Lyme disease primary prevention: Difference between revisions
| Line 6: | Line 6: | ||
==Primary Prevention== | ==Primary Prevention== | ||
=== Tick control === | |||
===Minimizing tick exposure=== | ===Minimizing tick exposure=== | ||
{| | {| | ||
| Line 47: | Line 50: | ||
=== Prophylaxis === | === Prophylaxis === | ||
* After a tick bite, routine use of antibiotic prophylaxis is not recommended.<ref name="pmid17029130"/> | * After a tick bite, routine use of antibiotic prophylaxis is not recommended.<ref name="pmid17029130" /> | ||
* A single dose of doxycycline'''(avoid in pregnancy and children <8 years)''' may be offered to adults (200mg) and children (4mg/kg, maximum 200mg) if all of the criteria are fulfilled: | * A single dose of doxycycline'''(avoid in pregnancy and children <8 years)''' may be offered to adults (200mg) and children (4mg/kg, maximum 200mg) if all of the criteria are fulfilled: | ||
** The tick is identified as ''I. scapularis'' (adult or nymph) | ** The tick is identified as ''I. scapularis'' (adult or nymph) | ||
Revision as of 19:55, 3 August 2017
|
Lyme disease Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Lyme disease primary prevention On the Web |
|
American Roentgen Ray Society Images of Lyme disease primary prevention |
|
Risk calculators and risk factors for Lyme disease primary prevention |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Ilan Dock, B.S.
Overview
Primary prevention of Lyme disease involves reducing exposure to ticks. Scientists have been developing all-natural chemical compounds made from plants that can repel or kill ticks. A Lyme disease vaccine is no longer available.
Primary Prevention
Tick control
Minimizing tick exposure
 |
Best way to prevent Lyme disease is to avoid tick infested areas. But it is unreasonable to assume that a person can completely eliminate activities that may result in tick exposure. Therefore, preventive measures should emphasize personal protection when exposed to natural areas where ticks are present:[1]
|
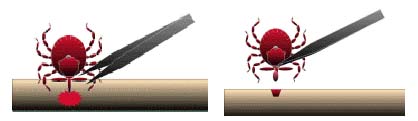
The best way to remove a tick
|
 |
|
Note:
|
 |
Prophylaxis
- After a tick bite, routine use of antibiotic prophylaxis is not recommended.[1]
- A single dose of doxycycline(avoid in pregnancy and children <8 years) may be offered to adults (200mg) and children (4mg/kg, maximum 200mg) if all of the criteria are fulfilled:
- The tick is identified as I. scapularis (adult or nymph)
- The tick is attached for ⩾36 hours. It is estimated by the degree of engorgement of the tick with blood or approximating the time of exposure to the tick.
- Within 72 hours of tick removal
- Local infection rate of tick with B. burgdorferi is ⩾20%
- There is no contraindication to use of doxycycline.
Vaccination
- A vaccine, called Lymerix, against a North American strain of the spirochetal bacteria was available from 1998 to 2002.
- It was produced by GlaxoSmithKline (GSK) and was based on the outer surface protein A (Osp-A) of Borrelia. Osp-A causes the human immune system to create antibodies that attack that protein.
- A group of patients who have been administered Lymerix developed arthritis, muscle pain and other troubling symptoms post-vaccination. Class-action litigation against GSK followed. Cassidy v. SmithKline Beecham, No. 99-10423 (Ct. Common Pleas, PA state court) (common settlement case).[7]
- It was later learned that patients with the genetic allele HLA-DR4 were susceptible to T-cell cross-reactivity between epitopes of OspA and lymphocyte function-associated antigen in these patients causing an autoimmune reaction.[8]
- New vaccines are being researched using outer surface protein C (Osp-C) and glycolipoprotein as methods of immunization.[9][10]
References
- ↑ 1.0 1.1 Wormser GP, Dattwyler RJ, Shapiro ED, Halperin JJ, Steere AC, Klempner MS; et al. (2006). "The clinical assessment, treatment, and prevention of lyme disease, human granulocytic anaplasmosis, and babesiosis: clinical practice guidelines by the Infectious Diseases Society of America". Clin Infect Dis. 43 (9): 1089–134. doi:10.1086/508667. PMID 17029130.
- ↑ Fradin MS (1998). "Mosquitoes and mosquito repellents: a clinician's guide". Ann Intern Med. 128 (11): 931–40. PMID 9634433.
- ↑ Carroll JF, Klun JA, Debboun M (2005). "Repellency of deet and SS220 applied to skin involves olfactory sensing by two species of ticks". Med Vet Entomol. 19 (1): 101–6. doi:10.1111/j.0269-283X.2005.00559.x. PMID 15752184.
- ↑ Centers for Disease Control (CDC) (1989). "Seizures temporally associated with use of DEET insect repellent--New York and Connecticut". MMWR Morb Mortal Wkly Rep. 38 (39): 678–80. PMID 2506420.
- ↑ General Tick Disease Information. Centers for Disease Control and Prevention (2015). http://www.cdc.gov/ticks/symptoms.html Accessed on December 30, 2015
- ↑ Tick Removal. Centers for Disease Control and Prevention (2015). http://www.cdc.gov/ticks/removing_a_tick.html Accessed on December 30, 2015
- ↑ Safety/Efficacy concerns re: Lyme vaccine: LYMErix Controversy LymeInfo.net
- ↑ Willett TA, Meyer AL, Brown EL, Huber BT (2004). "An effective second-generation outer surface protein A-derived Lyme vaccine that eliminates a potentially autoreactive T cell epitope". Proc. Natl. Acad. Sci. U.S.A. 101 (5): 1303–8. doi:10.1073/pnas.0305680101. PMID 14742868.
- ↑ Earnhart CG, Marconi RT (2007). "OspC phylogenetic analyses support the feasibility of a broadly protective polyvalent chimeric Lyme disease vaccine". Clin. Vaccine Immunol. 14 (5): 628–34. doi:10.1128/CVI.00409-06. PMID 17360854.
- ↑ Pozsgay V, Kubler-Kielb J (2007). "Synthesis of an experimental glycolipoprotein vaccine against Lyme disease". Carbohydr. Res. 342 (3–4): 621–6. doi:10.1016/j.carres.2006.11.014. PMID 17182019.