Leukemia: Difference between revisions
| Line 73: | Line 73: | ||
| align="left" style="background:#F5F5F5;" + | | | align="left" style="background:#F5F5F5;" + | | ||
* Fatigue | * Fatigue | ||
| align="center" style="background:#F5F5F5;" + | | | align="center" style="background:#F5F5F5;" + |↓ | ||
| align="center" style="background:#F5F5F5;" + |+ | | align="center" style="background:#F5F5F5;" + | + | ||
| align="center" style="background:#F5F5F5;" + |+ | | align="center" style="background:#F5F5F5;" + | + | ||
| align="center" style="background:#F5F5F5;" + | | | align="center" style="background:#F5F5F5;" + | | ||
* Fever | * Fever | ||
| Line 83: | Line 83: | ||
| align="center" style="background:#F5F5F5;" + | | | align="center" style="background:#F5F5F5;" + | | ||
* Bone tenderness | * Bone tenderness | ||
* Dyspnea | * [[Dyspnea]] | ||
| align="center" style="background:#F5F5F5;" + | | | align="center" style="background:#F5F5F5;" + | | ||
* | * [[Anemia]] | ||
* [[Thrombocytopenia]] | |||
| align="center" style="background:#F5F5F5;" + | | | align="center" style="background:#F5F5F5;" + | | ||
| align="center" style="background:#F5F5F5;" + | | | align="center" style="background:#F5F5F5;" + | | ||
| Line 102: | Line 103: | ||
! align="center" style="background:#DCDCDC;" + |[[Acute lymphoblastic leukemia]] | ! align="center" style="background:#DCDCDC;" + |[[Acute lymphoblastic leukemia]] | ||
| align="center" style="background:#F5F5F5;" + | | | align="center" style="background:#F5F5F5;" + | | ||
* Arrest of [[lymphoblasts]] | * Arrest of [[lymphoblasts]] | ||
* | * Chromosomal translocations: t(9;22) , t(12;21), t(5;14), t(1;19) | ||
| align="center" style="background:#F5F5F5;" + | | | align="center" style="background:#F5F5F5;" + | | ||
| align="center" style="background:#F5F5F5;" + | | | align="center" style="background:#F5F5F5;" + | | ||
| Line 114: | Line 111: | ||
| align="center" style="background:#F5F5F5;" + | | | align="center" style="background:#F5F5F5;" + | | ||
* Generalised weakness and [[Fatigue (physical)|fatigue]] | * Generalised weakness and [[Fatigue (physical)|fatigue]] | ||
| align="center" style="background:#F5F5F5;" + |↓ | |||
| align="center" style="background:#F5F5F5;" + | + | |||
| align="center" style="background:#F5F5F5;" + | - | |||
| align="center" style="background:#F5F5F5;" + | | |||
| align="center" style="background:#F5F5F5;" + | | |||
| align="center" style="background:#F5F5F5;" + | | | align="center" style="background:#F5F5F5;" + | | ||
* Fever | |||
| align="center" style="background:#F5F5F5;" + | - | |||
| align="center" style="background:#F5F5F5;" + | + | |||
| align="center" style="background:#F5F5F5;" + | + | |||
| align="center" style="background:#F5F5F5;" + | | | align="center" style="background:#F5F5F5;" + | | ||
* [[ | * [[Dyspnea]] | ||
* [[Stridor]] | * [[Stridor]] | ||
* [[Pallor]] | * [[Pallor]] | ||
* [[Papilledema]] | * [[Papilledema]] | ||
* | * [[Meningism|Nuchal rigidity]] | ||
* [[Cranial nerve palsy]] | * [[Cranial nerve palsy]] | ||
* Testicular enlargement | * [[Testicle|Testicular]] enlargement | ||
| align="center" style="background:#F5F5F5;" + | | | align="center" style="background:#F5F5F5;" + | | ||
* [[Eosinophilia]] | * [[Eosinophilia]] | ||
* [[Lymphocytosis]] | * [[Lymphocytosis]] | ||
* [[Thrombocytopenia]] | |||
* [[Thrombocytopenia]] | |||
| align="center" style="background:#F5F5F5;" + | | | align="center" style="background:#F5F5F5;" + | | ||
| align="center" style="background:#F5F5F5;" + | | | align="center" style="background:#F5F5F5;" + | | ||
| Line 154: | Line 143: | ||
! align="center" style="background:#DCDCDC;" + |[[Chronic myelogenous leukemia]] | ! align="center" style="background:#DCDCDC;" + |[[Chronic myelogenous leukemia]] | ||
| align="center" style="background:#F5F5F5;" + | | | align="center" style="background:#F5F5F5;" + | | ||
* Myeloproliferative expansion of pluripotent stem cells | * Myeloproliferative expansion of pluripotent stem cells | ||
* | * t(9;22) | ||
| align="center" style="background:#F5F5F5;" + | | | align="center" style="background:#F5F5F5;" + | | ||
| align="center" style="background:#F5F5F5;" + | | | align="center" style="background:#F5F5F5;" + | | ||
| align="center" style="background:#F5F5F5;" + | | | align="center" style="background:#F5F5F5;" + | | ||
* Generalised weakness and [[Fatigue (physical)|fatigue]] | |||
* Early satiety | |||
| align="center" style="background:#F5F5F5;" + |↓ | |||
| align="center" style="background:#F5F5F5;" + | + | |||
| align="center" style="background:#F5F5F5;" + | | | align="center" style="background:#F5F5F5;" + | | ||
| align="center" style="background:#F5F5F5;" + | | | align="center" style="background:#F5F5F5;" + | | ||
| align="center" style="background:#F5F5F5;" + | | | align="center" style="background:#F5F5F5;" + | | ||
| align="center" style="background:#F5F5F5;" + | | | align="center" style="background:#F5F5F5;" + | | ||
| align="center" style="background:#F5F5F5;" + | + | |||
| align="center" style="background:#F5F5F5;" + | | | align="center" style="background:#F5F5F5;" + | | ||
* Hyperviscosity | |||
* Papilledema | |||
* Venous obstruction | |||
| align="center" style="background:#F5F5F5;" + | | | align="center" style="background:#F5F5F5;" + | | ||
* WBC counts | * WBC counts 300,000-600,000 cells/μL | ||
| align="center" style="background:#F5F5F5;" + | | | align="center" style="background:#F5F5F5;" + | | ||
| align="center" style="background:#F5F5F5;" + | | | align="center" style="background:#F5F5F5;" + | | ||
| Line 193: | Line 173: | ||
| align="center" style="background:#F5F5F5;" + | | | align="center" style="background:#F5F5F5;" + | | ||
| align="center" style="background:#F5F5F5;" + | | | align="center" style="background:#F5F5F5;" + | | ||
* Elevated alkaline phosphatase (ALP) | |||
|- | |- | ||
! align="center" style="background:#DCDCDC;" + |CLL | ! align="center" style="background:#DCDCDC;" + |CLL | ||
Revision as of 17:06, 9 November 2018
Template:DiseaseDisorder infobox
|
Leukemia Microchapters |
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Seyedmahdi Pahlavani, M.D. [2], Usama Talib, BSc, MD [3]
Synonyms and keywords: Leukaemia
Overview
Leukemia (Greek leukos, “white”; haima, “blood”) could be defined as a group of hematopoietic stem cell malignancies due to genetic abnormalities that may lead to clonal proliferation of these cells. These group of diseases are classified based on type of hematopoietic stem cell involvement and duration of disease. The leukemias are the most common malignancies among children younger than 15 years. Among them, ALL is the most common leukemia accounts for 77% of childhood leukemia. However, CLL is the most common form of leukemia in adults, it accounts for 30% of all leukemias in the United states. The increased rate of proliferation and decreased rate of apoptosis in this progeny of cells may compromise normal bone marrow function and ultimately marrow failure. Clinical manifestations, diagnosis, laboratory findings, and therapy are different according to the type of malignancy.
Classification
Leukemia may be classified as follows:
| Leukemia | |||||||||||||||||||||||||||||||||||||||
| Lymphoid progeny | Myeloid progeny | ||||||||||||||||||||||||||||||||||||||
| Acute lymphoblastic leukemia (ALL) | Chronic lymphocytic leukemia (CLL) | Acute Myeloid Leukemia (AML) | Chronic myeloid leukemia (CML) | ||||||||||||||||||||||||||||||||||||
Differentiating Leukemia from other Diseases
Leukemia must be differentiated from various diseases that cause weight loss, night sweats, hepatosplenomegaly, and palpable lymph nodes, such as hairy cell leukaemia, prolymphocytic leukaemia, follicular lymphoma, and mantle cell lymphoma. Based on the expression of cell surface markers, the table below differentiates different types of leukemia from other diseases that cause similar clinical presentations:[1]
| Disease | Etiology | Clinical Manifestation | Laboratory Findings | Histopathology | Imaging | Gold standard diagnosis | Associated findings | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Demography | History | Symptoms | Signs | |||||||||||||||||||
| Constitutional symptoms | Weight | Bleeding | Abdominal Pain | Vital sign | Jaundice | LAP | Hepatosplenomegaly | Other | CBC | BMP | LFT | PT/PTT | ALP | U/A | ||||||||
| Acute myelogenous leukemia (AML) |
|
|
|
|
↓ | + | + |
|
|
|
|
| ||||||||||
| Acute lymphoblastic leukemia |
|
|
|
↓ | + | - |
|
- | + | + | ||||||||||||
| Chronic myelogenous leukemia |
|
|
↓ | + | + |
|
|
| ||||||||||||||
| CLL |
|
|
|
|
|
|||||||||||||||||
| Hairy cell leukemia | ||||||||||||||||||||||
| Mast cell leukemia | ||||||||||||||||||||||
| Large granular lymphocytic leukemia | ||||||||||||||||||||||
| Chronic neutrophilic leukemia | ||||||||||||||||||||||
| Chronic eosinophilic leukemia | ||||||||||||||||||||||
| Chronic monocytic leukemia | ||||||||||||||||||||||
| Prolymphocytic leukemia (PLL) | ||||||||||||||||||||||
| T-cell large granular lymphocytic leukemia (TLGL) | ||||||||||||||||||||||
| Aggressive NK-cell leukemia (ANKL) | ||||||||||||||||||||||
| Adult T-cell leukemia/lymphoma (ATLL) | ||||||||||||||||||||||
| Sezary syndrome | ||||||||||||||||||||||
| Myelodysplastic syndrome | ||||||||||||||||||||||
| Myeloproliferative disorders | ||||||||||||||||||||||
| Leukemoid reaction | ||||||||||||||||||||||
Epidemiology and Demographics
Prevalence
- In the United States, the age-adjusted prevalence of leukemia is 75.3 per 100,000 in 2011.[2]
Incidence
- The delay-adjusted incidence of leukemia in 2011 was estimated to be 15.48 per 100,000 persons in the United States.[2]
- In 2011, the age-adjusted incidence of leukemia was 13.66 per 100,000 persons in the United States.[2]
Age
- The overall age-adjusted incidence of leukemia in the United States between 2007 and 2011 is 13 per 100,000, the age-adjusted incidence of leukemia by age category is:[2]
- Under 65 years: 6.5 per 100,000
- 65 and over: 57.9 per 100,000
- Shown below is a table depicting the overall age-adjusted incidence of leukemia per 100,000 individuals by age in the United States between 2007 and 2011 for the different types of leukemia.[2]
| Acute lymphoblastic leukemia | Chronic lymphocytic leukemia | Acute myeloid leukemia | Chronic myeloid leukemia | |
| All ages | 1.7 | 4.4 | 3.8 | 1.7 |
| <65 | 1.7 | 1.4 | 1.8 | 0.9 |
| ≥65 | 1.6 | 25.2 | 17.5 | 6.8 |
Gender
- In the United States, the age-adjusted prevalence of leukemia by gender in 2011 is:[2]
- In males: 92.7 per 100,000
- In females: 60.7 per 100,000
- In the United States, the delay-adjusted incidence of leukemia by gender in 2011 is:[2]
- In males: 19.93 per 100,000 persons
- In females: 11.89 per 100,000 persons
- In the United States, the age-adjusted incidence of leukemia by gender on 2011 is:[2]
- In males: 17.58 per 100,000 persons
- In females: 10.49 per 100,000 persons
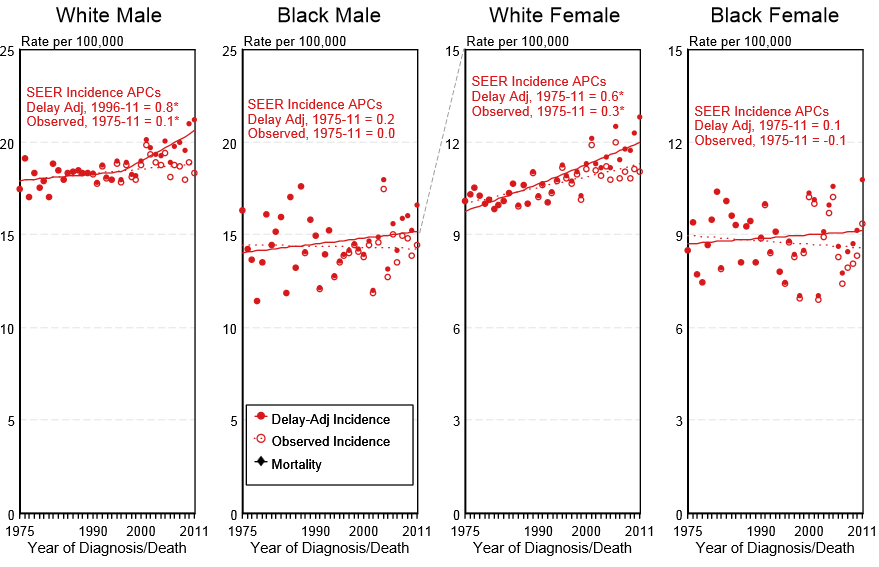
- Shown below is an image depicting the delay-adjusted incidence and observed incidence of leukemia by gender and race in the United States between 1975 and 2011. These graphs are adapted from SEER: The Surveillance, Epidemiology, and End Results Program of the National Cancer Institute.[2]
Race
- Shown below is a table depicting the age-adjusted prevalence of leukemia by race in 2011 in the United States.[2]
| All Races | White | Black | Asian/Pacific Islander | Hispanic | |
| Age-adjusted prevalence | 75.3 per 100,000 | 83.5 per 100,000 | 45.9 per 100,000 | 41.2 per 100,000 | 57.1 per 100,000 |
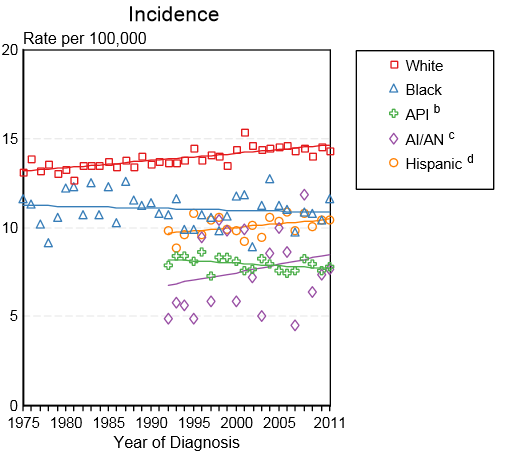
- Shown below is an image depicting the incidence of leukemia by race in the United States between 1975 and 2011.[2]
API: Asian/Pacific Islander; AI/AN: American Indian/ Alaska Native
Prognosis
5-Year Survival
- Between 2004 and 2010, the 5-year relative survival of patients with leukemia was 60.3%.[2]
- When stratified by age, the 5-year relative survival of patients with leukemia was 68.5% and 44.1% for patients <65 and ≥ 65 years of age respectively.[2]
- Shown below is a table depicting the 5-year relative survival of patients by the type of leukemia in the United States between 2004 and 2010.
| Acute lymphoblastic leukemia | Chronic lymphocytic leukemia | Acute myeloid leukemia | Chronic myeloid leukemia | |
| 5-year survival | 70% | 83.5% | 25.4% | 59.9% |
References
- ↑ Hoffbrand V, Moss P. Essential Haematology. John Wiley & Sons; 2011
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.