Dysphagia
| Dysphagia | |
| ICD-10 | R13 |
|---|---|
| ICD-9 | 787.2 |
| DiseasesDB | 17942 |
| MedlinePlus | 003115 |
|
WikiDoc Resources for Dysphagia |
|
Articles |
|---|
|
Most recent articles on Dysphagia |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Dysphagia at Clinical Trials.gov Clinical Trials on Dysphagia at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Dysphagia
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Dysphagia Discussion groups on Dysphagia Directions to Hospitals Treating Dysphagia Risk calculators and risk factors for Dysphagia
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Dysphagia |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Dysphagia (Template:IPA) is a medical term defined as "difficulty swallowing." It derives from the Greek root dys meaning difficulty or disordered, and phagia meaning "to eat". It is a sensation that suggests difficulty in the passage of solids or liquids from the mouth to the stomach.[1] Dysphagia is distinguished from similar symptoms including odynophagia, which is defined as painful swallowing, and globus, which is the sensation of a lump in the throat. A psychogenic dysphagia is known as phagophobia.
It is also worthwhile to refer to the physiology of swallowing in understanding dysphagia.
Epidemiology
Swallowing disorders can occur in all age groups, resulting from congenital abnormalities, structural damage, and/or medical conditions.[2] Swallowing problems are a common complaint among older individuals, and the incidence of dysphagia is higher in the elderly,[3] in patients who have had strokes,[4] and in patients who are admitted to acute care hospitals or chronic care facilities. Other causes of dysphagia include head and neck cancer and progressive neurologic diseases like Parkinson's disease, Multiple sclerosis, or Amyotrophic lateral sclerosis. Dysphagia is a symptom of many different causes, which can usually be elicited by a careful history by the treating physician.[5] It should be noted that some patients with dysphagia are not aware of the problem.[2]
Dysphagia is classified into two major types: oropharyngeal dysphagia (or transfer dysphagia) and esophageal dysphagia. In some patients, no organic cause for dysphagia can be found, and these patients are defined as having functional dysphagia.
Complete List of Diffential Diagnoses for Dysphagia
In alphabetical order. [6] [7]
- Abscess
- Achalasia
- Aerophagia
- Agranulocytosis
- Alcoholism
- Allergic swelling
- Amyloidosis
- Amyotrophic Lateral Sclerosis (ALS)
- Angina tonsillaris
- Anxiety disorders
- Aortic aneurysm
- Aspiration of foreign body
- Barret's Syndrome
- Behcet's Syndrome
- Botulism
- Brainstem stroke
- Bronchial carcinoma
- Bulbar palsy
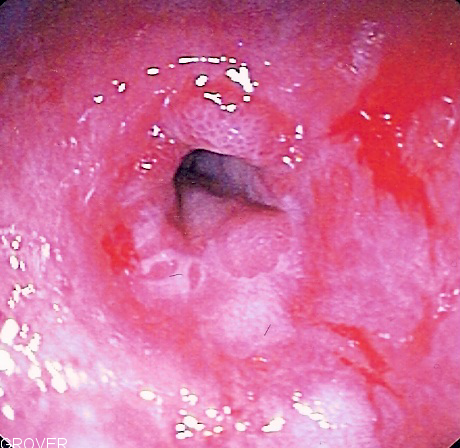
- Candidiasis
- Cascade stomach
- Central hypoglossal nerve paralysis
- Central vagal nucleus lesion
- Cerebrovascular accident (CVA)
- Chagas Disease
- Chemical burns
- CREST syndrome: (calcinosis, raynaud's phenomenon, esophageal dysmotility, sclerodactyly, telangiectasias)
- Cytomegalovirus (CMV)
- Dermatomyositis
- Diabetic neuropathy
- Diphtheria
- Diverticulum
- Enlarged left atrium
- Esophageal cancer
- Esophageal Crohn's disease
- Esophageal diverticulum
- Esophageal moniliasis
- Esophageal sarcoidosis
- Esophageal spasm
- Esophageal trauma
- Esophagotracheal fistula
- Extreme spinal curvature
- Fibrosis
- Food bolus
- Gastric cancer
- Gastritis
- Gastroparesis
- Global hystericus
- Globus syndrome
- Goiter
- Graft-versus-host disease
- Guillain-Barre Syndrome
- Herpangina
- Herpes simplex virus (HSV)
- Hiatal hernia
- Huntington's chorea
- Hyperthyroidism
- Hypokalemia
- Hypothyroidism
- Idiopathic human immunodeficiency virusHIV ulcers
- Impaired sensitivity in the larynx
- Intramural pseudodiverticulosis
- Laryngeal cancer
- Lateral funiculus angina
- Leiomyoma
- Ludwig's angina
- Lymph granulomatosis
- Lymphadenopathy
- Medication-induced esophagitis
- Mononucleosis
- Multiple Sclerosis
- Mumps
- Myasthenia Gravis
- Neoplastic (external compression)
- Nutcracker esophagus
- Oral candidiasis
- Osteophytes
- Palatoplegia after damage to the vagal nerve or the accessory nerve
- Paraneoplastic syndrome
- Parkinson's Disease
- Pericarditis
- Peripheral neuropathy
- Peripheral tongue paralysis with lesions of the hypoglossal nerve
- Pharyngitis
- Pleuritis
- Plummer-Vinson Syndrome
- Poliomyelitis
- Polyradiculitis
- Pseudoachalasia
- Pseudobulbar paralysis
- Pyloric stenosis
- Rabies
- Radiation esophagitis
- Reflux esophagitis
- Rheumatoid Arthritis
- Scarlet Fever
- Schatzki ring
- Scleroderma
- Stevens-Johnson Syndrome
- Stomatitis
- Syringobulbia
- Systemic Lupus Erythematosus
- Tetanus
- Tonsillar abscess
- Typhoid fever angina
- Vascular abnormality
- Vincent's angina
- Zenker's Diverticulum
Oropharyngeal dysphagia
Arises from abnormalities of the upper esophagus, pharynx, and oral cavity.
Signs and symptoms
Some signs and symptoms of swallowing difficulties or dysphagia include the inability to recognize food and taste it, difficulty placing food in the mouth, inability to control food or saliva in the mouth, difficulty initiating a swallow, coughing, choking, frequent pneumonia, unexplained weight loss, gurgly or wet voice after swallowing, nasal regurgitation, and patient complaint of swallowing difficulty.[2] When asked where the food is getting stuck patients will often point to the cervical (neck) region as the site of the obstruction. However, this may be misleading due to patients' inaccurate sensation of the site of obstruction (with obstructions / dysmotilities lower in the esophagus being common).
Symptoms of dysphagia in adults may include:
- Hesitation or inability to swallow
- Difficult or painful swallowing
- Constant feeling of a lump in the throat
- Food sticking in the throat
- Food coming up (regurgitation) through the throat or nose
- Chest pain or discomfort when swallowing
- Difficulty swallowing solid foods
- Frequent, repetitive swallowing
- Excessive throat clearing
- "Gurgly" sounding voice after eating
- Hoarse voice or recurrent sore throat
- Coughing during or after swallowing
- Necessity to "wash down" solid foods
- Recurrent episodes of pneumonia
- Frequent heartburn
- Food or stomach acid backing up into your throat (acid reflux)
- Unexpected weight loss
In infants and children, signs and symptoms may include:
- Low interest in feeding or meals
- Tension in the body while feeding
- Refusal to eat foods that have certain textures
- Lengthy feeding or eating times (30 minutes or longer)
- Food or liquid leaking from the mouth
- Coughing or gagging when eating or nursing
- Spitting up or vomiting during feeding or meals
- Strained breathing while eating and drinking
- Poor weight gain or growth
Complications
If left untreated, dysphagia can potentially cause aspiration pneumonia, malnutrition, or dehydration, all of which can be symptoms of dysphagia as well.[2]
Etiology and differential diagnosis
- A stroke can trigger a rapid onset of dysphagia with a high occurrence of aspiration. The function of normal swallowing may or may not return completely following an acute phase lasting approximately 6 weeks. [8]
- Parkinson's disease can cause "multiple prepharyngeal, pharyngeal, and esophageal abnormalities". The severity of the disease most often correlates with the severity of the swallowing disorder.[8]
- Neurologic disorders such as stroke, Parkinson's disease, amyotrophic lateral sclerosis, Bell's palsy, or myasthenia gravis can cause weakness of facial and lip muscles that are involved in coordinated mastication as well as weakness of other important muscles of mastication and swallowing.
- Oculopharyngeal muscular dystrophy is a genetic disease with palpebral ptosis, oropharyngeal dysphagia, and proximal limb weakness.
- Decrease in salivary flow, which can lead to dry mouth or xerostomia, can be due to Sjogren's syndrome, anticholinergics, antihistamines, or certain antihypertensives and can lead to incomplete processing of food bolus.
- Xerostomia can reduce the volume and increase the viscosity of oral secretions making bolus formation difficult as well as reducing the ability to initate and swallow the bolus[8]
- Dental problems can lead to inadequate chewing.
- Abnormality in oral mucosa such as from mucositis, aphthous ulcers, or herpetic lesions can interfere with bolus processing.
- Mechanical obstruction in the oropharynx may be due to malignancies, cervical rings or webs, or cervical osteophytes.
- Increased upper esophageal sphincter tone can be due to Parkinson's disease which leads to incomplete opening of the UES. This may lead to formation of a Zenker's diverticulum.
- Pharyngeal pouches typically cause difficulty in swallowing after the first mouthful of food, with regurgitation of the pouch contents. These pouches are also marked by malodorous breath due to decomposing foods residing in the pouches. (See Zenker's diverticulum)
- Dysphagia is often a side effect of surgical procedures like anterior cervical spine surgery, carotid endarterectomy, head and neck resection, oral surgeries like removal of the tongue, and parietal laryngectomies [8]
- Radiotherapy, used to treat head and neck cancer, can cause tissue fibrosis in the irradiated areas. Fibrosis of tongue and larynx lead to reduced tongue base retraction and laryngeal elevation during swallowing[8]
- Infection may cause pharyngitis which can prevent swallowing due to pain.
- Medications can cause central nervous system effects that can result in an oropharyngeal dysphagia. Examples: sedatives, hypnotic agents, anticonvulsants, antihistamines, neuroleptics, barbiturates, and antiseizure medication. Medications can also cause peripheral nervous system effects resulting in an oropharyngeal dysphagia. Examples: corticosteroids, L-tryptophan, and anticholinergics[8]
Assessment of adults
A Speech Language Pathologist is most often the first person called upon to evaluate a patient with suspected dysphagia. During this informal examination, medical history is obtained, the mini-mental state examination is administered, and oral and facial sensorimotor function, speech, and swallowing are evaluated non-instrumentally.
A patient needing further investigation will most likely receive a Modified Barium Swallow (MBS). Different consistencies of liquid and food mixed with barium sulfate are fed to the patient by spoon, cup or syringe, and x-rayed using videofluoroscopy. A patient's swallowing then can be evaluated and described. Some clinicians might choose to describe the swallow in detail, making mention of any delays or deviations from the norm. Others might choose to use a rating scale such as the Penetration Aspiration Scale. The scale was developed to describe the disordered physiology of a person's swallow using the numbers 1-8.[9] Other scales also exist for this purpose.
A patient can also be assessed using videoendoscopy, also known as flexible fiberoptic endoscopic examination of swallowing (FEES). The instrument, is placed into the nose until the clinician can view the pharynx and then he or she examines the pharynx and larynx before and after swallowing. During the actual swallow, the camera is blocked from viewing the anatomical structures. A rigid scope, placed into the oral cavity to view the structures of the pharynx and larynx, can also be used, however; the patient cannot swallow.[2]
Other less frequently used assessments of swallowing are imaging studies, ultrasound and scintigraphy and nonimaging studies, electromyography (EMG), electroglottography (EGG) (records vocal fold movement), cervical auscultation, and pharyngeal manometry.[2]
Treatment
After assessment, a Speech Language Pathologist will determine the safety of the patient's swallow and recommend treatment accordingly. The Speech Language Pathologist will also advise staff/caregivers and give information about what signs to look for to know if the client is aspirating (e.g. coughing, choking, voice quality becoming 'wet' or 'gurgly', chest colds, recurrent pneumonia) and feeding instructions if required, including posture while eating, consistency of food, and size of mouthfuls.
Postural techniques.[2]
- Head back (extension) – used when movement of the bolus from the front of the mouth to the back is inefficient; this allows gravity to help move the food.
- Chin down (flexion) – used when there is a delay in initiating the swallow; this allows the valleculae to widen, the airway to narrow, and the epiglottis to be pushed towards the back of the throat to better protect the airway from food.
- Chin down (flexion) – used when the back of the tongue is too weak to push the food towards the pharynx; this causes the back of the tongue to be closer to the pharyngeal wall.
- Head rotation (turning head to look over shoulder) to damaged or weaker side with chin down – used when the airway is not protected adequately causing food to be aspirated; this causes the epiglottis to be put in a more protective position, it narrows the entrance of the airway, and it increases vocal fold closure.
- Lying down on one side – used when there reduced contraction of the pharynx causing excess residue in the pharynx; this eliminates the pull of gravity that may cause the residue to be aspirated when the patient resumes breathing.
- Head rotation to damaged or weaker side – used when there is paralysis or paresis on one side of the pharyngeal wall; this causes the bolus to go down the stronger side.
- Head tilt (ear to shoulder) to stronger side – used when there is weakness on one side of the oral cavity and pharyngeal wall; this causes the bolus to go down the stronger side.
Swallowing Maneuvers.[2]
- Supraglottic swallow - The patient is asked to take a deep breath and hold their breath. While still holding their breath they are to swallow and then immediately cough after swallowing. This technique can be used when there is reduced or late vocal fold closure or there is a delayed pharyngeal swallow.
- Super-supraglottic swallow - The patient is asked to take a breath, hold their breath tightly while bearing down, swallow while still holding the breath hold, and then coughing immediately after the swallow. This technique can be used when there is reduced closure of the airway.
- Effortful swallow - The patient is instructed to squeeze their muscles tightly while swallowing. This may be used when there is reduced posterior movement of the tongue base.
- Mendelsohn maneuver - The patient is taught how to hold their adam's apple up during a swallow. This technique may be used when there is reduced laryngeal movement or a discoordinated swallow.
Diet modification
Diet modification may be warranted. Some patients require a soft diet that is easily chewed, and some require liquids of a thickened or thinned consistency.
-Environmental modification can be suggested to assist and reduce risk factors for aspiration. For example: having the patient use a straw while drinking liquids, putting a pillow behind the patient's head during feeding, removing distractors like too many people in the room or turning off the TV during feeding, etc.
Oral sensory awareness techniques
Oral sensory awareness techniques can be used with patients who have a swallow apraxia, tactile agnosia for food, delayed onset of the oral swallow, reduced oral sensation, or delayed onset of the pharyngeal swallow.[2]
- pressure of a spoon against tongue
- using a sour bolus
- using a cold bolus
- using a bolus that requires chewing
- using a bolus larger than 3mL
- thermal-tactile stimulation (controversial)
Vitalstim Therapy
Vitalstim Therapy ([2]) or electrical stimulation (E-stim) is targeted for oropharyngeal dysphagia and uses electrical stimulation to retrain the muscles used in swallowing. This type of therapy being used in a clinical setting is also very controversial because it lacks evidence of effectiveness. Please see external links for more information.
Prosthetics
- Palatal lift or obturator
- Maxillary denture
Surgical treatment
Surgical treatments are usually only recommended as a last resort.
- Tracheotomy
- Tracheostomy
- Vocal fold augmentation/injection
- Thryoplasty medialization
- Arytenoid adduction
- Partial or total laryngectomy
- Laryngotracheal separation
- Supralaryngetomy
- Palatoplasty
- Cricopharyngeal Myotomy
- Zenker's Diverticulectomy
- Percutaneous endoscopic gastrostomy
Esophageal dysphagia
Arises from the body of the esophagus, lower esophageal sphincter, or cardia of the stomach. Usually due to mechanical causes or motility problems.
Symptoms, signs, and evaluation
Patients usually experience food getting stuck several seconds after swallowing, and will point to the suprasternal notch or behind the sternum as the site of obstruction. If there is dysphagia to both solids and liquids, then it is most likely a motility problem. If there is dysphagia initially to solids but progresses to also involve liquids, then it is most likely a mechanical obstruction. Once a distinction has been made between a motility problem and a mechanical obstruction, it is important to note whether the dysphagia is intermittent or progressive. An intermittent motility dysphagia likely can be diffuse esophageal spasm (DES) or nonspecific esophageal motility disorder (NEMD). Progressive motility dysphagia disorders include scleroderma or achalasia with chronic heartburn, regurgitation, respiratory problems, or weight loss. Intermittent mechanical dysphagia is likely to be an esophageal ring. Progressive mechanical dysphagia is most likely due to peptic stricture or esophageal cancer.
Tree diagram of esophageal dysphagia
Schematically the above can be presented as a tree diagram:
| Esophageal dysphagia | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Solids & liquids (Neuromuscular) | Solids only (Mechanical obstruction) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Progressive | Intermittent | Intermittent | Progressive | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Scleroderma | Achalasia | Diffuse esophageal spasm | Lower esophageal ring | Cancer | Peptic stricture | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
Etiology and differential diagnosis (causes)
Peptic stricture, or narrowing of the esophagus, is usually a complication of acid reflux, most commonly due to gastroesophageal reflux (GERD). These patients are usually older and have had GERD for a long time. Acid reflux can also be due to other causes, such as Zollinger-Ellison syndrome, NG tube placement, and scleroderma. Other non-acid related causes of peptic strictures include infectious esophagitis, ingestion of chemical irritant, pill irritation, and radiation. Peptic stricture is a progressive mechanical dysphagia, meaning patients will complain of initial intolerance to solids followed by inability to tolerate liquids. Usually the threshold to solid intolerance is 13 mm of the esophageal lumen. Symptoms relating to the underlying cause of the stricture usually will also be present.
Esophageal cancer also presents with progressive mechanical dysphagia. Patients usually come with rapidly progressive dysphagia first with solids then with liquids, weight loss (> 10 kg), and anorexia (loss of appetite). Esophageal cancer usually affects the elderly. Esophageal cancers can be either squamous cell carcinoma or adenocarcinoma. Adenocarcinoma is the most prevalent in the US and is associated with patients with chronic GERD who has developed Barrett's esophagus (intestinal metaplasia of esophageal mucosa). Squamous cell carcinoma is more prevalent in Asia and is associated with tobacco smoking and alcohol use.
Esophageal rings and webs, are actual rings and webs of tissue that may occlude the esophageal lumen.
- Rings --- Also known as Schatzki rings from the discoverer, these rings are usually mucosal rings rather than muscular rings, and are located near the gastroesophageal junction at the squamo-columnar junction. Presence of multiple rings may suggest eosinophilic esophagitis. Rings cause intermittent mechanical dysphagia, meaning patients will usually present with transient discomfort and regurgitation while swallowing solids and then liquids, depending on the constriction of the ring.
- Webs --- Usually squamous mucosal protrusion into the esophageal lumen, especially anterior cervical esophagus behind the cricoid area. Patients are usually asymptomatic or have intermittent dysphagia. An important association of esophageal webs is to the Plummer-Vinson syndrome in iron deficiency, in which case patients will also have anemia, koilonychia, fatigue, and other symptoms of anemia.
Achalasia is an idiopathic motility disorder characterized by failure of lower esophageal sphincter (LES) relaxation as well as loss of peristalsis in the distal esophagus, which is mostly smooth muscle. Both of these features impair the ability of the esophagus to empty contents into the stomach. Patients usually complain of dysphagia to both solids and liquids. Dysphagia to liquids, in particular, is a characteristic of achalasia. Other symptoms of achalasia include regurgitation, night coughing, chest pain, weight loss, and heartburn. The combination of achalasia, adrenal insufficiency, and alacrima (lack of tear production) in children is known as the triple A (Allgrove) syndrome. In most cases the cause is unknown (idiopathic), but in some regions of the world, achalasia can also be caused by Chagas disease due to infection by Trypanosoma cruzi.
Scleroderma is a disease characterized by atrophy and sclerosis of the gut wall, most commonly of the distal esophagus (~90%). Consequently, the lower esophageal sphincter cannot close and this can lead to severe gastroesophageal reflux disease (GERD). Patients typically present with progressive dysphagia to both solids and liquids secondary to motility problems or peptic stricture from acid reflux.
Spastic motility disorders include diffuse esophageal spasm (DES), nutcracker esophagus, hypertensive lower esophageal sphincter, and nonspecific spastic esophageal motility disorders (NEMD).
- DES can be caused by many factors that affect muscular or neural functions, including acid reflux, stress, hot or cold food, or carbonated drinks. Patients present with intermittent dysphagia, chest pain, or heartburn.
Rare causes of esophageal dysphagia not mentioned above
- Diverticulum
- Aberrant subclavian artery, or (dysphagia lusoria)
- Cervical osteophytes
- Enlarged aorta
- Enlarged left atrium
- Mediastinal tumor
Diagnostic tools
Once esophageal dysphagia has been implicated, the next step is either a barium swallow or an upper endoscopy. If there is any suspicion of a proximal lesion such as:
- History of surgery for laryngeal or esophageal cancer
- History of radiation or irritating injury
- Achalasia
- Zenker's diverticulum
A barium swallow should be performed first instead of endoscopy to prevent any perforation. If achalasia suspected on barium swallow, manometry is performed next to confirm. If a stricture is suspected, endoscopy is performed. Any other lesions found are treated as such.
If there is no suspicion of any of the above, endoscopy can be performed first. Any structural or mucosal abnormality is treated. A normal endoscopy should be followed by manometry; and if manometry is also normal, the diagnosis is functional dysphagia.
Treatment
The patient is generally sent for a GI, pulmonary, ENT, or oncology consult, depending on the suspected underlying cause. A consultation with a dietician may also be needed, as many patients may need dietary modifications.
See also
References
- ↑ Sleisinger and Fordtran's Gastrointestinal and Liver Disease, 7th edition, Chapter 6, p. 63
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 Logemann, Jeri A. (1998). Evaluation and treatment of swallowing disorders. Austin, Tex: Pro-Ed. ISBN 0-89079-728-5.
- ↑ Shamburek RD; Farrar JT. Disorders of the digestive system in the elderly. N Engl J Med 1990 Feb 15;322(7):438-43.
- ↑ Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005 Dec;36(12):2756-63. Epub 2005 Nov 3.
- ↑ Schatzki R. Panel discussion on diseases of the esophagus. Am J Gastro. 31:117 (1959).
- ↑ Sailer, Christian, Wasner, Susanne. Differential Diagnosis Pocket. Hermosa Beach, CA: Borm Bruckmeir Publishing LLC, 2002:77 ISBN 1591032016
- ↑ Kahan, Scott, Smith, Ellen G. In A Page: Signs and Symptoms. Malden, Massachusetts: Blackwell Publishing, 2004:68 ISBN 140510368X
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 Murray, J. (1999). Manual of Dysphagia Assessment in Adults. San Diego: Singular Publishing.
- ↑ Rosenbek, J. C., Robbins J. A., Roecker, E. B., Coyle, J. L., & Wood, J. L. (1996). A penetration aspiration scale. "Dysphagia, 11," 93-98.
Template:Skin and subcutaneous tissue symptoms and signs Template:Nervous and musculoskeletal system symptoms and signs Template:Urinary system symptoms and signs Template:Cognition, perception, emotional state and behaviour symptoms and signs Template:Speech and voice symptoms and signs Template:General symptoms and signs