Hypoglycemia pathophysiology: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{CMG}} {{AE}} {{MAD}} | {{CMG}} {{AE}} {{MAD}} | ||
==Overview== | ==Overview== | ||
The pathophysiology of hypoglycemia depends on the failure of physiological defense mechanisms and hormones such as [[insulin]], [[glucagon]] and [[epinephrine]] to correct hypoglycemia. Most of these defense mechanisms are hormones that control [[glycogenolysis]] and [[gluconeogenesis|gluconeogenesis.]] | The pathophysiology of hypoglycemia depends on the failure of physiological defense mechanisms and hormones such as [[insulin]], [[glucagon]] and [[epinephrine]] to correct hypoglycemia. Most of these defense mechanisms are hormones that control [[glycogenolysis]] and [[gluconeogenesis|gluconeogenesis.]] | ||
==Pathogenesis== | ==Pathogenesis== | ||
=== Physiological effect of insulin === | === Physiological effect of insulin === | ||
Insulin binds to its receptor which starts many protein activation cascades | Insulin binds to its receptor which starts many protein activation cascades | ||
The insulin signal transduction pathway begins when insulin binds to the insulin receptor proteins. | The insulin signal transduction pathway begins when insulin binds to the insulin receptor proteins. | ||
Once the transduction pathway is completed, the GLUT-4 storage vesicles becomes one with the cellular membrane. | Once the transduction pathway is completed, the GLUT-4 storage vesicles becomes one with the cellular membrane. | ||
As a result, the GLUT-4 protein channels become embedded into the membrane, allowing glucose to be transported into the cell. | As a result, the GLUT-4 protein channels become embedded into the membrane, allowing glucose to be transported into the cell. | ||
| Line 36: | Line 29: | ||
* '''[[Epinephrine]]''' | * '''[[Epinephrine]]''' | ||
Epinephrine response to hypoglycemia also becomes suppressed in many patients.<ref name="pmid8450063">{{cite journal| author=Dagogo-Jack SE, Craft S, Cryer PE| title=Hypoglycemia-associated autonomic failure in insulin-dependent diabetes mellitus. Recent antecedent hypoglycemia reduces autonomic responses to, symptoms of, and defense against subsequent hypoglycemia. | journal=J Clin Invest | year= 1993 | volume= 91 | issue= 3 | pages= 819-28 | pmid=8450063 | doi=10.1172/JCI116302 | pmc=288033 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8450063 }}</ref> This happens when blood glucose level falls in-between 65–70mmHg. A suppressed [[epinephrine]] response causes defective glucose counter-regulation and hypoglycemia unawareness.<ref name="pmid18387080">{{cite journal| author=Geddes J, Schopman JE, Zammitt NN, Frier BM| title=Prevalence of impaired awareness of hypoglycaemia in adults with Type 1 diabetes. | journal=Diabet Med | year= 2008 | volume= 25 | issue= 4 | pages= 501-4 | pmid=18387080 | doi=10.1111/j.1464-5491.2008.02413.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18387080 }}</ref> This may be due to shifting the glycemic threshold for the sympathoadrenal response to a lower plasma glucose concentration. | Epinephrine response to hypoglycemia also becomes suppressed in many patients.<ref name="pmid8450063">{{cite journal| author=Dagogo-Jack SE, Craft S, Cryer PE| title=Hypoglycemia-associated autonomic failure in insulin-dependent diabetes mellitus. Recent antecedent hypoglycemia reduces autonomic responses to, symptoms of, and defense against subsequent hypoglycemia. | journal=J Clin Invest | year= 1993 | volume= 91 | issue= 3 | pages= 819-28 | pmid=8450063 | doi=10.1172/JCI116302 | pmc=288033 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8450063 }}</ref> This happens when blood glucose level falls in-between 65–70mmHg. A suppressed [[epinephrine]] response causes defective glucose counter-regulation and hypoglycemia unawareness.<ref name="pmid18387080">{{cite journal| author=Geddes J, Schopman JE, Zammitt NN, Frier BM| title=Prevalence of impaired awareness of hypoglycaemia in adults with Type 1 diabetes. | journal=Diabet Med | year= 2008 | volume= 25 | issue= 4 | pages= 501-4 | pmid=18387080 | doi=10.1111/j.1464-5491.2008.02413.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18387080 }}</ref> This may be due to shifting the glycemic threshold for the sympathoadrenal response to a lower plasma glucose concentration. | ||
The brain is the first organ to be affected by decreased blood glucose level. Impairment of judgment and [[Seizure]]s may occur resulting in [[coma]]. | The brain is the first organ to be affected by decreased blood glucose level. Impairment of judgment and [[Seizure]]s may occur resulting in [[coma]]. | ||
| Line 43: | Line 35: | ||
* They are usually small(90%), sporadic(90%), [[solitary]](90%) and [[benign]](90%) tumors. | * They are usually small(90%), sporadic(90%), [[solitary]](90%) and [[benign]](90%) tumors. | ||
* It usually occurs sporadically but 10% are found to be associated with [[MEN 1]] syndrome.<sup>[[Insulinoma pathophysiology#cite note-pmid18672144-2|[2]]]</sup> | * It usually occurs sporadically but 10% are found to be associated with [[MEN 1]] syndrome.<sup>[[Insulinoma pathophysiology#cite note-pmid18672144-2|[2]]]</sup> | ||
* It is thought that insulinoma is mediated by mTOR/P70S6K signaling pathway. Inhibitors of mTOR([[rapamycin]]) or dual PI3K/mTOR(NVP-BEZ2235)thus have become new drugs for treating insulinoma. An oral mTOR inhibitor, [[Everolimus]], make better [[Glycemic control|glycemic contro]]<nowiki/>l in people having insulinoma.<sup>[[Insulinoma pathophysiology#cite note-pmid19129539-4|[4]]]</sup> | * It is thought that insulinoma is mediated by mTOR/P70S6K signaling pathway. Inhibitors of mTOR([[rapamycin]]) or dual PI3K/mTOR(NVP-BEZ2235)thus have become new drugs for treating insulinoma. An oral mTOR inhibitor, [[Everolimus]], make better [[Glycemic control|glycemic contro]]<nowiki/>l in people having insulinoma.<sup>[[Insulinoma pathophysiology#cite note-pmid19129539-4|[4]]]</sup> | ||
* [[Mitochondria]] play a key role in glucose and insulin coupling to assure insulin secretion after glucose stimulation in pancreatic β cells. Coupling is impaired due to abnormal mitochondrial function in β cells causes the death of the cell.<sup>[[Insulinoma pathophysiology#cite note-pmid22766318-6|[6]]]</sup>YY1 regulates this mitochondrial function.<sup>[[Insulinoma pathophysiology#cite note-pmid18046414-7|[7]]]</sup>T372R mutation increase the [[transcription]] of YY1.<sup>[[Insulinoma pathophysiology#cite note-CaoGao2013-8|[8]]]</sup>The understanding of role and functions of YY1 in β cells in near future might prove to be therapeutic potentials. | * [[Mitochondria]] play a key role in glucose and insulin coupling to assure insulin secretion after glucose stimulation in pancreatic β cells. Coupling is impaired due to abnormal mitochondrial function in β cells causes the death of the cell.<sup>[[Insulinoma pathophysiology#cite note-pmid22766318-6|[6]]]</sup>YY1 regulates this mitochondrial function.<sup>[[Insulinoma pathophysiology#cite note-pmid18046414-7|[7]]]</sup>T372R mutation increase the [[transcription]] of YY1.<sup>[[Insulinoma pathophysiology#cite note-CaoGao2013-8|[8]]]</sup>The understanding of role and functions of YY1 in β cells in near future might prove to be therapeutic potentials. | ||
* The progression to [[hypoglycemia]] is actually because of decreased glucose synthesis rather than increased use due to the direct effect of [[insulin]] on the [[liver]].<sup>[[Insulinoma pathophysiology#cite note-RizzaHaymond1981-9|[9]]]</sup> | * The progression to [[hypoglycemia]] is actually because of decreased glucose synthesis rather than increased use due to the direct effect of [[insulin]] on the [[liver]].<sup>[[Insulinoma pathophysiology#cite note-RizzaHaymond1981-9|[9]]]</sup> | ||
* The neuroglycopenic symptoms appear eventually due to decreased [[blood glucose]]. [[Hypoglycemia]] stimulates [[catecholamine]] release which produces [[adrenergic]] symptoms.<sup>[[Insulinoma pathophysiology#cite note-pmid1305178-10|[10]]]</sup> | * The neuroglycopenic symptoms appear eventually due to decreased [[blood glucose]]. [[Hypoglycemia]] stimulates [[catecholamine]] release which produces [[adrenergic]] symptoms.<sup>[[Insulinoma pathophysiology#cite note-pmid1305178-10|[10]]]</sup> | ||
Revision as of 22:54, 24 August 2017
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Mohammed Abdelwahed M.D[2]
Overview
The pathophysiology of hypoglycemia depends on the failure of physiological defense mechanisms and hormones such as insulin, glucagon and epinephrine to correct hypoglycemia. Most of these defense mechanisms are hormones that control glycogenolysis and gluconeogenesis.
Pathogenesis
Physiological effect of insulin
Insulin binds to its receptor which starts many protein activation cascades The insulin signal transduction pathway begins when insulin binds to the insulin receptor proteins. Once the transduction pathway is completed, the GLUT-4 storage vesicles becomes one with the cellular membrane. As a result, the GLUT-4 protein channels become embedded into the membrane, allowing glucose to be transported into the cell.
The actions of insulin on the global human metabolism level include:
- Insulin decreases blood glucose concentration by inducing intake of glucose by the cell. This is possible because Insulin causes the insertion of the GLUT4 transporter in the cell membranes of muscle and fat tissues which allows glucose to enter the cell. [53]
- Increase of DNA replication and protein synthesis via control of amino acid uptake
- Induction of glycogen synthesis when glucose levels are high. 59
- Increase of cellular potassium uptake.[61][62]
- Decreased gluconeogenesis and glycogenolysis: decreases production of glucose from noncarbohydrate substrates, primarily in the liver (the vast majority of endogenous insulin arriving at the liver never leaves the liver); increase of insulin causes glucose production by the liver from assorted substrates.[58]
- Increase of lipid synthesis: insulin forces fat cells to take in blood glucose, which is converted into triglycerides; decrease of insulin causes the reverse.
- Decrease of lipolysis: insulin forces reduction in conversion of fat cell lipid stores into blood fatty acids and glycerol; decrease of insulin causes the reverse.[58]
- Decrease of proteolysis : insulin decreases the breakdown of protein. [58]
- Decrease of renal sodium excretion.[64
Pathogenesis of hypoglycemia in diabetics
The pathophysiology of hypoglycemia depends on the failure of physiological defense mechanisms and hormones such as insulin, glucagon and epinephrine to correct hypoglycemia. Most of these defense mechanisms are hormones that control glycogenolysis and gluconeogenesis as follows:
The most important and the first mechanism to counter-regulate hypoglycemia is the ability to suppress insulin release. This happens early when blood glucose level is in-between 80–85 mmHg. This cannot occur in patients with absolute beta-cell failure as patients with type 1 diabetes and long-standing type 2 diabetes.[1]High insulin level inhibits hepatic glycogenolysis causing more hypoglycemia.
Hypoglycemia stimulates secretion of glucagon. This happens when blood glucose level falls in-between 65–70 mmHg. Failure to secrete glucagon may be the result of beta-cell failure and high insulin level that inhibits glucagon secretion.[2]
Epinephrine response to hypoglycemia also becomes suppressed in many patients.[3] This happens when blood glucose level falls in-between 65–70mmHg. A suppressed epinephrine response causes defective glucose counter-regulation and hypoglycemia unawareness.[4] This may be due to shifting the glycemic threshold for the sympathoadrenal response to a lower plasma glucose concentration. The brain is the first organ to be affected by decreased blood glucose level. Impairment of judgment and Seizures may occur resulting in coma.
Pathogenesis of hypoglycemia in insulinoma:
- Insulinoma is a rare benign pancreatic neuroendocrine tumor that arises from β islet cells.[1]
- They are usually small(90%), sporadic(90%), solitary(90%) and benign(90%) tumors.
- It usually occurs sporadically but 10% are found to be associated with MEN 1 syndrome.[2]
- It is thought that insulinoma is mediated by mTOR/P70S6K signaling pathway. Inhibitors of mTOR(rapamycin) or dual PI3K/mTOR(NVP-BEZ2235)thus have become new drugs for treating insulinoma. An oral mTOR inhibitor, Everolimus, make better glycemic control in people having insulinoma.[4]
- Mitochondria play a key role in glucose and insulin coupling to assure insulin secretion after glucose stimulation in pancreatic β cells. Coupling is impaired due to abnormal mitochondrial function in β cells causes the death of the cell.[6]YY1 regulates this mitochondrial function.[7]T372R mutation increase the transcription of YY1.[8]The understanding of role and functions of YY1 in β cells in near future might prove to be therapeutic potentials.
- The progression to hypoglycemia is actually because of decreased glucose synthesis rather than increased use due to the direct effect of insulin on the liver.[9]
- The neuroglycopenic symptoms appear eventually due to decreased blood glucose. Hypoglycemia stimulates catecholamine release which produces adrenergic symptoms.[10]
Pathogenesis of hypoglycemia in non-islet-cell tumors hypoglycemia(NICTH):
- Non-islet-cell tumors are large tumors of mesenchymal or epithelial cell types originate from the pancreas.
- NICTH appears to be increased glucose utilization and inhibition of glucose release from the liver.
- This happens as a result of tumor production of incompletely processed IGF-2.[5]
- Incompletely processed IGF-2 also suppresses glucagon and growth hormone release.[6]
- The net result is continued glucose utilization by skeletal muscle and inhibition of glucose release, glycogenolysis, and gluconeogenesis in the liver.[6]
Genetics
Genes associated with Diabetes mellitus include the following:[7]
- Currently, 58 genomic regions are found to be associated with Type 1 DM.
- Major susceptibility gene for type 1 DM is located on HLA region of chromosome 6. It accounts for 40-50% of the genetic risk for type 1 DM. This region encodes for class II major histocompatibility complex (MHC) molecules. Class II major histocompatibility complex (MHC) molecules play an important role in presenting antigen to helper T cells and initiating immune response.
- Other major susceptibility genes which were associated with Type 1 DM include polymorphisms in the promoter region of the insulin gene, the CTLA-4 gene, interleukin 2 receptor, CTLA4, and PTPN22 etc
- Presence of certain genes confer protection against the development of the disease. Haplotype DQA1*0102, DQB1*0602 is extremely rare in individuals with type 1 DM (<1%) and appears to provide protection from type 1 DM.
Genetics associated with Bechwith-wiedmann syndrome:[8]
- Deregulation of imprinted gene expression in the chromosome 11p15.5 region can result in the BWS phenotype].
- The critical BWS genes in that region include insulin-like growth factor 2 (IGF2), H19, cyclin-dependent kinase inhibitor 1C (CDKN1C), potassium channel voltage-gated KQT-like subfamily member 1 (KCNQ1), and KCNQ1-overlapping transcript 1 (KCNQ1OT1, or long QT intronic transcript 1).
Autoimmune hypoglycemia genetics:[9]
- Serological HLA typing demonstrated the patient had HLA-DR4.
- DNA typing showed she had HLA-DRB1*0401 and HLA-DRB1*0406 is strikingly associated with patients with insulin autoimmune syndrome who have polyclonal insulin autoantibodies.
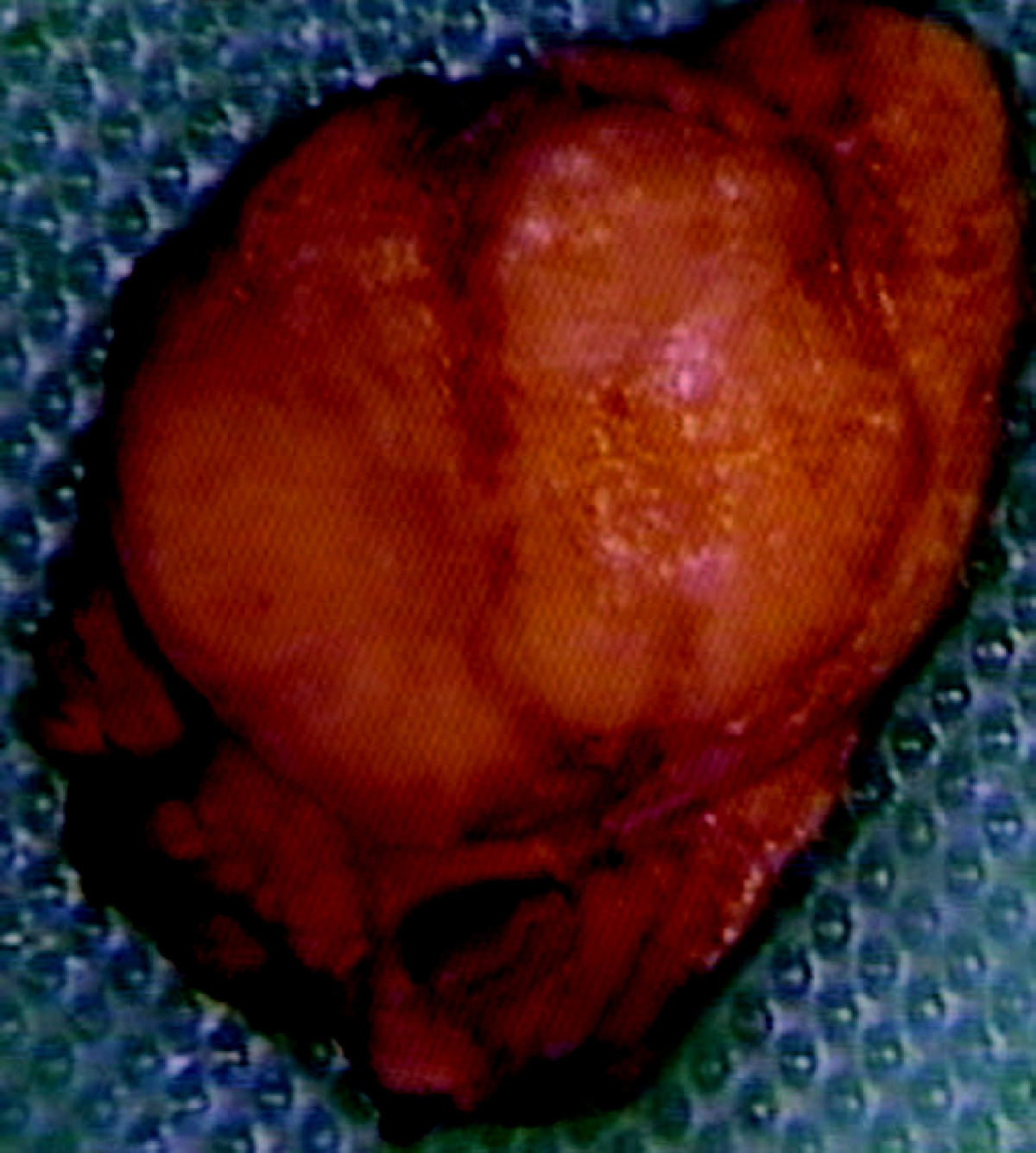
Gross pathology
On gross pathology insulinomas have a gray to red brown appearance, encapsulated [12]and are usually small and solitary tumors. Although there is a case report of a large(9cm), pedunculated and weighing more than 100g.[10]
- Almost all insulinomas are present throughout the pancreas and extrapancreatic ones causing hypoglycemia are rare(<2%).[11]
- Various other findings are noted on gross pathology such as:[12]
- Size of the tumor
- Metastasis to lymph nodes
- Extrapancreatic involvement
- Distant metastasis
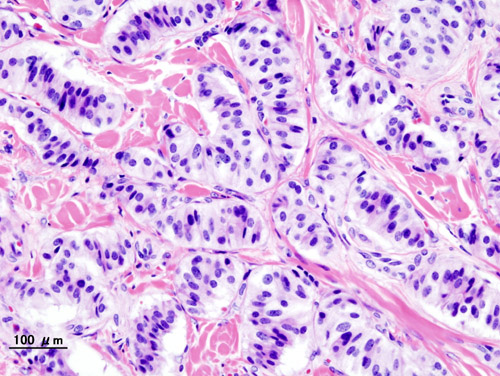
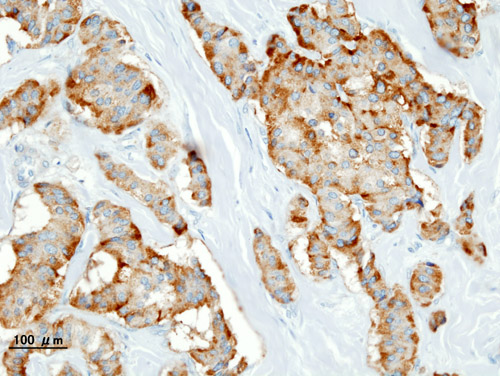
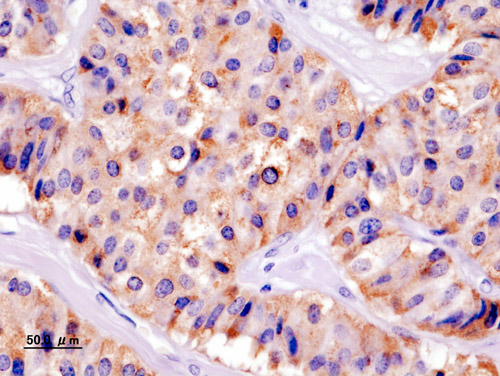
Microscopic pathology
On microscopic histopathological analysis,patterns like trabecular, gyriform, lobular and solid structures particularly with amyloid in fibrovascular stroma are characteristic findings of insulinoma..[13] It is also evaluated for the mitotic index(mitosis per 10 high power field) and immunohistochemistry staining by Chromogranin A, synaptophysin, and Ki-67 index.[14] The structure of tumor cells observed under electron microscopy as: Group A characterised by abundant well-granulated typical B cells with trabecular arrangement and Group B as scarce well -granulated typical B cells and a medullary arrangement.
References
- ↑ Dunning BE, Gerich JE (2007). "The role of alpha-cell dysregulation in fasting and postprandial hyperglycemia in type 2 diabetes and therapeutic implications". Endocr Rev. 28 (3): 253–83. doi:10.1210/er.2006-0026. PMID 17409288.
- ↑ Raju B, Cryer PE (2005). "Loss of the decrement in intraislet insulin plausibly explains loss of the glucagon response to hypoglycemia in insulin-deficient diabetes: documentation of the intraislet insulin hypothesis in humans". Diabetes. 54 (3): 757–64. PMID 15734853.
- ↑ Dagogo-Jack SE, Craft S, Cryer PE (1993). "Hypoglycemia-associated autonomic failure in insulin-dependent diabetes mellitus. Recent antecedent hypoglycemia reduces autonomic responses to, symptoms of, and defense against subsequent hypoglycemia". J Clin Invest. 91 (3): 819–28. doi:10.1172/JCI116302. PMC 288033. PMID 8450063.
- ↑ Geddes J, Schopman JE, Zammitt NN, Frier BM (2008). "Prevalence of impaired awareness of hypoglycaemia in adults with Type 1 diabetes". Diabet Med. 25 (4): 501–4. doi:10.1111/j.1464-5491.2008.02413.x. PMID 18387080.
- ↑ Cryer PE, Axelrod L, Grossman AB, Heller SR, Montori VM, Seaquist ER; et al. (2009). "Evaluation and management of adult hypoglycemic disorders: an Endocrine Society Clinical Practice Guideline". J Clin Endocrinol Metab. 94 (3): 709–28. doi:10.1210/jc.2008-1410. PMID 19088155.
- ↑ 6.0 6.1 Dynkevich Y, Rother KI, Whitford I, Qureshi S, Galiveeti S, Szulc AL; et al. (2013). "Tumors, IGF-2, and hypoglycemia: insights from the clinic, the laboratory, and the historical archive". Endocr Rev. 34 (6): 798–826. doi:10.1210/er.2012-1033. PMID 23671155.
- ↑ Pociot F, Lernmark Å (2016). "Genetic risk factors for type 1 diabetes". Lancet. 387 (10035): 2331–9. doi:10.1016/S0140-6736(16)30582-7. PMID 27302272.
- ↑ Weksberg R, Shuman C, Smith AC (2005). "Beckwith-Wiedemann syndrome". Am J Med Genet C Semin Med Genet. 137C (1): 12–23. doi:10.1002/ajmg.c.30058. PMID 16010676.
- ↑ Murakami M, Mizuide M, Kashima K, Kojima A, Tomioka SI, Kohama T; et al. (2000). "Identification of monoclonal insulin autoantibodies in insulin autoimmune syndrome associated with HLA-DRB1*0401". Horm Res. 54 (1): 49–52. doi:63437 Check
|doi=value (help). PMID 11182636. - ↑ Mittendorf EA, Liu YC, McHenry CR (2005). "Giant insulinoma: case report and review of the literature". J Clin Endocrinol Metab. 90 (1): 575–80. doi:10.1210/jc.2004-0825. PMID 15522939.
- ↑ Okabayashi T, Shima Y, Sumiyoshi T, Kozuki A, Ito S, Ogawa Y; et al. (2013). "Diagnosis and management of insulinoma". World J Gastroenterol. 19 (6): 829–37. doi:10.3748/wjg.v19.i6.829. PMC 3574879. PMID 23430217.
- ↑ de Herder WW, Niederle B, Scoazec JY, Pauwels S, Kloppel G, Falconi M; et al. (2006). "Well-differentiated pancreatic tumor/carcinoma: insulinoma". Neuroendocrinology. 84 (3): 183–8. doi:10.1159/000098010. PMID 17312378.
- ↑ Lloyd, Ricardo (2010). Endocrine pathology : differential diagnosis and molecular advances. New York London: Springer. ISBN 978-1441910684.
- ↑ de Herder, Wouter W.; Niederle, Bruno; Scoazec, Jean-Yves; Pauwels, Stanislas; Klöppel, Günter; Falconi, Massimo; Kwekkeboom, Dik J.; Öberg, Kjel; Eriksson, Barbro; Wiedenmann, Bertram; Rindi, Guido; O’Toole, Dermot; Ferone, Diego (2007). "Well-Differentiated Pancreatic Tumor/Carcinoma: Insulinoma". Neuroendocrinology. 84 (3): 183–188. doi:10.1159/000098010. ISSN 0028-3835.