Differentiating Diabetes insipidus from other diseases
|
Diabetes insipidus Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Differentiating Diabetes insipidus from other diseases On the Web |
|
American Roentgen Ray Society Images of Differentiating Diabetes insipidus from other diseases |
|
FDA on Differentiating Diabetes insipidus from other diseases |
|
CDC on Differentiating Diabetes insipidus from other diseases |
|
Differentiating Diabetes insipidus from other diseases in the news |
|
Blogs on Differentiating Diabetes insipidus from other diseases |
|
Risk calculators and risk factors for Differentiating Diabetes insipidus from other diseases |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Omodamola Aje B.Sc, M.D. [2]
Overview
Diabetes insipidus must be differentiated from other diseases that cause polyuria, which is defined as a urine output exceeding 3 L/day in adults and 2 L/m2 in children; increased urine frequency, or nocturia; and polydipsia. It is important to know that levels of hypo- or hypernatremia is not sufficient to describe the underlying cause of diabetes insipidus.
Differentiating Diabetes insipidus from other Diseases
Central diabetes insipidus Acquired Trauma (surgery, deceleration injury) Vascular (cerebral hemorrhage, infarction, anterior communicating artery aneurysm or ligation, intra-hypothalamic hemorrhage) Neoplastic (craniopharyngioma, meningioma, germinoma, pituitary tumor or metastases) Granulomatous (histiocytosis, sarcoidosis) Infectious (meningitis, encephalitis) Inflammatory/autoimmune (lymphocytic infundibuloneurohypophysitis) Drug/toxin-induced (ethanol, diphenylhydantoin, snake venom) Other disorders (hydrocephalus, ventricular/suprasellar cyst, trauma, degenerative diseases) Idiopathic Congenital Congenital malformations Autosomal dominant: AVP-neurophysin gene mutations Autosomal recessive X-linked recessive Idiopathic Nephrogenic diabetes insipidus Acquired Drug-induced (demeclocycline, lithium, cisplatin, methoxyflurane, etc.) Hypercalcemia, hypokalemia Infiltrating lesions (sarcoidosis, amyloidosis, multiple myeloma, Sjogren's disease) Vascular (sickle cell disease) Congenital X-linked recessive (OMIM 304800): AVP V2 receptor gene mutations Autosomal recessive: AQP2 water channel gene mutations Primary polydipsia Psychogenic Dipsogenic (downward resetting of thirst threshold) Gestational diabetes insipidus Diabetes mellitus
Differentiating diabetes insipidus based on the type of diabetes insipidus caused
[1][2] Wolfram Syndrome (DIDMOAD)[3]
| Type of DI | Subclass | Disease | Defining signs and symptoms | Lab/Imaging findings |
|---|---|---|---|---|
| Central | Acquired | Histiocytosis |
|
 |
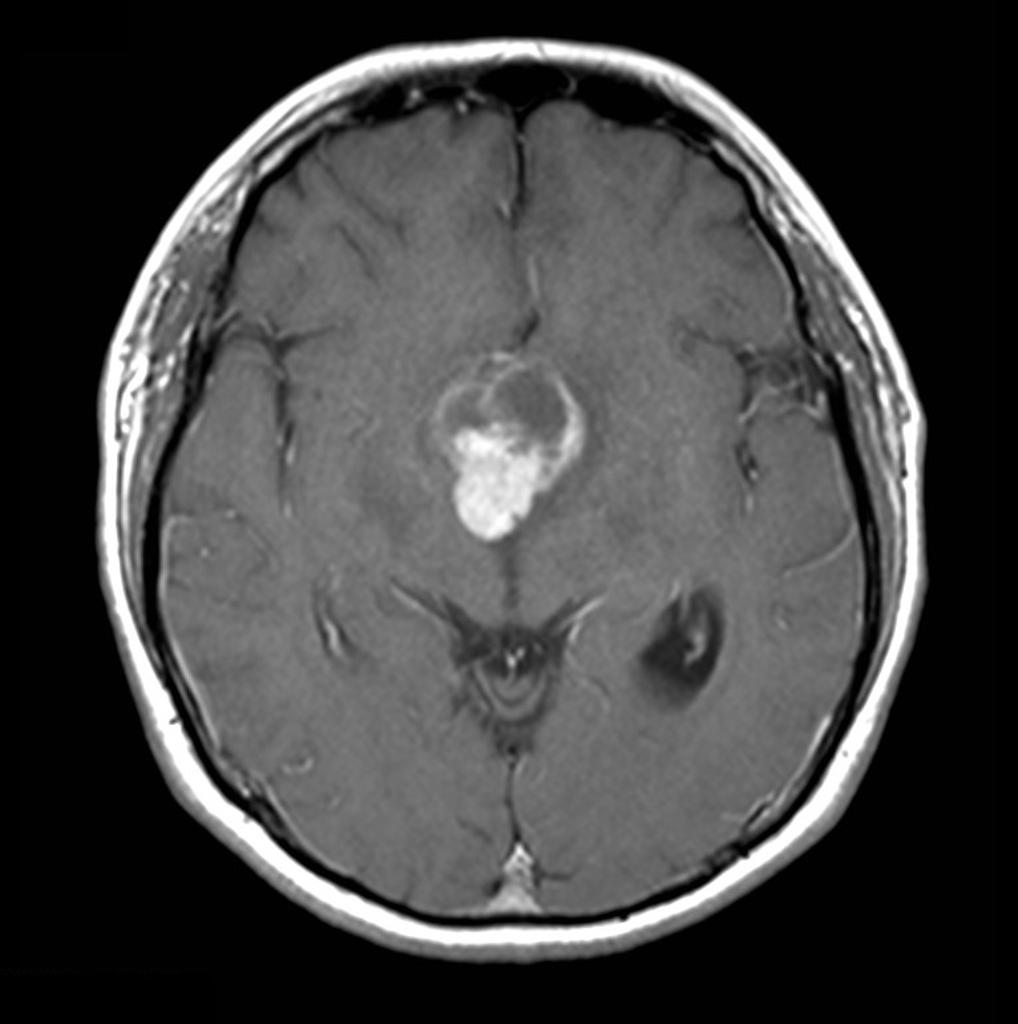
| Craniopharyngioma |
|
 | ||
| Sarcoidosis |
|
 | ||
| Congenital | Hydrocephalus |
|
Dilated ventricles on CT and MRI
 | |
| Wolfram Syndrome (DIDMOAD) |
| |||
| Nephrogenic | Acquired | Drug-induced (demeclocycline, lithium) |
| |
| Hypercalcemia |
| |||
| Hypokalemia |
| |||
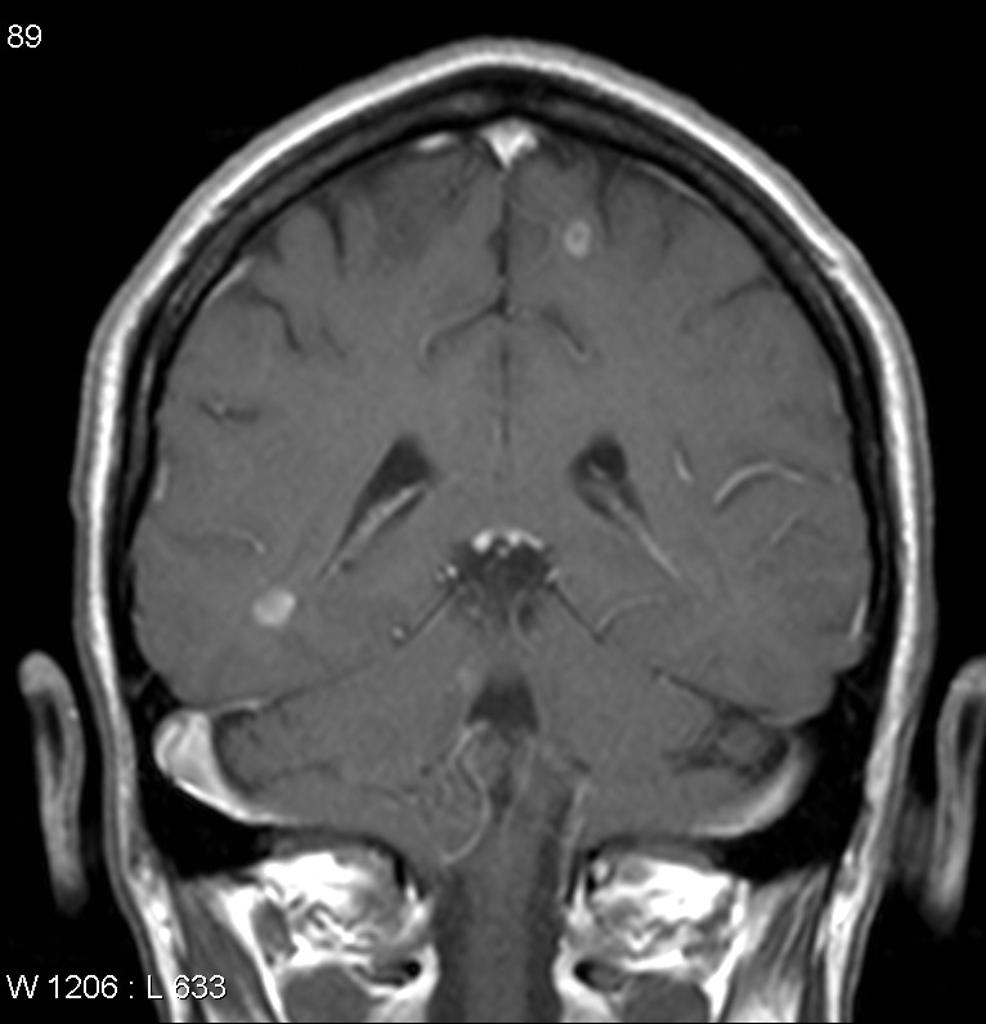
| Multiple myeloma |
|
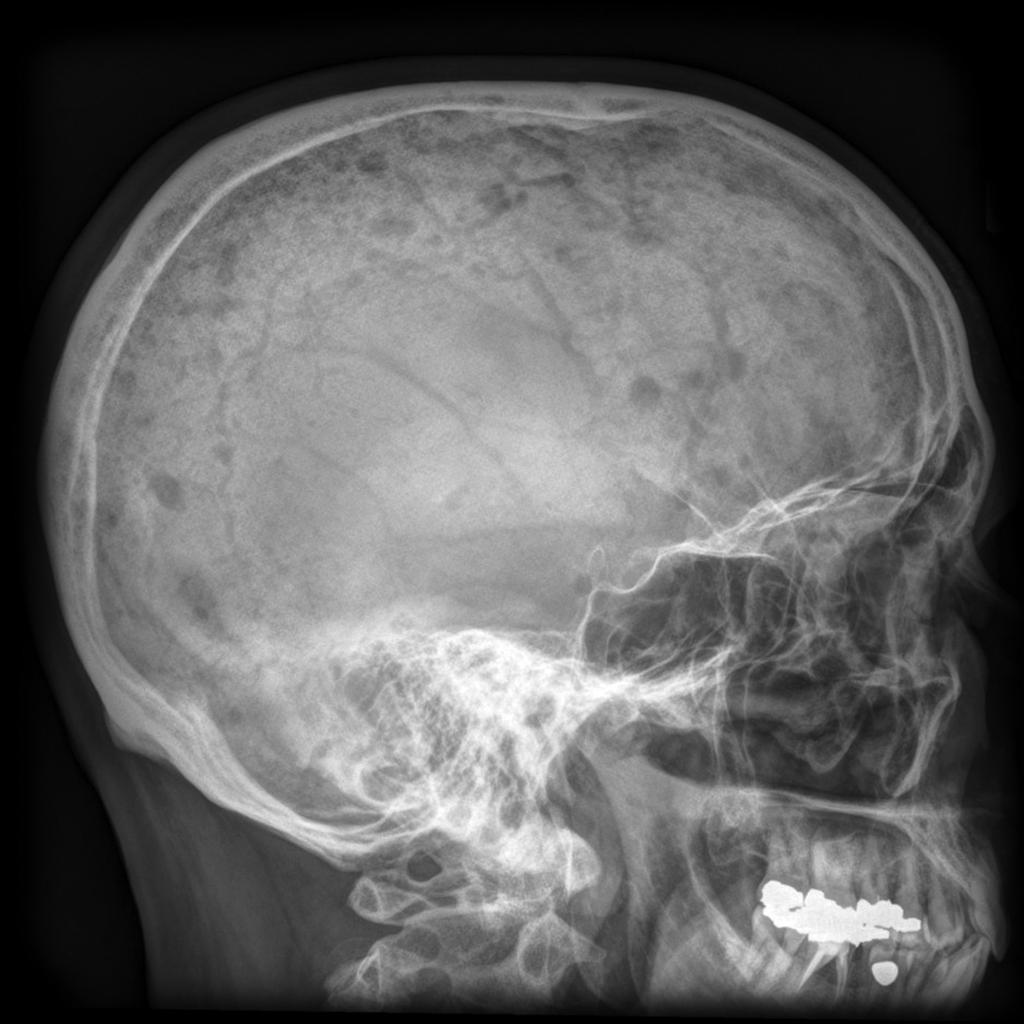 | ||
| Sickle cell disease |
|
 | ||
| Primary polydipsia | Psychogenic |
| ||
| Gestational diabetes insipidus |
| |||
| Diabetes mellitus |
| |||
References
- ↑ Willcutts MD, Felner E, White PC (1999). "Autosomal recessive familial neurohypophyseal diabetes insipidus with continued secretion of mutant weakly active vasopressin". Hum Mol Genet. 8 (7): 1303–7. PMID 10369876.
- ↑ Abu Libdeh A, Levy-Khademi F, Abdulhadi-Atwan M, Bosin E, Korner M, White PC; et al. (2010). "Autosomal recessive familial neurohypophyseal diabetes insipidus: onset in early infancy". Eur J Endocrinol. 162 (2): 221–6. doi:10.1530/EJE-09-0772. PMID 19897608.
- ↑ Barrett TG, Bundey SE (1997). "Wolfram (DIDMOAD) syndrome". J Med Genet. 34 (10): 838–41. PMC 1051091. PMID 9350817.
- ↑ Ghosh KN, Bhattacharya A (1992). "Gonotrophic nature of Phlebotomus argentipes (Diptera: Psychodidae) in the laboratory". Rev Inst Med Trop Sao Paulo. 34 (2): 181–2. PMID 1340034.