HIV AIDS natural history, complications, and prognosis
|
AIDS Microchapters |
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
HIV AIDS natural history, complications, and prognosis On the Web |
|
American Roentgen Ray Society Images of HIV AIDS natural history, complications, and prognosis |
|
FDA on HIV AIDS natural history, complications, and prognosis |
|
CDC on HIV AIDS natural history, complications, and prognosis |
|
HIV AIDS natural history, complications, and prognosis in the news |
|
Blogs on HIV AIDS natural history, complications, and prognosis |
|
Risk calculators and risk factors for HIV AIDS natural history, complications, and prognosis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] ; Ammu Susheela, M.D. [2] ; Alejandro Lemor, M.D. [3]
Overview
Currently there is no cure for AIDS but taking treatment dramatically increased the amount of time people with HIV remain alive. Research continues in the areas of drug treatments and vaccine development. Unfortunately, HIV medications are not always available in the developing world, where the bulk of cases now occur. Opportunistic infections and other coinfections that might be common in HIV-infected persons, such as sexually transmitted infections, can also have adverse effects on the natural history of HIV infection.
Natural History
In the early days of the HIV epidemic, knowledge about the natural history of HIV accrued rapidly. However, the widespread use of effective antiretroviral therapy (ART) brought a shift in focus of the research community away from studies of natural history to those of treated infection.[1] HIV infection leads to progressive decline in CD4+ T-lymphocyte count increasing the risk for opportunistic infections and malignancies. Despite having a variable rate of progression determined by specific host and viral factors, the median time from infection to the development of AIDS ranges from 8 to 10 years among untreated individuals.[2] With the advent of highly active antiretroviral therapy (HAART), survival increases and CD4 cell recovery occurs at varying rates. The rate of recovery is influenced by age, baseline CD4 cell count, baseline viral load and initial and sustained viral suppression.[3]
Disease Progression

Acute HIV syndrome
Approximately half of patients that acquire HIV develop a mononucleosis-like syndrome within 3-6 weeks during which the viral titers are very elevated. This causes a rapid drop in CD4 T-Cell count as these cells are the primary host for viral replication. Within several weeks patients mount a strong immune response to the virus that causes a drop in the viral titers. However, this response is not adequate to completely suppress viral replication. Although viremia may become undetectable, replication persists in the lymphoid organs. Although a significant number of patients do not have an acute HIV syndrome, these processes do occur albeit without symptoms.[4]
Clinical Latency
This period is sometimes called asymptomatic HIV infection or chronic HIV infection. After the initial phase, the majority of patients with HIV develop a clinical latency period that lasts several years. During this period, all patients have a progressive decline in immune status and gradual depletion of CD4 T-cells. This period does not represent a true microbiological or pathological latency, but rather defines a time period without clinically manifest disease. People who are on highly active antiretroviral therapy (HAART) may live with clinical latency for several decades.[4]
Clinically Apparent Disease (AIDS)
The eventual outcome of most HIV infections is gradual immune system deterioration resulting in AIDS. Clinically apparent disease is classically diagnosed following an AIDS-defining illness i.e. an opportunistic infection or neoplasm that demonstrates a significant compromise of the immune system. Another diagnostic sign, although not strictly clinical, is the decline of CD4 T-cell count below 200 cells/mm3. Without treatment, individuals diagnosed with AIDS may survive approximately 1-3 years.[4]
Distinct Patterns of Progression
The natural course of untreated HIV infection varies widely. The past decade has seen considerable interest in the identification of subgroups of HIV-positive persons who exhibit distinct patterns of disease progression:[1]
- Long-term nonprogressors (LTNP) are individuals who remain asymptomatic for a prolonged period of time off ART with a high CD4 cell count. Although it is widely reported that 1–5% of the HIV-positive population are LTNP, these estimates are complicated by the fact that there is no standardized definition of a LTNP, and thus definitions used (and the way in which they are applied, particularly in the presence of varying follow-up and irregularly measured CD4 cell counts) differ widely. LTNP status can be lost, and thus the reported prevalence of LTNP within a study will depend on the required period of follow-up. Predictors of loss of LTNP status are a high baseline HIV DNA level and a more rapid increase in HIV DNA over the first year of follow-up, suggesting the presence of ongoing (but low-grade) viral replication. Indeed, HIV RNA levels in plasma increased by 0.04 log10 copies/ml per year over the first 8 years after diagnosis. As such, it is likely that virtually all HIV-positive persons will eventually experience disease progression if left untreated.[1]
- Elite controllers or viral controllers are individuals who are able to suppress HIV replication to such an extent that viral load levels remain undetectable in the absence of ART. As with LTNP, several studies have attempted to identify factors associated with elite controller status. Loss of naive CD4 T cells seems to be a universal feature of elite controllers, despite the ability of such individuals to maintain undetectable viral loads. However, CD4 naive lymphocytes from elite controllers tend to be less susceptible to HIV infection than such lymphocytes from progressors or uninfected individuals. This specific feature was linked with upregulation of a cellular kinase (p21). HIV-specific CD4 activation is a hallmark of viral control but, many other host factors have been linked with this phenotype, including cellular restriction factors such as APOBEC, tetherin, and SAMHD1. In addition, several viral factors may also play a role, including deletions or mutations with the viral genes that may have an impact on the ability of the virus to replicate. [1]
Complications
HIV infection makes individuals highly susceptible to severe opportunistic infections and neoplastic disease.
1. Infections common to HIV/AIDS
- Pneumocystis jirovecii pneumonia
- Tuberculosis
- Disseminated Mycobacterium avium complex
- Salmonellosis (Septicemia)
- Cytomegalovirus retinitis
- Candidiasis
- Cryptococcal meningitis
- Cerebral Toxoplasmosis
- Cryptococcal meningitis
- Disseminated Coccidiomycosis
- Disseminated Histoplasmosis
- Cryptosporidiosis
- Isosporiasis
2. Cancers common to HIV/AIDS
- Primary CNS Lymphoma
- Burkitt's Lymphoma
- Large B-cell Lymphoma
- Invasive cervical cancer
- Invasive anal cancer
3. Other Complications
- HIV-associated nephropathy
- HIV-induced pericarditis
- HIV-associated wasting syndrome
- Aortitis
- AIDS Dementia complex
Coinfections
Effect of Geographic Area on Opportunistic Infection
The opportunistic infection in AIDS patient reflect the pathogen that are common in that area.
- In USA: Person with AIDS tends to present with commensal organism such as Pneumoncystis and Candida.
- In a study done by National Center of HIV/AIDS,[5] PCP was the most common AIDS-defining opportunistic infection to occur first.
- PCP was the first OI to occur for 36% of HIV-infected persons.
- The most common incident AIDS-defining OI (274 cases per 1000 person-years).
- The most common AIDS-defining OI to have occurred during the course of AIDS (53% of persons who died with AIDS had PCP diagnosed at some time during their course of AIDS).
- In a study done by National Center of HIV/AIDS,[5] PCP was the most common AIDS-defining opportunistic infection to occur first.
- In developing nations: AIDS patients tends to present with Tuberculosis, as it is more prevalent in those countries.
A. The Major Pulmonary Illnesses
-
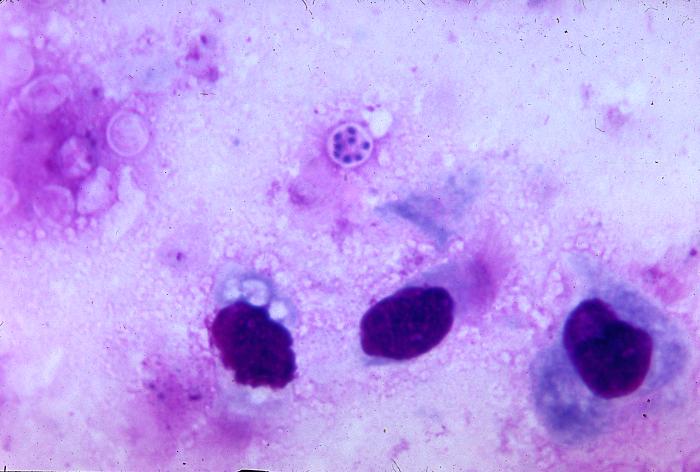
Pneumocystis jiroveci is present in this lung impression smear, using Giemsa stain
-
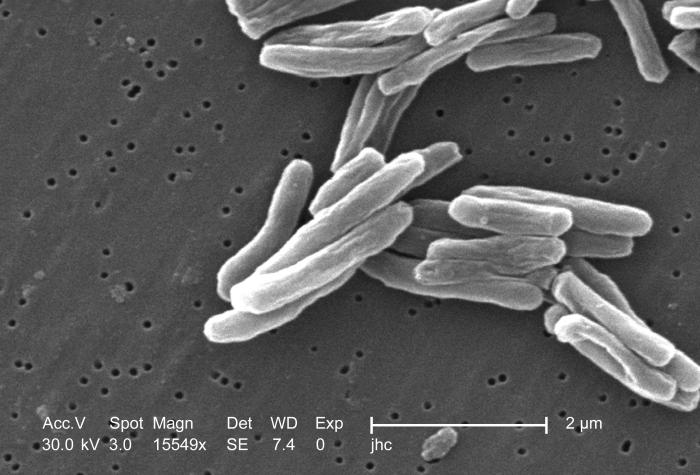
Scanning electron micrograph (SEM) of a number of Gram-positive Mycobacterium tuberculosis bacteria
Pneumocystis jiroveci Pneumonia
- Pneumocystis jiroveci pneumonia (originally known as Pneumocystis carinii pneumonia, often abbreviated PCP) is relatively rare in normal, immunocompetent people but common among HIV-infected individuals. Before the advent of effective treatment and diagnosis in Western countries it was a common immediate cause of death.
- In developing countries, it is still one of the first indications of AIDS in untested individuals, although it does not generally occur unless the CD4 count is less than 200 per µl.
Tuberculosis
- Among infections associated with HIV, tuberculosis (TB) is unique in that it may be transmitted to immunocompetent persons via the respiratory route, is easily treatable once identified, may occur in early-stage HIV disease, and is preventable with drug therapy. However, multi-drug resistance is a potentially serious problem.
- Even though its incidence has declined because of the use of directly observed therapy and other improved practices in Western countries, this is not the case in developing countries where HIV is most prevalent.
- In early-stage HIV infection (CD4 count >300 cells per µl), TB typically presents as a pulmonary disease.
- In advanced HIV infection, TB may present atypically and extrapulmonary TB is common infecting bone marrow, bone, urinary and gastrointestinal tracts, liver, regional lymph nodes, and the central nervous system (Decker and Lazarus, 2000).
B. The Major Gastro-intestinal Illnesses
Esophagitis
- Esophagitis is an inflammation of the lining of the lower end of the esophagus (gullet or swallowing tube leading to the stomach). In HIV infected individuals, this could be due to fungus (candidiasis), virus (herpes simplex-1 or cytomegalovirus). In rare cases, it could be due to mycobacteria (Zaidi and Cervia, 2002).
Unexplained Chronic Diarrhea
- In HIV infection, there are many possible causes of diarrhea, including common bacterial (Salmonella, Shigella, Listeria, Campylobacter, or Escherichia coli) and parasitic infections, and uncommon opportunistic infections such as cryptosporidiosis, microsporidiosis, Mycobacterium avium complex (MAC) and cytomegalovirus (CMV) colitis.
- Diarrhea may follow a course of antibiotics (common for Clostridium difficile). It may also be a side effect of several drugs used to treat HIV, or it may simply accompany HIV infection, particularly during primary HIV infection. In the later stages of HIV infection, diarrhea is thought to be a reflection of changes in the way the intestinal tract absorbs nutrients, and may be an important component of HIV-related wasting (Guerrant et al., 1990).
C. The Major Neurological Illnesses
Toxoplasmosis
 |
- Toxoplasmosis is a disease caused by the single-celled parasite called Toxoplasma gondii. T. gondii usually infects the brain causing toxoplasma encephalitis. It can also infect and cause disease in the eyes and lungs (Luft and Chua, 2000).
Progressive Multifocal Leukoencephalopathy
- Progressive multifocal leukoencephalopathy (PML) is a demyelinating disease, in which the myelin sheath covering the axons of nerve cells is gradually destroyed, impairing the transmission of nerve impulses. It is caused by a virus called JC virus which occurs in 70% of the population in latent form, causing disease only when the immune system has been severly weakened, as is the case for AIDS patients. It progresses rapidly, usually causing death within months of diagnosis (Sadler and Nelson, 1997).
HIV-associated Dementia
- HIV-1 associated dementia (HAD) is a metabolic encephalopathy induced by HIV infection and fueled by immune activation of brain macrophages and microglia (Gray et al., 2001). These cells are actively infected with HIV and secrete neurotoxins of both host and viral origin. Specific neurologic impairments are manifested by cognitive, behavioral, and motor abnormalities that occur after years of HIV infection and is associated with low CD4+ T cell levels and high plasma viral loads. Prevalence is between 15-30% in Western countries (Heaton et al., 1995; White et al., 1995) and has only been seen in 1-2% of India based infections (Satischandra et al., 2000; Wadia et al., 2001).
D. HIV-associated malignancies
- Patients with HIV infection are susceptible to a number of malignancies (Yarchoan et al., 2005). The most common is Kaposi's sarcoma, and the appearance of this tumor in young gay men in New York in 1981 was one of the first signals of the AIDS epidemic. In addition, patients with HIV infection have a higher incidence of certain high grade B cell lymphomas, especially Burkitt-like and large cell lymphomas. These tumors, as well as aggressive cervical cancer in women, confer a diagnosis of AIDS in patients with HIV infection.
AIDS-related lymphoma describes lymphomas occurring in patients with acquired immunodeficiency syndrome (AIDS).
- A lymphoma is a type of cancer arising from lymphoid cells. In AIDS, the incidences of non-Hodgkin's lymphoma, primary cerebral lymphoma and Hodgkin's disease are all increased.
Non-Hodgkin's Lymphoma
- Non-Hodgkin's lymphoma (NHL) is present in about 3% of HIV positive people at the time of their diagnosis of HIV. 20% of HIV positive patients will develop NHL.
Primary Cerebral Lymphoma
- Primary cerebral lymphoma (or primary central nervous system lymphoma) is a form of NHL. It is very rare in immunocompetent people, with an incidence of 5-30 cases per million person-years. However the incidence in immunocompromised individuals is greatly increased, up to 100 per million person-years.
- Primary cerebral lymphoma is strongly associated with Epstein-Barr virus (EBV). The presence of EBV DNA in cerebrospinal fluid is highly suggestive of primary cerebral lymphoma.
- Treatment of AIDS patients with antiretroviral drugs reduces the incidence of primary cerebral lymphoma.
Hodgkin's Disease
- The incidence of Hodgkin's disease in the general population is about 10-30 per million person-years. This increases to 170 per million person-years in HIV positive patients.
E. The Major Dermatological illnesses
- AIDS-associated Kaposi sarcoma or KS-AIDS presents with cutaneous lesions that begin as one or several red to purple-red macules, rapidly progressing to papules, nodules, and plaques, with a predilection for the head, neck, trunk, and mucous membranes.
-
Kaposi's sarcoma lesion commonly found in patients with stage IV AIDS
-
Intraoral Kaposi’s sarcoma lesion with an overlying candidiasis infection
Cognitive Impairment in HIV
For AIDS dementia complex , click here
Anatomical Areas Involved
- HIV is associated with pathological changes in mainly subcortical and fronto-striatal areas of the brain, including the basal ganglia, deep white matter, and hippocampal regions.
- Neuroimaging studies of HIV patients indicate that significant volume reductions are apparent in the frontal white matter, whereas subcortically, hypertrophy is apparent in the basal ganglia, especially the putamen.[6]
- Some studies suggest loss of brain volume in cortical and subcortical regions even in asymptomatic HIV patients and patients who were on stable treatment.[7] Cerebral brain volume is associated with factors related to duration of the disease and CD4 nadir; patients with a longer history of chronic HIV and higher CD4 nadir present with greater cerebral atrophy.[7]
- CD4 lymphocyte counts have also been related to greater rates of brain tissue loss.[8]
- Current factors, such as plasma HIV RNA, have been found to be associated with brain volumes as well, especially with regards to basal ganglia volume[7] and total white matter.[9]
- Changes in the brain may be ongoing but asymptomatic, that is with minimal interference in functioning, making it difficult to diagnose HIV-associated neurocognitive disorders in the early stages.[10]
Behavioral Aspects of Neurocognitive Impairments
Cognitive Impairments
- Cognitive impairments associated with HIV occur in the domains of attention, memory, verbal fluency, and visuospatial construction. Specifically for memory, the lowered activity of the hippocampus changes the basis for memory encoding and affects mechanisms such as long-term potentiation.[11]
- Severity of impairment in different domains varies depending on whether or not a patient is being treated with HAART or monotherapy.[12]
- Studies have shown that patients exhibit cognitive deficits consistent with dysfunction of fronto-striatal circuits including associated parietal areas, the latter of which may account for observed deficits in visuospatial function.[13][14]
Psychological Dysfunction
- In addition to cognitive impairments, psychological dysfunction is also noted. For example, patients with HIV have higher rates of clinical depression and alexithymia, i.e., difficulty processing or recognizing one’s own emotions.[13] Patients also have more difficulty recognizing facial emotions.[15]
- Without combination antiretroviral therapy, cognitive impairments increase with successive stages of HIV.[16] HIV patients in early stages show mild difficulties in concentration and attention.[17] In advanced cases of HIV-associated dementia, speech delay, motor dysfunction, and impaired thought and behavior are observed.[17] Specifically, lower motor speeds were found to correlate with hypertrophy of the right putamen.[6]
- The diagnosis of HIV-associated neurocognitive impairment is made using clinical criteria after considering and ruling out other possible causes.[17] The severity of neurocognitive impairment is associated with nadir CD4, suggesting that earlier treatment to prevent immunosuppression due to HIV may help prevent HIV-associated neurocognitive disorders.[16]
Benefits of Staging the System
- Easy to evaluate for new treatments
- Define prognosis and guide patient counselling
- Frame work for management and follow up
- Contribute to the quality of the care of individuals who are HIV infected.
Prognosis
Without treatment, the net median survival time after infection with HIV is estimated to be 9 to 11 years, depending on the HIV subtype, and the median survival rate after diagnosis of AIDS in resource-limited settings where treatment is not available ranges between 6 and 19 months, depending on the study.[18] In areas where it is widely available, the development of HAART as effective therapy for HIV infection and AIDS reduced the death rate from this disease by 80%, and raised the life expectancy for a newly-diagnosed HIV-infected person to about 20 years.[19]
Related Chapters
References
- ↑ 1.0 1.1 1.2 1.3 Sabin CA, Lundgren JD (2013). "The natural history of HIV infection". Curr Opin HIV AIDS. 8 (4): 311–7. doi:10.1097/COH.0b013e328361fa66. PMC 4196796. PMID 23698562.
- ↑ Vergis EN, Mellors JW (2000). "Natural history of HIV-1 infection". Infect Dis Clin North Am. 14 (4): 809–25, v–vi. PMID 11144640.
- ↑ Giles M, Workman C (2009). "Clinical manifestations and the natural history of HIV" (PDF). Australian Society for HIV Management: 125–32. ISBN 9781920773571.
- ↑ 4.0 4.1 4.2 Pantaleo G, Graziosi C, Fauci AS (1993). "New concepts in the immunopathogenesis of human immunodeficiency virus infection". N Engl J Med. 328 (5): 327–35. doi:10.1056/NEJM199302043280508. PMID 8093551.
- ↑ Jones JL, Hanson DL, Dworkin MS, Alderton DL, Fleming PL, Kaplan JE, Ward J (1999). "Surveillance for AIDS-defining opportunistic illnesses, 1992-1997". MMWR CDC Surveill Summ. 48 (2): 1–22. PMID 12412613. Unknown parameter
|month=ignored (help);|access-date=requires|url=(help) - ↑ 6.0 6.1 Castelo, JMB; Courtney, MG; Melrose, RJ; Stern, CE (2007), "Putamen hypertrophy in nondemented patients with human immunodeficiency virus infection and cognitive impairments", Archives of Neurology, 64 (9): 1275–1280, doi:10.1001/archneur.64.9.1275, PMID 17846265
- ↑ 7.0 7.1 7.2 Cohen, RA; Harezlak, J; et al. (1981), "Effects of nadir CD4 count and duration of human immunodeficiency virus infection on brain volumes in highly active antiretroviral therapy era", Journal of Neurovirology, 16 (1): 25–32, doi:10.3109/13550280903552420, PMC 2995252, PMID 20113183
- ↑ Cardenas, VA; Meyerhoff, DJ; Studholme, C; Kornak, J; Rothlind, J; Lampiris, H; Neuhaus, J; Grant, RM; Chao, LL (2009), "Evidence for ongoing brain injury in human immunodeficiency virus-positive patients treated with antiretroviral therapy", Journal of Neurovirology, 15 (4): 324–333, doi:10.1080/13550280902973960, PMC 2889153, PMID 19499454
- ↑ Jernigan, TL; Archibald, SL; Fennema-Notestine, C; Taylor, MJ; Theilmann, RJ; Julaton, MD; Notestine, RJ; Wolfson, T; Letendre, SL (2011), "Clinical factors related to brain structure in HIV: the CHARTER study", Journal of Neurovirology, 17 (3): 248–57, doi:10.1007/s13365-011-0032-7, PMID 21544705
- ↑ Wang, X; Foryt, P; Ochs, R; Chung, JH; Wu, Y; Parris, T; Ragin, A (2011), "Abnormalities in Resting-State Functional Connectivity in Early Human Immunodeficiency Virus Infection", Brain Connectivity, 1: 208–217
- ↑ Castelo, JMB; Sherman, SJ; Courtney, MG; Melrose, RJ; Stern, SE (2006), "Altered hippocampal-prefrontal activation in HIV patients during episodic memory encoding", Neurology, 66 (11): 1688–1695, doi:10.1212/01.wnl.0000218305.09183.70, PMID 16769942
- ↑ Cysique, LA; Maruff, P; Brew, BJ (2004), "Prevalence and pattern of neuropsychological impairment in human immunodeficiency virus-infected/acquired immunodeficiency syndrome (HIV/AIDS) patients across pre-and post-highly active antiretroviral therapy eras: A combined study of two cohorts", Journal of Neurovirology, 10 (6): 350–357, doi:10.1080/13550280490521078, PMID 15765806
- ↑ 13.0 13.1 Bogdanova, Y; Diaz-Santos, M; Cronin-Golomb, A (2010), "Neurocognitive correlates of alexithymia in asymptomatic individuals with HIV", Neuropsychologia, 48 (5): 1295–1304, doi:10.1016/j.neuropsychologia.2009.12.033, PMC 2843804, PMID 20036267
- ↑ Olesen, PJ; Schendan, HE; Amick, MM; Cronin-Golomb, A (2007), "HIV infection affects parietal-dependent spatial cognition: Evidence from mental rotation and hierarchical pattern perception", Behavioral Neuroscience, 121 (6): 1163–1173, doi:10.1037/0735-7044.121.6.1163, PMID 18085869
- ↑ Clark, US; Cohen, RA; Westbrook, ML; Devlin, KN; Tashima, KT (2010), "Facial emotion recognition impairments in individuals with HIV", Journal of the International Neuropsychological Society, 16 (6): 1127–1137, doi:10.1017/S1355617710001037, PMC 3070304, PMID 20961470
- ↑ 16.0 16.1 Heaton, RK; Franklin, DR; Ellis, RJ; McCutchan, JA; Letendre, SL; Leblanc, S; Corkran, SH; Duarte, NA; Clifford, DB (2010), "HIV-associated neurocognitive disorders before and during the era of combination antiretroviral therapy: differences in rates, nature, and predictors", Journal of Neurovirology, 17 (1): 3–16, doi:10.1007/s13365-010-0006-1, PMC 3032197, PMID 21174240
- ↑ 17.0 17.1 17.2 Ances, BM; Ellis, RJ (2007), "Dementia and neurocognitive disorders due to HIV-1 infection", Seminars in Neurology, 27 (1): 86–92, doi:10.1055/s-2006-956759, PMID 17226745
- ↑ Template:Cite paper
- ↑ Knoll B, Lassmann B, Temesgen Z (2007). "Current status of HIV infection: a review for non-HIV-treating physicians". Int J Dermatol. 46 (12): 1219–28. doi:10.1111/j.1365-4632.2007.03520.x. PMID 18173512.
- Pages using duplicate arguments in template calls
- CS1 maint: PMC format
- CS1 maint: Multiple names: authors list
- Pages with citations using unsupported parameters
- Pages using citations with accessdate and no URL
- HIV/AIDS
- Disease
- Immune system disorders
- Infectious disease
- Viral diseases
- Pandemics
- Sexually transmitted infections
- Syndromes
- Virology
- AIDS origin hypotheses
- Medical disasters
- Acronyms
- Immunodeficiency
- Microbiology