dystrophin-deficient mdx mice | journal = Hum Mol Genet | volume = 11 | issue = 3 | pages = 263–72 | date = May 2002 | pmid = 11823445 | doi = 10.1093/hmg/11.3.263 }}</ref><ref name="Haslett">{{cite journal | vauthors = Haslett JN, Sanoudou D, Kho AT, Bennett RR, Greenberg SA, Kohane IS, Beggs AH, Kunkel LM | title = Gene expression comparison of biopsies from Duchenne muscular dystrophy (DMD) and normal skeletal muscle | journal = Proc Natl Acad Sci U S A | volume = 99 | issue = 23 | pages = 15000–15005 | year = 2002 | pmid = 12415109 | pmc = 137534 | doi = 10.1073/pnas.192571199 }}</ref><ref name="Hirata">{{cite journal | vauthors = Hirata A, Masuda S, Tamura T, Kai K, Ojima K, Fukase A, Motoyoshi K, Kamakura K, Miyagoe-Suzuki Y, Takeda S | title = Expression profiling of cytokines and related genes in regenerating skeletal muscle after cardiotoxin injection: a role for osteopontin | journal = Am J Pathol | volume = 163 | issue = 1 | pages = 203–215 | year = 2003 | pmid = 12819025 | pmc = 1868192 | doi = 10.1016/S0002-9440(10)63644-9 }}</ref> and has also been shown to increase scarring of diaphragm muscles of aged dystrophic mice.<ref name="Vetrone">{{cite journal | vauthors = Vetrone SA, Montecino-Rodriguez E, Kudryashova E, Kramerova I, Hoffman EP, Liu SD, Miceli MC, Spencer MJ | title = Osteopontin promotes fibrosis in dystrophic mouse muscle by modulating immune cell subsets and intramuscular TGF-beta | journal = J Clin Invest | volume = 119 | issue = 6 | pages = 1583–1594 | year = 2009 | pmid = 19451692 | pmc = 2689112 | doi = 10.1172/JCI37662 }}</ref> A recent study has identified osteopontin as a determinant of disease severity in patients with [[Duchenne muscular dystrophy]].<ref name="Pegoraro">{{cite journal | vauthors = Pegoraro E, Hoffman EP, Piva L, Gavassini BF, Cagnin S, Ermani M, Bello L, Soraru G, Pacchioni B, Bonifati MD, Lanfranchi G, Angelini C, Kesari A, Lee I, Gordish-Dressman H, Devaney JM, McDonald CM | title = SPP1 genotype is a determinant of disease severity in Duchenne muscular dystrophy | journal = Neurology | volume = 76 | issue = 3 | pages = 219–226 | year = 2011 | pmid = 21178099 | pmc = 3034396 | doi = 10.1212/WNL.0b013e318207afeb }}</ref> This study found that a mutation in the osteopontin gene promoter, known to cause low levels of osteopontin expression, is associated with a decrease in age to loss of ambulation and muscle strength in patients with [[Duchenne muscular dystrophy]]. | |||
===Role in hip osteoarthritis === | |||
An increase in Plasma OPN levels has been observed in patients with idiopathic hip OA. Furthermore, a correlation between OPN plasma levels and the severity of the disease has been noted.<ref name="pmid27229171">{{cite journal | vauthors = El Deeb S, Abdelnaby R, Khachab A, Bläsius K, Tingart M, Rath B | title = Osteopontin as a biochemical marker and severity indicator for idiopathic hip osteoarthritis | journal = Hip International : The Journal of Clinical and Experimental Research on Hip Pathology and Therapy | volume = 26 | issue = 4 | pages = 397–403 | date = July 2016 | pmid = 27229171 | doi = 10.5301/hipint.5000361 }}</ref> | |||
== Role in implantation == | |||
OPN is expressed in endometrial cells during implantation. Due to the production of progesterone by the ovaries, OPN is up-regulated immensely to aid in this process. The endometrium must undergo decidualization, the process in which the endometrium undergoes changes to prepare for implantation, which will lead to the attachment of the embryo. The endometrium houses stromal cells that will differentiate to produce an optimal environment for the embryo to attach (decidualization). OPN is a vital protein for stromal cell proliferation and differentiation as well as it binds to the receptor αvβ3 to assist with adhesion. OPN along with decidualization ultimately encourages the successful implantation of the early embryo. A OPN gene knock-out results in attachment instability at the maternal-fetal interface.<ref name="pmid24442579">{{cite journal | vauthors = Kang YJ, Forbes K, Carver J, Aplin JD | title = The role of the osteopontin-integrin αvβ3 interaction at implantation: functional analysis using three different in vitro models | journal = Human Reproduction (Oxford, England) | volume = 29 | issue = 4 | pages = 739–49 | year = 2014 | pmid = 24442579 | doi = 10.1093/humrep/det433 }}</ref><ref name="pmid12890718">{{cite journal | vauthors = Johnson GA, Burghardt RC, Bazer FW, Spencer TE | title = Osteopontin: roles in implantation and placentation | journal = Biology of Reproduction | volume = 69 | issue = 5 | pages = 1458–71 | year = 2003 | pmid = 12890718 | doi = 10.1095/biolreprod.103.020651 }}</ref> | |||
==References== | == References == | ||
{{reflist|2}} | {{reflist|2}} | ||
| Line 66: | Line 138: | ||
</gallery> | </gallery> | ||
==Further reading== | == Further reading == | ||
{{refbegin | 2}} | {{refbegin | 2}} | ||
* {{cite journal | vauthors = Fujisawa R | title = [Recent advances in research on bone matrix proteins] | journal = Nippon Rinsho | volume = Suppl 3 | issue = | pages = 72–8 | year = 2002 | pmid = 11979972 | doi = | series = 60 }} | |||
* {{cite journal | vauthors = Denhardt DT, Mistretta D, Chambers AF, Krishna S, Porter JF, Raghuram S, Rittling SR | title = Transcriptional regulation of osteopontin and the metastatic phenotype: evidence for a Ras-activated enhancer in the human OPN promoter | journal = Clin. Exp. Metastasis | volume = 20 | issue = 1 | pages = 77–84 | year = 2003 | pmid = 12650610 | doi = 10.1023/A:1022550721404 }} | |||
*{{cite journal | * {{cite journal | vauthors = Yeatman TJ, Chambers AF | title = Osteopontin and colon cancer progression | journal = Clin. Exp. Metastasis | volume = 20 | issue = 1 | pages = 85–90 | year = 2003 | pmid = 12650611 | doi = 10.1023/A:1022502805474 }} | ||
*{{cite journal | * {{cite journal | vauthors = O'Regan A | title = The role of osteopontin in lung disease | journal = Cytokine Growth Factor Rev. | volume = 14 | issue = 6 | pages = 479–88 | year = 2004 | pmid = 14563350 | doi = 10.1016/S1359-6101(03)00055-8 }} | ||
*{{cite journal | * {{cite journal | vauthors = Wai PY, Kuo PC | title = The role of Osteopontin in tumor metastasis | journal = J. Surg. Res. | volume = 121 | issue = 2 | pages = 228–41 | year = 2004 | pmid = 15501463 | doi = 10.1016/j.jss.2004.03.028 }} | ||
*{{cite journal | * {{cite journal | vauthors = Konno S, Hizawa N, Nishimura M, Huang SK | title = Osteopontin: a potential biomarker for successful bee venom immunotherapy and a potential molecule for inhibiting IgE-mediated allergic responses | journal = Allergology International | volume = 55 | issue = 4 | pages = 355–9 | year = 2007 | pmid = 17130676 | doi = 10.2332/allergolint.55.355 }} | ||
*{{cite journal | * {{cite journal | vauthors = Rodrigues LR, Teixeira JA, Schmitt FL, Paulsson M, Lindmark-Mänsson H | title = The role of osteopontin in tumor progression and metastasis in breast cancer | journal = Cancer Epidemiol. Biomarkers Prev. | volume = 16 | issue = 6 | pages = 1087–97 | year = 2007 | pmid = 17548669 | doi = 10.1158/1055-9965.EPI-06-1008 }} | ||
*{{cite journal | * {{cite journal | vauthors = Ramaiah SK, Rittling S | title = Role of osteopontin in regulating hepatic inflammatory responses and toxic liver injury | journal = Expert Opinion on Drug Metabolism & Toxicology | volume = 3 | issue = 4 | pages = 519–26 | year = 2007 | pmid = 17696803 | doi = 10.1517/17425225.3.4.519 }} | ||
*{{cite journal | |||
*{{cite journal | |||
}} | |||
{{refend}} | {{refend}} | ||
==External links== | == External links == | ||
* {{MeshName|Osteopontin}} | * {{MeshName|Osteopontin}} | ||
{{Cytokines}} | {{Cytokines}} | ||
[[ | {{Cytokine receptor ligands}} | ||
[[ | |||
[[Category:Glycoproteins]] | |||
[[Category:Extracellular matrix proteins]] | |||
[[Category:Matricellular proteins]] | |||
Latest revision as of 18:20, 17 January 2019
| VALUE_ERROR (nil) | |||||||
|---|---|---|---|---|---|---|---|
| Identifiers | |||||||
| Aliases | |||||||
| External IDs | GeneCards: [1] | ||||||
| Orthologs | |||||||
| Species | Human | Mouse | |||||
| Entrez |
|
| |||||
| Ensembl |
|
| |||||
| UniProt |
|
| |||||
| RefSeq (mRNA) |
|
| |||||
| RefSeq (protein) |
|
| |||||
| Location (UCSC) | n/a | n/a | |||||
| PubMed search | n/a | n/a | |||||
| Wikidata | |||||||
| |||||||
| Osteopontin | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Identifiers | |||||||||
| Symbol | Osteopontin | ||||||||
| Pfam | PF00865 | ||||||||
| InterPro | IPR002038 | ||||||||
| PROSITE | PDOC00689 | ||||||||
| |||||||||
- Not to be confused with Osteocalcin, Osteonectin or Osteoprotegerin (OPG).
Osteopontin (OPN), also known as bone sialoprotein I (BSP-1 or BNSP), early T-lymphocyte activation (ETA-1), secreted phosphoprotein 1 (SPP1), 2ar and Rickettsia resistance (Ric),[1] is a protein that in humans is encoded by the SPP1 gene (secreted phosphoprotein 1). The murine ortholog is Spp1. Osteopontin is a SIBLING (glycoprotein) that was first identified in 1986 in osteoblasts.
The prefix osteo- indicates that the protein is expressed in bone, although it is also expressed in other tissues. The suffix -pontin is derived from "pons," the Latin word for bridge, and signifies osteopontin's role as a linking protein. Osteopontin is an extracellular structural protein and therefore an organic component of bone. Synonyms for this protein include sialoprotein I and 44K BPP (bone phosphoprotein).
The gene has 7 exons, spans 5 kilobases in length and in humans it is located on the long arm of chromosome 4 region 22 (4q1322.1). The protein is composed of ~300 amino acids residues and has ~30 carbohydrate residues attached including 10 sialic acid residues, which are attached to the protein during post-translational modification in the Golgi apparatus. The protein is rich in acidic residues: 30-36% are either aspartic or glutamic acid.
Structure
General structure
OPN is a highly negatively charged, extracellular matrix protein that lacks an extensive secondary structure.[2] It is composed of about 300 amino acids (297 in mouse; 314 in human) and is expressed as a 33-kDa nascent protein; there are also functionally important cleavage sites. OPN can go through posttranslational modifications, which increase its apparent molecular weight to about 44 kDa.[3] The OPN gene is composed of 7 exons, 6 of which containing coding sequence.[4][5] The first two exons contain the 5' untranslated region (5' UTR).[6] Exons 2, 3, 4, 5, 6, and 7 code for 17, 13, 27, 14, 108 and 134 amino acids, respectively.[6] All intron-exon boundaries are of the phase 0 type, thus alternative exon splicing maintains the reading frame of the OPN gene.
Isoforms
Full-length OPN (OPN-FL) can be modified by thrombin cleavage, which exposes a cryptic sequence, SVVYGLR on the cleaved form of the protein known as OPN-R (Fig. 1). This thrombin-cleaved OPN (OPN-R) exposes an epitope for integrin receptors of α4β1, α9β1, and α9β4.[7][8] These integrin receptors are present on a number of immune cells such as mast cells,[9] neutrophils,[10] and T cells. It is also expressed by monocytes and macrophages.[11] Upon binding these receptors, cells use several signal transduction pathways to elicit immune responses in these cells. OPN-R can be further cleaved by Carboxypeptidase B (CPB) by removal of C-terminal arginine and become OPN-L. The function of OPN-L is largely unknown.
It appears an intracellular variant of OPN (iOPN) is involved in a number of cellular processes including migration, fusion and motility.[12][13][14][15] Intracellular OPN is generated using an alternative translation start site on the same mRNA species used to generate the extracellular isoform.[16] This alternative translation start site is downstream of the N-terminal endoplasmic reticulum-targeting signal sequence, thus allowing cytoplasmic translation of OPN.
Various human cancers, including breast cancer, have been observed to express splice variants of OPN.[17][18] The cancer-specific splice variants are osteopontin-a, osteopontin-b, and osteopontin-c. Exon 5 is lacking from osteopontin-b, whereas osteopontin-c lacks exon 4.[17] Osteopontin-c has been suggested to facilitate the anchorage-independent phenotype of some human breast cancer cells due to its inability to associate with the extracellular matrix.[17]
Biosynthesis
Osteopontin is biosynthesized by a variety of tissue types including cardiac fibroblasts,[19] preosteoblasts, osteoblasts, osteocytes, odontoblasts, some bone marrow cells, hypertrophic chondrocytes, dendritic cells, macrophages,[20] smooth muscle,[21] skeletal muscle myoblasts,[22] endothelial cells, and extraosseous (non-bone) cells in the inner ear, brain, kidney, deciduum, and placenta. Synthesis of osteopontin is stimulated by calcitriol (1,25-dihydroxy-vitamin D3).
Regulation
Regulation of the osteopontin gene is incompletely understood. Different cell types may differ in their regulatory mechanisms of the OPN gene. OPN expression in bone predominantly occurs by osteoblasts and osteocyctes (bone-forming cells) as well as osteoclasts (bone-resorbing cells).[23] Runx2 (aka Cbfa1) and osterix (Osx) transcription factors are required for the expression of OPN [24] Runx2 and Osx bind promoters of osteoblast-specific genes such as Col1α1, Bsp, and Opn and upregulate transcription.[25]
Hypocalcemia and hypophosphatemia (instances that stimulate kidney proximal tubule cells to produce calcitriol (1α,25-dihydroxyvitamin D3)) lead to increases in OPN transcription, translation and secretion.[26] This is due to the presence of a high-specificity vitamin D response element (VDRE) in the OPN gene promoter.[27][28][29]
Extracellular inorganic phosphate (ePi) has also been identified as a modulator of OPN expression.[30]
Stimulation of OPN expression also occurs upon exposure of cells to pro-inflammatory cytokines,[31] classical mediators of acute inflammation (e.g. tumour necrosis factor α [TNFα], infterleukin-1β [IL-1β]), angiotensin II, transforming growth factor β (TGFβ) and parathyroid hormone (PTH),[32][33] although a detailed mechanistic understanding of these regulatory pathways are not yet known. Hyperglycemia and hypoxia are also known to increase OPN expression.[32][34][35]
Biological function
Role in biomineralization
OPN belongs to a family of secreted acidic proteins whose members have an abundance of negatively charged amino acids such as Asp and Glu.[36] OPN also has a large number of consensus sequence sites for post-translational phosphorylation of Ser residues to form phosphoserine, providing additional negative charge.[37] Contiguous stretches of high negative charge in OPN have been identified and named the polyAsp motif (poly-aspartic acid) and the ASARM motif (acidic serine- and aspartate-rich motif), with the latter sequence having multiple phosphorylation sites.[38][39][40][41] This overall negative charge of OPN, along with its specific acidic motifs and the fact that OPN is an intrinsically disordered protein[42][43] allowing for open and flexible structures, permit OPN to bind strongly to calcium atoms available at crystal surfaces in various biominerals.[41][44][45] Such binding of OPN to various types of calcium-based biominerals ‒ such as calcium-phosphate mineral in bones and teeth,[46] calcium-carbonate mineral in inner ear otoconia[47] and avian eggshells,[48] and calcium-oxalate mineral in kidney stones[49][50][51] – acts as a mineralization inhibitor to regulate crystal growth.[52]
OPN is a substrate protein for a number of enzymes whose actions may modulate the mineralization-inhibiting function of OPN. PHEX (phosphate-regulating gene with homologies to endopeptidases on the X chromosome) is one such enzyme, which extensively degrades OPN, and whose inactivating gene mutations (in X-linked hypophosphatemia, XLH) lead to altered processing of OPN such that inhibitory OPN cannot be degraded and accumulates in the bone (and tooth) extracellular matrix, likely contributing locally to the osteomalacia (soft hypomineralized bones) characteristic of XLH.[53][54][55]
Along with its role in the regulation of normal mineralization within the extracellular matrices of bones and teeth,[56] OPN is also upregulated at sites of pathologic, ectopic calcification[57][58] – such as for example, in urolithiasis and vascular calcification ‒ presumably at least in part to inhibit debilitating mineralization in these soft tissues.
Role in bone remodeling
Osteopontin has been implicated as an important factor in bone remodeling.[59] Specifically, research suggests it plays a role in anchoring osteoclasts to the mineral matrix of bones.[9] The organic part of bone is about 20% of the dry weight, and counts in, other than osteopontin, collagen type I, osteocalcin, osteonectin, bone sialo protein, and alkaline phosphatase. Collagen type I counts for 90% of the protein mass. The inorganic part of bone is the mineral hydroxyapatite, Ca10(PO4)6(OH)2. Loss of this mineral may lead to osteoporosis, as the bone is depleted for calcium if this is not supplied in the diet.
OPN serves to initiate the process by which osteoclasts develop their ruffled borders to begin bone resorption. It is also found in urine, where it inhibits kidney stone formation.
Role in immune functions
As discussed, OPN binds to several integrin receptors including α4β1, α9β1, and α9β4 expressed by leukocytes. These receptors have been well-established to function in cell adhesion, migration, and survival in these cells. Therefore, recent research efforts have focused on the role of OPN in mediating such responses.
Osteopontin (OPN) is expressed in a range of immune cells, including macrophages, neutrophils, dendritic cells, and T and B cells, with varying kinetics. OPN is reported to act as an immune modulator in a variety of manners.[2] Firstly, it has chemotactic properties, which promote cell recruitment to inflammatory sites. It also functions as an adhesion protein, involved in cell attachment and wound healing. In addition, OPN mediates cell activation and cytokine production, as well as promoting cell survival by regulating apoptosis.[2] The following examples are found.[2]
Role in Heart
OPN expression increases under a variety of conditions of the heart, and is associated with increased myocyte apoptosis and myocardial dysfunction.[60]
Chemotaxis
OPN plays an important role in neutrophil recruitment in alcoholic liver disease.[10][61] OPN is important for the migration of neutrophil in vitro.[62] In addition, OPN recruits inflammatory cells to arthritis joints in the collagen-induced arthritis model of rheumatoid arthritis.[63][64] A recent in vitro study in 2008 has found that OPN plays a role in mast cell migration.[65] Here OPN knock-out mast cells were cultured and they observed a decreased level of chemotaxis in these cells compared to wildtype mast cells. OPN was also found to act as a macrophage chemotactic factor.[66] In this study, researchers looked at the accumulation of macrophages in the brain of rhesus monkeys and found that OPN prevented macrophages from leaving the accumulation site, indicating an increased level of chemotaxis.
Cell activation
Activated T cells are promoted by IL-12 to differentiate towards the Th1 type, producing cytokines including IL-12 and IFNγ. OPN inhibits production of the Th2 cytokine IL-10, which leads to enhanced Th1 response. OPN influences cell-mediated immunity and has Th1 cytokine functions. It enhances B cell immunoglobulin production and proliferation.[2] Recent studies in 2008 suggest that OPN also induces mast cell degranulation.[65] The researchers here observed that IgE-mediated anaphylaxis was significantly reduced in OPN knock-out mice compared to wild-type mice. The role of OPN in activation of macrophages has also been implicated in a cancer study, when researchers discovered that OPN-producing tumors were able to induce macrophage activation compared to OPN-deficient tumors.[67]
Apoptosis
OPN is an important anti-apoptotic factor in many circumstances. OPN blocks the activation-induced cell death of macrophages and T cells as well as fibroblasts and endothelial cells exposed to harmful stimuli.[68][69] OPN prevents non-programmed cell death in inflammatory colitis.[70]
Potential clinical application
The fact that OPN interacts with multiple cell surface receptors that are ubiquitously expressed makes it an active player in many physiological and pathological processes including wound healing, bone turnover, tumorigenesis, inflammation, ischemia, and immune responses1. Therefore, manipulation of plasma (or local) OPN levels may be useful in the treatment of autoimmune diseases, cancer metastasis, bone (and tooth) mineralization diseases, osteoporosis, and some forms of stress.[2]
Role in autoimmune diseases
OPN has been implicated in pathogenesis of rheumatoid arthritis. For instance, researchers found that OPN-R, the thrombin-cleaved form of OPN, was elevated in the rheumatoid arthritis joint. However, the role of OPN in rheumatoid arthritis is still unclear. One group found that OPN knock-out mice were protected against arthritis.[71] while others were not able to reproduce this observation.[72] OPN has been found to play a role in other autoimmune diseases including autoimmune hepatitis, allergic airway disease, and multiple sclerosis.[73]
Role in cancers and inflammatory diseases
It has been shown that OPN drives IL-17 production;[74] OPN is overexpressed in a variety of cancers, including lung cancer, breast cancer, colorectal cancer, stomach cancer, ovarian cancer, papillary thyroid carcinoma, melanoma and pleural mesothelioma; OPN contributes both glomerulonephritis and tubulointerstitial nephritis; and OPN is found in atheromatous plaques within arteries. Thus, manipulation of plasma OPN levels may be useful in the treatment of autoimmune diseases, cancer metastasis, osteoporosis and some forms of stress.[2]
Research has implicated osteopontin in excessive scar-forming and a gel has been developed to inhibit its effect.[75]
Role in colitis
Opn is up-regulated in inflammatory bowel disease (IBD).[76] Opn expression is highly up-regulated in intestinal immune and non-immune cells and in the plasma of patients with Crohn’s disease (CD) and ulcerative colitis (UC), as well as in the colon and plasma of mice with experimental colitis.[76][77][78] Increased plasma Opn levels are related to the severity of CD inflammation, and certain Opn gene (Spp1) haplotypes are modifiers of CD susceptibility. Opn has also a proinflammatory role in TNBS- and dextran sulfate sodium (DSS)-induced colitis, which are mouse models for IBD. Opn was found highly expressed by a specific dendritic cell (DC) subset derived from murine mesenteric lymph nodes (MLNs)and is highly proinflammatory for colitis.[79] Dendritic cells are important for the development of intestinal inflammation in humans with IBD and in mice with experimental colitis. Opn expression by this inflammatory MLN DC subset is crucial for their pathogenic action during colitis.[79]
Role in allergy and asthma
Osteopontin has recently been associated with allergic inflammation and asthma. Expression of Opn is significantly increased in lung epithelial and subepithelial cells of asthmatic patients in comparison to healthy subjects.[80] Opn expression is also upregulated in lungs of mice with allergic airway inflammation.[80] The secreted form of Opn (Opn-s) plays a proinflammatory role during allergen sensitization (OVA/Alum), as neutralization of Opn-s during that phase results in significantly milder allergic airway inflammation.[80] In contrast, neutralization of Opn-s during antigenic challenge exacerbates allergic airway disease.[80] These effects of Opn-s are mainly mediated by the regulation of Th2-suppressing plasmacytoid dendritic cells (DCs) during primary sensitization and Th2-promoting conventional DCs during secondary antigenic challenge.[80] OPN deficiency was also reported to protect against remodeling and bronchial hyperresponsiveness (BHR), again using a chronic allergen-challenge model of airway remodeling.[81] Furthermore, it was recently demonstrated that OPN expression is upregulated in human asthma, is associated with remodeling changes and its subepithelial expression correlates to disease severity.[82] OPN has also been reported to be increased in the sputum supernatant of smoking asthmatics,[83] as well as the BALF and bronchial tissue of smoking controls and asthmatics.[84]
Role in muscle disease and injury
Evidence is accumulating that suggests that osteopontin plays a number of roles in diseases of skeletal muscle, such as Duchenne muscular dystrophy. Osteopontin has been described as a component of the inflammatory environment of dystrophic and injured muscles,[22][85][86][87] and has also been shown to increase scarring of diaphragm muscles of aged dystrophic mice.[88] A recent study has identified osteopontin as a determinant of disease severity in patients with Duchenne muscular dystrophy.[89] This study found that a mutation in the osteopontin gene promoter, known to cause low levels of osteopontin expression, is associated with a decrease in age to loss of ambulation and muscle strength in patients with Duchenne muscular dystrophy.
Role in hip osteoarthritis
An increase in Plasma OPN levels has been observed in patients with idiopathic hip OA. Furthermore, a correlation between OPN plasma levels and the severity of the disease has been noted.[90]
Role in implantation
OPN is expressed in endometrial cells during implantation. Due to the production of progesterone by the ovaries, OPN is up-regulated immensely to aid in this process. The endometrium must undergo decidualization, the process in which the endometrium undergoes changes to prepare for implantation, which will lead to the attachment of the embryo. The endometrium houses stromal cells that will differentiate to produce an optimal environment for the embryo to attach (decidualization). OPN is a vital protein for stromal cell proliferation and differentiation as well as it binds to the receptor αvβ3 to assist with adhesion. OPN along with decidualization ultimately encourages the successful implantation of the early embryo. A OPN gene knock-out results in attachment instability at the maternal-fetal interface.[91][92]
References
- ↑ "Entrez Gene: SPP1 secreted phosphoprotein 1".
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 Wang KX, Denhardt DT (2008). "Osteopontin: role in immune regulation and stress responses". Cytokine Growth Factor Rev. 19 (5–6): 333–45. doi:10.1016/j.cytogfr.2008.08.001. PMID 18952487.
- ↑ Rangaswami H, Bulbule A, Kundu GC (February 2006). "Osteopontin: role in cell signaling and cancer progression". Trends Cell Biol. 16 (2): 79–87. doi:10.1016/j.tcb.2005.12.005. PMID 16406521.
- ↑ Young MF, Kerr JM, Termine JD, Wewer UM, Wang MG, McBride OW, Fisher LW (August 1990). "cDNA cloning, mRNA distribution and heterogeneity, chromosomal location, and RFLP analysis of human osteopontin (OPN)" (Submitted manuscript). Genomics. 7 (1): 491–502. doi:10.1016/0888-7543(90)90191-V. PMID 1974876.
- ↑ Kiefer MC, Bauer DM, Barr PJ (April 1989). "The cDNA and derived amino acid sequence for human osteopontin". Nucleic Acids Res. 17 (1): 3306. doi:10.1093/nar/17.8.3306. PMC 317745. PMID 2726470.
- ↑ 6.0 6.1 Crosby AH, Edwards SJ, Murray JC, Dixon MJ (May 1995). "Genomic organization of the human osteopontin gene: exclusion of the locus from a causative role in the pathogenesis of dentinogenesis imperfecta type II". Genomics. 27 (1): 155–160. doi:10.1006/geno.1995.1018. PMID 7665163.
- ↑ Laffón A, García-Vicuña R, Humbría A, Postigo AA, Corbí AL, de Landázuri MO, Sánchez-Madrid F (August 1991). "Upregulated expression and function of VLA-4 fibronectin receptors on human activated T cells in rheumatoid arthritis". J. Clin. Invest. 88 (2): 546–52. doi:10.1172/JCI115338. PMC 295383. PMID 1830891.
- ↑ Seiffge D (December 1996). "Protective effects of monoclonal antibody to VLA-4 on leukocyte adhesion and course of disease in adjuvant arthritis in rats". J. Rheumatol. 23 (12): 2086–91. PMID 8970045.
- ↑ 9.0 9.1 Reinholt FP, Hultenby K, Oldberg A, Heinegård D (June 1990). "Osteopontin--a possible anchor of osteoclasts to bone". Proc. Natl. Acad. Sci. U.S.A. 87 (12): 4473–5. doi:10.1073/pnas.87.12.4473. PMC 54137. PMID 1693772.
- ↑ 10.0 10.1 Banerjee A, Apte UM, Smith R, Ramaiah SK (March 2006). "Higher neutrophil infiltration mediated by osteopontin is a likely contributing factor to the increased susceptibility of females to alcoholic liver disease". J. Pathol. 208 (4): 473–85. doi:10.1002/path.1917. PMID 16440289.
- ↑ Sodek J, Batista Da Silva AP, Zohar R (May 2006). "Osteopontin and mucosal protection". J. Dent. Res. 85 (5): 404–15. doi:10.1177/154405910608500503. PMID 16632752.
- ↑ Zohar R, Suzuki N, Suzuki K, Arora P, Glogauer M, McCulloch CA, Sodek J (July 2000). "Intracellular osteopontin is an integral component of the CD44-ERM complex involved in cell migration". J Cell Physiol. 184 (1): 118–130. doi:10.1002/(SICI)1097-4652(200007)184:1<118::AID-JCP13>3.0.CO;2-Y. PMID 10825241.
- ↑ Suzuki K, Zhu B, Rittling SR, Denhardt DT, Goldberg HA, McCulloch CA, Sodek J (August 2002). "Colocalization of intracellular osteopontin with CD44 is associated with migration, cell fusion, and resorption in osteoclasts". J Bone Miner Res. 17 (1): 1486–1497. doi:10.1359/jbmr.2002.17.8.1486. PMID 12162503.
- ↑ Zhu B, Suzuki K, Goldberg HA, Rittling SR, Denhardt DT, McCulloch CA, Sodek J (January 2004). "Osteopontin modulates CD44-dependent chemotaxis of peritoneal macrophages through G-protein-coupled receptors: evidence of a role for an intracellular form of osteopontin". Journal of Cellular Physiology. 198 (1): 155–167. doi:10.1002/jcp.10394. PMID 14584055.
- ↑ Junaid A, Moon MC, Harding GE, Zahradka P (February 2007). "Osteopontin localizes to the nucleus of 293 cells and associates with polo-like kinase-1". Am J Physiol Cell Physiol. 292 (1): 919–926. doi:10.1152/ajpcell.00477.2006. PMID 17005603.
- ↑ Shinohara ML, Kim HJ, Kim JH, Garcia VA, Cantor H (May 2008). "Alternative translation of osteopontin generates intracellular and secreted isoforms that mediate distinct biological activities in dendritic cells". Proc Natl Acad Sci USA. 105 (1): 7235–7239. doi:10.1073/pnas.0802301105. PMC 2438233. PMID 18480255.
- ↑ 17.0 17.1 17.2 He B, Mirza M, Weber GF (April 2006). "An osteopontin splice variant induces anchorage independence in human breast cancer cells". Oncogene. 25 (1): 2192–2202. doi:10.1038/sj.onc.1209248. PMID 16288209.
- ↑ Mirza M, Shaughnessy E, Hurley JK, Vanpatten KA, Pestano GA, He B, Weber GF (February 2008). "Osteopontin-c is a selective marker of breast cancer". Int J Cancer. 122 (1): 889–897. doi:10.1002/ijc.23204. PMID 17960616.
- ↑ Ashizawa N, Graf K, Do YS, Nunohiro T, Giachelli CM, Meehan WP, Tuan TL, Hsueh WA (November 1996). "Osteopontin is produced by rat cardiac fibroblasts and mediates A(II)-induced DNA synthesis and collagen gel contraction". J. Clin. Invest. 98 (10): 2218–27. doi:10.1172/JCI119031. PMC 507670. PMID 8941637.
- ↑ Murry CE, Giachelli CM, Schwartz SM, Vracko R (December 1994). "Macrophages express osteopontin during repair of myocardial necrosis". Am. J. Pathol. 145 (6): 1450–62. PMC 1887495. PMID 7992848.
- ↑ Ikeda T, Shirasawa T, Esaki Y, Yoshiki S, Hirokawa K (December 1993). "Osteopontin mRNA is expressed by smooth muscle-derived foam cells in human atherosclerotic lesions of the aorta". J. Clin. Invest. 92 (6): 2814–20. doi:10.1172/JCI116901. PMC 288482. PMID 8254036.
- ↑ 22.0 22.1 Uaesoontrachoon K, Yoo HJ, Tudor EM, Pike RN, Mackie EJ, Pagel CN (April 2008). "Osteopontin and skeletal muscle myoblasts: Association with muscle regeneration and regulation of myoblast function in vitro". Int. J. Biochem. Cell Biol. 40 (10): 2303–14. doi:10.1016/j.biocel.2008.03.020. PMID 18490187.
- ↑ Merry K, Dodds R, Littlewood A, Gowen M (April 1993). "Expression of Osteopontin mRNA by osteoclasts and osteoblasts in modelling adult human bone". J Cell Sci. 104 (4): 1013–1020. PMID 8314886.
- ↑ Nakashima K, Zhou X, Kunkel G, Zhang Z, Deng JM, Behringer RR, de Crombrugghe B (January 2002). "The novel zinc finger-containing transcription factor osterix is required for osteoblast differentiation and bone formation". Cell. 108 (1): 17–29. doi:10.1016/S0092-8674(01)00622-5. PMID 11792318.
- ↑ Ducy P, Zhang R, Geoffroy V, Ridall AL, Karsenty G (May 1997). "Osf2/Cbfa1: a transcriptional activator of osteoblast differentiation". Cell. 89 (1): 747–754. doi:10.1016/S0092-8674(00)80257-3. PMID 9182762.
- ↑ Yucha C, Guthrie D (December 2003). "Renal homeostasis of calcium". Nephrol Nurs J. 30 (1): 755–764. PMID 14730782.
- ↑ Prince CW, Butler WT (September 1987). "1,25-Dihydroxyvitamin D3 regulates the biosyntheis of osteopontin, a bone-derived cell attachment protein, in clonal osteoblast-like osteosarcoma cells". Coll Relat Res. 7 (1): 305–313. doi:10.1016/s0174-173x(87)80036-5. PMID 3478171.
- ↑ Oldberg A, Jirskog-Hed B, Axelsson S, Heinegård D (December 1989). "Regulation of bone sialoprotein mRNA by steroid hormones". J Cell Biol. 109 (1): 3183–3186. doi:10.1083/jcb.109.6.3183. PMC 2115918. PMID 2592421.
- ↑ Chang PL, Prince CW (May 1991). "1 alpha,25-Dihydroxyvitamin D3 enhances 12-O-tetradecanoylphorbol-13-acetate- induced tumorigenic transformation and osteopontin expression in mouse JB6 epidermal cells". Cancer Res. 51 (8): 2144–2150. PMID 2009532.
- ↑ Fatherazi S, Matsa-Dunn D, Foster BL, Rutherford RB, Somerman MJ, Presland RB (January 2009). "Phosphate regulates osteopontin gene transcription". J Dent Res. 88 (1): 39–44. doi:10.1177/0022034508328072. PMC 3128439. PMID 19131315.
- ↑ Guo H, Cai CQ, Schroeder RA, Kuo PC (January 2001). "Osteopontin is a negative feedback regulator of nitric oxide synthesis in murine macrophages". J Immunol. 166 (1): 1079–1086. doi:10.4049/jimmunol.166.2.1079. PMID 11145688.
- ↑ 32.0 32.1 Ricardo SD, Franzoni DF, Roesener CD, Crisman JM, Diamond JR (May 2000). "Angiotensinogen and AT(1) antisense inhibition of osteopontin translation in rat proximal tubular cells". Am J Physiol Renal Physiol. 278 (1): 708–716. doi:10.1152/ajprenal.2000.278.5.F708. PMID 10807582.
- ↑ Noda M, Rodan GA (February 1989). "Transcriptional regulation of osteopontin production in rat osteoblast-like cells by parathyroid hormone". J Cell Biol. 108 (1): 713–718. doi:10.1083/jcb.108.2.713. PMC 2115413. PMID 2465299.
- ↑ Hullinger TG, Pan Q, Viswanathan HL, Somerman MJ (January 2001). "TGFbeta and BMP-2 activation of the OPN promoter: roles of smad- and hox-binding elements". Exp Cell Res. 262 (1): 69–74. doi:10.1006/excr.2000.5074. PMID 11120606.
- ↑ Sodhi CP, Phadke SA, Batlle D, Sahai A (April 2001). "Hypoxia and high glucose cause exaggerated mesangial cell growth and collagen synthesis: role of osteopontin". Am J Physiol Renal Physiol. 280 (1): 667–674. doi:10.1152/ajprenal.2001.280.4.F667. PMID 11249858.
- ↑ Fisher LW, Fedarko NS (2003). "Six genes expressed in bones and teeth encode the current members of the SIBLING family of proteins". Connect. Tissue Res. 44 Suppl 1: 33–40. doi:10.1080/03008200390152061. PMID 12952171.
- ↑ Christensen B, Nielsen MS, Haselmann KF, Petersen TE, Sørensen ES (August 2005). "Post-translationally modified residues of native human osteopontin are located in clusters: identification of 36 phosphorylation and five O-glycosylation sites and their biological implications". Biochem. J. 390 (Pt 1): 285–92. doi:10.1042/BJ20050341. PMC 1184582. PMID 15869464.
- ↑ David V, Martin A, Hedge AM, Drezner MK, Rowe PS (March 2011). "ASARM peptides: PHEX-dependent and -independent regulation of serum phosphate". Am. J. Physiol. Renal Physiol. 300 (3): F783–91. doi:10.1152/ajprenal.00304.2010. PMC 3064126. PMID 21177780.
- ↑ Martin A, David V, Laurence JS, Schwarz PM, Lafer EM, Hedge AM, Rowe PS (April 2008). "Degradation of MEPE, DMP1, and release of SIBLING ASARM-peptides (minhibins): ASARM-peptide(s) are directly responsible for defective mineralization in HYP". Endocrinology. 149 (4): 1757–72. doi:10.1210/en.2007-1205. PMC 2276704. PMID 18162525.
- ↑ Addison WN, Nakano Y, Loisel T, Crine P, McKee MD (October 2008). "MEPE-ASARM peptides control extracellular matrix mineralization by binding to hydroxyapatite: an inhibition regulated by PHEX cleavage of ASARM". J. Bone Miner. Res. 23 (10): 1638–49. doi:10.1359/jbmr.080601. PMID 18597632.
- ↑ 41.0 41.1 Addison WN, Masica DL, Gray JJ, McKee MD (April 2010). "Phosphorylation-dependent inhibition of mineralization by osteopontin ASARM peptides is regulated by PHEX cleavage". J. Bone Miner. Res. 25 (4): 695–705. doi:10.1359/jbmr.090832. PMID 19775205.
- ↑ Kurzbach D, Platzer G, Schwarz TC, Henen MA, Konrat R, Hinderberger D (July 2013). "Cooperative Unfolding of Compact Conformations of the Intrinsically Disordered Protein Osteopontin". Biochemistry. 52 (31): 5167–75. doi:10.1021/bi400502c. PMC 3737600. PMID 23848319.
- ↑ Kalmar L, Homola D, Varga G, Tompa P (September 2012). "Structural disorder in proteins brings order to crystal growth in biomineralization". Bone. 51 (3): 528–34. doi:10.1016/j.bone.2012.05.009. PMID 22634174.
- ↑ Azzopardi PV, O'Young J, Lajoie G, Karttunen M, Goldberg HA, Hunter GK (2010). "Roles of electrostatics and conformation in protein-crystal interactions". PLoS ONE. 5 (2): e9330. doi:10.1371/journal.pone.0009330. PMC 2824833. PMID 20174473.
- ↑ Hunter GK, O'Young J, Grohe B, Karttunen M, Goldberg HA (December 2010). "The flexible polyelectrolyte hypothesis of protein-biomineral interaction". Langmuir. 26 (24): 18639–46. doi:10.1021/la100401r. PMID 20527831.
- ↑ McKee MD, Nanci A (May 1995). "Postembedding colloidal-gold immunocytochemistry of noncollagenous extracellular matrix proteins in mineralized tissues". Microsc. Res. Tech. 31 (1): 44–62. doi:10.1002/jemt.1070310105. PMID 7626799.
- ↑ Takemura T, Sakagami M, Nakase T, Kubo T, Kitamura Y, Nomura S (September 1994). "Localization of osteopontin in the otoconial organs of adult rats". Hear. Res. 79 (1–2): 99–104. doi:10.1016/0378-5955(94)90131-7. PMID 7806488.
- ↑ Hincke MT, Nys Y, Gautron J, Mann K, Rodriguez-Navarro AB, McKee MD (2012). "The eggshell: structure, composition and mineralization". Front. Biosci. 17: 1266–80. doi:10.2741/3985. PMID 22201802.
- ↑ McKee MD, Nanci A, Khan SR (December 1995). "Ultrastructural immunodetection of osteopontin and osteocalcin as major matrix components of renal calculi". J. Bone Miner. Res. 10 (12): 1913–29. doi:10.1002/jbmr.5650101211. PMID 8619372.
- ↑ O'Young J, Chirico S, Al Tarhuni N, Grohe B, Karttunen M, Goldberg HA, Hunter GK (2009). "Phosphorylation of osteopontin peptides mediates adsorption to and incorporation into calcium oxalate crystals". Cells Tissues Organs (Print). 189 (1–4): 51–5. doi:10.1159/000151724. PMID 18728346.
- ↑ Chien YC, Masica DL, Gray JJ, Nguyen S, Vali H, McKee MD (August 2009). "Modulation of calcium oxalate dihydrate growth by selective crystal-face binding of phosphorylated osteopontin and polyaspartate peptide showing occlusion by sectoral (compositional) zoning". J. Biol. Chem. 284 (35): 23491–501. doi:10.1074/jbc.M109.021899. PMC 2749123. PMID 19581305.
- ↑ Sodek J, Ganss B, McKee MD (2000). "Osteopontin". Crit. Rev. Oral Biol. Med. 11 (3): 279–303. doi:10.1177/10454411000110030101. PMID 11021631.
- ↑ McKee MD, Hoac B, Addison WN, Barros NM, Millán JL, Chaussain C (October 2013). "Extracellular matrix mineralization in periodontal tissues: Noncollagenous matrix proteins, enzymes, and relationship to hypophosphatasia and X-linked hypophosphatemia". Periodontology 2000. 63 (1): 102–22. doi:10.1111/prd.12029. PMC 3766584. PMID 23931057.
- ↑ Boukpessi T, Hoac B, Coyac BR, Leger T, Garcia C, Wicart P, Whyte MP, Glorieux FH, Linglart A, Chaussain C, McKee MD (February 2017). "Osteopontin and the dento-osseous pathobiology of X-linked hypophosphatemia". Bone. 95: 151–161. doi:10.1016/j.bone.2016.11.019. PMID 27884786.
- ↑ Barros NM, Hoac B, Neves RL, Addison WN, Assis DM, Murshed M, Carmona AK, McKee MD (March 2013). "Proteolytic processing of osteopontin by PHEX and accumulation of osteopontin fragments in Hyp mouse bone, the murine model of X-linked hypophosphatemia". Journal of Bone and Mineral Research. 28 (3): 688–99. doi:10.1002/jbmr.1766. PMID 22991293.
- ↑ McKee MD, Addison WN, Kaartinen MT (2005). "Hierarchies of extracellular matrix and mineral organization in bone of the craniofacial complex and skeleton". Cells Tissues Organs (Print). 181 (3–4): 176–88. doi:10.1159/000091379. PMID 16612083.
- ↑ Steitz SA, Speer MY, McKee MD, Liaw L, Almeida M, Yang H, Giachelli CM (December 2002). "Osteopontin inhibits mineral deposition and promotes regression of ectopic calcification". Am. J. Pathol. 161 (6): 2035–46. doi:10.1016/S0002-9440(10)64482-3. PMC 1850905. PMID 12466120.
- ↑ Giachelli CM (March 1999). "Ectopic calcification: gathering hard facts about soft tissue mineralization". Am. J. Pathol. 154 (3): 671–5. doi:10.1016/S0002-9440(10)65313-8. PMC 1866412. PMID 10079244.
- ↑ Choi ST, Kim JH, Kang EJ, Lee SW, Park MC, Park YB, Lee SK (December 2008). "Osteopontin might be involved in bone remodelling rather than in inflammation in ankylosing spondylitis". Rheumatology (Oxford). 47 (12): 1775–9. doi:10.1093/rheumatology/ken385. PMID 18854347.
- ↑ Singh M, Dalal S, Singh K (2014). "Osteopontin: At the cross-roads of myocyte survival and myocardial function". Life Sci. 118 (1): 1–6. doi:10.1016/j.lfs.2014.09.014. PMC 4254317. PMID 25265596.
- ↑ Apte UM, Banerjee A, McRee R, Wellberg E, Ramaiah SK (August 2005). "Role of osteopontin in hepatic neutrophil infiltration during alcoholic steatohepatitis". Toxicol. Appl. Pharmacol. 207 (1): 25–38. doi:10.1016/j.taap.2004.12.018. PMID 15885730.
- ↑ Koh A, da Silva AP, Bansal AK, Bansal M, Sun C, Lee H, Glogauer M, Sodek J, Zohar R (December 2007). "Role of osteopontin in neutrophil function". Immunology. 122 (4): 466–75. doi:10.1111/j.1365-2567.2007.02682.x. PMC 2266047. PMID 17680800.
- ↑ Ohshima S, Kobayashi H, Yamaguchi N, Nishioka K, Umeshita-Sasai M, Mima T, Nomura S, Kon S, Inobe M, Uede T, Saeki Y (April 2002). "Expression of osteopontin at sites of bone erosion in a murine experimental arthritis model of collagen-induced arthritis: possible involvement of osteopontin in bone destruction in arthritis". Arthritis Rheum. 46 (4): 1094–101. doi:10.1002/art.10143. PMID 11953989.
- ↑ Sakata M, Tsuruha JI, Masuko-Hongo K, Nakamura H, Matsui T, Sudo A, Nishioka K, Kato T (July 2001). "Autoantibodies to osteopontin in patients with osteoarthritis and rheumatoid arthritis". J. Rheumatol. 28 (7): 1492–5. PMID 11469452.
- ↑ 65.0 65.1 Nagasaka A, Matsue H, Matsushima H, Aoki R, Nakamura Y, Kambe N, Kon S, Uede T, Shimada S (February 2008). "Osteopontin is produced by mast cells and affects IgE-mediated degranulation and migration of mast cells". Eur. J. Immunol. 38 (2): 489–99. doi:10.1002/eji.200737057. PMID 18200503.
- ↑ Burdo TH, Wood MR, Fox HS (June 2007). "Osteopontin prevents monocyte recirculation and apoptosis". J. Leukoc. Biol. 81 (6): 1504–11. doi:10.1189/jlb.1106711. PMC 2490714. PMID 17369493.
- ↑ Crawford HC, Matrisian LM, Liaw L (November 1998). "Distinct roles of osteopontin in host defense activity and tumor survival during squamous cell carcinoma progression in vivo". Cancer Res. 58 (22): 5206–15. PMID 9823334.
- ↑ Denhardt DT, Noda M, O'Regan AW, Pavlin D, Berman JS (May 2001). "Osteopontin as a means to cope with environmental insults: regulation of inflammation, tissue remodeling, and cell survival". J. Clin. Invest. 107 (9): 1055–61. doi:10.1172/JCI12980. PMC 209291. PMID 11342566.
- ↑ Standal T, Borset M, Sundan A (September 2004). "Role of osteopontin in adhesion, migration, cell survival and bone remodeling". Exp. Oncol. 26 (3): 179–84. PMID 15494684.
- ↑ Da Silva AP, Pollett A, Rittling SR, Denhardt DT, Sodek J, Zohar R (September 2006). "Exacerbated tissue destruction in DSS-induced acute colitis of OPN-null mice is associated with downregulation of TNF-alpha expression and non-programmed cell death". J. Cell. Physiol. 208 (3): 629–39. doi:10.1002/jcp.20701. PMID 16741956.
- ↑ Yumoto K, Ishijima M, Rittling SR, Tsuji K, Tsuchiya Y, Kon S, Nifuji A, Uede T, Denhardt DT, Noda M (April 2002). "Osteopontin deficiency protects joints against destruction in anti-type II collagen antibody-induced arthritis in mice". Proc. Natl. Acad. Sci. U.S.A. 99 (7): 4556–61. doi:10.1073/pnas.052523599. PMC 123686. PMID 11930008.
- ↑ Jacobs JP, Pettit AR, Shinohara ML, Jansson M, Cantor H, Gravallese EM, Mathis D, Benoist C (August 2004). "Lack of requirement of osteopontin for inflammation, bone erosion, and cartilage damage in the K/BxN model of autoantibody-mediated arthritis". Arthritis Rheum. 50 (8): 2685–94. doi:10.1002/art.20381. PMID 15334485.
- ↑ Chabas D, Baranzini SE, Mitchell D, Bernard CC, Rittling SR, Denhardt DT, Sobel RA, Lock C, Karpuj M, Pedotti R, Heller R, Oksenberg JR, Steinman L (November 2001). "The influence of the proinflammatory cytokine, osteopontin, on autoimmune demyelinating disease". Science. 294 (5547): 1731–5. doi:10.1126/science.1062960. PMID 11721059.
- ↑ Steinman L (February 2007). "A brief history of T(H)17, the first major revision in the T(H)1/T(H)2 hypothesis of T cell-mediated tissue damage". Nat. Med. 13 (2): 139–45. doi:10.1038/nm1551. PMID 17290272.
- ↑ "Gel 'to speed up wound healing'". Health. BBC NEWS. 2008-01-22. Retrieved 2009-01-26.
- ↑ 76.0 76.1 Gassler N, Autschbach F, Gauer S, Bohn J, Sido B, Otto HF, Geiger H, Obermüller N (November 2002). "Expression of osteopontin (Eta-1) in Crohn disease of the terminal ileum". Scand J Gastroenterol. 37 (11): 1286–95. doi:10.1080/003655202761020560. PMID 12465727.
- ↑ Sato T, Nakai T, Tamura N, Okamoto S, Matsuoka K, Sakuraba A, Fukushima T, Uede T, Hibi T (September 2005). "Osteopontin/Eta-1 upregulated in Crohn's disease regulates the Th1 immune response". Gut. 54 (9): 1254–62. doi:10.1136/gut.2004.048298. PMC 1774642. PMID 16099792.
- ↑ Mishima R, Takeshima F, Sawai T, Ohba K, Ohnita K, Isomoto H, Omagari K, Mizuta Y, Ozono Y, Kohno S (February 2007). "High plasma osteopontin levels in patients with inflammatory bowel disease". J Clin Gastroenterol. 41 (2): 167–72. doi:10.1097/MCG.0b013e31802d6268. PMID 17245215.
- ↑ 79.0 79.1 Kourepini E, Aggelakopoulou M, Alissafi T, Paschalidis N, Simoes DC, Panoutsakopoulou V (March 2014). "Osteopontin expression by CD103- dendritic cells drives intestinal inflammation". Proc Natl Acad Sci U S A. 111 (9): E856–E865. doi:10.1073/pnas.1316447111. PMC 3948306. PMID 24550510.
- ↑ 80.0 80.1 80.2 80.3 80.4 Xanthou G, Alissafi T, Semitekolou M, Simoes DC, Economidou E, Gaga M, Lambrecht BN, Lloyd CM, Panoutsakopoulou V (May 2007). "Osteopontin has a crucial role in allergic airway disease through regulation of dendritic cell subsets". Nat. Med. 13 (5): 570–9. doi:10.1038/nm1580. PMC 3384679. PMID 17435770.
- ↑ Simoes DC, Xanthou G, Petrochilou K, Panoutsakopoulou V, Roussos C, Gratziou C (May 2009). "Osteopontin deficiency protects against airway remodeling and hyperresponsiveness in chronic asthma". Am J Respir Crit Care Med. 179 (10): 894–902. doi:10.1164/rccm.200807-1081OC. PMID 19234104.
- ↑ Samitas K, Zervas E, Vittorakis S, Semitekolou M, Alissafi T, Bossios A, Gogos H, Economidou E, Lötvall J, Xanthou G, Panoutsakopoulou V, Gaga M (2010). "Osteopontin expression and relation to disease severity in human asthma". Eur. Respir. J. 37 (2): 331–41. doi:10.1183/09031936.00017810. PMID 20562127.
- ↑ Hillas G, Loukides S, Kostikas K, Simoes D, Petta V, Konstantellou E, Emmanouil P, Papiris S, Koulouris N, Bakakos P (Jan 2013). "Increased levels of osteopontin in sputum supernatant of smoking asthmatics". Cytokine. 61 (1): 251–5. doi:10.1016/j.cyto.2012.10.002. PMID 23098767.
- ↑ Samitas K, Zervas E, Xanthou G, Panoutsakopoulou V, Gaga M (Feb 2013). "Osteopontin is increased in the bronchoalveolar lavage fluid and bronchial tissue of smoking asthmatics". Cytokine. 61 (3): 713–5. doi:10.1016/j.cyto.2012.12.028. PMID 23384656.
- ↑ Porter JD, Khanna S, Kaminski HJ, Rao JS, Merriam AP, Richmonds CR, Leahy P, Li J, Guo W, Andrade FH (May 2002). "A chronic inflammatory response dominates the skeletal muscle molecular signature in dystrophin-deficient mdx mice". Hum Mol Genet. 11 (3): 263–72. doi:10.1093/hmg/11.3.263. PMID 11823445.
- ↑ Haslett JN, Sanoudou D, Kho AT, Bennett RR, Greenberg SA, Kohane IS, Beggs AH, Kunkel LM (2002). "Gene expression comparison of biopsies from Duchenne muscular dystrophy (DMD) and normal skeletal muscle". Proc Natl Acad Sci U S A. 99 (23): 15000–15005. doi:10.1073/pnas.192571199. PMC 137534. PMID 12415109.
- ↑ Hirata A, Masuda S, Tamura T, Kai K, Ojima K, Fukase A, Motoyoshi K, Kamakura K, Miyagoe-Suzuki Y, Takeda S (2003). "Expression profiling of cytokines and related genes in regenerating skeletal muscle after cardiotoxin injection: a role for osteopontin". Am J Pathol. 163 (1): 203–215. doi:10.1016/S0002-9440(10)63644-9. PMC 1868192. PMID 12819025.
- ↑ Vetrone SA, Montecino-Rodriguez E, Kudryashova E, Kramerova I, Hoffman EP, Liu SD, Miceli MC, Spencer MJ (2009). "Osteopontin promotes fibrosis in dystrophic mouse muscle by modulating immune cell subsets and intramuscular TGF-beta". J Clin Invest. 119 (6): 1583–1594. doi:10.1172/JCI37662. PMC 2689112. PMID 19451692.
- ↑ Pegoraro E, Hoffman EP, Piva L, Gavassini BF, Cagnin S, Ermani M, Bello L, Soraru G, Pacchioni B, Bonifati MD, Lanfranchi G, Angelini C, Kesari A, Lee I, Gordish-Dressman H, Devaney JM, McDonald CM (2011). "SPP1 genotype is a determinant of disease severity in Duchenne muscular dystrophy". Neurology. 76 (3): 219–226. doi:10.1212/WNL.0b013e318207afeb. PMC 3034396. PMID 21178099.
- ↑ El Deeb S, Abdelnaby R, Khachab A, Bläsius K, Tingart M, Rath B (July 2016). "Osteopontin as a biochemical marker and severity indicator for idiopathic hip osteoarthritis". Hip International : The Journal of Clinical and Experimental Research on Hip Pathology and Therapy. 26 (4): 397–403. doi:10.5301/hipint.5000361. PMID 27229171.
- ↑ Kang YJ, Forbes K, Carver J, Aplin JD (2014). "The role of the osteopontin-integrin αvβ3 interaction at implantation: functional analysis using three different in vitro models". Human Reproduction (Oxford, England). 29 (4): 739–49. doi:10.1093/humrep/det433. PMID 24442579.
- ↑ Johnson GA, Burghardt RC, Bazer FW, Spencer TE (2003). "Osteopontin: roles in implantation and placentation". Biology of Reproduction. 69 (5): 1458–71. doi:10.1095/biolreprod.103.020651. PMID 12890718.
Additional images
Further reading
- Fujisawa R (2002). "[Recent advances in research on bone matrix proteins]". Nippon Rinsho. 60. Suppl 3: 72–8. PMID 11979972.
- Denhardt DT, Mistretta D, Chambers AF, Krishna S, Porter JF, Raghuram S, Rittling SR (2003). "Transcriptional regulation of osteopontin and the metastatic phenotype: evidence for a Ras-activated enhancer in the human OPN promoter". Clin. Exp. Metastasis. 20 (1): 77–84. doi:10.1023/A:1022550721404. PMID 12650610.
- Yeatman TJ, Chambers AF (2003). "Osteopontin and colon cancer progression". Clin. Exp. Metastasis. 20 (1): 85–90. doi:10.1023/A:1022502805474. PMID 12650611.
- O'Regan A (2004). "The role of osteopontin in lung disease". Cytokine Growth Factor Rev. 14 (6): 479–88. doi:10.1016/S1359-6101(03)00055-8. PMID 14563350.
- Wai PY, Kuo PC (2004). "The role of Osteopontin in tumor metastasis". J. Surg. Res. 121 (2): 228–41. doi:10.1016/j.jss.2004.03.028. PMID 15501463.
- Konno S, Hizawa N, Nishimura M, Huang SK (2007). "Osteopontin: a potential biomarker for successful bee venom immunotherapy and a potential molecule for inhibiting IgE-mediated allergic responses". Allergology International. 55 (4): 355–9. doi:10.2332/allergolint.55.355. PMID 17130676.
- Rodrigues LR, Teixeira JA, Schmitt FL, Paulsson M, Lindmark-Mänsson H (2007). "The role of osteopontin in tumor progression and metastasis in breast cancer". Cancer Epidemiol. Biomarkers Prev. 16 (6): 1087–97. doi:10.1158/1055-9965.EPI-06-1008. PMID 17548669.
- Ramaiah SK, Rittling S (2007). "Role of osteopontin in regulating hepatic inflammatory responses and toxic liver injury". Expert Opinion on Drug Metabolism & Toxicology. 3 (4): 519–26. doi:10.1517/17425225.3.4.519. PMID 17696803.
External links
- Osteopontin at the US National Library of Medicine Medical Subject Headings (MeSH)