Facial nerve paralysis
| Facial nerve paralysis | |
 | |
|---|---|
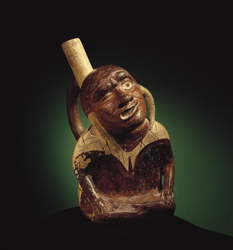
| Moche. Culture Representation of Facial Paralysis. 300 A.D. Larco Museum Collection, Lima, Peru. | |
| ICD-9 | 351 |
| eMedicine | plastic/522 |
| MeSH | D005158 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Facial nerve paralysis and Bell's palsy is due to a loss of voluntary movement of the muscles on one side of the face due to abnormal function of the facial nerve(s). A Peripheral palsy affects all ipsilateral muscles of facial expression (paralysis results on the entire ipsilateral side). A supranuclear palsy involves the lower part of the face.
Facial nerve paralysis is a common problem that involves the paralysis of any structures innervated by the facial nerve. The pathway of the facial nerve is long and relatively convoluted, and so there are a number of causes that may result in facial nerve paralysis. The most common is Bell's palsy, an idiopathic disease that may only be diagnosed by exclusion.
A thorough medical history and physical examination are the first steps in making a diagnosis.
During the physical examination, a distinction must first be made between paralysis and paresis (incomplete paralysis). Not surprisingly, paralysis is far more serious and requires immediate treatment. It must also be determined whether the forehead is involved in the motor defect or not. This is usually accomplished by assessing how well a patient can raise her eyebrows. The question is an important one because it helps determine if the lesion is in the upper motor neuron component of the facial nerve, or in its lower motor neuron component.
Laboratory investigations include an audiogram, nerve conduction studies (ENoG), computed tomography (CT) or magnetic resonance (MR) imaging.
Causes
Bell's palsy
Bell's palsy is the most common cause of acute facial nerve paralysis (>80%). Previously considered idiopathic, it has been recently linked to herpes zoster of the facial nerve (rarely Lyme disease).
Bell's palsy is an exclusion diagnosis. Some factors that tend to rule out Bell's palsy include:
- Recurrent paralysis
- Slowly progressive paralysis (The onset of Bell's palsy is very sudden)
- Twitching
- Associated symptoms (either cochlear or neurologic)
Bell's palsy is believed in the most recent studies to be due to herpes virus. Other proposed etiologies include vascular problems in the inner ear. Treatment include steroids and antivirals.
Trauma
Physical trauma, especially fractures of the temporal bone, may also cause acute facial nerve paralysis. Understandably, the likelihood of facial paralysis after trauma depends on the location of the trauma. Most commonly, facial paralysis follows temporal bone fractures, though the likelihood depends on the type of fracture.
Transverse fractures in the horizontal plane present the highest likelihood of facial paralysis (40-50%). Patients may also present with hemotympanum (blood behind the tympanic membrane), sensory deafness, and vertigo – the latter two symptoms due to damage to vestibulocochlear nerve (cranial nerve VIII) and the inner ear. Longitudinal fracture in the vertical plane present a lower likelihood of paralysis (20%). Patients may present with hematorrhea (blood coming out of the external auditory meatus), tympanic membrane tear, fracture of external auditory canal, and conductive hearing loss.
Traumatic injuries can be assessed by computed tomography (CT) and nerve conduction studies (ENoG). In patients with mild injury, management is the same as with Bell's palsy – protect the eyes and wait. In patients with severe injury, progress is followed with nerve conduction studies. If nerve conduction studies show a large (>90%) change in nerve conduction, the nerve should be decompressed. The facial paralysis can follow immediately the trauma due to direct damage to the facial nerve, in such cases a surgical treatment may be attempted. In other cases the facial paralysis can occur a long time after the trauma due to oedema and inflammation. In those cases steroids can be a good help.
Tumours
A tumour compressing the facial nerve anywhere along its complex pathway can result in facial paralysis. Common culprits are facial neuromas, congenital cholesteatomas, hemangiomas, acoustic neuromas, parotid gland neoplasms, or metastases of other tumours.
Patients with facial nerve paralysis resulting from tumours usually present with a progressive, twitching paralysis, other neurological signs, or a recurrent Bell's palsy-type presentation. The latter should always be suspicious, as Bell's palsy should not recur. A chronically discharging ear must be treated as a cholesteatoma until proven otherwise; hence, there must be immediate surgical exploration.
Computed tomography (CT) or magnetic resonance (MR) imaging should be used to identify the location of the tumour, and it should be managed accordingly.
Herpes zoster oticus
Herpes zoster oticus is essentially a herpes zoster infection that affects cranial nerves VII (facial nerve) and VIII (vestibulocochlear nerve). Patients present with facial paralysis, ear pain, vesicles, sensorineural hearing loss, and vertigo. Management includes antivirals and oral steroids.
Acute and chronic otitis media
Otitis media is an infection in the middle ear, which can spread to the facial nerve and inflame it, causing compression of the nerve in its canal. Antibiotics are used to control the otitis media, and other options include a wide myringotomy (an incision in the tympanic membrane) or decompression if the patient does not improve
Chronic otitis media usually presents in an ear with chronic discharge (otorrhea), or hearing loss, with or without ear pain (otalgia). Once suspected, there should be immediate surgical exploration to determine if a cholesteatoma has formed and must be removed.
Neurosarcoidosis
Facial nerve paralysis, sometimes bilateral, is a common manifestation of neurosarcoidosis (sarcoidosis of the nervous system), itself a rare condition.
Differential Diagnosis of Causes of Facial nerve paralysis
In alphabetical order. [1] [2]
- Acoustic neuroma
- Acute otitis externa
- Altitude (barotrauma)
- Anti tetanus serum
- Basal skull fracture
- Botulism
- Brain stem injury
- Cardiofacial Syndrome
- Cholesteatoma
- Cortical injury
- Coxsackievirus infection
- Diabetes Mellitus
- Diphtheria
- Diving (barotrauma)
- Familial Bell's palsy
- Facial nerve neuroma
- Forceps delivery (birth)
- Glomus jugulare tumor
- Gradenigo's Syndrome
- Guillain-Barre Syndrome
- Heerfordt's Syndrome
- Hemangioblastoma
- Hemangioma
- Herpes zoster oticus
- Herpetic vessicles
- HIV infection
- Hypertension
- Hyperthyroidism
- Influenza
- Intoxication
- Ischemic cerebral insult
- Leprosy
- Lyme Disease
- Malignant otitis externa
- Mandibular block anesthesia
- Mastoiditis
- Melkersson-Rosenthal Syndrome
- Meningiomas
- Meningoencephalitis
- Mobius' Syndrome
- Molding (birth)
- Mononucleosis
- Mumps
- Myasthenia Gravis
- Parotid tumor
- Parotitis
- Penetrating inner ear injury
- Pontine glioma
- Pregnancy
- Primary temporal bone tumors
- Rabies vaccine
- Ramsay Hunt's Syndrome
- Sarcoidosis
- Surgery
- Syphilis
- Temporal bone fracture
- Tetanus
- Tuberculosis
- Tumor
Physical Examination
- Complete ears, nose, and throat (ENT) and neurologic exams with physical
Laboratory Findings
- Complete blood count (CBC)
- Erythrocyte sedimentation rate (ESR)
- Lyme titer
- Glucose
MRI and CT
Other Diagnostic Studies
- Workup for cerebrovascular accident (CVA)
- Demyelinating processes
- Cerebrospinal fluid (CSF) analysis
Treatment
- Massage of weakened muscles, tape eye and use eye shield during sleep and possible electrical stimulation of paralyzed muscles (Bell's palsy)
- Treat underlying disease etiologies
- Consider neurologic referral
Pharmacotherapy
- Corticosteroids and IV acyclovir for Bell's palsy
References
Additional Resources
- Acute facial nerve paralysis - Powerpoint slides from a lecture presented to second year medical school students at the University of Western Ontario by Dr. Lorne Parnes on 19 November 2004. These notes are licensed under the FDL.
- Acute facial nerve paralysis - Notes from a lecture presented to second year medical school students at the University of Western Ontario by Dr. Lorne Parnes on 19 November 2004. These notes are licensed under the FDL.
Template:PNS diseases of the nervous system
Template:SIB
de:Fazialislähmung hr:Kljenuti ličnog živca no:Facialisparese