Cysticercosis differential diagnosis: Difference between revisions
Jump to navigation
Jump to search
Ahmed Younes (talk | contribs) |
m (Bot: Removing from Primary care) |
||
| (7 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
[[Image:Home_logo1.png|right|250px|link=https://www.wikidoc.org/index.php/Cysticercosis]] | |||
{{CMG}};{{AE}}{{AY}} | {{CMG}};{{AE}}{{AY}} | ||
| Line 18: | Line 18: | ||
| | | | ||
* Presenting symptoms differ according to the site of the cysticerci. | * Presenting symptoms differ according to the site of the cysticerci. | ||
* [[Parenchymal]] | * [[Parenchymal]] neurocysticercosis causes all the symptoms and signs of [[Space occupying lesion|space occupying lesions]]. | ||
* Extraparenchymal neurocysticercosis causes manifestations of [[increased intracranial pressure]] if cysts are present in the [[subarachnoid space]] or in the [[ventricles]], manifestations of [[spinal cord compression]] if present in the spinal cord or causes eye disease if cysts are present in the [[orbit]]. | * Extraparenchymal neurocysticercosis causes manifestations of [[increased intracranial pressure]] if cysts are present in the [[subarachnoid space]] or in the [[ventricles]], manifestations of [[spinal cord compression]] if present in the spinal cord or causes eye disease if cysts are present in the [[orbit]]. | ||
| Line 24: | Line 24: | ||
* [[Immunoblot|CDC's immunoblot]] is based on detection of [[antibody]] to one or more of [[Glycoprotein|7 lentil-lectin purified structural glycoprotein]] [[antigens]] from the larval cysts. | * [[Immunoblot|CDC's immunoblot]] is based on detection of [[antibody]] to one or more of [[Glycoprotein|7 lentil-lectin purified structural glycoprotein]] [[antigens]] from the larval cysts. | ||
* It is 100% [[Specificity (tests)|specific]] and has a [[sensitivity]] superior to that of any other test yet evaluated | * It is 100% [[Specificity (tests)|specific]] and has a [[sensitivity]] superior to that of any other test yet evaluated | ||
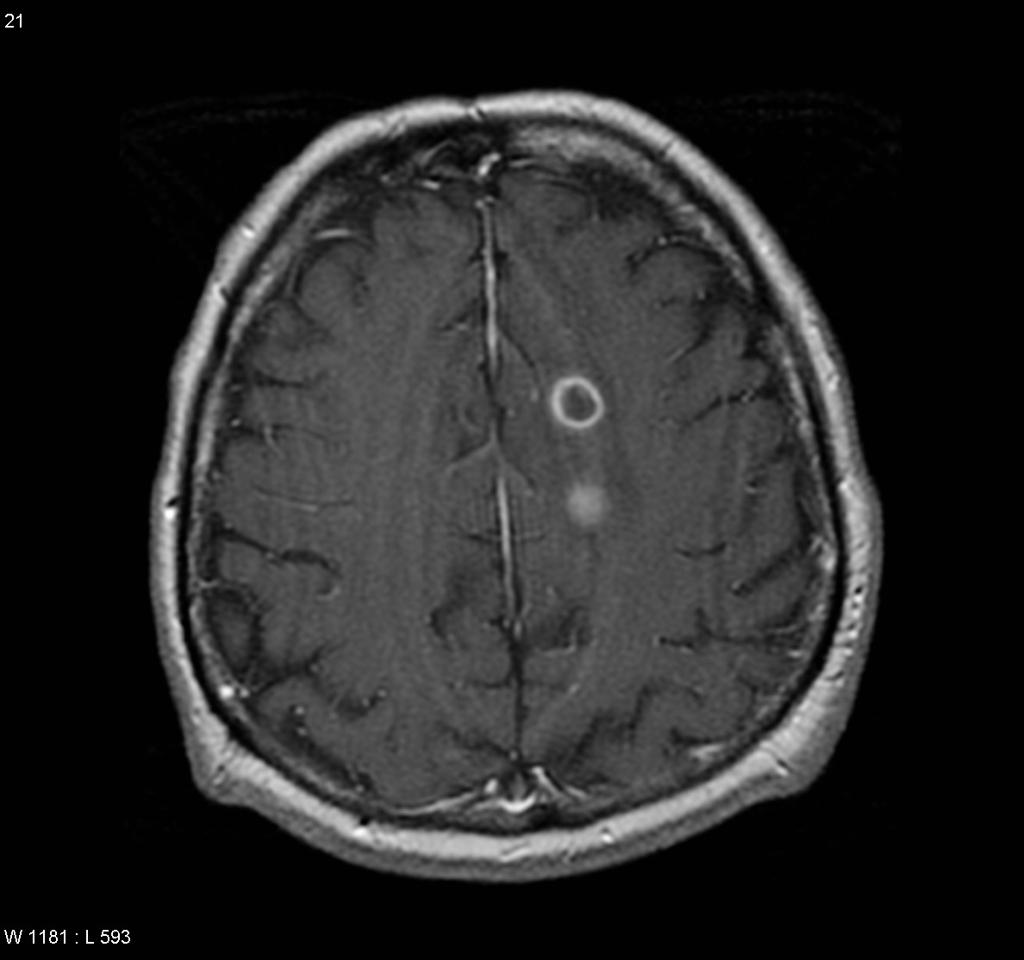
|[[Computed tomography|Computerized tomography (CT)]] is superior to [[magnetic resonance imaging|magnetic resonance imaging (MRI)]] for demonstrating small [[calcification]]s. However, [[MRI]] shows [[cysts]] in some locations (cerebral convexity, [[Ependyma|ventricular ependyma]]) better than [[CT]], is more [[Sensitivity|sensitive]] than CT to demonstrate surrounding [[cerebral edema|edema]], and may show internal changes indicating the death of cysticerci. | | | ||
* [[Computed tomography|Computerized tomography (CT)]] is superior to [[magnetic resonance imaging|magnetic resonance imaging (MRI)]] for demonstrating small [[calcification]]s. | |||
* However, [[MRI]] shows [[cysts]] in some locations (cerebral convexity, [[Ependyma|ventricular ependyma]]) better than [[CT]], is more [[Sensitivity|sensitive]] than CT to demonstrate surrounding [[cerebral edema|edema]], and may show internal changes indicating the death of cysticerci. | |||
|- | |- | ||
|[[Brain abscess]] | |[[Brain abscess]] | ||
| Line 60: | Line 62: | ||
# Signs of [[increased intracranial pressure]] | # Signs of [[increased intracranial pressure]] | ||
# [[Focal neurologic signs|Focal neurologic deficits]]. | # [[Focal neurologic signs|Focal neurologic deficits]]. | ||
|[[TB|T.B.]] should be investigated everywhere else in the body (e.g. [[Lymphadenopathy|peripheral lymphadenopathy]], [[Sputum culture|sputum]] and [[blood culture]]) | | | ||
* [[TB|T.B.]] should be investigated everywhere else in the body (e.g. [[Lymphadenopathy|peripheral lymphadenopathy]], [[Sputum culture|sputum]] and [[blood culture]]) | |||
| | | | ||
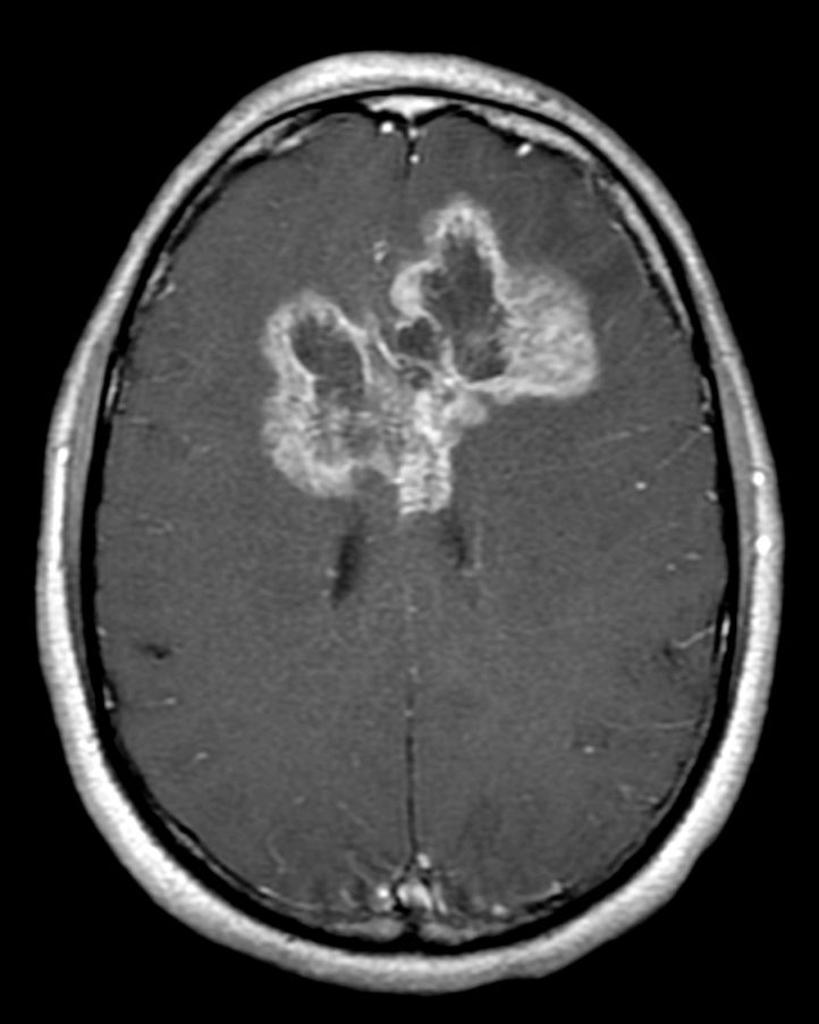
* [[CT]]: [[Contrast enhanced CT|Contrast-enhanced CT]] scan shows a ring enhancing lesion surrounded by an area of hypodensity ([[cerebritis]]) and the resulting [[mass effect]]. | * [[CT]]: [[Contrast enhanced CT|Contrast-enhanced CT]] scan shows a ring enhancing lesion surrounded by an area of hypodensity ([[cerebritis]]) and the resulting [[mass effect]]. | ||
| Line 66: | Line 69: | ||
|- | |- | ||
|Neurosarcoidosis | |Neurosarcoidosis | ||
|70% of the patients present with the neurological symptoms rather than the presentation of systemic disease. Common presentations are:<ref name="urlNeurosarcoidosis">{{cite web |url=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3975794/ |title=Neurosarcoidosis |format= |work= |accessdate=}}</ref> | | | ||
* 70% of the patients present with the neurological symptoms rather than the presentation of systemic disease. Common presentations are:<ref name="urlNeurosarcoidosis">{{cite web |url=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3975794/ |title=Neurosarcoidosis |format= |work= |accessdate=}}</ref> | |||
# Cranial nerve neuropathies: [[Facial palsy]] is the most common presentation. | # Cranial nerve neuropathies: [[Facial palsy]] is the most common presentation. | ||
# [[Meningeal]] involvement: diffuse [[Meningitis|meningeal inflammation]] can cause diffuse [[Polyneuropathy|basilar polyneuropathy]] in 40% of the patients. with [[neurosarcoidosis]]. | # [[Meningeal]] involvement: diffuse [[Meningitis|meningeal inflammation]] can cause diffuse [[Polyneuropathy|basilar polyneuropathy]] in 40% of the patients. with [[neurosarcoidosis]]. | ||
| Line 80: | Line 83: | ||
* [[Lumbar puncture]] shows elevated [[CSF]] proteins together with mild-moderate [[pleocytosis]]. It is usually accompanied by [[oligoclonal bands]].<ref name="urlNeurosarcoidosis">{{cite web |url=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3975794/ |title=Neurosarcoidosis |format= |work= |accessdate=}}</ref> | * [[Lumbar puncture]] shows elevated [[CSF]] proteins together with mild-moderate [[pleocytosis]]. It is usually accompanied by [[oligoclonal bands]].<ref name="urlNeurosarcoidosis">{{cite web |url=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3975794/ |title=Neurosarcoidosis |format= |work= |accessdate=}}</ref> | ||
|[[Magnetic resonance imaging|MRI]] with [[contrast]] shows enhancement of the inflamed areas (i.e. [[cranial nerves]], [[meninges]] or [[Hypothalamic pituitary adrenal axis|HPO axis]]) | | | ||
* [[Magnetic resonance imaging|MRI]] with [[contrast]] shows enhancement of the inflamed areas (i.e. [[cranial nerves]], [[meninges]] or [[Hypothalamic pituitary adrenal axis|HPO axis]]) | |||
|} | |} | ||
{| class="wikitable" | {| class="wikitable" | ||
| Line 97: | Line 101: | ||
!Prominent clinical feature | !Prominent clinical feature | ||
!Radiological findings | !Radiological findings | ||
|- | |- | ||
|[[Coats disease]] | |[[Coats disease]] | ||
| Line 121: | Line 121: | ||
|- | |- | ||
|Hyperthyroid Ophthalmopathy | |Hyperthyroid Ophthalmopathy | ||
|The hallmark is [[Exophthalmos|Eye protrusion]], [[photophobia]], [[lacrimation]] and later in the disease, diminished eye motility.<ref name="urlThyroid Ophthalmopathy - EyeWiki">{{cite web |url=http://eyewiki.aao.org/Thyroid_Ophthalmopathy |title=Thyroid Ophthalmopathy - EyeWiki |format= |work= |accessdate=}}</ref> | | | ||
* The hallmark is [[Exophthalmos|Eye protrusion]], [[photophobia]], [[lacrimation]] and later in the disease, diminished eye motility.<ref name="urlThyroid Ophthalmopathy - EyeWiki">{{cite web |url=http://eyewiki.aao.org/Thyroid_Ophthalmopathy |title=Thyroid Ophthalmopathy - EyeWiki |format= |work= |accessdate=}}</ref> | |||
| | | | ||
* [[Ultrasonography]]: inflamed thickened [[extraocular muscles]]. | * [[Ultrasonography]]: inflamed thickened [[extraocular muscles]]. | ||
| Line 143: | Line 144: | ||
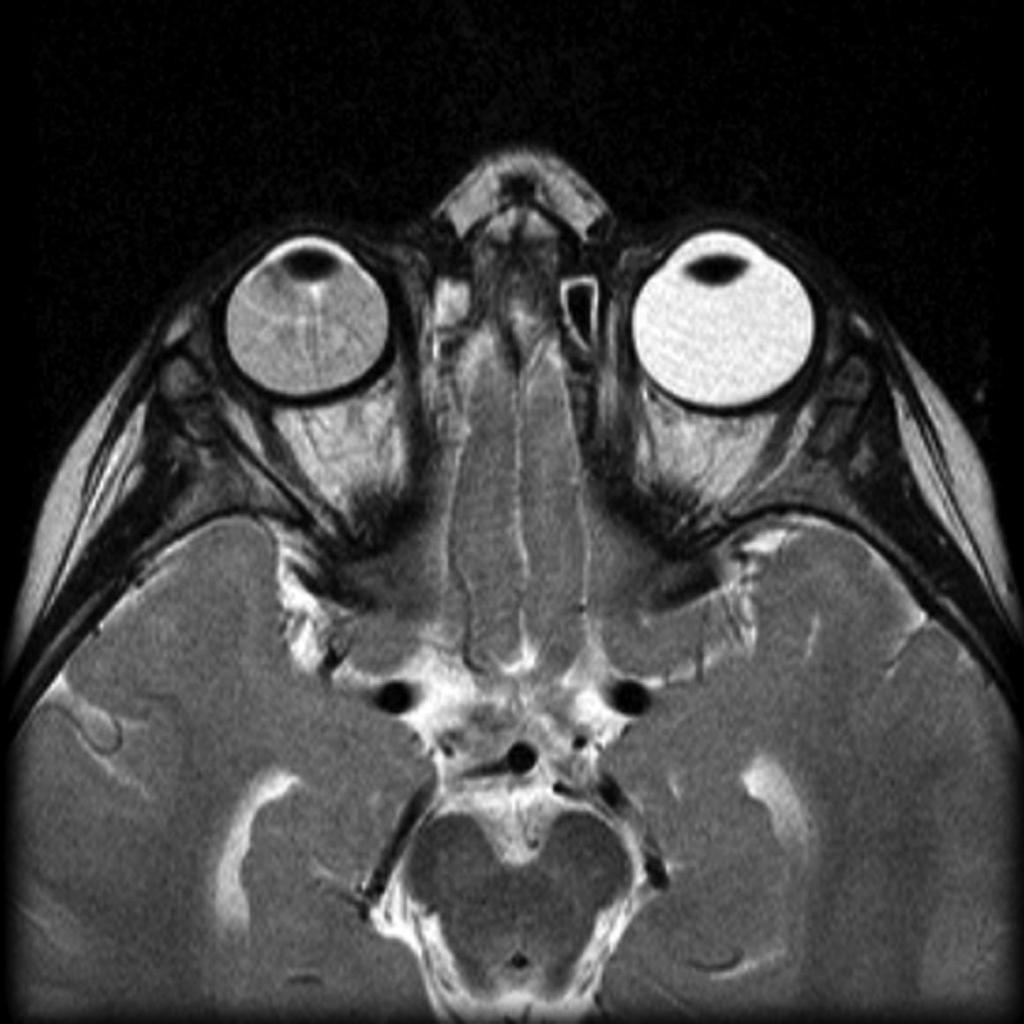
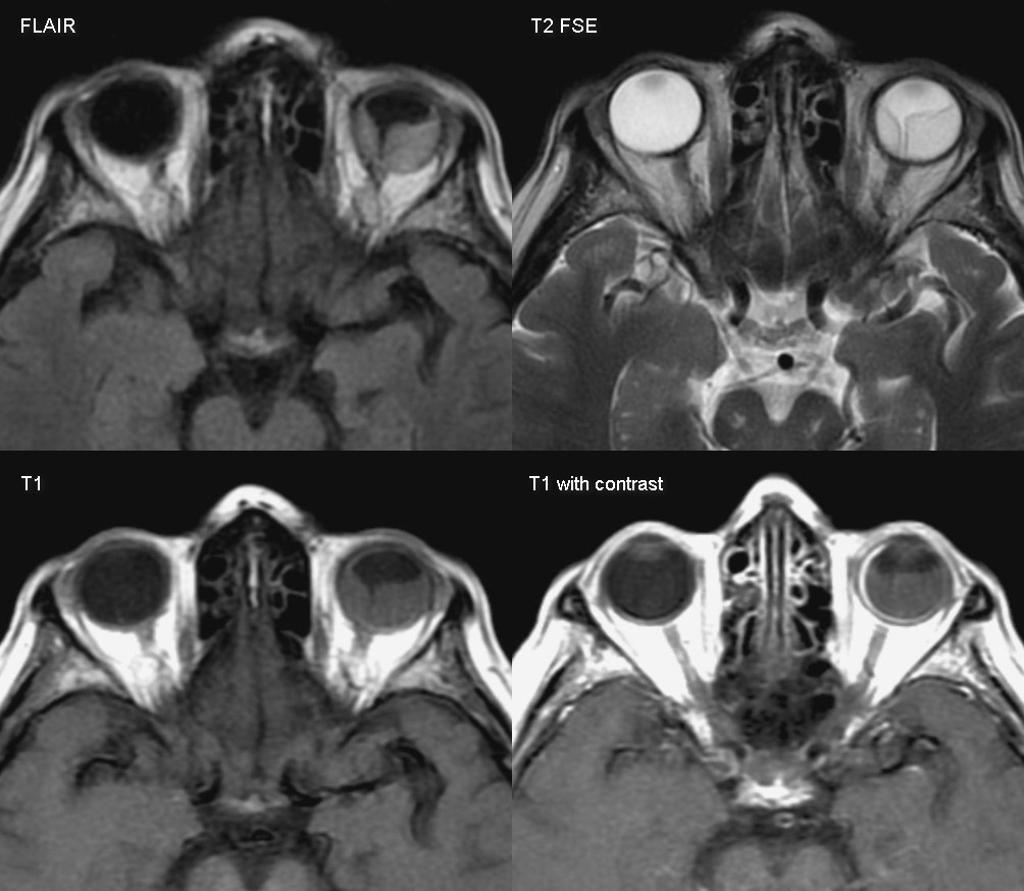
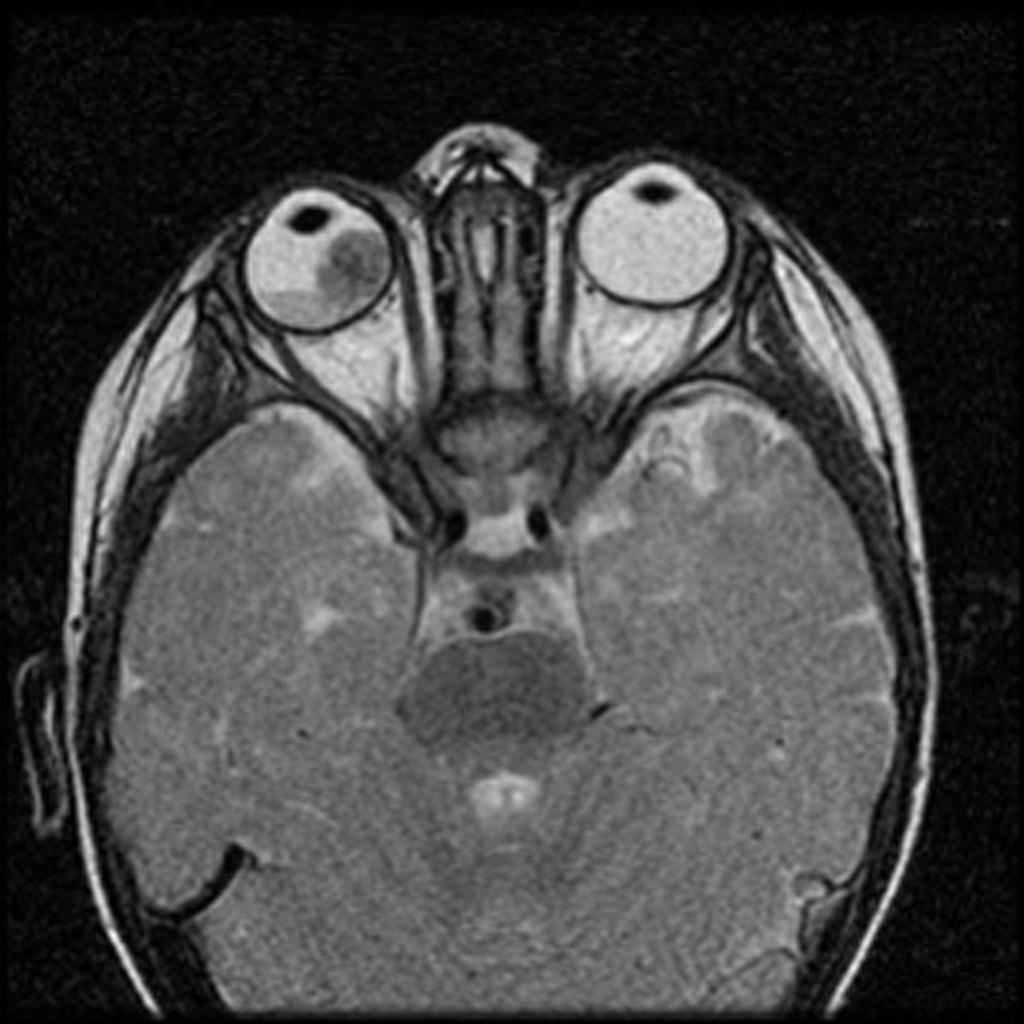
![[Image:Retinoblastoma-3.jpg|center|300px|thumb|MRI of the orbit showing retinoblastoma - Case courtesy of https://radiopaedia.org/. From the case https://radiopaedia.org/cases/11877]] | ![[Image:Retinoblastoma-3.jpg|center|300px|thumb|MRI of the orbit showing retinoblastoma - Case courtesy of https://radiopaedia.org/. From the case https://radiopaedia.org/cases/11877]] | ||
![[Image:Thyroid-orbitopathy-severe-2.jpg|center|300px|thumb|CT head showing hyperthyroid induced orbitopathy - Case courtesy of A.Prof Frank Gaillard, https://radiopaedia.org/. From the case https://radiopaedia.org/cases/4854]] | ![[Image:Thyroid-orbitopathy-severe-2.jpg|center|300px|thumb|CT head showing hyperthyroid-induced orbitopathy - Case courtesy of A.Prof Frank Gaillard, https://radiopaedia.org/. From the case https://radiopaedia.org/cases/4854]] | ||
|} | |} | ||
| Line 150: | Line 151: | ||
{{Reflist|2}} | {{Reflist|2}} | ||
[[Category: | [[Category:Emergency medicine]] | ||
[[Category: | [[Category:Disease]] | ||
[[Category:Up-To-Date]] | |||
[[Category:Infectious disease]] | [[Category:Infectious disease]] | ||
[[Category: | [[Category:Neurology]] | ||
[[Category:Dermatology]] | |||
Latest revision as of 21:11, 29 July 2020

Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Ahmed Younes M.B.B.CH [2]
Overview
Cysticercosis must be differentiated from other diseases that cause brain cystic lesions (as brain abscess and brain tumors) or ocular lesions (as retinal detachment and coats disease).
Differentiating cysticercosis from other diseases
| Disease | Prominent clinical features | Lab findings | Radiological findings |
|---|---|---|---|
| Neurocysticercosis |
|
|
|
| Brain abscess |
|
|
|
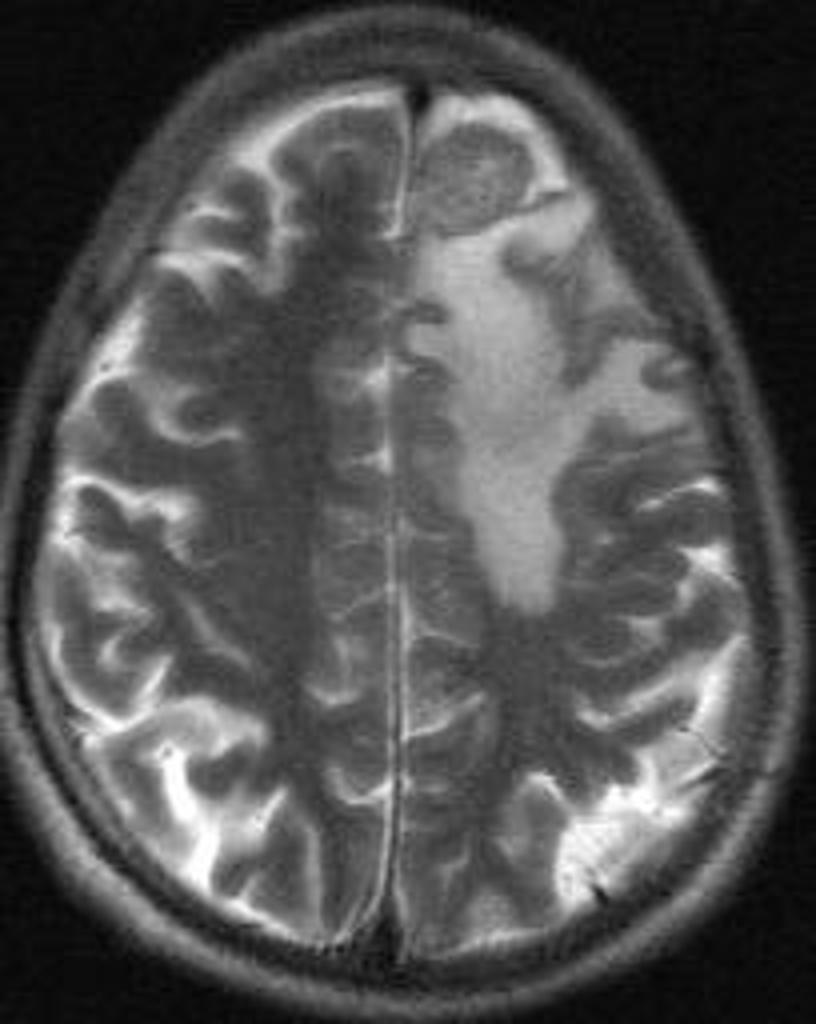
| Brain tumors |
|
| |
| Brain tuberculoma |
|
|
|
| Neurosarcoidosis |
|
|
|
 |
 |
 |
 |
|---|
| Disease | Prominent clinical feature | Radiological findings |
|---|---|---|
| Coats disease |
|
|
| Retinal detachment |
|
|
| Hyperthyroid Ophthalmopathy |
|
|
| Retinoblastoma |
|
|
 |
 |
 |
 |
|---|
References
- ↑ Brouwer MC, Tunkel AR, McKhann GM, van de Beek D (2014). "Brain abscess". N. Engl. J. Med. 371 (5): 447–56. doi:10.1056/NEJMra1301635. PMID 25075836.
- ↑ "Brain Abscess — NEJM".
- ↑ 3.0 3.1 "Primary Brain Tumors in Adults - American Family Physician".
- ↑ "The Journal of Association of Chest Physicians - Tuberculoma of the brain - A diagnostic dilemma: Magnetic resonance spectroscopy a new ray of hope : Download PDF".
- ↑ 5.0 5.1 "Neurosarcoidosis".
- ↑ 6.0 6.1 "How to Diagnose and Manage Coats' Disease".
- ↑ 7.0 7.1 "Management of retinal detachment: a guide for non-ophthalmologists".
- ↑ 8.0 8.1 "Thyroid Ophthalmopathy - EyeWiki".
- ↑ 9.0 9.1 "c.ymcdn.com".