Multiple myeloma differential diagnosis
|
Multiple myeloma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Multiple myeloma differential diagnosis On the Web |
|
American Roentgen Ray Society Images of Multiple myeloma differential diagnosis |
|
Risk calculators and risk factors for Multiple myeloma differential diagnosis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Haytham Allaham, M.D. [2]
Overview
Multiple myeloma must be differentiated from monoclonal gammopathy of undetermined significance (MGUS), isolated plasmacytoma of the bone, and extramedullary plasmacytoma.[1]
Differentiating Multiple Myeloma from other Diseases
- The table below summarizes how to differentiate multiple myeloma from other conditions that cause similar presentation:[1]
| Plasma Cell Neoplasm | M Protein Type | Pathology | Clinical Presentation |
| MGUS | IgG kappa or lambda; or IgA kappa or lambda | <10% plasma cells in bone marrow | Asymptomatic, with minimal evidence of disease (aside from the presence of an M protein) |
| Isolated plasmacytoma of bone | IgG kappa or lambda; or IgA kappa or gamma | Solitary lesion of bone; <10% plasma cells in marrow of uninvolved site | Asymptomatic or symptomatic |
| Extramedullary plasmacytoma | IgG kappa or lambda; or IgA kappa or gamma | Solitary lesion of soft tissue in the nasopharynx, tonsils, or sinuses | Asymptomatic or symptomatic |
| Multiple myeloma | IgG kappa or lambda; or IgA kappa or gamma | Often multiple lesions of bone | Symptomatic |
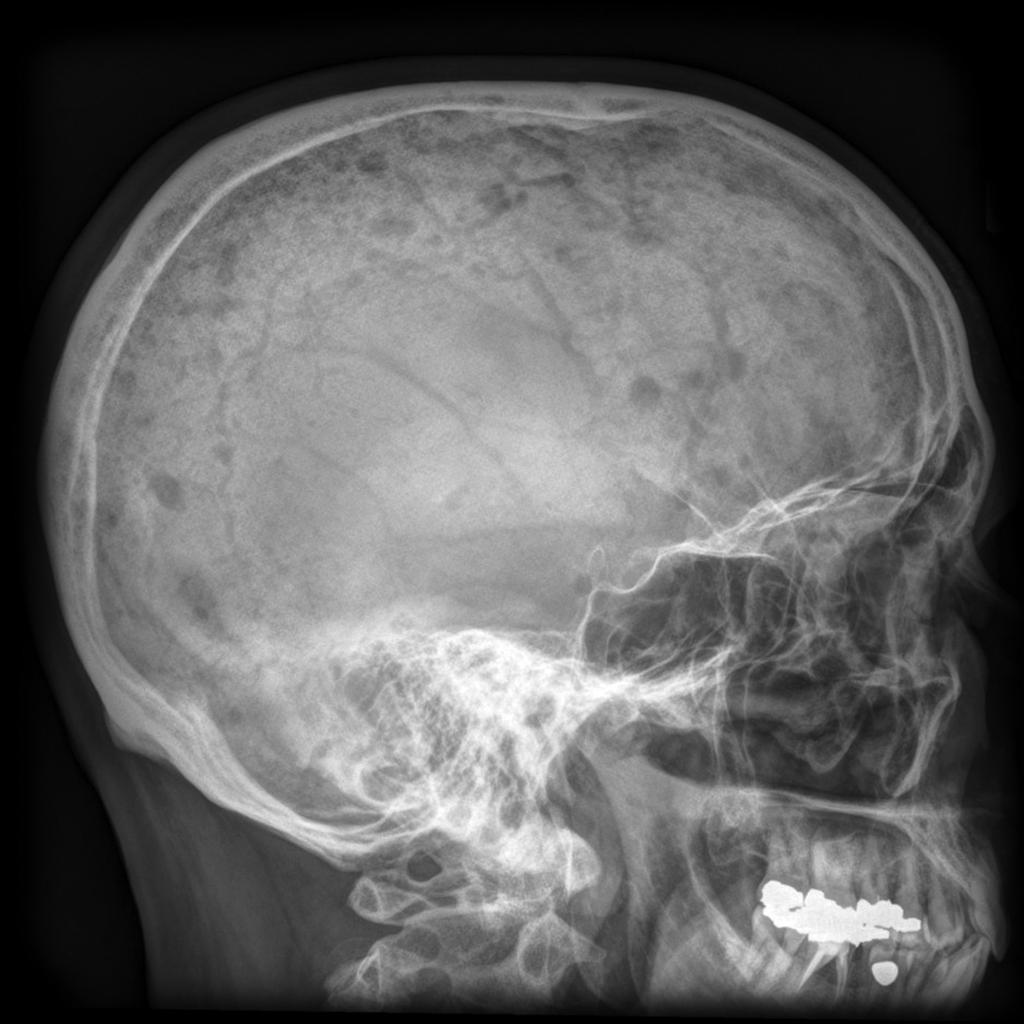
- Another important differential diagnosis is that of widespread bony metastases. Findings that favor the diagnosis of bony metastases over that of multiple myeloma include:[2]
- Bone metastases more commonly affect the vertebral pedicles rather than vertebral bodies.
- Bone metastases rarely involve mandible and distal axial skeleton.
- Although both entities have variable bone scan appearances (both hot and cold) unlike multiple myeloma, extensive bony metastases rarely have a normal appearance.
- Multiple myeloma must also be differentiated from other causes of bone pain and fatigue such as:
- Waldenstrom Hypergammaglobulinemia
- Bone fracture
- Fibrous dysplasia
- Enchondroma
- Eosinophilic granuloma
- Giant cell tumor
- Osteoblastoma
- Aneurysmal bone cyst
- Solitary bone cyst
- Hyperparathyroidism
- Infection
- Chondroblastoma
- Chondromyxoid Fibroma
- Reactive plasmacytosis
- Macroglobulinemia
- Osteoporosis (osteoporotic fracture)
- Idiopathic transient osteoporosis of hip
- Osteomalacia
- Osteogenesis imperfecta
- Multiple myeloma
- Homocystinuria
- Hypermetabolic resorptive osteoporosis.
|
Multiple myeloma must be differentiated from other causes of diabetes insipidus.
| Type of DI | Subclass | Disease | Defining signs and symptoms | Lab/Imaging findings |
|---|---|---|---|---|
| Central | Acquired | Histiocytosis |
|
 |
| Craniopharyngioma |
|
 | ||
| Sarcoidosis |
|
 | ||
| Congenital | Hydrocephalus |
|
Dilated ventricles on CT and MRI
 | |
| Wolfram Syndrome (DIDMOAD) |
| |||
| Nephrogenic | Acquired | Drug-induced (demeclocycline, lithium) |
| |
| Hypercalcemia |
| |||
| Hypokalemia |
| |||
| Multiple myeloma |
|
 | ||
| Sickle cell disease |
|
 | ||
| Primary polydipsia | Psychogenic |
| ||
| Gestational diabetes insipidus |
| |||
| Diabetes mellitus |
| |||
References
- ↑ 1.0 1.1 "Myeloma - SEER Stat Fact Sheets". Retrieved 17 February 2014.
- ↑ Multiple myeloma. Radiopaedia (2015)http://radiopaedia.org/articles/multiple-myeloma-1 Accessed on September, 20th 2015
- ↑ Ghosh KN, Bhattacharya A (1992). "Gonotrophic nature of Phlebotomus argentipes (Diptera: Psychodidae) in the laboratory". Rev Inst Med Trop Sao Paulo. 34 (2): 181–2. PMID 1340034.