Intracerebral hemorrhage pathophysiology: Difference between revisions
No edit summary |
|||
| (23 intermediate revisions by the same user not shown) | |||
| Line 5: | Line 5: | ||
==Overview== | ==Overview== | ||
Intracerebral hemorrhage (ICH) is bleeding directly into the brain tissue and usually results from rupture of small penetrating arteries in the brain. Degenerative changes in the vessel wall may be associated with advancing age, [[Hypertension|chronic HTN]], [[diabetes]], and other vascular risk factor and It usually occurs at or near the [[bifurcation]] of affected arterioles.<ref name="pmid11346811" /><ref name="pmid4105427" /> The exact cause of brain damage following intracerebral hemorrhage is unknown. It is thought that ICH may result in brain injury by decreasing blood flow into the area surrounding the clot and causing neuronal ischemia or by overexertion of [[matrix metalloproteinases|matrix metalloproteinases (MMPs)]], which may result in the breakdown of the [[blood brain barrier]] and [[edema]].<ref name="caplan" /><ref name="pmid23920015" /><ref name="pmid9010429" /><ref name="pmid8249006" /> | |||
==Pathophysiology== | ==Pathophysiology== | ||
Spontaneous bleeding into the brain parenchyma results from rupture of small penetrating arteries in the brain. Degenerative changes in the vessel wall may be associated with advancing age, [[Hypertension|chronic HTN,]] [[Diabetes mellitus|diabetes]], and other vascular risk factor and It usually occurs at or near the [[bifurcation]] of affected arterioles.<ref name="pmid11346811">{{cite journal| author=Qureshi AI, Tuhrim S, Broderick JP, Batjer HH, Hondo H, Hanley DF| title=Spontaneous intracerebral hemorrhage. | journal=N Engl J Med | year= 2001 | volume= 344 | issue= 19 | pages= 1450-60 | pmid=11346811 | doi=10.1056/NEJM200105103441907 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11346811 }} </ref><ref name="pmid4105427">{{cite journal| author=Fisher CM| title=Pathological observations in hypertensive cerebral hemorrhage. | journal=J Neuropathol Exp Neurol | year= 1971 | volume= 30 | issue= 3 | pages= 536-50 | pmid=4105427 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=4105427 }} </ref> | |||
The exact cause of brain damage following intracerebral hemorrhage is unknown. It is thought that ICH may result in brain injury by following mechanisms:<ref name="pmid9010429">{{cite journal| author=Lee KR, Kawai N, Kim S, Sagher O, Hoff JT| title=Mechanisms of edema formation after intracerebral hemorrhage: effects of thrombin on cerebral blood flow, blood-brain barrier permeability, and cell survival in a rat model. | journal=J Neurosurg | year= 1997 | volume= 86 | issue= 2 | pages= 272-8 | pmid=9010429 | doi=10.3171/jns.1997.86.2.0272 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9010429 }} </ref><ref name="pmid8249006">{{cite journal| author=Mendelow AD| title=Mechanisms of ischemic brain damage with intracerebral hemorrhage. | journal=Stroke | year= 1993 | volume= 24 | issue= 12 Suppl | pages= I115-7; discussion I118-9 | pmid=8249006 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8249006 }} </ref> | |||
*Neuronal [[ischemia]] following decreased blood flow to the area surrounding the clot | |||
*Overexpression of [[matrix metalloproteinases|matrix metalloproteinases (MMPs)]], which may result in the breakdown of the [[blood brain barrier]] and [[edema]] | |||
===Intraparenchymal hemorrhage=== | ===Intraparenchymal hemorrhage=== | ||
High blood pressure and aging blood vessels are the most common causes of intracerebral hemorrhage (intraparenchymal hemorrhage). | *High blood pressure and aging blood vessels are the most common causes of intracerebral hemorrhage (intraparenchymal hemorrhage). Hypertensive [[Intracerebral hemorrhage]] (ICH) usually results from spontaneous rupture of a small artery deep in the brain.<ref name="pmid22522444">{{cite journal| author=Folsom AR, Yatsuya H, Mosley TH, Psaty BM, Longstreth WT| title=Risk of intraparenchymal hemorrhage with magnetic resonance imaging-defined leukoaraiosis and brain infarcts. | journal=Ann Neurol | year= 2012 | volume= 71 | issue= 4 | pages= 552-9 | pmid=22522444 | doi=10.1002/ana.22690 | pmc=3377969 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22522444 }} </ref><ref name="pmid20581068">{{cite journal| author=Delgado Almandoz JE, Schaefer PW, Goldstein JN, Rosand J, Lev MH, González RG et al.| title=Practical scoring system for the identification of patients with intracerebral hemorrhage at highest risk of harboring an underlying vascular etiology: the Secondary Intracerebral Hemorrhage Score. | journal=AJNR Am J Neuroradiol | year= 2010 | volume= 31 | issue= 9 | pages= 1653-60 | pmid=20581068 | doi=10.3174/ajnr.A2156 | pmc=3682824 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20581068 }} </ref> Breaks in the vessel wall usually occurs following [[chronic hypertension]]. Prolonged hypertentsion usually result in [[intimal hyperplasia]] and hyalinosis, which may result in [[Necrosis|focal necrosis]] and cause in vessel wall breaks. [[Massive hemorrhage]] may occur when the patients have a bleeding disorder and clotting system is unable to control the bleeding.<ref name="pmid1633473">{{cite journal| author=Garcia JH, Ho KL| title=Pathology of hypertensive arteriopathy. | journal=Neurosurg Clin N Am | year= 1992 | volume= 3 | issue= 3 | pages= 497-507 | pmid=1633473 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1633473 }} </ref> | ||
Hypertensive Intracerebral hemorrhage (ICH) usually results from spontaneous rupture of a small artery deep in the brain.<ref name="pmid22522444">{{cite journal| author=Folsom AR, Yatsuya H, Mosley TH, Psaty BM, Longstreth WT| title=Risk of intraparenchymal hemorrhage with magnetic resonance imaging-defined leukoaraiosis and brain infarcts. | journal=Ann Neurol | year= 2012 | volume= 71 | issue= 4 | pages= 552-9 | pmid=22522444 | doi=10.1002/ana.22690 | pmc=3377969 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22522444 }} </ref><ref name="pmid20581068">{{cite journal| author=Delgado Almandoz JE, Schaefer PW, Goldstein JN, Rosand J, Lev MH, González RG et al.| title=Practical scoring system for the identification of patients with intracerebral hemorrhage at highest risk of harboring an underlying vascular etiology: the Secondary Intracerebral Hemorrhage Score. | journal=AJNR Am J Neuroradiol | year= 2010 | volume= 31 | issue= 9 | pages= 1653-60 | pmid=20581068 | doi=10.3174/ajnr.A2156 | pmc=3682824 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20581068 }} </ref> | |||
Breaks in the vessel wall usually occurs following chronic hypertension. Prolonged hypertentsion usually result in [[intimal hyperplasia]] and hyalinosis, which may result in [[focal necrosis]] and cause in vessel wall breaks. [[Massive hemorrhage]] may occur when the patients have a bleeding disorder and clotting system is unable to control the bleeding.<ref name="pmid1633473">{{cite journal| author=Garcia JH, Ho KL| title=Pathology of hypertensive arteriopathy. | journal=Neurosurg Clin N Am | year= 1992 | volume= 3 | issue= 3 | pages= 497-507 | pmid=1633473 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1633473 }} </ref> | * Intracerebral hemorrhage can also caused by an [[arteriovenous malformation|arteriovenous malformation (AVM)]]. AVM occurs as a result of abnormal connection between arteries and veins in the brain and can result in vessels break and bleed into the brain. | ||
Intracerebral hemorrhage can also caused by an [[arteriovenous malformation|arteriovenous malformation (AVM)]]. AVM occurs as a result of abnormal connection between arteries and veins in the brain and can | |||
Additionally, In older people, an abnormal protein called [[amyloid]] may accumulate in arteries of the brain and result in amyloid | *Additionally, In older people, an abnormal protein called [[amyloid]] may accumulate in arteries of the brain and result in amyloid angiopathy. [[Cerebral amyloid angiopathy|Cerebral amyloid angiopathy (CAA)]] weakens the arteries and can cause [[hemorrhage]]. [[Apolipoprotein E|Apolipoprotein E (ApoE]]) genotype plays an important role in the pathogenesis of CAA.<ref name="pmid9189032">{{cite journal| author=Nicoll JA, Burnett C, Love S, Graham DI, Dewar D, Ironside JW et al.| title=High frequency of apolipoprotein E epsilon 2 allele in hemorrhage due to cerebral amyloid angiopathy. | journal=Ann Neurol | year= 1997 | volume= 41 | issue= 6 | pages= 716-21 | pmid=9189032 | doi=10.1002/ana.410410607 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9189032 }}</ref> Recurrent lobar ICH is common among patients with [[cerebral amyloid angiopathy]].<ref name="pmid7604411">{{cite journal| author=Passero S, Burgalassi L, D'Andrea P, Battistini N| title=Recurrence of bleeding in patients with primary intracerebral hemorrhage. | journal=Stroke | year= 1995 | volume= 26 | issue= 7 | pages= 1189-92 | pmid=7604411 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=7604411 }} </ref><ref name="pmid9222177">{{cite journal| author=Neau JP, Ingrand P, Couderq C, Rosier MP, Bailbe M, Dumas P et al.| title=Recurrent intracerebral hemorrhage. | journal=Neurology | year= 1997 | volume= 49 | issue= 1 | pages= 106-13 | pmid=9222177 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9222177 }} </ref> | ||
====Anatomical locations==== | ====Anatomical locations==== | ||
The most common sites include: | The most common sites for hypertensive ICH include:<ref name="pmid20167915">{{cite journal| author=Cordonnier C, Klijn CJ, van Beijnum J, Al-Shahi Salman R| title=Radiological investigation of spontaneous intracerebral hemorrhage: systematic review and trinational survey. | journal=Stroke | year= 2010 | volume= 41 | issue= 4 | pages= 685-90 | pmid=20167915 | doi=10.1161/STROKEAHA.109.572495 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20167915 }}</ref><ref name="pmid11346811">{{cite journal| author=Qureshi AI, Tuhrim S, Broderick JP, Batjer HH, Hondo H, Hanley DF| title=Spontaneous intracerebral hemorrhage. | journal=N Engl J Med | year= 2001 | volume= 344 | issue= 19 | pages= 1450-60 | pmid=11346811 | doi=10.1056/NEJM200105103441907 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11346811 }} </ref> | ||
*[[Basal ganglia]] (especially the [[putamen]]) | *[[Basal ganglia]] (especially the [[putamen]]) | ||
*[[Thalamus]] | *[[Thalamus]] | ||
*[[Cerebellum]] | *[[Cerebellum]] | ||
*[[Pons]] | *[[Pons]] | ||
The small arteries in these areas seem more sensitive to hypertension and as a result, it may progress to vascular injury. | The small arteries in these areas seem more sensitive to [[hypertension]] and as a result, it may progress to vascular injury. | ||
If intracerebral hemorrhage (ICH) occurs in other brain areas or in non hypertensive patients, the other causes of [[intracerebral hemorrhage]] should be considered such as: | If intracerebral hemorrhage (ICH) occurs in other brain areas or in non hypertensive patients, the other causes of [[intracerebral hemorrhage]] should be considered such as:<ref name="pmid11346811">{{cite journal| author=Qureshi AI, Tuhrim S, Broderick JP, Batjer HH, Hondo H, Hanley DF| title=Spontaneous intracerebral hemorrhage. | journal=N Engl J Med | year= 2001 | volume= 344 | issue= 19 | pages= 1450-60 | pmid=11346811 | doi=10.1056/NEJM200105103441907 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11346811 }} </ref> | ||
*[[Neoplasms]] | *[[Neoplasms]] | ||
*Hemorrhagic disorders | *Hemorrhagic disorders | ||
*[[Vascular malformations of the brain|Vascular malformations]] | *[[Vascular malformations of the brain|Vascular malformations]] | ||
**[[Arteriovenous malformation | **[[Arteriovenous malformation|Arteriovenous malformation (AVM)]] | ||
*[[Cerebral amyloid angiopathy]] | *[[Cerebral amyloid angiopathy]] (mostly lobar) | ||
===Intraventricular hemorrhage=== | ===Intraventricular hemorrhage=== | ||
| Line 41: | Line 43: | ||
===Microbleeds=== | ===Microbleeds=== | ||
It is a clinically silent cerebral microbleeds directly into the brain tissue. | It is a clinically silent cerebral microbleeds directly into the brain tissue. | ||
It is thought that [[intimal hyperplasia]] and [[hyalinosis]] following hypertension and amyloid disposition may result in [[pseudoaneurysm]] formation and blood vessel leakage.<ref name="pmid21233474">{{cite journal| author=Altmann-Schneider I, Trompet S, de Craen AJ, van Es AC, Jukema JW, Stott DJ et al.| title=Cerebral microbleeds are predictive of mortality in the elderly. | journal=Stroke | year= 2011 | volume= 42 | issue= 3 | pages= 638-44 | pmid=21233474 | doi=10.1161/STROKEAHA.110.595611 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21233474 }} </ref><ref name="pmid22949472">{{cite journal| author=Liu W, Liu R, Sun W, Peng Q, Zhang W, Xu E et al.| title=Different impacts of blood pressure variability on the progression of cerebral microbleeds and white matter lesions. | journal=Stroke | year= 2012 | volume= 43 | issue= 11 | pages= 2916-22 | pmid=22949472 | doi=10.1161/STROKEAHA.112.658369 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22949472 }} </ref> | It is thought that [[intimal hyperplasia]] and [[hyalinosis]] following [[hypertension]] and [[Amyloid angiopathy|amyloid disposition]] may result in [[pseudoaneurysm]] formation and blood vessel leakage.<ref name="pmid21233474">{{cite journal| author=Altmann-Schneider I, Trompet S, de Craen AJ, van Es AC, Jukema JW, Stott DJ et al.| title=Cerebral microbleeds are predictive of mortality in the elderly. | journal=Stroke | year= 2011 | volume= 42 | issue= 3 | pages= 638-44 | pmid=21233474 | doi=10.1161/STROKEAHA.110.595611 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21233474 }} </ref><ref name="pmid22949472">{{cite journal| author=Liu W, Liu R, Sun W, Peng Q, Zhang W, Xu E et al.| title=Different impacts of blood pressure variability on the progression of cerebral microbleeds and white matter lesions. | journal=Stroke | year= 2012 | volume= 43 | issue= 11 | pages= 2916-22 | pmid=22949472 | doi=10.1161/STROKEAHA.112.658369 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22949472 }} </ref> | ||
====Associated conditions==== | ====Associated conditions==== | ||
* Microbleeds are usually associated with:<ref name="pmid21307170">{{cite journal| author=Poels MM, Ikram MA, van der Lugt A, Hofman A, Krestin GP, Breteler MM et al.| title=Incidence of cerebral microbleeds in the general population: the Rotterdam Scan Study. | journal=Stroke | year= 2011 | volume= 42 | issue= 3 | pages= 656-61 | pmid=21307170 | doi=10.1161/STROKEAHA.110.607184 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21307170 }} </ref><ref name="pmid23449261">{{cite journal| author=Klarenbeek P, van Oostenbrugge RJ, Rouhl RP, Knottnerus IL, Staals J| title=Higher ambulatory blood pressure relates to new cerebral microbleeds: 2-year follow-up study in lacunar stroke patients. | journal=Stroke | year= 2013 | volume= 44 | issue= 4 | pages= 978-83 | pmid=23449261 | doi=10.1161/STROKEAHA.111.676619 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23449261 }} </ref><ref name="pmid20548041">{{cite journal| author=Goos JD, Henneman WJ, Sluimer JD, Vrenken H, Sluimer IC, Barkhof F et al.| title=Incidence of cerebral microbleeds: a longitudinal study in a memory clinic population. | journal=Neurology | year= 2010 | volume= 74 | issue= 24 | pages= 1954-60 | pmid=20548041 | doi=10.1212/WNL.0b013e3181e396ea | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20548041 }} </ref><ref name="pmid15155954">{{cite journal| author=Jeerakathil T, Wolf PA, Beiser A, Hald JK, Au R, Kase CS et al.| title=Cerebral microbleeds: prevalence and associations with cardiovascular risk factors in the Framingham Study. | journal=Stroke | year= 2004 | volume= 35 | issue= 8 | pages= 1831-5 | pmid=15155954 | doi=10.1161/01.STR.0000131809.35202.1b | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15155954 }} </ref> | * Microbleeds are usually associated with:<ref name="pmid21307170">{{cite journal| author=Poels MM, Ikram MA, van der Lugt A, Hofman A, Krestin GP, Breteler MM et al.| title=Incidence of cerebral microbleeds in the general population: the Rotterdam Scan Study. | journal=Stroke | year= 2011 | volume= 42 | issue= 3 | pages= 656-61 | pmid=21307170 | doi=10.1161/STROKEAHA.110.607184 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21307170 }} </ref><ref name="pmid23449261">{{cite journal| author=Klarenbeek P, van Oostenbrugge RJ, Rouhl RP, Knottnerus IL, Staals J| title=Higher ambulatory blood pressure relates to new cerebral microbleeds: 2-year follow-up study in lacunar stroke patients. | journal=Stroke | year= 2013 | volume= 44 | issue= 4 | pages= 978-83 | pmid=23449261 | doi=10.1161/STROKEAHA.111.676619 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23449261 }} </ref><ref name="pmid20548041">{{cite journal| author=Goos JD, Henneman WJ, Sluimer JD, Vrenken H, Sluimer IC, Barkhof F et al.| title=Incidence of cerebral microbleeds: a longitudinal study in a memory clinic population. | journal=Neurology | year= 2010 | volume= 74 | issue= 24 | pages= 1954-60 | pmid=20548041 | doi=10.1212/WNL.0b013e3181e396ea | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20548041 }} </ref><ref name="pmid15155954">{{cite journal| author=Jeerakathil T, Wolf PA, Beiser A, Hald JK, Au R, Kase CS et al.| title=Cerebral microbleeds: prevalence and associations with cardiovascular risk factors in the Framingham Study. | journal=Stroke | year= 2004 | volume= 35 | issue= 8 | pages= 1831-5 | pmid=15155954 | doi=10.1161/01.STR.0000131809.35202.1b | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15155954 }} </ref> | ||
**[[Hypertension]] | **[[Hypertension]] | ||
**[[Diabetes mellitus]] | **[[Diabetes mellitus]] | ||
**[[Cigarette smoking]] | **[[Cigarette smoking]] | ||
**[[Chronic obstructive pulmonary disease| | **[[Chronic obstructive pulmonary disease|Chronic obstructive pulmonary disease (COPD)]] | ||
**Age | **Age | ||
**Male sex | **Male sex | ||
====Anatomical locations==== | ====Anatomical locations==== | ||
The microbleeds anatomical locations are varies with their etiology:<ref name="pmid22949472">{{cite journal| author=Liu W, Liu R, Sun W, Peng Q, Zhang W, Xu E et al.| title=Different impacts of blood pressure variability on the progression of cerebral microbleeds and white matter lesions. | journal=Stroke | year= 2012 | volume= 43 | issue= 11 | pages= 2916-22 | pmid=22949472 | doi=10.1161/STROKEAHA.112.658369 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22949472 }} </ref> | The microbleeds anatomical locations are varies with their etiology:<ref name="pmid22949472">{{cite journal| author=Liu W, Liu R, Sun W, Peng Q, Zhang W, Xu E et al.| title=Different impacts of blood pressure variability on the progression of cerebral microbleeds and white matter lesions. | journal=Stroke | year= 2012 | volume= 43 | issue= 11 | pages= 2916-22 | pmid=22949472 | doi=10.1161/STROKEAHA.112.658369 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22949472 }} </ref> | ||
| Line 56: | Line 59: | ||
*Amyloid microbleeds | *Amyloid microbleeds | ||
**Superficial lobar regions of the cerebral hemispheres | **Superficial lobar regions of the cerebral hemispheres | ||
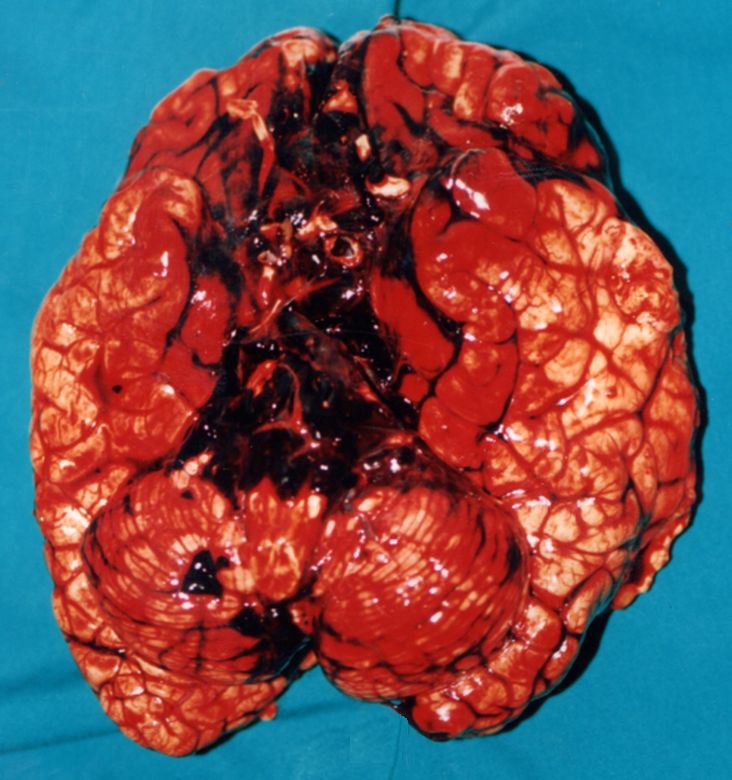
===Gross pathology=== | |||
The following are images associated with gross pathology of cerebral hemorrhage: | |||
<div align="center"> | |||
<gallery heights="250" widths="250"> | |||
Image:Hemorràgia cerebral.1444.jpg| | |||
Image:Hemorràgia intracerebral.0541.jpg | |||
</gallery> | |||
</div> | |||
==References== | ==References== | ||
Latest revision as of 16:49, 6 December 2016
|
Intracerebral hemorrhage Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
AHA/ASA Guidelines for the Management of Spontaneous Intracerebral Hemorrhage (2015) |
|
AHA/ASA Guideline Recommendation for the Primary Prevention of Stroke (2014) |
|
Case Studies |
|
Intracerebral hemorrhage pathophysiology On the Web |
|
American Roentgen Ray Society Images of Intracerebral hemorrhage pathophysiology |
|
Risk calculators and risk factors for Intracerebral hemorrhage pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sara Mehrsefat, M.D. [2]
Overview
Intracerebral hemorrhage (ICH) is bleeding directly into the brain tissue and usually results from rupture of small penetrating arteries in the brain. Degenerative changes in the vessel wall may be associated with advancing age, chronic HTN, diabetes, and other vascular risk factor and It usually occurs at or near the bifurcation of affected arterioles.[1][2] The exact cause of brain damage following intracerebral hemorrhage is unknown. It is thought that ICH may result in brain injury by decreasing blood flow into the area surrounding the clot and causing neuronal ischemia or by overexertion of matrix metalloproteinases (MMPs), which may result in the breakdown of the blood brain barrier and edema.[3][4][5][6]
Pathophysiology
Spontaneous bleeding into the brain parenchyma results from rupture of small penetrating arteries in the brain. Degenerative changes in the vessel wall may be associated with advancing age, chronic HTN, diabetes, and other vascular risk factor and It usually occurs at or near the bifurcation of affected arterioles.[1][2]
The exact cause of brain damage following intracerebral hemorrhage is unknown. It is thought that ICH may result in brain injury by following mechanisms:[5][6]
- Neuronal ischemia following decreased blood flow to the area surrounding the clot
- Overexpression of matrix metalloproteinases (MMPs), which may result in the breakdown of the blood brain barrier and edema
Intraparenchymal hemorrhage
- High blood pressure and aging blood vessels are the most common causes of intracerebral hemorrhage (intraparenchymal hemorrhage). Hypertensive Intracerebral hemorrhage (ICH) usually results from spontaneous rupture of a small artery deep in the brain.[7][8] Breaks in the vessel wall usually occurs following chronic hypertension. Prolonged hypertentsion usually result in intimal hyperplasia and hyalinosis, which may result in focal necrosis and cause in vessel wall breaks. Massive hemorrhage may occur when the patients have a bleeding disorder and clotting system is unable to control the bleeding.[9]
- Intracerebral hemorrhage can also caused by an arteriovenous malformation (AVM). AVM occurs as a result of abnormal connection between arteries and veins in the brain and can result in vessels break and bleed into the brain.
- Additionally, In older people, an abnormal protein called amyloid may accumulate in arteries of the brain and result in amyloid angiopathy. Cerebral amyloid angiopathy (CAA) weakens the arteries and can cause hemorrhage. Apolipoprotein E (ApoE) genotype plays an important role in the pathogenesis of CAA.[10] Recurrent lobar ICH is common among patients with cerebral amyloid angiopathy.[11][12]
Anatomical locations
The most common sites for hypertensive ICH include:[13][1]
- Basal ganglia (especially the putamen)
- Thalamus
- Cerebellum
- Pons
The small arteries in these areas seem more sensitive to hypertension and as a result, it may progress to vascular injury.
If intracerebral hemorrhage (ICH) occurs in other brain areas or in non hypertensive patients, the other causes of intracerebral hemorrhage should be considered such as:[1]
- Neoplasms
- Hemorrhagic disorders
- Vascular malformations
- Cerebral amyloid angiopathy (mostly lobar)
Intraventricular hemorrhage
Intraventricular hemorrhage (IVH) can be:[14][15]
- Primary, confined to the ventricles
- Secondary, originating as an extension of an ICH
Most IVH is secondary and related to hypertensive hemorrhages involving the basal ganglia and thalamus.
Microbleeds
It is a clinically silent cerebral microbleeds directly into the brain tissue. It is thought that intimal hyperplasia and hyalinosis following hypertension and amyloid disposition may result in pseudoaneurysm formation and blood vessel leakage.[16][17]
Associated conditions
Anatomical locations
The microbleeds anatomical locations are varies with their etiology:[17]
- Hypertensive microbleeds
- Deep subcortical and infratentorial regions
- Amyloid microbleeds
- Superficial lobar regions of the cerebral hemispheres
Gross pathology
The following are images associated with gross pathology of cerebral hemorrhage:
References
- ↑ 1.0 1.1 1.2 1.3 Qureshi AI, Tuhrim S, Broderick JP, Batjer HH, Hondo H, Hanley DF (2001). "Spontaneous intracerebral hemorrhage". N Engl J Med. 344 (19): 1450–60. doi:10.1056/NEJM200105103441907. PMID 11346811.
- ↑ 2.0 2.1 Fisher CM (1971). "Pathological observations in hypertensive cerebral hemorrhage". J Neuropathol Exp Neurol. 30 (3): 536–50. PMID 4105427.
- ↑
- ↑
- ↑ 5.0 5.1 Lee KR, Kawai N, Kim S, Sagher O, Hoff JT (1997). "Mechanisms of edema formation after intracerebral hemorrhage: effects of thrombin on cerebral blood flow, blood-brain barrier permeability, and cell survival in a rat model". J Neurosurg. 86 (2): 272–8. doi:10.3171/jns.1997.86.2.0272. PMID 9010429.
- ↑ 6.0 6.1 Mendelow AD (1993). "Mechanisms of ischemic brain damage with intracerebral hemorrhage". Stroke. 24 (12 Suppl): I115–7, discussion I118-9. PMID 8249006.
- ↑ Folsom AR, Yatsuya H, Mosley TH, Psaty BM, Longstreth WT (2012). "Risk of intraparenchymal hemorrhage with magnetic resonance imaging-defined leukoaraiosis and brain infarcts". Ann Neurol. 71 (4): 552–9. doi:10.1002/ana.22690. PMC 3377969. PMID 22522444.
- ↑ Delgado Almandoz JE, Schaefer PW, Goldstein JN, Rosand J, Lev MH, González RG; et al. (2010). "Practical scoring system for the identification of patients with intracerebral hemorrhage at highest risk of harboring an underlying vascular etiology: the Secondary Intracerebral Hemorrhage Score". AJNR Am J Neuroradiol. 31 (9): 1653–60. doi:10.3174/ajnr.A2156. PMC 3682824. PMID 20581068.
- ↑ Garcia JH, Ho KL (1992). "Pathology of hypertensive arteriopathy". Neurosurg Clin N Am. 3 (3): 497–507. PMID 1633473.
- ↑ Nicoll JA, Burnett C, Love S, Graham DI, Dewar D, Ironside JW; et al. (1997). "High frequency of apolipoprotein E epsilon 2 allele in hemorrhage due to cerebral amyloid angiopathy". Ann Neurol. 41 (6): 716–21. doi:10.1002/ana.410410607. PMID 9189032.
- ↑ Passero S, Burgalassi L, D'Andrea P, Battistini N (1995). "Recurrence of bleeding in patients with primary intracerebral hemorrhage". Stroke. 26 (7): 1189–92. PMID 7604411.
- ↑ Neau JP, Ingrand P, Couderq C, Rosier MP, Bailbe M, Dumas P; et al. (1997). "Recurrent intracerebral hemorrhage". Neurology. 49 (1): 106–13. PMID 9222177.
- ↑ Cordonnier C, Klijn CJ, van Beijnum J, Al-Shahi Salman R (2010). "Radiological investigation of spontaneous intracerebral hemorrhage: systematic review and trinational survey". Stroke. 41 (4): 685–90. doi:10.1161/STROKEAHA.109.572495. PMID 20167915.
- ↑ Engelhard HH, Andrews CO, Slavin KV, Charbel FT. Current manage- ment of intraventricular hemorrhage. Surg Neurol. 2003;60:15–21.
- ↑ Huttner HB, Hartmann M, Köhrmann M, Neher M, Stippich C, Hähnel S, Kress B. Repeated digital substraction angiography after perimesencephalic subarachnoid hemorrhage? J Neuroradiol. 2006;33:87–89.
- ↑ Altmann-Schneider I, Trompet S, de Craen AJ, van Es AC, Jukema JW, Stott DJ; et al. (2011). "Cerebral microbleeds are predictive of mortality in the elderly". Stroke. 42 (3): 638–44. doi:10.1161/STROKEAHA.110.595611. PMID 21233474.
- ↑ 17.0 17.1 Liu W, Liu R, Sun W, Peng Q, Zhang W, Xu E; et al. (2012). "Different impacts of blood pressure variability on the progression of cerebral microbleeds and white matter lesions". Stroke. 43 (11): 2916–22. doi:10.1161/STROKEAHA.112.658369. PMID 22949472.
- ↑ Poels MM, Ikram MA, van der Lugt A, Hofman A, Krestin GP, Breteler MM; et al. (2011). "Incidence of cerebral microbleeds in the general population: the Rotterdam Scan Study". Stroke. 42 (3): 656–61. doi:10.1161/STROKEAHA.110.607184. PMID 21307170.
- ↑ Klarenbeek P, van Oostenbrugge RJ, Rouhl RP, Knottnerus IL, Staals J (2013). "Higher ambulatory blood pressure relates to new cerebral microbleeds: 2-year follow-up study in lacunar stroke patients". Stroke. 44 (4): 978–83. doi:10.1161/STROKEAHA.111.676619. PMID 23449261.
- ↑ Goos JD, Henneman WJ, Sluimer JD, Vrenken H, Sluimer IC, Barkhof F; et al. (2010). "Incidence of cerebral microbleeds: a longitudinal study in a memory clinic population". Neurology. 74 (24): 1954–60. doi:10.1212/WNL.0b013e3181e396ea. PMID 20548041.
- ↑ Jeerakathil T, Wolf PA, Beiser A, Hald JK, Au R, Kase CS; et al. (2004). "Cerebral microbleeds: prevalence and associations with cardiovascular risk factors in the Framingham Study". Stroke. 35 (8): 1831–5. doi:10.1161/01.STR.0000131809.35202.1b. PMID 15155954.