Lyme disease historical perspective: Difference between revisions
Jump to navigation
Jump to search
No edit summary |
No edit summary |
||
| Line 26: | Line 26: | ||
*In 1976, Jay Sanford, a former physician at the [[Walter Reed Army Institute of Research]], published a chapter in the book ''The Biology of Parasitic Spirochetes.'' In it, Dr. Sanford stated: "The ability of [[borrelia]], especially tick-borne strains, to persist in the brain and in the eye during remission after treatment with arsenic or with penicillin or even after apparent cure, is well known.” <ref name="Sanford">{{cite book | author = Sanford JP | chapter = Relapsing Fever—Treatment and Control | title = Biology of Parasitic [[Spirochetes]] | editor = Johnson RC (ed) | publisher = Academic Press | year = 1976 | isbn = 9780123870506}}</ref> Although the notion of persistent neurological infection was identified early on by military researchers such as Dr. Sanford, later Lyme researchers curiously denied the possibility of persistent ''Borrelia'' infection in the brain, with many researchers ignoring evidence of persistent infection. | *In 1976, Jay Sanford, a former physician at the [[Walter Reed Army Institute of Research]], published a chapter in the book ''The Biology of Parasitic Spirochetes.'' In it, Dr. Sanford stated: "The ability of [[borrelia]], especially tick-borne strains, to persist in the brain and in the eye during remission after treatment with arsenic or with penicillin or even after apparent cure, is well known.” <ref name="Sanford">{{cite book | author = Sanford JP | chapter = Relapsing Fever—Treatment and Control | title = Biology of Parasitic [[Spirochetes]] | editor = Johnson RC (ed) | publisher = Academic Press | year = 1976 | isbn = 9780123870506}}</ref> Although the notion of persistent neurological infection was identified early on by military researchers such as Dr. Sanford, later Lyme researchers curiously denied the possibility of persistent ''Borrelia'' infection in the brain, with many researchers ignoring evidence of persistent infection. | ||
*In 1980, Allen C. Steere, a rheumatologist at Yale university and his colleagues began to test [[antibiotics|antibiotic]] regimens in adult patients with Lyme disease.<ref>{{cite journal |author=Steere AC, Hutchinson GJ, Rahn DW, ''et al'' |title=Treatment of the early manifestations of Lyme disease |journal=Ann. Intern. Med. |volume=99 |issue=1 |pages=22-6 |year=1983 |pmid=6407378}}</ref> | *In 1980, Allen C. Steere, a rheumatologist at Yale university and his colleagues began to test [[antibiotics|antibiotic]] regimens in adult patients with Lyme disease.<ref>{{cite journal |author=Steere AC, Hutchinson GJ, Rahn DW, ''et al'' |title=Treatment of the early manifestations of Lyme disease |journal=Ann. Intern. Med. |volume=99 |issue=1 |pages=22-6 |year=1983 |pmid=6407378}}</ref> | ||
*In 1982, [[Jorge Benach|Jorge L. Benach]], a pathologist at the State University of New York at Stony Brook identified a novel [[spirochete]] which was cultured from the mid-gut of ''[[Ixodes]]'' ticks in Shelter Island, New York, and subsequently from patients with [[Lyme disease]]. The infecting agent soon after isolated by [[Willy Burgdorfer]], a researcher at the [[National Institutes of Health]], who specialized in the study of spirochete microorganisms such as ''Borrelia'' and ''Rickettsia''. The spirochete was named ''Borrelia burgdorferi'' in his honor. Burgdorfer | *In 1982, [[Jorge Benach|Jorge L. Benach]], a pathologist at the State University of New York at Stony Brook identified a novel [[spirochete]] which was cultured from the mid-gut of ''[[Ixodes]]'' ticks in Shelter Island, New York, and subsequently from patients with [[Lyme disease]]. The infecting agent was soon after isolated by [[Willy Burgdorfer]], a researcher at the [[National Institutes of Health]], who specialized in the study of spirochete microorganisms such as ''Borrelia'' and ''Rickettsia''. The spirochete was named ''Borrelia burgdorferi'' in his honor.Willy Burgdorfer and Alan Barbour were partners in the successful effort to culture the spirochete.<ref name="pmid8221514">{{cite journal| author=Burgdorfer W| title=How the discovery of Borrelia burgdorferi came about. | journal=Clin Dermatol | year= 1993 | volume= 11 | issue= 3 | pages= 335-8 | pmid=8221514 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8221514 }} </ref> | ||
*After identification ''B. burgdorferi'' as the causative agent of Lyme disease, antibiotics were selected for testing, guided by in vitro antibiotic sensitivities, including [[tetracycline antibiotics]], [[amoxicillin]], [[cefuroxime axetil]], intravenous and intramuscular [[penicillin]] and intravenous [[ceftriaxone]].<ref>{{cite journal |author=Luft BJ, Volkman DJ, Halperin JJ, Dattwyler RJ |title=New chemotherapeutic approaches in the treatment of Lyme borreliosis |journal=Ann. N. Y. Acad. Sci. |volume=539 |issue= |pages=352-61 |year=1988 |pmid=3056203}}</ref><ref>{{cite journal |author=Dattwyler RJ, Volkman DJ, Conaty SM, Platkin SP, Luft BJ |title=Amoxycillin plus probenecid versus doxycycline for treatment of [[erythema migrans]] borreliosis |journal=Lancet |volume=336 |issue=8728 |pages=1404-6 |year=1990 |pmid=1978873}}</ref> | *After identification ''B. burgdorferi'' as the causative agent of Lyme disease, antibiotics were selected for testing, guided by in vitro antibiotic sensitivities, including [[tetracycline antibiotics]], [[amoxicillin]], [[cefuroxime axetil]], intravenous and intramuscular [[penicillin]] and intravenous [[ceftriaxone]].<ref>{{cite journal |author=Luft BJ, Volkman DJ, Halperin JJ, Dattwyler RJ |title=New chemotherapeutic approaches in the treatment of Lyme borreliosis |journal=Ann. N. Y. Acad. Sci. |volume=539 |issue= |pages=352-61 |year=1988 |pmid=3056203}}</ref><ref>{{cite journal |author=Dattwyler RJ, Volkman DJ, Conaty SM, Platkin SP, Luft BJ |title=Amoxycillin plus probenecid versus doxycycline for treatment of [[erythema migrans]] borreliosis |journal=Lancet |volume=336 |issue=8728 |pages=1404-6 |year=1990 |pmid=1978873}}</ref> | ||
*The mechanism of tick transmission was also the subject of much discussion. ''B. burgdorferi'' spirochetes were identified in tick saliva in 1987, confirming the hypothesis that transmission occurred via tick salivary glands.<ref>{{cite journal |author=Ribeiro JM, Mather TN, Piesman J, Spielman A |title=Dissemination and salivary delivery of Lyme disease spirochetes in vector ticks (Acari: Ixodidae) |journal=J. Med. Entomol. |volume=24 |issue=2 |pages=201-5 |year=1987 |pmid=3585913}}</ref> | *The mechanism of tick transmission was also the subject of much discussion. ''B. burgdorferi'' spirochetes were identified in tick saliva in 1987, confirming the hypothesis that transmission occurred via tick salivary glands.<ref>{{cite journal |author=Ribeiro JM, Mather TN, Piesman J, Spielman A |title=Dissemination and salivary delivery of Lyme disease spirochetes in vector ticks (Acari: Ixodidae) |journal=J. Med. Entomol. |volume=24 |issue=2 |pages=201-5 |year=1987 |pmid=3585913}}</ref> | ||
Revision as of 17:47, 1 August 2017
|
Lyme disease Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Lyme disease historical perspective On the Web |
|
American Roentgen Ray Society Images of Lyme disease historical perspective |
|
Risk calculators and risk factors for Lyme disease historical perspective |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Ilan Dock, B.S. Anmol Pitliya, M.B.B.S. M.D.[2]
Overview
Historical Perspective
Early History
 |
|
- In the 1920s, Garin and Bujadoux, French physicians described a patient with meningoencephalitis, painful sensory radiculitis, and erythema migrans following a tick bite, and they postulated the symptoms were due to a spirochetal infection.[5]
- In the 1940s, Alfred Bannwarth, a German neurologist described several cases of chronic lymphocytic meningitis and polyradiculoneuritis, some of which were accompanied by erythematous skin lesions.[5]
- In 1948, Carl Lennhoff, a Swedish dermatologist observed spirochete-like structures in skin specimens.[6]
- In the 1950s, relations between tick bite, lymphocytoma, EM and Bannwarth's syndrome are seen throughout Europe leading to the use of penicillin for treatment.[7][8][9]
- In 1970, Rudolph Scrimenti , a U.S. physician from Wisconsin reported the first case of erythema migrans in U.S. and treated it with penicillin based on European literature.[10]
- In the United States, Lyme disease was not recognized until a cluster of cases were identified in three towns in Southeastern Connecticut in 1975. These towns included Lyme and Old Lyme, which gave the disease its popular name.[11] The cases were originally thought to be juvenile rheumatoid arthritis .This was further investigated by Dr. David Snydman and Dr. Allen Steere of the Epidemic Intelligence Service, and by others from Yale University. They recognized that the patients in the United States had erythema migrans and "Lyme arthritis" was one manifestation of the same tick-borne condition known in Europe.[12]
- Before 1976, elements of B. burgdorferi sensu lato complex infection were known as tickborne meningopolyneuritis, Garin-Bujadoux syndrome, Bannworth syndrome, Afzelius syndrome, Montauk Knee or sheep tick fever. Since 1976 the disease is most often referred to as Lyme disease, Lyme borreliosis or simply 'borreliosis'.[13][14]
- In 1976, Jay Sanford, a former physician at the Walter Reed Army Institute of Research, published a chapter in the book The Biology of Parasitic Spirochetes. In it, Dr. Sanford stated: "The ability of borrelia, especially tick-borne strains, to persist in the brain and in the eye during remission after treatment with arsenic or with penicillin or even after apparent cure, is well known.” [15] Although the notion of persistent neurological infection was identified early on by military researchers such as Dr. Sanford, later Lyme researchers curiously denied the possibility of persistent Borrelia infection in the brain, with many researchers ignoring evidence of persistent infection.
- In 1980, Allen C. Steere, a rheumatologist at Yale university and his colleagues began to test antibiotic regimens in adult patients with Lyme disease.[16]
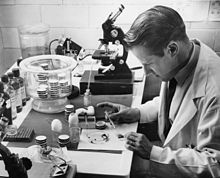
- In 1982, Jorge L. Benach, a pathologist at the State University of New York at Stony Brook identified a novel spirochete which was cultured from the mid-gut of Ixodes ticks in Shelter Island, New York, and subsequently from patients with Lyme disease. The infecting agent was soon after isolated by Willy Burgdorfer, a researcher at the National Institutes of Health, who specialized in the study of spirochete microorganisms such as Borrelia and Rickettsia. The spirochete was named Borrelia burgdorferi in his honor.Willy Burgdorfer and Alan Barbour were partners in the successful effort to culture the spirochete.[17]
- After identification B. burgdorferi as the causative agent of Lyme disease, antibiotics were selected for testing, guided by in vitro antibiotic sensitivities, including tetracycline antibiotics, amoxicillin, cefuroxime axetil, intravenous and intramuscular penicillin and intravenous ceftriaxone.[18][19]
- The mechanism of tick transmission was also the subject of much discussion. B. burgdorferi spirochetes were identified in tick saliva in 1987, confirming the hypothesis that transmission occurred via tick salivary glands.[20]
References
- ↑ Weber, Klaus (1993). Aspects of Lyme Borreliosis. Berlin, Heidelberg: Springer Berlin Heidelberg. ISBN 978-3-642-77614-4.
- ↑ Forschner, Karen (2003). Everything you need to know about Lyme disease and other tick-borne disorders. Hoboken, N.J: John Wiley. ISBN 978-0471473640.
- ↑ Balfour A (1911). "THE INFECTIVE GRANULE IN CERTAIN PROTOZOAL INFECTIONS, AS ILLUSTRATED BY THE SPIROCHAETOSIS OF SUDANESE FOWLS". Br Med J. 1 (2622): 752. PMC 2333723. PMID 20765548.
- ↑ Dworkin, Mark S.; Schwan, Tom G.; Anderson, Donald E.; Borchardt, Stephanie M. (2008). "Tick-Borne Relapsing Fever". Infectious Disease Clinics of North America. 22 (3): 449–468. doi:10.1016/j.idc.2008.03.006. ISSN 0891-5520.
- ↑ 5.0 5.1 Ryberg B (1984). "Bannwarth's syndrome (lymphocytic meningoradiculitis) in Sweden". Yale J Biol Med. 57 (4): 499–503. PMC 2590032. PMID 6516452.
- ↑ Lenhoff C (1948). "Spirochetes in aetiologically obscure diseases". Acta Dermato-Venreol. 28: 295–324.
- ↑ Bianchi GE (1950). "Penicillin therapy of lymphocytoma". Dermatologica. 100 (4–6): 270–3. PMID 15421023.
- ↑ Hollstrom E (1951). "Successful treatment of erythema migrans Afzelius". Acta Derm. Venereol. 31 (2): 235–43. PMID 14829185.
- ↑ Paschoud JM (1954). "Lymphocytoma after tick bite". Dermatologica (in German). 108 (4–6): 435–7. PMID 13190934.
- ↑ Scrimenti RJ (1970). "Erythema chronicum migrans". Archives of dermatology. 102 (1): 104–5. PMID 5497158.
- ↑ Steere AC (2006). "Lyme borreliosis in 2005, 30 years after initial observations in Lyme Connecticut". Wien. Klin. Wochenschr. 118 (21–22): 625–33. doi:10.1007/s00508-006-0687-x. PMID 17160599.
- ↑ Sternbach G, Dibble C (1996). "Willy Burgdorfer: Lyme disease". J Emerg Med. 14 (5): 631–4. PMID 8933327.
- ↑ Mast WE, Burrows WM (1976). "Erythema chronicum migrans and "Lyme arthritis"". JAMA. 236 (21): 2392. PMID 989847.
- ↑ Steere AC, Malawista SE, Snydman DR; et al. (1977). "Lyme arthritis: an epidemic of oligoarticular arthritis in children and adults in three connecticut communities". Arthritis Rheum. 20 (1): 7–17. PMID 836338.
- ↑ Sanford JP (1976). "Relapsing Fever—Treatment and Control". In Johnson RC (ed). Biology of Parasitic Spirochetes. Academic Press. ISBN 9780123870506.
- ↑ Steere AC, Hutchinson GJ, Rahn DW; et al. (1983). "Treatment of the early manifestations of Lyme disease". Ann. Intern. Med. 99 (1): 22–6. PMID 6407378.
- ↑ Burgdorfer W (1993). "How the discovery of Borrelia burgdorferi came about". Clin Dermatol. 11 (3): 335–8. PMID 8221514.
- ↑ Luft BJ, Volkman DJ, Halperin JJ, Dattwyler RJ (1988). "New chemotherapeutic approaches in the treatment of Lyme borreliosis". Ann. N. Y. Acad. Sci. 539: 352–61. PMID 3056203.
- ↑ Dattwyler RJ, Volkman DJ, Conaty SM, Platkin SP, Luft BJ (1990). "Amoxycillin plus probenecid versus doxycycline for treatment of erythema migrans borreliosis". Lancet. 336 (8728): 1404–6. PMID 1978873.
- ↑ Ribeiro JM, Mather TN, Piesman J, Spielman A (1987). "Dissemination and salivary delivery of Lyme disease spirochetes in vector ticks (Acari: Ixodidae)". J. Med. Entomol. 24 (2): 201–5. PMID 3585913.
Categories:
- CS1 maint: Unrecognized language
- CS1 maint: Explicit use of et al.
- CS1 maint: Multiple names: authors list
- CS1 maint: Extra text: editors list
- Needs overview
- Bacterial diseases
- Insect-borne diseases
- Lyme disease
- Zoonoses
- Spirochaetes
- Disease
- Infectious disease
- Dermatology
- Emergency medicine
- Intensive care medicine